Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Relationship Between the Hemoglobin-to-Red Cell Distribution Width Ratio and All-Cause Mortality in Ischemic Stroke Patients with Atrial Fibrillation: An Analysis from the MIMIC-IV Database
Authors Qin Z , Liao N, Lu X, Duan X, Zhou Q , Ge L
Received 7 December 2021
Accepted for publication 6 February 2022
Published 18 February 2022 Volume 2022:18 Pages 341—354
DOI https://doi.org/10.2147/NDT.S350588
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Yuping Ning
Zuoan Qin,1,2 Nuohan Liao,3 Xuelin Lu,4 Xiangjie Duan,5 Quan Zhou,6 Liangqing Ge1,2
1Jinan University, Guangzhou, 510632, People’s Republic of China; 2Department of Cardiology, The First People’s Hospital of Changde City, Changde, 415003, People’s Republic of China; 3University of South China, Hengyang, Hunan, 421002, People’s Republic of China; 4Department of Pathology, The First People’s Hospital of Changde City, Changde, 415003, People’s Republic of China; 5Department of Infectious Diseases, The First People’s Hospital of Changde City, Changde, 415003, People’s Republic of China; 6Department of Science and Education, The First People’s Hospital of Changde City, Changde, 415003, People’s Republic of China
Correspondence: Liangqing Ge, Email [email protected]
Aim: To investigate the association between the hemoglobin-to-red cell distribution width (RDW) ratio (HRR) and all-cause mortality in ischemic stroke patients with atrial fibrillation (AF).
Design: This study was a retrospective cohort analysis. In total, 1018 ischemic stroke patients with AF were enrolled using the Medical Information Mart for Intensive Care database, (MIMIC)-IV. The patients were divided into four groups according to the HRR values. The primary outcome was 180-day all-cause mortality.
Methods: Multivariate Cox proportional risk regression models were used to examine the association between HRR and all-cause mortality. The non-linear relationship between HRR and all-cause mortality was confirmed using a Cox proportional risk regression model fitted by cubic spline function and smooth curve fitting.
Results: A total of 246/1018 patients (24.17%) died. The serum HRR values were negatively associated with 180-day all-cause mortality (hazard ratio (HR) 0.80, 95% confidence interval (CI) 0.68– 0.94). A two-piecewise regression model was used to obtain a threshold inflection point value of 9.74. The HR and the 95% CI on the left inflection point were 0.73 and 0.61– 0.87 (p = 0.0005); on the right inflection point they were 1.06 and 0.82– 1.38 (p = 0.6383).
Conclusion: The relationship between all-cause mortality and the HRR values was non-linear in ischemic stroke patients with AF. All-cause mortality and HRR values were negatively correlated when the HRR value was ≤ 9.74.
Keywords: ischemic stroke, atrial fibrillation, all-cause mortality, MIMIC-IV
Introduction
According to the report of the Global Burden of Disease Study 2017, strokes are the second leading cause of death and disability worldwide.1 In recent decades, the incidence and mortality rates of ischemic strokes have declined progressively in high income countries but have not changed or have increased in many low and middle income countries.2 AF is one of the most common cardiac arrhythmias and has become a global health interest as its prevalence and associated mortality have grown exponentially in the past decade.3 Strokes are common in patients with AF; AF also increases the risk of a systemic embolism.4 AF is a powerful risk factor for strokes, independently increasing the risk by approximately 5 times in all ages.5 Ischemic strokes with AF are associated with mortality or a significantly higher disability, particularly in older patients.6 In recent years, a series of studies on the HRR and prognosis of cancer patients have been reported,7–10 and a few studies on the HRR and prognosis of coronary heart disease patients have been reported.11 So far, However, there is no relevant report studies HRR on the prognosis of severe ischemic stroke patients with AF and the correlation of adverse events. To the best of our knowledge, this is one of the first studies using the MIMIC-IV database to research the results of ischemic strokes combined with AF. Using the US MIMIC-IV database (version 1.0),12 we conducted the prognosis and related of severely ill ischemic stroke patients with AF as a large sample retrospective analysis.
Materials and Methods
Data Source
This study was a retrospective cohort analysis using the MIMIC-IV database (version 1.0). This database was identified according to the Health Insurance Portability and Accountability Act Safe Harbor provision and has approval from the Massachusetts Institute of Technology and the Institutional Review Board of Beth Israel Deaconess Medical Center (BIDMC).13 The MIMIC-IV database contains the clinical information of patients who were in the intensive care unit (ICU) at BIDMC between 2008 and 2019. One author, Zuoan Qin, completed the Collaborative Institutional Training Initiative examination (certification number: 36208651) to achieve access to the database for the data extraction.
Study Population and Variable Extraction
The total number of outpatients and inpatients listed in the MIMIC-IV database was 257,366 individuals in 2008–2019 with 50,048 patients admitted to the ICU. Only the 2700 patients diagnosed with an ischemic stroke were considered for this research. Among those patients, the inclusion criteria were: adult patients (age ≥ 18 years) with an ischemic stroke defined as ICD-9 codes of 4660, 34,661, 34,662, 34,663, 43,301, 43,311, 43,321, 43,331, 43,381, 43,391, 43,401, 43,411 and 43,491; or ICD-10 codes of I63. The exclusion criteria were: age < 18 years old; patients receiving acute reperfusion therapy; and patients receiving mechanical thrombectomy surgery.All experiments were performed following The First People’s Hospital of Changde City and national guidelines and regulations, and the experiment was approved by the ethics committee of The First People’s Hospital of Changde City.
Definition of HRR and the Outcome Measurement
The HRR is defined using the following equation: HRR = hemoglobin (g/L)/RDW (109/L).7–11 The primary outcome was set to all-cause mortality within 180 days. The secondary results were all-cause mortality within 30, 60 and 90 days. The survival information was obtained from a table named “patients” in the MIMIC-IV database. The length of stay data were extracted from the table named “admissions”. The variables in this study included characteristics, comorbidities, laboratory variables, a severity scoring system, drug use, intensive care unit length of stay (ICU LOS) (days) and time of death. The patient characteristics were collected as follows:
(1) Characteristics: age, gender, heart rate (beats/minute), mean arterial pressure (MAP) (mmHg), respiratory rate (breath/minute), temperature (◦C), saturation of peripheral oxygen (SPO2) (%);
(2) Comorbidities: hypertension, hyperlipidemia, diabetes mellitus, congestive heart failure, myocardial infarction, peripheral vascular disease (PVD), dementia, severe liver disease, rheumatoid arthritis, malignancy, a metastatic solid tumor, paraplegia, peptic ulcer disease, chronic pulmonary disease;
(3) The first value of vital signs and laboratory data within 24 h of intensive care unit (ICU) admission laboratory parameters: white blood cell (WBC), red blood cell (RBC), red cell distribution width (RDW), hemoglobin, platelets, international normalized ratio (INR), prothrombin time (PT), activated partial thromboplastin time (APTT), aspartate aminotransferase (ALT), alanine aminotransferase (AST), creatinine, blood urea nitrogen (BUN), anion gap, bicarbonate, calcium, chloride, potassium, sodium, glucose;
(4) Severity scoring system: sequential organ failure assessment (SOFA) score, simplified acute physiology score (APS) III, simplified acute physiology score (SAPS) II, acute respiratory distress syndrome (ARDS), Oxford acute severity of illness score (OASIS), HAS-BLED score;
(5) Drug use: warfarin, novel oral anticoagulants (NOACs), antiplatelet agents;
(6) Intensive care unit length of stay (ICU LOS) (days) and 30, 60, 90 and 180-day all-cause mortality.
Statistical Analysis
In the first step, we listed the baseline data of the participants (Table 1). The continuous variables were expressed as mean ± standard deviation. The classification variables were expressed as a frequency and a percentage. In the second step, a one-way analysis of variance (one-way ANOVA) test (normal distribution) or a Kruskal–Wallis H-test (skew distribution) was used to detect the difference between the different HRRs (four quantiles). We used univariate and multivariate Cox proportional hazard regression models to build three different models including a crude model (unadjusted for covariates), model 1 (adjusted for age and gender only) and model 2 (adjusted for potential confounding factors).We used weighted univariate and multivariate logistic regression models based on the recommendations of the STROBE statement. We also demonstrated the results of an unadjusted, a minimum adjusted and a fully adjusted analysis. Whether to adjust the covariance or not was determined by the following principle: when added to the model, the matching odds ratio was changed by at least 10%. In addition, we also used the generalized additive model (GAM) to identify the non-linear relationships. If a non-linear correlation was observed, we performed a two-piece linear regression model to calculate the threshold effect of the HRR on all-cause mortality based on the smoothed graph. When the ratio of the HRR to the all-cause mortality was obvious in the smooth curve, the recursive method automatically calculated the inflection point and the maximum model likelihood was used. A hierarchical linear regression model was used for the subgroup analysis.
 |
Table 1 Baseline Characteristics |
We used the statistical packages R (The R Foundation; http://www.r-project.org; version 3.4.3) and Empower Stats (www.empowerstats.com; X&Y Solutions, Inc.) to perform the whole process of the data analysis.
Results
Selection of Participants
The study included 2700 patients who were admitted to the intensive care unit due to an ischemic stroke for the first time, of which 1682 were excluded from the study. Of those excluded, 1674 patients had no history of AF and 8 patients were without hemoglobin or RDW data. A total of 1018 participants were selected for the final data analysis (see the flowchart in Figure 1).
 |
Figure 1 Flowchart of subject screening. |
Baseline Characteristics
The 1018 patients (aged ≥ 18 years) were aged 77.52 ± 11.38 years and comprised 561 (55.1%) females. Of the 1018 patients, 246 (24.17%) died within 180 days. According to the HRR values, 255, 254, 254 and 255 patients belonged to the Q1 (≥ 2.20 and < 6.51), Q2 (≥ 6.52 and < 8.35), Q3 (≥ 8.36 and < 9.84) and Q4 (≥ 9.85 and < 15.83) categories, respectively. The difference group was evaluated by the Pearson χ2 test for the binary variables and the t-test for the continuous variables. The continuous variables were expressed in the form of mean ± standard deviation (SD) and the binary variables were expressed in the form of counts and proportions. All variables are listed in Table 1.
Univariate Analysis
Table 2 shows the results of the univariate analysis that indicated that the age (p = 0.0001), WBC (p = 0.0165), RDW (p = 0.0007), BUN (p = 0.0002), anion gap (p = 0.0001), APSIII (p < 0.0001), SAPSII (p < 0.0001), OASIS (p < 0.0001), SOFA (p = 0.0002), malignancy (p = 0.0052), metastatic solid tumor (p = 0.0034) and respiratory rate (p = 0.0002) positively correlated with mortality. HRR (p =0.0144), Hyperlipidemia (p = 0.0364), warfarin use (p < 0.0001), NOAC drug use (p < 0.0001), antiplatelet agent drug use (p < 0.0001), SPO2 (%) (p = 0.0002) and ICU LOS (p < 0.0001) negatively correlated with mortality.
 |
Table 2 Factors Correlated to All-Cause Mortality in HRR by Univariate Analysis |
The Association Between the HRR and All-Cause Mortality
Both univariate and multivariate Cox proportional-hazards regression models were introduced to evaluate the associations between the HRR and 30-day, 60-day, 60-day and 180-day mortality of in ischemic stroke patients with AF (Table 3). Meanwhile, we show the non-adjusted and adjusted models in Table 3. We found that lower the HRR was associated with increased risk of 30-day mortality (non-adjusted model: HR,0.95, 95% CI, 0.89–1.00, p = 0.0648; minimally-adjusted model: HR,0.95, 95% CI,0.90–1.01, p = 0.0811; fully-adjusted model: HR,0.79,95% CI,0.67–0.93, p = 0.0057),the same finding that lowering the HRR was associated with an increased risk of 60-day, 90-day, and 180-day mortality (Table 3). For the purpose of sensitivity analysis, we also treated the HRR as a categorical variable (the four quantiles) and discovered the same trend.
 |
Table 3 Univariate and Multivariate Results by Cox Regression |
Analysis of the Non-Linear Relationship Between the HRR and 180-Day All-Cause Mortality
In this study, we observed that the relationship between the HRR and all-cause mortality in patients with an ischemic stroke was non-linear (Figure 2) after adjusting for gender, age, hyperlipidemia, myocardial infarctions, congestive heart failure, PVD, dementia, severe liver disease, malignancy, metastatic solid tumors, paraplegia, peptic ulcer disease, chronic pulmonary disease, rheumatoid arthritis, INR, PT, PTT, WBC, RBC, platelets, ALT, AST, anion gap bicarbonate, BUN, calcium, chloride, creatinine, glucose, potassium, sodium, warfarin use, NOAC drug use, antiplatelet agent drug use and ICU LOS. Using a two-segment linear regression model, we calculated that the inflection point was 9.74 (HRR = 9.74) (Table 4). There was no significant correlation to the right of the inflection point (HR (95% CI) 1.06 (0.82–1.38), p = 0.6383); however, there was a negative correlation between the HRR value and all-cause mortality to the left of the threshold inflection point (HR 0.73, 95% CI 0.61–0.87, p = 0.0005).
 |
Table 4 Analysis of Nonlinear Relationship the HRR and 180-Day All-Cause Mortality |
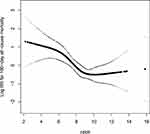 |
Figure 2 The nonlinear relationship between the HRR and 180-day All-Cause Mortality. |
Subgroup Analysis of the Associations Between the HRR Values and All-Cause Mortality
Table 5 displays the results of the subgroup analysis regarding the outcome of all-cause mortality. The tests for the interactions were not statistically significant for gender, age, hyperlipidemia, diabetes mellitus, congestive heart failure, myocardial infarctions, PVD, dementia, severe liver disease, rheumatoid arthritis, malignancy, metastatic solid tumors, peptic ulcer disease, warfarin use and antiplatelet agent drug use (p = 0.4026, 0.6493, 0.1864, 0.2439, 0.5211, 0.5523, 0.2827, 0.6618, 0.3607, 0.5779, 0.2330, 0.4142, 0.4907, 0.7837 and 0.4865, respectively). The tests for interactions were significant for hypertension (p = 0.0184) and NOAC drug use (p = 0.0089). The negative association between the HRR values and all-cause mortality was more obvious in the ischemic stroke patients with AF without hypertension (HR = 0.75, 95% CI = 0.65–0.87, p = 0.0002) than those with hypertension (HR = 0.91, 95% CI = 0.79–1.05, p = 0.1923).The negative association between the HRR values and all-cause mortality was more obvious in the ischemic stroke patients with AF without NOAC drug use (HR = 0.60, 95% CI = 0.45–0.80, p = 0.0006) than those with NOAC drug use (HR = 0.61, 95% CI = 0.77–0.99, p = 0.321).
 |
Table 5 Subgroup Analysis of the Associations Between the HRR Values and All-Cause Mortality |
Discussion
In this study, we clearly revealed the potential non-linear trend between the HRR and all-cause mortality in ischemic stroke patients with AF. This large retrospective cohort study of critically ill patients with an ischemic stroke has demonstrated that patients with a reduced HRR are more likely to have a higher risk of all-cause mortality even after adjusting for traditional cerebrovascular risk factors.
Strokes remain the second most common cause of death and the main cause of disability in the world.14 An ischemic stroke is the most common type of stroke, accounting for 87% of all stroke types.15 AF is the main cause of a cardiogenic acute ischemic stroke. According to the latest research, the overall mortality rate of ischemic strokes in many countries is on a downward trend.16,17 However, ischemic strokes are still an important cause of death in patients with cerebrovascular diseases and may lead to permanent disability and a significant economic and social burden.18 The decrease in mortality from an ischemic stroke may be partly attributable to improved hospital management.19 Although the overall ischemic stroke hospitalization rate in the United States has decreased, there is an increased hospitalization rate for age-specific ischemic stroke in patients aged 25–64 years.20 Therefore, many clinicians are eager to study the prognosis of ischemic stroke patients.
AF is a known risk factor for ischemic strokes.4,21,22 There are approximately > 2.7 million American AF patients and AF is responsible for 10–12% of all ischemic strokes in the United States each year.23 Among all 19,515 participants of the China‐AF study, 17,898 patients had follow‐up data and 12,045 patients had complete data, After a mean follow‐up of 2.5 years, 1715 cases of the primary endpoint were documented, were each associated with increased risk of all‐cause mortality and nonfatal ischemic stroke.24 The annual risk of an ischemic stroke among individuals with AF can be as high as 18.2% depending on the coexistence of various risk factors.25 Previous reports have demonstrated that in patients with AF, it is meaningful to predict the risk of AF through hemoglobin data.26,27 Lim et al28 reported a nationwide population-based study and found that anemia is a risk factor for incident AF. Both low and high hemoglobin levels are associated with an increased AF risk. Maintaining hemoglobin levels within normal ranges would lower the risk of AF development. Hemoglobin has an oxygen-carrying capacity and can affect the energy balance in the penumbra.29 Patients with low hemoglobin have a reduced ability to carry oxygen in the blood and there is increased blood viscosity in patients with high hemoglobin. Low or high hemoglobin levels increase the risk of ischemic strokes. Sacco et al30 found that there is a U-shaped association between hemoglobin and a poor prognosis of ischemic strokes. Red cell distribution width (RDW) is a measure of the variability of the size of red blood cells. It is calculated automatically or manually by dividing the standard deviation of red blood cell volume and the volume of red blood cell expressed as a percentage. Elevated RDW is a result of increased destruction of red blood cells, eg in the course of haemolysis or red blood cell production dysfunction related to a deficiency of iron, vitamin B12, folic acid or ongoing inflammation.31 Recently, quite a number of publications also demonstrated the utility of the RDW as a prognostic factor for various diseases of the cardiovascular system such as coronary heart disease, peripheral artery disease, acute coronary syndrome, heart failure and stroke.32 Mohindra et al33 showed that a proposed RDW index could potentially be an important parameter in predicting the prognosis of ischemic stroke patients. In the past two years, HRR has been widely reported as an important observation indicator of cancer prognosis.Both hemoglobin and RDW are important components of HRR, and the relationship between lower hemoglobin, higher RDW, and frailty in elderly CHD patients has been confirmed, lower HRR is associated with increased frailty risk and has a certain predictive value in elderly hospitalized patients with CHD,11 our study is consistent with previous finding. In this study, we expounded on that finding. The relationship between all-cause mortality in ischemic stroke patients with AF and the HRR values was non-linear,The low level HRR values increase the risk of death in ischemic stroke patients with AF.
Our work has a number of strengths. First, our study was the first undertaken to research the mortality risk factors of ischemic stroke patients with AF. This study focused on the compound variables of the HRR and was the first to investigate the relationship between the HRR and mortality in ischemic stroke patients with AF. Second, the study used real-world data for a large and diverse population study design. Third, we used a two-part Cox proportional risk regression model to perform a threshold effect analysis on the relationship between the HRR and all-cause mortality and performed a subgroup analysis of the association between the HRR and all-cause mortality. Fourth, we analyzed the exposure variable HRR as not only a continuous variable but also a categorical variable and calculated the hazard ratio using binary logistic regression models. Such a method can minimize the incidence of a contingency in the statistical analysis and enhance the reliability of the final results. Our study also had a few limitations. First, this was a single-center retrospective observational study so it was difficult to avoid selection bias. Second, although we adjusted for certain factors, our results may have been influenced by other unknown factors. Third, no long-term follow-up events were provided from the MIMIC-IV database.
Conclusions
The relationship between all-cause mortality and the HRR values was non-linear in ischemic stroke patients with AF. All-cause mortality and the HRR values were negatively correlated when the HRR value was ≤ 9.74.
Institutional Review Board Statement
The MIMIC-IV database was built by the Massachusetts Institute of Technology and was approved to waive the documentation of informed consent by the Institutional Review Board of Beth Israel Deaconess Medical Center. For the access of the database, Zuoan Qin completed the Collaborative Institutional Training Initiative course named “Data or Specimens Only Research” and obtained the relevant certification (certification number:36208651).
Informed Consent Statement
There was no requirement of individual informed consent to extract data from the MIMIC-IV database because the MIMIC-IV database information was publicly available and all patient data were deidentified.
Funding
This article is funded by the Technology Research and Development Funding Project of Hunan Provincial Innovation Platform and Talent Program Clinical Medical Research Center (No.2021SK4042).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the Global Burden of Disease Study 2017. Neuroepidemiology. 2020;54(2):171–179. doi:10.1159/000506396
2. Feigin VL, Krishnamurthi RV, Parmar P, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: the GBD 2013 study. Neuroepidemiology. 2015;45(3):161–176. doi:10.1159/000441085
3. Freedman B, Hindricks G, Banerjee A, et al. World heart federation roadmap on atrial fibrillation – a 2020 update. Glob Heart. 2021;16(1):41. doi:10.5334/gh.1023
4. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham study. Stroke. 1991;22:983–988. doi:10.1161/01.STR.22.8.983
5. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics—2017 update a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi:10.1161/CIR.0000000000000485
6. Kabra R, Girotra S, Sarrazin MV. Clinical outcomes of mortality, readmissions, and ischemic stroke among medicare patients undergoing left atrial appendage closure via implanted device. JAMA Netw Open. 2019;2(10):e1914268. doi:10.1001/jamanetworkopen.2019.14268
7. Yılmaz A, Yılmaz H, Tekin SB, Bilici M. The prognostic significance of hemoglobin-to-red cell distribution width ratio in muscle-invasive bladder cancer. Biomark Med. 2020;14(9):727–738. doi:10.2217/bmm-2020-0045
8. Yılmaz H, Yılmaz A, Demirağ G. Prognostic significance of hemoglobin-to-red cell distribution width ratio in patients with metastatic renal cancer. Future Oncol. 2021;17(29):3853–3864. doi:10.2217/fon-2021-0040
9. Wu F, Yang S, Tang X, et al. Prognostic value of baseline hemoglobin-to-red blood cell distribution width ratio in small cell lung cancer: a retrospective analysis. Thorac Cancer. 2020;11(4):888–897. doi:10.1111/1759-7714.13330
10. Tham T, Olson C, Wotman M, et al. Evaluation of the prognostic utility of the hemoglobin-to-red cell distribution width ratio in head and neck cancer. Eur Arch Otorhinolaryngol. 2018;275(11):2869–2878. doi:10.1007/s00405-018-5144-8
11. Qu J, Zhou T, Xue M, et al. Correlation analysis of hemoglobin-to-red blood cell distribution width ratio and frailty in elderly patients with coronary heart disease. Front Cardiovasc Med. 2021;8:728800. doi:10.3389/fcvm.2021.728800
12. Goldberger AL, Amaral LA, Glass L, et al. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation. 2000;101(23):E215–E220. doi:10.1161/01.CIR.101.23.e215
13. Johnson AE, Stone DJ, Celi LA, Pollard TJ. The MIMIC code repository: enabling reproducibility in critical care research. J Am Med Inform Assoc. 2018;25(1):32–39. doi:10.1093/jamia/ocx084
14. Murray CJL, Lopez AD. Measuring the global burden of disease. N Engl J Med. 2013;369(5):448–457. doi:10.1056/NEJMra1201534
15. Shiber JR, Fontane E, Adewale A. Stroke registry: hemorrhagic vs ischemic strokes. Am J Emerg Med. 2010;28(3):331–333. doi:10.1016/j.ajem.2008.10.026
16. Hsieh C-Y, Wu DP, Sung S-F. Trends in vascular risk factors, stroke performance measures, and outcomes in patients with first-ever ischemic stroke in Taiwan between 2000 and 2012. J Neurol Sci. 2017;378:80–84. doi:10.1016/j.jns.2017.05.002
17. Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990–2010. Lancet Glob Health. 2013;1(5):e259–e281. doi:10.1016/S2214-109X(13)70089-5
18. Katan M, Luft A. Global burden of stroke. Semin Neurol. 2018;38(2):208–211. doi:10.1055/s-0038-1649503
19. Minnerup J, Wersching H, Unrath M, Berger K. Explaining the Decrease of In-Hospital Mortality from Ischemic Stroke. PLoS One. 2015;10:e0131473. doi:10.1371/journal.pone.0131473
20. Ramirez L, Kim-Tenser MA, Sanossian N, et al. Trends in acute ischemic stroke hospitalizations in the United States. J Am Heart Assoc. 2016;5(5):e003233. doi:10.1161/JAHA.116.003233
21. Wańkowicz P, Nowacki P, Gołąb-Janowska M. Atrial fibrillation risk factors in patients with ischemic stroke. Arch Med Sci. 2019;17(1):19–24. doi:10.5114/aoms.2019.84212
22. Friberg L, Hammar N, Pettersson H, Rosenqvist M. Increased mortality in paroxysmal atrial fibrillation: report from the Stockholm cohort-study of atrial fibrillation (SCAF). Eur Heart J. 2007;28(19):2346–2353. doi:10.1093/eurheartj/ehm308
23. Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–2236. doi:10.1161/STR.0000000000000024
24. Jiang C, Lan D-H, Xin D, et al. Prevalence of modifiable risk factors and relation to stroke and death in patients with atrial fibrillation: a report from the China atrial fibrillation registry study. J Cardiovasc Electrophysiol. 2019;30(12):2759–2766. doi:10.1111/jce.14231
25. Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285(22):2864–2870. doi:10.1001/jama.285.22.2864
26. Kim IS, Lee BK, Yang PS, Joung B, Kim JY. Sex-based approach for the clinical impact of the increased hemoglobin on incident AF in the general population. Korean Circ J. 2020;50:1095–1110. doi:10.4070/kcj.2020.0412
27. Park J. Increased Hb levels are associated with the incidence of atrial fibrillation: but is it related to the occurrence of stroke? Korean Circ J. 2020;50(12):1111–1112. doi:10.4070/kcj.2020.0495
28. Lim WH, Choi EK, Han KD, et al. Impact of hemoglobin levels and their dynamic changes on the risk of atrial fibrillation: a nationwide population-based study. Sci Rep. 2020;10:6762. doi:10.1038/s41598-020-63878-9
29. Taylor kimberly W, Lima FO, O’Connor S, Furie KL. Sex differences and hemoglobin levels in relation to stroke outcomes. Neurology. 2013;80(8):719–724. doi:10.1212/WNL.0b013e31828250ff
30. Sacco S, Marini C, Olivieri L, Pistoia F, Carolei A. Contribution of hematocrit to early mortality after ischemic stroke. Eur Neurol. 2007;58(4):233–238. doi:10.1159/000107946
31. Duchnowski P, Hryniewiecki T, Kusmierczyk M, Szymanski P. Red cell distribution width is a prognostic marker of perioperative stroke in patients undergoing cardiac valve surgery. Interact Cardiovasc Thorac Surg. 2017;25(6):925–929. doi:10.1093/icvts/ivx216
32. Duchnowski P, Szymański P, Kuśmierczyk M, Hryniewiecki T. Usefulness of FRAIL scale in heart valve diseases. Clin Interv Aging. 2020;15:1071–1075. doi:10.2147/CIA.S239054
33. Mohindra R, Mishra U, Mathew R, Negi NS. Red cell distribution width (RDW) index as a predictor of severity of acute ischemic stroke: a correlation study. Adv J Emerg Med. 2020;4(2):e24. doi:10.22114/ajem.v0i0.257
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
