Back to Journals » Journal of Pain Research » Volume 9
Relationship between self-reported pain sensitivity and pain after total knee arthroplasty: a prospective study of 71 patients 8 weeks after a standardized fast-track
Authors Valeberg BT, Hovik L, Gjeilo KH
Received 20 May 2016
Accepted for publication 22 June 2016
Published 8 September 2016 Volume 2016:9 Pages 625—629
DOI https://doi.org/10.2147/JPR.S113258
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Berit T Valeberg,1 Lise H Høvik,2 Kari H Gjeilo3–6
1Faculty of Nursing, Oslo and Akershus University College of Applied Sciences, Oslo, 2Clinic of Anaesthesia and Intensive Care Medicine, St. Olavs Hospital, Trondheim University Hospital, 3Department of Cardiothoracic Surgery, 4Department of Cardiology, 5National Competence Centre for Complex Symptom Disorders, St. Olavs Hospital, Trondheim University Hospital, 6Department of Circulation and Medical Imaging, Faculty of Medicine, Norwegian University of Science and Technology, Trondheim, Norway
Background and purpose: This was a prospective cohort study assessing data from 71 adult patients undergoing total knee arthroplasty (TKA) following a standardized fast-track program between January and July 2013. The objective was to examine the relationship between self-rated pain sensitivity, as measured by the Pain Sensitivity Questionnaire (PSQ), and postoperative pain after TKA.
Methods: The baseline questionnaires, PSQ and Brief Pain Inventory, were given to the patients for self-administration at the presurgical evaluation (1–2 weeks prior to surgery). The follow-up questionnaire, Brief Pain Inventory, was administered at the first follow-up, 8 weeks after surgery.
Results: A statistically significant association was found between average preoperative pain and average pain 8 weeks after surgery (P=0.001). The PSQ-minor was statistically significantly associated with average pain only for patients younger than 70 years (P=0.03).
Interpretation: This is the first study to examine the relationship between pain sensitivity measured by PSQ and postoperative pain in patients after TKA. We found that a lower score on the PSQ-minor was statistically significantly associated with patients’ pain 8 weeks after TKA surgery, but only for younger patients. Further research is needed to explore whether the PSQ could be a useful screening tool for patients’ pain sensitivity in clinical settings.
Keywords: postoperative pain, pain sensitivity, pain sensitivity questionnaire, total knee arthroplasty
Introduction
Postoperative pain is an ongoing challenge, despite the use of multimodal approaches for pain management.1 An analgesic gap is described in the transmission between parenteral, regional, and oral administration of analgesics in the immediate postoperative period while patients are still hospitalized.2 Suboptimal pain control in patients at home points to another “analgesic gap”, the transmission between hospital discharge and pain management at home.3,4 Early discharge from hospital requires patients’ adherence to pain medication regimen in the subacute postoperative period.
Total knee arthroplasty (TKA) is a surgical procedure with a high prevalence of postoperative pain.1 This is paradoxical because pain is also the most important reason why patients seek surgery for TKA.5 TKA improves function and reduces pain in the majority of patients.6 However, levels of dissatisfaction are estimated to be as high as 20%.7 The main reason for dissatisfaction appears to be pain.8 The patient’s ability to carry out the rehabilitation program is crucial for a good result.3,9,10
From a systematic review of postoperative pain, it was found that both younger age and preoperative pain together with preoperative anxiety and surgical procedure were the predictors of postoperative pain.11 Rakel et al12 found that younger patients are at a greater risk of pain in rest, but not of higher movement pain after TKA.
The ability to predict which patients are at increased risk of postoperative pain and who require more analgesics would allow more individually tailored pain management methods and reduce severe postoperative pain at home.13,14
Sensitivity to pain may be one of the factors contributing to differences in postoperative pain perception. Pain sensitivity measured by quantitative sensory testing (QST), using different physical stimuli, such as thermal, pressure, or electrical pain stimuli, has been shown to predict postoperative pain.14–18 The most traditional measures for quantifying pain perception are pain thresholds, pain intensity, pain tolerance, and magnitude estimation of suprathreshold pain.18 A systematic review of 14 studies investigating the predictive strength of different QST on postoperative pain found that the predictive strength of QST is much higher than for single-factor analyses of age, sex, and psychological factors. The review demonstrated that QST assessments may predict up to 54% of the variance in postoperative pain.19 However, QST is time consuming and not always feasible in a clinical setting. It requires extra staff, equipment, and associated costs. The procedures may also be potentially aversive for patients.20
The Pain Sensitivity Questionnaire (PSQ) was developed to overcome the obstacles of assessing pain sensitivity by experimental stimulation.20 The questionnaire is based on pain intensity ratings of imagined painful situations occurring in daily life. The validation of the original instrument showed a statistically significant correlation between the PSQ and experimental pain intensity in a healthy population.20 The same correlation was found when validating the Norwegian version of the PSQ in healthy volunteers. In a study of chronic pain patients, significant correlations between the PSQ and experimental pain intensity and threshold were found.21 In a recent study of chronic back pain patients, pain sensitivity measured by the PSQ was predictive of pain ratings when injected with subcutaneous lidocaine.22 One study has evaluated the influence of preoperative pain sensitivity, as measured by the PSQ, on the surgical outcome 12 months after lumbar spine surgery. They found that patients with high pain sensitivity had less improvement in back pain, leg pain, and disability than patients with low pain sensitivity.23 No studies have explored the relationship between preoperative pain sensitivity measured by the PSQ and postoperative pain. Therefore, the purpose of this study was to examine the relationship between pain sensitivity measured by the PSQ and postoperative pain after TKA.
Patients and methods
This prospective cohort study recruited patients from the Department of Orthopedic Surgery, St. Olav’s Hospital, Trondheim University Hospital, Norway, between January and July 2013. Criteria for exclusion were inability to write or read Norwegian, cognitive impairments (inability to provide informed consent), or refusal to participate. All patients followed a standardized fast-track treatment and were mobilized on the day of surgery. The recovery program was based on individual and group physiotherapy when hospitalized, and the patients were instructed to follow the recommended training program. For pain treatment at home, the patients were advised to take paracetamol regularly and were given a prescription of tramadol hydrochloride and nonsteroidal anti-inflammatory drugs if the medical condition allowed it.
The Regional Committee for Medical and Health Research Ethics in Central Norway approved the study (no. 2012/1698/REK midt). Written informed consent was obtained from each patient at inclusion.
Instruments and scoring procedures
Demographic and medical information included age, sex, cohabitation, and American Society of Anesthesiologists (ASA) group criteria, collected from an institutional database.24 ASA is a physical status classification system based on the risk of anesthesia-related death.25
Pain
The Brief Pain Inventory (BPI) is a short, self-report generic pain questionnaire designed to assess the severity and impact of pain.26 Four questions relate to pain intensity (“worst,” “least,” and “average” pain [during the past 24 hours], and pain “now”) and seven questions relate to pain interference with function. The pain intensity items are presented as numerical rating scales, from 0 (no pain) to 10 (worst pain imaginable). Average pain intensity was defined as mild (0–3), moderate (4–6), and severe (7–10).27
The seven items measuring pain interference with patient function are presented as numerical rating scales from 0 (does not interfere) to 10 (interferes completely). The interference items ask how pain interferes with general activity, mood, walking, work, relations with others, sleep, and enjoyment of life. The Norwegian version of the BPI has satisfactory psychometric properties.28,29
Pain Sensitivity Questionnaire
The PSQ is a self-administered assessment tool based on pain intensity ratings of imagined painful situations in daily life. It consists of 17 items, each describing different daily life situations with scorings ranging from 0 (not painful) to 10 (worst pain imaginable). Fourteen items relate to situations that are perceived to be painful by most healthy individuals. Three items describe situations that are not normally regarded as painful by most people, and these serve as sensory references for the participants and are not used in the final scoring. The painful items represent different types of pain (hot, cold, sharp, and blunt) and different body sites (head and upper and lower extremities). The PSQ is measured as a mean of all items – total PSQ – and divided in two subscales consisting of seven items each, PSQ-minor (items representing less painful situations) and PSQ-moderate (items representing moderately painful situations).20
Procedures
The baseline questionnaires (PSQ and BPI) were self-administered by the patients at the presurgical evaluation (1–2 weeks prior to surgery). Because of the fast-track structure, this day consists of presurgical information and optimization by the surgeon, anesthesiologist, nurse, and physiotherapist. All patients for joint replacement (hip and knee) undergo patient school the same day. The follow-up questionnaire (BPI) was administered at the first follow-up, 8 weeks after surgery.
Statistical analyses were performed with PASW® statistics software for Windows (version 21; IBM Corporation, Armonk, NY, USA). Descriptive statistics and frequency distributions were generated for patients’ demographic and clinical characteristics. Linear regression analysis was performed to evaluate the effect of age, preoperative pain, and PSQ on postoperative pain 8 weeks after surgery. We used the BPI item of average pain as the independent variable because it refers to the variations in pain during the last 24 hours. The PSQ-minor was used as a measure of pain sensitivity as it has shown to have the best predictive value of pain in prior studies.20,22 There was no linear correlation between age and postoperative pain 8 weeks after surgery. However, our data revealed a statistically significant interaction between age and pain. Therefore, all analyses were stratified by age, and this variable was dichotomized into older than 70 years (n=21) and younger than 70 years (n=45). A P-value <0.05 was considered statistically significant.
Results
A total of 82 of the 89 patients undergoing TKA in the study period fulfilled the inclusion criteria. Three patients refused to participate and eight patients were not included because of lack of staffing resources. Thus, 71 of the 82 patients were included (87%). At the 8-week follow-up, 65 patients completed the questionnaires (92%).
Patient age ranged between 40 years and 86 years, and there were almost equal numbers of males and females. Most patients were in the ASA groups 1 and 2 (Table 1). A total of 80% of the patients graded their average preoperative pain to be moderate or severe (pain ≥4). Eight weeks after surgery, patients had significantly reduced all their pain and pain interference scores (Table 2).
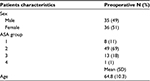  | Table 1 Characteristics of the patients (N=71) Abbreviation: ASA, American Society of Anesthesiologists. |
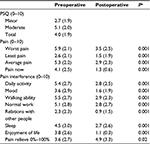  | Table 2 Preoperative (N=71) and postoperative (N=65) clinical characteristics of the patients Note: aPaired sample t-test. Abbreviation: PSQ, Pain Sensitivity Questionnaire. |
There was an interaction between patient age and pain sensitivity; therefore, all analyses were stratified by age. Furthermore, our data revealed a statistically significant association between preoperative average pain and average pain, 8 weeks following surgery (P=0.001). PSQ-minor was a statistically significant predictor of average pain only for patients younger than 70 years (P=0.03; Table 3).
  | Table 3 Linear regression analysis with average pain intensity 8 weeks after surgery as independent variable (N=65) |
Discussion
This is the first study to examine whether pain sensitivity measured by PSQ is associated with postoperative pain in patients after TKA. Only one prior study was found to measure pain sensitivity by means of the PSQ preoperatively to investigate the relationship to surgical outcome. In contrast to our study, this study found that patients with higher pain sensitivity before surgery had less improvement in back pain, leg pain, and disability 12 months after spinal stenosis surgery compared with patients who had lower pain sensitivity.23 In our study, we found that pain sensitivity was associated with postoperative pain only for patients younger than 70 years and that patients who scored lower on pain sensitivity had higher pain intensity postoperatively. We can only speculate, however, one reason for these somewhat contradictory results could be that the patients undergoing spine surgery reported higher preoperative pain sensitivity than TKA patients. In the study evaluating the outcome after spine surgery, patients were divided in a low PSQ group (PSQ score <6.5) and a high PSQ group (PSQ score ≥6.5).23 The scores of PSQ-minor were higher in both these groups compared to our study. Furthermore, due to less experience with pain, younger patients may underestimate their pain in less painful situations and may be less prepared when experiencing more painful situations in “real” life.
We found that lower scores on the PSQ-minor were a statistically significant predictor of patients’ pain 8 weeks after TKA surgery, but only for patients younger than 70 years. In the validation study of the PSQ, PSQ scores in chronic pain patients were not significantly related to age or sex.21 In general, it seems that younger patients exhibit more pain after uncomplicated TKA,30 and whether younger patients in general have different pain sensitivity measured by PSQ compared with older patients must be further explored. Given a limited sample size, we were not able to explore more in depth the relationship between age and pain sensitivity. Further analyses are warranted.
Prior research has shown that risk factors for poorer outcomes after TKA surgery include female sex, younger age, higher than normal depressive or anxiety state, and pain catastrophizing.30 Further research is needed to explore whether PSQ may be a useful tool in screening patients’ pain sensitivity in clinical settings. Screening instruments may help identify vulnerable patients before surgery, prompting special considerations concerning management of postoperative pain for these patients. It may also be important to prevent the transition from acute to persistent postoperative pain. Knowledge of vulnerable patients may also be useful in the education of patients prior to surgery, so they can be given a realistic expectation of their possible satisfaction following TKA. This is in accordance with the recommendations given in a recent systematic review.31
Both pain and pain interference with function decreased significantly after TKA, 8 weeks postoperatively. The average pain scores (a score of below 4) showed an overall satisfactory outcome for the patients. The possibility to detect whether preoperative PSQ scores could predict pain intensity scores at 8 weeks might be better if the patients’ pain both in activity and at rest were assessed in detail. The patients in our sample only reported an overall average mild pain. We do not know whether the patients were active or inactive most of the time when they reported their average pain. In a prior study, TKA patients reported higher pain intensity in activity than at rest, and cutaneous pain sensitivity predicted only postoperative pain in activity and not pain at rest.12
The small sample size limited the opportunity to examine other factors, such as sex and psychological factors, which may have influenced the outcome of surgery. The small sample size also limits the generalization of the findings. Despite these limitations, this study contributes to the understanding of self-reported pain sensitivity and pain after TKA and suggests that the PSQ may be useful. However, further research is needed to examine whether the PSQ could be a suitable screening tool for detecting patients at risk for poorer outcomes after surgery.
Acknowledgment
Milada Cvancarova Småstuen contributed to the statistics.
Disclosure
The authors report no conflicts of interest in this work.
References
Aasvang EK, Luna IE, Kehlet H. Challenges in postdischarge function and recovery: the case of fast-track hip and knee arthroplasty. Br J Anaesth. 2015;115(6):861–866. | ||
Ng A, Hall F, Atkinson A, Leong Kong K, Hahn A. Bridging the analgesic gap. Acute Pain. 2000;3(4):194–199. | ||
Strassels SA, McNicol E, Wagner AK, Rogers WH, Gouveia WA, Carr DB. Persistent postoperative pain, health-related quality of life, and functioning 1 month after hospital discharge. Acute Pain. 2004;6(3–4):95–104. | ||
Andersen L, Gaarn-Larsen L, Kristensen BB, Husted H, Otte KS, Kehlet H. Subacute pain and function after fast-track hip and knee arthroplasty. Anaesthesia. 2009;64(5):508–513. | ||
Santaguida PLP, Hawker GA, Hudak PL, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51(6):428–436. | ||
Shan L, Shan B, Suzuki A, Nouh F, Saxena A. Intermediate and long-term quality of life after total knee replacement. J Bone Joint Surg Am. 2015;97(2):156–168. | ||
Bourne R, Chesworth B, Davis A, Mahomed N, Charron KJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. | ||
Baker PN, van der Meulen JH, Lewsey J, Gregg PJ; National Joint Registry for England and Wales. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br. 2007;89(7):893–900. | ||
Scuderi GR. The stiff total knee arthroplasty: causality and solution. J Arthroplasty. 2005;20(4 suppl 2):23–26. | ||
Pavlin DJ, Chen C, Penaloza DA, Buckley FP. A survey of pain and other symptoms that affect the recovery process after discharge from an ambulatory surgery unit. J Clin Anesth. 2004;16(3):200–206. | ||
Ip HYV, Abrishami A, Peng PWH, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. 2009;111(3):657–677. | ||
Rakel BA, Blodgett NP, Bridget Zimmerman M, et al. Predictors of postoperative movement and resting pain following total knee replacement. Pain. 2012;153(11):2192–2203. | ||
Abrishami A, Chan J, Chung F, Wong J. Preoperative pain sensitivity and its correlation with postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. 2011;114(2):445–457. | ||
Pan PH, Coghill R, Houle TT, et al. Multifactorial preoperative predictors for postcesarean section pain and analgesic requirement. Anesthesiology. 2006;104(3):417–425. | ||
Hsu Y, Somma J, Hung Y, Tsai P, Yang C, Chen C. Predicting postoperative pain by preoperative pressure pain assessment. Anesthesiology. 2005;103(3):613–618. | ||
Werner MU, Duun P, Kehlet H. Prediction of postoperative pain by preoperative nociceptive responses to heat stimulation. Anesthesiology. 2004;100(1):115–119. | ||
Granot M, Lowenstein L, Yarnitsky D, Tamir A, Zimmer EZ. Postcesarean section pain prediction by preoperative experimental pain assessment. Anesthesiology. 2003;98(6):1422–1426. | ||
Granot M. Can we predict persistent postoperative pain by testing preoperative experimental pain? Curr Opin Anesthesiol. 2009;22(3):425–430. | ||
Werner M, Mjöbo HN, Nielsen PR, Rudin ÅMD. Prediction of postoperative pain: a systematic review of predictive experimental pain studies. Anesthesiology. 2010;112(6):1494–1502. | ||
Ruscheweyh R, Marziniak M, Stumpenhorst F, Reinholz J, Knecht S. Pain sensitivity can be assessed by self-rating: development and validation of the pain sensitivity questionnaire. Pain. 2009;146(1–2):65–74. | ||
Ruscheweyh R, Verneuer B, Dany K, et al. Validation of the pain sensitivity questionnaire in chronic pain patients. Pain. 2012;153(6):1210–1218. | ||
Sellers AB, Ruscheweyh R, Kelley BJ, Ness TJ, Vetter TR. Validation of the english language pain sensitivity questionnaire. Reg Anesth Pain Med. 2013;38(6):508–514. | ||
Kim H-J, Lee J-I, Kang K-T, et al. Influence of pain sensitivity on surgical outcomes after lumbar spine surgery in patients with lumbar spinal stenosis. Spine. 2015;40(3):193–200. | ||
Bjørgen S, Jessen V, Husby OS, Røset Ø, Foss OA. Internal quality register for joint prostheses. Tidsskr Nor Laegeforen. 2012;132(6):626–627. | ||
American Society of Anestehesiologist [webpage on the Internet]. ASA Physical Status Classification System; 2014. Available from: https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system. Accessed July 25, 2016. | ||
Daut RL, Cleeland CS, Flanery RC. Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain. 1983;17(2):197–210. | ||
Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17–24. | ||
Klepstad P, Loge JH, Borchgrevink PC, Mendoza TR, Cleeland CS, Kaasa S. The Norwegian brief pain inventory questionnaire: translation and validation in cancer pain patients. J Pain Symptom Manage. 2002;24(5):517–525. | ||
Gjeilo KH, Stenseth R, Wahba A, Lydersen S, Klepstad P. Validation of the brief pain inventory in patients six months after cardiac surgery. J Pain Symptom Manage. 2007;34(6):648–656. | ||
Bonnin MP, Basiglini L, Archbold HAP. What are the factors of residual pain after uncomplicated TKA? Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1411–1417. | ||
Beswick AD, Wylde V, Gooberman-Hill R. Interventions for the prediction and management of chronic postsurgical pain after total knee replacement: systematic review of randomised controlled trials. BMJ Open. 2015;5:e007387. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
