Back to Journals » OncoTargets and Therapy » Volume 9
Relationship between serum carcinoembryonic antigen level and epidermal growth factor receptor mutations with the influence on the prognosis of non-small-cell lung cancer patients
Authors Cai Z
Received 10 December 2015
Accepted for publication 25 February 2016
Published 27 June 2016 Volume 2016:9 Pages 3873—3878
DOI https://doi.org/10.2147/OTT.S102199
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr William C. Cho
Zuxun Cai
Department of Thoracic Surgery, Henan Provincial Chest Hospital, Zhengzhou City, People’s Republic of China
Objective: To investigate the relationship between serum carcinoembryonic antigen (CEA) level and epidermal growth factor receptor (EGFR) gene mutations in non-small-cell lung cancer (NSCLC) patients and to analyze the influence of CEA level on postoperative survival time in lung cancer patients.
Methods: A total of 296 patients who were treated in Thoracic Surgery Department of Henan Provincial Chest Hospital from September 2011 to September 2013 were recruited. The level of tumor markers, such as CEA, was determined before the surgery, and EGFR gene mutations were detected after surgery. Thereby, the relationship between tumor makers, including CEA, and EGFR mutation and its influence on prognosis could be investigated.
Results: Among 296 patients, the positive rate of EGFR gene mutation was 37.84% (112/296); the mutation occurred more frequently in nonsmokers, adenocarcinoma patients, women, and patients aged <60 years (P<0.05). Both tumor markers and chemosensitivity indicators were related to the profile of EGFR mutations. Elevated squamous cell carcinoma and Cyfra21-1 as well as positively expressed ERCC1 were more common in patients with wild-type EGFR (P<0.05), whereas increased CEA level was observed more frequently in patients with EGFR gene mutation (P=0.012). The positive rate of EGFR gene mutations was higher as the serum CEA level increased, that is, the positive rate in patients with serum CEA level <5, 5–20, and >20 µg/L was 39.81%, 45.32%, and 65.47%, respectively (P=0.004). Logistic regression analysis showed that CEA level was an independent factor in predicting EGFR gene mutations, and serum CEA level was also an independent factor in affecting the prognosis of NSCLC patients, as the overall 2-year survival rate was 73.86% in elevated CEA group and 86.43% in normal group (P<0.01).
Conclusion: The prognosis of NSCLC patients receiving resection can be predicted according to serum CEA level, which is associated with EGFR mutations in NSCLC patients and provides a preliminarily guidance for EGFR mutations.
Keywords: serum carcinoembryonic antigen, epidermal growth factor receptor, non-small cell lung cancer, resection, prognosis
Introduction
Lung cancer is one of the malignant tumors causing human deaths, of which non-small-cell lung cancer (NSCLC) accounts for 85%. Although chemoradiotherapy techniques and traditional operation methods have greatly improved, the survival rate of NSCLC patients is still <20%.1,2 At present, in the clinical diagnosis and treatment of NSCLC, molecular targeting therapy using epidermal growth factor receptor (EGFR) as the target is prominent. EGFR is closely associated with neovascularization, tumor invasion, and metastasis, can be mutated and/or overexpressed, and guides the tumor growth through signal transduction.3 EGFR gene mutation is of great significance in formulating treatment measures of lung cancer and predicting the prognosis. Serum carcinoembryonic antigen (CEA) is a vital indicator in predicting the efficacy of targeted therapy and chemotherapy as well as the postoperative recurrence and metastasis. However, it is still unclear whether CEA can predict EGFR gene mutation and its influence on NSCLC patients undergoing surgery. The current study was designed to investigate the relationship between CEA level and EGFR gene mutations in lung cancer patients and to analyze the influence of CEA levels on postoperative survival time of lung cancer patients.
Materials and methods
Data collection
The study was approved by the institutional research ethics committee of Henan Provincial Chest Hospital. A total of 296 lung cancer patients (mean age: [59.1±5.4] [range: 29–90] years) who received standard radical resection in Henan Provincial Chest Hospital between September 2011 and September 2013 were recruited. Among them, the proportion of the patients aged <60 and ≥60 years was 53.04% (157/296) and 46.96% (139/296), respectively. Inclusion criteria were 1) having a clear preoperative diagnosis of lung cancer; 2) exclusion of metastasis in brain, liver, adrenal gland, and contralateral lung by preoperative chest computed tomography (CT), brain CT or magnetic resonance imaging, and abdomen B ultrasound, and exclusion of distant metastasis by whole-body electroconvulsive therapy (some underwent positron emission tomography–CT); 3) not receiving any preoperative anticancer therapy, such as radiotherapy and chemotherapy; 4) undergoing complete resection; 5) having complete case and follow-up data, except for patients who died within 30 days after operation; 6) obtaining written informed consent from the subjects or their families. All enrolled patients had been confirmed by pathological examination to have not undergone other adjuvant therapies before surgery and to have undergone the conventional detection test for tumor marker at Day 7 before surgery.
Treatment methods
All the patients adopted the surgery-based comprehensive treatment, with 14 receiving total pneumonectomy, 267 pulmonary lobectomy, and 15 lung segment/wedge resection. The patients with Stage IB or higher lung cancer were given postoperative adjuvant therapy mainly using cisplatin/carboplatin combined with paclitaxel/vinorelbine/gemcitabine. For the patients exhibiting postoperative recurrence, multisite metastasis, and distant metastasis of mediastinal lymph nodes, postoperative radiotherapy was performed (a total of 127 cases), whereas for those with positive EGFR mutation, postoperative EGFR-tyrosine kinase inhibitor (TKI) therapy was given auxiliarily, and the remaining received the adjuvant therapy after recurrence and metastasis.
Postoperative follow-up
Follow-up was started from the day of surgery and ended on the last follow-up day or when the patient died. The follow-up methods were performed mainly by outpatient service, reexamination, letters, and telephone. The overall survival (OS) rate was calculated from the day of surgery to the last follow-up day or to patients’ death (calculated in months). The disease-free survival (DFS) was the period from the day of surgery to the day when recurrence and metastasis were detected for the first time (calculated in months). The last follow-up visit occurred in January 2016.
Statistical methods
SPSS 19.0 statistical analysis software package was adopted for data analysis. Paired t-test was applied for comparison of continuous variables among groups; χ2-test was used for comparison of classified variables; Kaplan–Meier method was adopted to calculate the survival rate; log-rank test was employed for single-factor analysis; Cox proportional hazard model was used for multiple-factor analysis; logistic regression analysis was employed to analyze the relationship between EGFR gene mutation and various factors. Values of P<0.05 was considered statistically significant.
Results
Influences of EGFR mutations on EGFR-TKI treatment
Among 296 patients, 27 received EGFR-TKI treatment, including 25 with EGFR mutations showing squamous carcinoma or adenocarcinoma and two with wild-type EGFR exhibiting adenocarcinoma on postoperative pathology. By comparing EGFR-TKI reactions at 19 vs 21 exons, no statistical significance was seen in DFS and OS (P>0.05).
Relationships between clinicopathological factors and EGFR mutations
Based on the results of the postoperative detection of EGFR gene mutation, a positive result was found in 112 patients (37.84%), including five cases of exon 18 and 20 mutations, 58 cases of exon 19 deletion mutation, and 49 cases of exon 21 point mutations. Additionally, three cases had point mutations at two sites, accounting for 2.68% (3/112) of all mutation cases. A total of 36 males and 76 females were found to have mutations; 95 cases (84.82%) had adenocarcinoma, five cases (6.25%) had large-cell lung carcinoma, and eight cases (7.14%) had squamous carcinoma; 68 cases (60.71%) had never smoked and 44 cases (39.29%) were smokers or had smoked; 166 cases (56.08%) had Stage I disease, 39 cases (13.18%) had Stage II disease, and 91 cases (30.74%) had Stage III disease. According to the results of the comparisons between wild-type and EGFR mutation groups, patients with adenocarcinoma, females, and nonsmokers were prone to EGFR mutations (Table 1).
  | Table 1 Mutant epidermal growth factor receptor (EGFR) or wild-type EGFR with clinicopathologic features in patients with nonsmall cell lung cancer |
Relationship between tumor markers with chemosensitivity indicators and EGFR mutations
Within 1 week before surgery, all these patients underwent conventional detection of tumor markers, including CEA, cytokeratin (Cyfra21-1), neuron-specific enolase, squamous cell carcinoma (SCC) antigen, and tissue polypeptide-specific antigen. The results indicated that CEA levels in patients with positive EGFR mutations increased more frequently, whereas changes of SCC and Cyfra21-1 levels were more common in patients with negative EGFR mutations (P<0.05). The stratification analysis indicated no statistical difference in the potential relationship between tumor markers and different point mutations (exons 19 and 20) (P>0.05). From the immunohistochemical results, the negative expression of ERCC1 was more common in patients with EGFR mutations (Table 2). Logistic regression analysis was performed for the clinical factors, probably affecting the EGFR mutation prediction, so as to explore deeply the relationship between EGFR mutation and CEA level, and the results demonstrated that CEA level was an independent factor in predicting EGFR gene mutation (Table 3). The positive rate of EGFR mutation in patients with serum CEA level <5, 5–20, and >20 μg/L was 39.81%, 45.32%, and 65.47%, respectively (P=0.004). Thus, we found that the rate of EGFR gene mutations increased as the serum CEA level increased.
Influence of CEA level on the survival time of NSCLC patients
A total of 90 patients showed an increase in CEA level. Both OS and DFS in the normal CEA level group were higher than those in the increased CEA level group, with 2-year OS and DFS of 86.43% and 79.5% vs 73.86% and 50.46%, respectively (P<0.01), as shown in Figure 1. As shown by Cox proportional hazard model analysis, CEA level was an independent factor affecting the postoperative survival time for NSCLC patients (odds ratio =1.747; P=0.031).
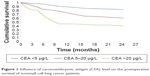  | Figure 1 Influence of carcinoembryonic antigen (CEA) level on the postoperative survival of nonsmall cell lung cancer patients. |
Discussion
EGFR is one of the critical targets in the treatment of NSCLC, whereas EGFR gene mutations occur only in the tumor tissues, especially in NSCLC, and these mutations do not exist in normal tissue cells.4 Based on the present study, in nonsmoking, adenocarcinoma, and female patients, EGFR mutation rate was relatively higher and had a higher sensitivity to EGFR-TKI therapy. The population who benefit from the EGFR-TKI treatment include adenocarcinoma, nonsmoking, and female patients, which might be associated with higher EGFR gene mutation rate. In individualized treatment of NSCLC, detection of EGFR mutation is of great significance. The somatic mutation of EGFR is mainly focused on exons 19 and 21. At present, only these two mutations are considered to be able to predict the efficacy of EGFR inhibitor.5–7 The efficacy prediction is difficult in the clinical treatment with EGFR-TKI. However, in clinical practice, predicting EGFR gene mutation state could benefit the patients undergoing EGFR-TKI treatment.
In this study, positive expression of ERCC1 reflected more wild-type EGFR gene, which was more common in squamous carcinoma, male, and smoking patients. These are the “nondominant crowd” who were treated with EGFR-TKI. This may be the reason why positive expression of ERCC1 protein was more common in patients with negative EGFR mutations. As shown in the present study, according to preoperative detection of tumor markers in wild-type group, increased SCC and Cyfra21-1 levels were more common, which may be closely associated with squamous carcinoma. The increase of serum CEA predicted an elevation of EGFR mutation ratio, and the reason might be that activation of downstream molecules of EGFR mutant promotes antiapoptosis, and the expression level of CEA is enhanced by EGFR. Elevated CEA level can also predict the survival time and response rate of NSCLC patients undergoing EGFR-TKI treatment. In patients with increased CEA level, there is a higher EGFR-TKI response rate and maybe a longer survival time. In particular, the patients with squamous carcinoma and unknown EGFR mutation status are more likely to benefit from it.8
CEA is a better marker for predicting the effect of lung cancer treatment, monitoring the patients’ condition of disease, and evaluating the prognosis. The results of the present study revealed that CEA level was an independent factor and was able to predict the EGFR gene mutation. The incidence of EGFR gene mutations gradually increased as the serum CEA level increased. The positive rate of mutation in patients with serum CEA level <5, 5–20, and >20 μg/L was 39.81%, 45.32%, and 65.47%, respectively. Hence, the EGFR mutation profile can be preliminarily forecast using preoperative CEA level. Studies9,10 have reported that staging of lung cancer was closely associated with CEA level, which was an independent factor in the prognosis of lung cancer patients. An increase of CEA level in Stage I lung cancer patients (especially for female patients) resulted in a shorter survival time. Therefore, to enhance the survival rate of such patients, adjuvant therapies could be provided in a timely manner. The results of this study indicated that the survival time was shorter in the increased CEA level group, with 2-year OS of only 73.22%, whereas it was 86.43% in the normal group, showing a statistically significant difference (P<0.01). By further adopting Cox risk model, we found that CEA level was an independent prognostic influence factor for patients with resection of lung cancer.
Conclusion
The present study preliminarily reveals the relationship between EGFR mutation and CEA level, which is similar to that reported previously.11,12 For NSCLC patients, the preoperative detection of CEA level can be utilized to guide the adjuvant therapy of EGFR-TKI so that the total efficacy rate of EGFR-TKI might be enhanced. The preoperative CEA level could also predict the survival time of NSCLC patients. If the preoperative detection suggests an increase in the level of CEA, postoperative adjuvant therapy should be adopted selectively to maximize the total survival rate of NSCLC patients.
Acknowledgment
The author would like to thank the key program in science and technology of Henan Province, 2009 (No 092102310284) for the financial support.
Disclosure
The author reports no conflicts of interest in this work.
References
Zheng J, Xie GY, Li J, et al. Clinical significance of EGFR mutations in non-small cell lung cancer. Chin J Clin Oncol. 2014;41(14):904–907. | ||
Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008. Int J Cancer. 2010;127(12):2893–2917. | ||
Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350(21):2129–2139. | ||
Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304(5676):1497–1500. | ||
Zhao LD, Li JL, Wang Y, et al. [Factors affecting the sensitivity of EGFR-TKI treatment in advanced non-small cell lung cancer]. Zhonghua Zhong Liu Za Zhi. 2011;33(3):217–221. Chinese. | ||
Rosell R, Morán T, Carcereny E, et al. Non-small-cell lung cancer harbouring mutations in the EGFR kinase domain. Clin Transl Oncol. 2010;12(2):75–80. | ||
Won YW, Han JY, Lee GK, et al. Comparison of clinical outcome of patients with non-small-cell lung cancer harbouring epidermal growth factor receptor exon 19 or exon 21 mutations. J Clin Pathol. 2011;64(11):947–952. | ||
Shoji F, Yoshino L, Yano T, et al. Serum carcinoembryonic antigen level is associated with epidermal growth factor receptor mutations in recurrent lung adenocarcinomas. Cancer. 2007;110(12):2793–2798. | ||
Tomita M, Shimizu T, Hara M. Serum carcinoembryonic antigen level in non-small-cell lung cancer patients with preoperative normal serum level. Cardiovasc Surg. 2009;57(6):303–306. | ||
Hsu WH, Huang CS, Hsu HS. Preoperative serum carcinoembryonic antigen level is a prognostic factor in women with early non-small-cell lung cancer. Ann Thorac Surg. 2007;83(2):419–424. | ||
Zhong-Ming Y, Xian-Ping D, Lei P, et al. Analysis of CEA expression and EGFR mutation status in non-small cell lung cancers. Asian Pac J Cancer Prev. 2014;15(8):3451–3455. | ||
Jin-Bing P, Yu-Hong H, Guo-Jun Z. Correlation between EGFR mutations and serum tumor markers in lung adenocarcinoma patients. Asian Pac J Cancer Prev. 2013;14(2):695–700. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


