Back to Journals » Advances in Medical Education and Practice » Volume 9
Relationship between poor quality sleep, excessive daytime sleepiness and low academic performance in medical students
Authors El Hangouche AJ , Jniene A, Aboudrar S, Errguig L, Rkain H, Cherti M , Dakka T
Received 12 January 2018
Accepted for publication 2 May 2018
Published 7 September 2018 Volume 2018:9 Pages 631—638
DOI https://doi.org/10.2147/AMEP.S162350
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Md Anwarul Azim Majumder
Abdelkader Jalil El Hangouche,1–3 Asmaa Jniene,1 Souad Aboudrar,1 Leila Errguig,1 Hanan Rkain,1 Mohammed Cherti,2 Taoufiq Dakka1
1Exercise Physiology and Autonomic Nervous System Team “EPE-SNA”, Laboratory of Physiology, Faculty of Medicine and Pharmacy of Rabat, Mohamed V University, Rabat, Morocco; 2Department of Cardiology, Ibn Sina Hospital, Faculty of Medicine and Pharmacy of Rabat, Mohamed V University, Rabat, Morocco; 3Laboratory of Physiology, Faculty of Medicine and Pharmacy of Tangier, Abdelmalek Essaadi University, Tangier, Morocco
Purpose: Poor quality of sleep and excessive daytime sleepiness affect cognitive ability and have a negative impact on the academic performance of medical students. This study aims to determine the prevalence of excessive daytime sleepiness, sleep quality and psychological distress as well as assess their association with low academic performance in this population.
Participants and methods: A cross-sectional study was conducted among 457 medical students from the Faculty of Medicine and Pharmacy of Rabat, Morocco, who completed the Pittsburgh Sleep Quality Index (PSQI) questionnaire and the Epworth Sleepiness Scale to determine the quality of sleep and excessive daytime sleepiness, respectively. Sociodemographic variables and psychological distress (Kessler Psychological Distress Scale) were also measured. Multivariate linear regression was performed in order to evaluate the link between low academic performance and sleep quality after adjusting for other covariates.
Results: Among the included students, the median age was 20 (19; 21) years; 70.7% of the participants were females. Almost one-third of the students (36.6%) had excessive daytime sleepiness and this was more frequently observed in female students (43% vs 20.1%, <0.001). Furthermore, 58.2% of the students were poor sleepers (PSQI ≥5), while 86.4% of them had psychological distress. The bivariate analysis showed that psychological distress was associated with decreased risk of low performance (ß=0.04; 95% CI=0.005–0.07; P=0.024). Being a poor sleeper was statistically associated with poor academic performance (ß= −0.07; 95% CI=−0.14 to −0.002; P=0.04) in the multivariate analysis. In our study, daytime sleepiness was not statistically associated with academic performance.
Conclusion: A poor sleep quality determined by PSQI ≥5 was related to poor academic achievement at the end of the study year in medical students.
Keywords: quality of sleep, daytime sleepiness, psychological distress, academic performance, medical students
Introduction
In the last decades, excessive daytime sleepiness and poor quality of sleep have been increasingly recognized as symptoms that must be identified and managed early because of their high prevalence in the general population, their numerous and potentially serious consequences, and their association with the majority of sleep disorders.1 Excessive daytime sleepiness refers to uncontrollable dozing off and drowsiness during the daytime, leading to the inability to remain alert and cautious in performing important daily activities.2 Excessive daytime sleepiness can be caused in a large proportion by poor quality of sleep and can directly affect the behavior and job performance of the individuals.3,4 The prevalence of excessive daytime sleepiness would be 12%–16% among the general population,5,6 and approximately one-third of adults report it as some form of insomnia during the course of a year.7
Among university students, sleep disturbances have been observed to be prevalent.8,9 In a study in the United Kingdom, 24% of university students reported that they have difficulty in going to sleep and slept less than 7 hours per night, and 45% complained that they were unable to wake up properly.10 New social and academic environment, excessive use of social media11,12 and unhealthy lifestyle choices are some of the factors attributed to sleep problems among undergraduate students.13
In addition to these factors, medical students generally do not have adequate quality of life due to their high academic load, hospital shifts and long hours of night study, which may even upset their quality of sleep and increase the risk of excessive daytime sleepiness.14,15
Among the many consequences of this worrying finding, poor sleep quality has been associated with increased risk of burnout,16 psychoactive substance use,13 anxiety and depression.17,18 Moreover, numerous studies have shown a negative impact of daytime sleepiness and poor sleep quality on the academic performance of medical university students.19–21 Indeed, hours of sleep acquired before exam time has been identified as a predictor of exam scores among medical students;22 also excessive daytime sleepiness before exams has been shown to correlate with worse academic achievement.23
In fact, sleep represents a set of many physiologic processes under primarily neurobiological regulation that impact several physiologic systems including the neurocognitive functioning.19,24 For instance, a number of studies have demonstrated that a period of sleep protects memories from interference, improves performance and reorganizes memory traces in a way that encourages creativity and rememorization. These benefits come from the reactivation of brain networks, involving the hippocampal structure, as well as from their synchronization with neocortical networks during sleep, thereby underpinning sleep-dependent memory consolidation and reorganization.25
Additionally, other non-academic issues such as psychological distress management are also important for academic success.26 In fact, some studies have found that high levels of stress can affect the level of concentration and academic performance.27
From a Moroccan perspective, it is important to have a better understanding of medical students’ mental and physical health and to identify and address their unmet needs through medical school counseling centers. Therefore, the objectives of this study were to determine the prevalence of poor sleep quality of sleep, daytime sleepiness and psychological distress among medical students and their association with academic performance in Morocco. According to our research, there are no data in our context assessing this association.
Participants and methods
Study design and sampling method
To put the study results in perspective to an international audience, it is important to mention that Moroccan medical university aligns with the European system. Hence, medical students are selected immediately after their high school graduation. During the five first years, Moroccan medical students only attend clinical sessions and lectures, and they are neither expected to be on call during their clinical years nor obligated to actively participate in all clinical care beyond their teaching sessions. Being part of a medical team and being on call are expected from students in their obligatory internship years (namely, sixth and seventh year). Interns are not perceived as students and are not a target group of this study.
A cross-sectional study was conducted from February 2017 to April 2017 in the Faculty of Medicine and Pharmacy of Rabat - Morocco. A sample of 600 medical students in the first to the fifth year was selected randomly from the list of all students registered in the Faculty of Medicine of Rabat University of Mohammed V, which was obtained from the Academic Affairs Department of the University.
The students registered in the sixth and seventh year were excluded from the study, because their academic evaluation is not based on the score obtained at the end of the academic year but rather on criteria related to their internship. Pharmacy students were also excluded, due to the fact that they have a different academic program and educational constraints in comparison with medical students. A total of 457 students (76.2%) agreed to participate. The investigation was conducted 1 month before the examination period so that the students were not affected by the additional stressful factors.
This study was approved by the Research and Ethics Committees of the Faculty of Medicine and Pharmacy of Rabat Research. All participants provided written informed consent.
Data collection and instrument
The students were interviewed after obtaining an informed consent from each participant, through a standard self-administered questionnaire, divided into four sections, and each section included several questions to assess the following items:
- The anthropometric characteristics (age, sex, body mass index [BMI] defined as the body mass divided by the square of the body height and is expressed in units of kg/m2, resulting from mass in kilograms and height in meters).
- Evaluation of excessive daytime sleepiness using the Epworth Sleepiness Scale (ESS), a self-administered questionnaire with eight-item scale to assess the chance of falling asleep or dozing off during different daily life situations in an ordinary day. The method of scoring is identical in all questions. The patient gives the score of 0–3 for each situation where there is no chance, slight chance, moderate chance and high chance of dozing or falling asleep, respectively. The score obtained from the scale ranges from 0 to 24. A score ranging from 0 to 10 is defined as normal, while a score of 11–24 is considered to be abnormal and indicative of excessive daytime somnolence.2,28–30
- The qualitative assessment of sleep using the Pittsburgh Sleep Quality Index (PSQI) consists of 19 items and seven clinically relevant domains of sleep difficulties: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, use of sleep medication and daytime dysfunction. A global score of overall sleep quality can be calculated by adding up the single scores of these dimensions, resulting in scores ranging from 0 to 21. Global scores >5 are generally used to indicate poor sleep.31
- Evaluation of the level of psychological distress using Kessler Psychological Distress Scale (K6), which involves 6 questions about a person’s emotional state. Each question is scored from 0 (none of the time) to 4 (all of the time). Scores of K6 range from 0 to 24, with established threshold: 0–13 (low levels of psychological distress) and 14–24 (high levels of psychological distress) applied to provide a measure of psychological distress among the participants.32
The assessment of the students’ academic performance consisted of collecting all the marks obtained by each student on the annual final exams and calculating the general average mark of the year. This method seemed to be the most accurate to us because all students aim for the highest mark allowing them to validate their modules and their academic year.
Statistical analysis
A double data entry was performed for data quality insurance. Analysis was made using SPSS v13 Software.
The data were collected and transposed on an EXCEL table and analyzed by the “SPSS 20.0” software. The normal distribution of data was assessed by Kolmogorov–Smirnov test.
The quantitative variables, in asymmetric distribution, were expressed by median and interquartile range and, in symmetric distribution, by mean and SD. Categorical variables were summarized as numbers and percentages.
To compare means according to sex, Mann–Whitney test (age, BMI) or Student’s t-test (average mark) was used. For categorical variables (sex, daytime sleepiness [ESS], sleep quality [PSQI], level of psychological distress [K6]), percentages were compared using the Pearson’s chi-squared test.
Univariate and multivariate linear regression models were used to identify the associated factors with decrease of academic performance. P-values <0.05 were considered significant. All beta coefficients were reported with a 95% confidence interval.
Results
The survey included 600 medical university students randomly recruited from the Faculty of Medicine and Pharmacy of Rabat in Morocco using a simple random sample selection method. The response rate was 76.2%.
The sociodemographic characteristics of the interviewed students were as follows: 70.7% were women, the median age was 20 (19;21) years and the median of BMI was 21.4 (19.8; 23.1) kg/m2. There were differences among sexes for the variables of age and BMI (Table 1).
Concerning the assessment of daytime sleepiness among those students, the mean score of ESS was 9±4.2 (Figure 1), 36.3% of students had excessive daytime somnolence (ESS >10) and more frequently in the female students than male students (43% vs 20.1%; P<0.001; Table 1).
  | Figure 1 Histograms showing the distribution of Epworth Sleepiness Scale and PSQI Score in the study population. Abbreviation: PSQI, Pittsburgh Sleep Quality Index. |
For the qualitative assessment of sleep, the mean score of PSQI was 6.3±3 (Figure 1), the score was greater than 5 in 58.2% of students (poor sleepers), with no significant difference between the female and male students (Table 1).
In terms of assessing students’ status of psychological distress using the K6 scale, we found that 86.4% of students presented tendency toward high levels of psychological distress (K6 >13). There were no differences among sexes for the variables of PSQI or K6.
The assessment of the students’ academic performance showed that the mean of general average marks of all students was 12.74 of 20±2.26 with no significant difference according to the sex (Table 1).
According to their academic year, there were no statistically significant differences among students regarding the following statements: daytime sleepiness and psychological distress, whereas we found a significant difference regarding quality of sleep: students in third to fifth medical year have a poor quality of sleep compared to the students in first or second year (Table 2).
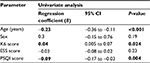
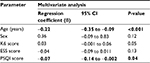
Investigating the relationship between both the students’ excessive daytime sleepiness (ESS score) and quality of sleep (PSQI score), respectively, with the decrease of their academic performance and adjusting on the factors collected by the questionnaire (age, sex and level of psychological distress); The linear regression analysis suggested, in univariate model, the high level of psychological distress (K6 score) as factor of increased academic performance (β=0.04; 95% CI=0.005–0.07; P<0.024) and showed that factors associated to low academic performance were the old age (β=−0.22; 95% CI=−0.35 to −0.09; P<0.001) and the poor sleep (β=−0.07; 95% CI=−0.14 to −0.002; P=0.04). However, regarding daytime sleepiness, we found that in our study it was not statistically associated with academic performance (Tables 3 and 4).
In the light of our results, besides the positive relationship between psychological stress in medical students and academic performance (β=0,04), we found, after adjusting for other factors, that disturbed and poor quality of sleep in our medical students’ population is significantly associated with low academic performance, and this negative association between poor sleep and academic performance can be predicted by the following equation of regression in adjusted model:
Academic performance (general average mark) = 16.89 −0.22*age +0.36*sex (1: man; 2: woman) + 0.03*K6 score 0.04*ESS score-0.07*PSQI score, with adjusted R-squared: 0.06 (Tables 3 and 4).
Discussion
The aim of this study was to asses sleep quality, excessive daytime sleepiness and psychological distress among Moroccan medical students 1 month before the examination period and their potential consequences on academic performance. Our findings showed that more than a third of medical students present with an excessive daytime sleepiness; 58.2% reported disturbed sleep and 86.4% presented tendency toward high levels of psychological distress. Additionally, we found that academic performance was statistically associated with a poor quality of sleep and psychological distress. However, the current study revealed that daytime sleepiness does not affect Moroccan medical students’ academic performance.
Sleep is an essential component of physical and mental health.33 A large body of evidence supports the notion that good sleep is important for optimal neurocognitive and psychomotor performance.34,35 Indeed, several studies have demonstrated a directly proportional correlation between suboptimal sleep duration (less than 7–8 h of sleep per night), sleep and wake habits, and poor academic performance.20,36,37 Recently, a meta-analytic review of 61 studies from 71 different populations has provided evidence that short-term sleep restriction significantly impacts waking neurocognitive functioning.33
Excessive daytime sleepiness is particularly frequent in university students, with a prevalence ranging between 24% and 39%.38–40 In our study, the overall prevalence of excessive daytime sleepiness was 36.3% with more prevalence in female students (43%). Our finding is consistent with those of other studies conducted in Malaysia (35.5%), Pakistan (39.5%) and Saudi Arabia (37.8%), but much lower than the prevalence of excessive daytime sleepiness shown in the medical students in Brazil (63%).38,41–43 The findings of Lund et al and Angelone et al corroborate that female students have higher prevalence of daytime sleepiness than male students.13,44
The reported excessive daytime sleepiness in our study does not seem to affect significantly the academic performance of the included students as found in the study of Al-Zahrani et al.38
However, the findings of other previous studies support the fact that daytime sleepiness may negatively affect academic achievement and motivation of students.21 Indeed, Dewald et al reported daytime sleepiness as a determinant of school performance in children and adolescents, and a more recent study reported that daytime sleepiness in first year nursing students who regard their own academic achievement as poor was higher.20,34,45 These discordant results can be explained by the heterogeneity of the participants described in the literature. Hence, the effect of daytime sleepiness on academic performance is more found in studies focusing on young children than studies focusing on older subjects; this influence may also differ according to the nature of the studies and the skills assessed during the exam.38,45
Several causes may be behind excessive daytime sleepiness. Researchers have found that university students who had lower nocturnal sleep duration or an irregular sleep–wake schedule were more likely to report daytime sleepiness.39,46,47 However, Lund et al found no association between sleep duration and daytime sleepiness, inferring that the association may have been diminished by daytime napping and other factors such as poor time management or irregular sleep patterns.13 In this context, it has been suggested that the investigation of factors affecting daytime sleepiness should include other sleep hygiene and lifestyle factors, including tea or coffee consumption and sleep environment variables such as temperature, light and noise.48,49
Poor quality of sleep assessed by PSQI scoring was found in almost two-thirds (58.2%) of included students with no significant sex difference, which is lower than finding in Colombia (79.3%)14 and almost the double of the prevalence in medical students in Saudi Arabia (30%)50 and Malaysia (41.8%).42 While no significant difference was elicited in the academic achievement of those having normal sleep versus those with excessive daytime sleepiness, in our study, we found that poor quality of sleep is significantly associated with low academic performance of medical university students. In fact, previous studies and the present study findings support the conclusion that having poor quality of sleep may negatively affect academic performance of students.42
Recently, Machado-Duque et al demonstrated that poor sleep quality determined by low sleep efficiency <65% was significantly related to poor academic achievement at the end of semester in medical students.14 Also, a statistically significant difference was reported between the excellent scoring and average students with regard to subjective feelings of insufficient sleep and sleeping less than 6 h for six nights (chronic sleep deprivation).23 This negative association has been explained in several studies by the stress of the medical student due to high academic load such as exams or clinical practices, which leads to a vicious circle between stress, poor sleep quality and low academic performance.51,52
Other variables that were associated with low sleep quality were nightmares and pain at night, which can be responsible for multiple nocturnal awakenings, which decrease the sleep efficiency and affect its quality.53
It is interesting to note that an important portion of our study population (86.4%) reported symptoms of psychological distress according to K6, and this prevalent stress among the included students was positively and significantly associated with improved academic performance. In literature, there was evidence that the psychological distress and symptoms of depression and anxiety were significant predictors of poor sleep quality among the students.19,54,55 Moreover, besides sleep quality (bad vs good), the psychological distress remained statistically significantly associated with excessive daytime sleepiness.42 Also, some studies reported that higher level of stress is associated with poor academic performance among medical students.56
Those findings are in opposition to our results that suggested that there is a positive correlation between psychological distress and academic performance. This finding is supported by the study of Kumar et al who showed the beneficial effects of stress on female medical students; stress did positively impact their attendance rate and day-to-day performance, which are significantly higher compared to their male counterparts.57 However, other studies did not establish any correlation between psychological distress and academic performance.58
This contrasting result could be explained by the fact that in our study, the stress assessment was conducted during the preparation phase, 1 month before the final exam. This means that stress can eventually have a beneficial effect if it does not occur during the examination period. Another possible explanation would be the fact that female students represented the majority of our sample, reflecting the reality of the distribution of the students in our faculty and thus interfering with different management of stress according to sex. Moreover, our funding suggests that there are other mechanisms and processes behind the positive and beneficial impact of stress on academic performance and that these do not interfere with sleep disturbances.
Many factors, such as pursuing graduate studies, may influence students’ concepts of sleeping time, leading to a deficit of sleep quality. For instance, intensive education programs conducted for health care professions, such as medicine, force students to increasingly sacrifice their sleep hours, as we have found in our study.34 Likewise, several studies have been carried out to assess baseline knowledge, attitudes and perceptions about sleep among medical students; except for some notable exceptions, the authors have found inadequate knowledge and many misconceptions regarding sleep.61–63 This body of literature suggests that sleep education in current medical curricula is generally inadequate worldwide. For this reason, sleep disturbances remain a public health problem that requires taking interventional measures and raising the awareness of educational institutions in order to improve student action in building up of their own sleep quality.
The authors acknowledge some limitations of this study. The reliance on the self-reported questionnaire in data collection made our data more subjective. The number of women enrolled in our sample was higher than men; this is due to the high proportion of women in our faculty. Also, in order to reduce the duration of the interview and maintain a high response rate, we did not include questions regarding socioeconomic dimension of students and the existence of specific sleep disorder as obstructive sleep apnea or periodic limb movement in our survey. Larger multicenter and longitudinal studies are needed to examine the causes of sleep disorders and to implement preventive measures to enhance the university students’ academic performance.
Conclusion
Our study findings reveal that poor sleep quality and excessive daytime sleepiness and psychological distress are highly prevalent in medical students. Significant associations were observed between poor sleep quality and low academic performance. This warrants giving attention to this important aspect in medical students’ life through educational interventions. With these findings, awareness about the negative impacts of sleep disturbances on academic performance can be raised by both teaching staff and medical students. Therefore, measures to improve sleep habits among medical students are highly recommended.
Acknowledgment
The authors gratefully acknowledge all the medical students who participated in and contributed to the study.
Disclosure
The authors report no conflicts of interest in this work.
References
Ohayon MM. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev. 2008;12(2):129–141. | ||
Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540–545. | ||
Sierra JC, Jiménez-Navarro C, Martín-Ortiz JD. Calidad del sueño en estudiantes universitarios: importancia de la higiene del sueño [Quality of sleep in university students: importance of sleep hygiene.]. Salud Mental. 2002;25(6):35–43. Spanish [with English abstract]. | ||
Bonnet MH, Arand DL. We are chronically sleep deprived. Sleep. 1995;18(10):908–911. | ||
Roth T, Roehrs TA. Etiologies and sequelae of excessive daytime sleepiness. Clin Ther. 1996;18(4):562–576; discussion 561. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-V-TR). 5th ed. Text Revision. Washington, DC: American Psychiatric Association; 2013. | ||
Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985;42(3):225–232. | ||
Adeosun SO, Asa SO, Babalola OO, Akanmu MA. Effects of night-reading on daytime sleepiness, sleep quality and academic performance of undergraduate pharmacy students in Nigeria. Sleep Biol Rhythms. 2008;6(2):91–94. | ||
James BO, Omoaregba JO, Igberase OO. Prevalence and correlates of poor sleep quality among medical students at a Nigerian university. Ann Nigerian Med. 2011;5(1):1. | ||
Webb E, Ashton CH, Kelly P, Kamali F. Alcohol and drug use in UK university students. Lancet. 1996;348(9032):922–925. | ||
Xu XL, Zhu RZ, Sharma M, Zhao Y. The influence of social media on sleep quality: a study of undergraduate students in Chongqing, China. J Nurs Care. 2015;4(3):1–7. | ||
Chokroverty S. Sleep Disorders Medicine: Basic Science, Technical Considerations, and Clinical Aspects. 3rd ed. Philadelphia, PA: Saunders, an imprint of Elsevier Inc.; 2009. | ||
Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46(2):124–132. doi:10.1016/j.jadohealth.2009.06.016. | ||
Machado-Duque ME, Echeverri Chabur JE, Machado-Alba JE. [Excessive daytime sleepiness, poor quality sleep, and low academic performance in medical students]. Rev Colomb Psiquiatr. 2015;44(3):137–142. Spanish [with English abstract]. | ||
Collazo CAR, Rodríguez FO, Rodríguez YH. El estrés académico en estudiantes latinoamericanos de la carrera de Medicina [Academic stress in Latin American students of the Medicine career]. Revista Iberoamericana de Educación. 2008;46(7):1. Spanish [with English abstract]. | ||
Kang JH, Chen SC. Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health. 2009;9:248. | ||
Fernández-Mendoza J, Vela-Bueno A, Vgontzas AN, et al. Nighttime sleep and daytime functioning correlates of the insomnia complaint in young adults. J Adolesc. 2009;32(5):1059–1074. | ||
Millman RP; Working Group on Sleepiness in Adolescents/Young Adults; AAP Committee on Adolescence. Excessive sleepiness in adolescents and young adults: causes, consequences, and treatment strategies. Pediatrics. 2005;115(6):1774–1786. | ||
Cvejic E, Huang S, Vollmer-Conna U. Can you snooze your way to an “A”? Exploring the complex relationship between sleep, autonomic activity, wellbeing and performance in medical students. Aust N Z J Psychiatry. 2018;52(1):39–46. | ||
Bahammam AS, Alaseem AM, Alzakri AA, Almeneessier AS, Sharif MM. The relationship between sleep and wake habits and academic performance in medical students: a cross-sectional study. BMC Med Educ. 2012;12:61. | ||
Abdulghani HM, Alrowais NA, Bin-Saad NS, Al-Subaie NM, Haji AMA, Alhaqwi AI. Sleep disorder among medical students: relationship to their academic performance. Med Teach. 2012;34 (Suppl 1):S37–S41. | ||
Sitticharoon C, Srisuma S, Kanavitoon S, Summachiwakij S. Exploratory study of factors related to educational scores of first preclinical year medical students. Adv Physiol Educ. 2014;38(1):25–33. | ||
Mirghani HO, Ahmed MA, Elbadawi AS. Daytime sleepiness and chronic sleep deprivation effects on academic performance among the Sudanese medical students. J Taibah Univ Med Sci. 2015;10(4):467–470. | ||
Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66:143–172. | ||
Cherdieu M, Versace R, Rey AE, Vallet GT, Mazza S. Sleep on your memory traces: How sleep effects can be explained by Act–In, a functional memory model. Sleep Med Rev. 2018;39:155–163. | ||
Abdulghani HM, Al-Drees AA, Khalil MS, Ahmad F, Ponnamperuma GG, Amin Z. What factors determine academic achievement in high achieving undergraduate medical students? A qualitative study. Med Teach. 2014;36 (Suppl 1):S43–S48. | ||
Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross-sectional study. Med Educ. 2005;39(6):594–604. | ||
Pahwa P, Karunanayake C, Hagel L, et al. Prevalence of high Epworth Sleepiness Scale scores in a rural population. Can Respir J. 2012;19(2):e10–e14. | ||
Johns M, Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997;20(10):844–849. | ||
Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15(4):376–381. | ||
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. | ||
Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. | ||
Lowe CJ, Safati A, Hall PA. The neurocognitive consequences of sleep restriction: a meta-analytic review. Neurosci Biobehav Rev. 2017;80:586–604. | ||
Demir G. Daytime sleepiness and related factors in nursing students. Nurse Educ Today. 2017;59 (Suppl C):21–25. | ||
Giri P, Baviskar M, Phalke D. Study of sleep habits and sleep problems among medical students of Pravara Institute of Medical Sciences Loni, Western Maharashtra, India. Ann Med Health Sci Res. 2013;3(1):51–54. | ||
Gaultney JF. The prevalence of sleep disorders in college students: impact on academic performance. J Am Coll Health. 2010;59(2):91–97. | ||
Gilbert SP, Weaver CC. Sleep quality and academic performance in University students: a wake-up call for college psychologists. J College Stud Psychother. 2010;24(4):295–306. | ||
Al-Zahrani JM, Aldossari KK, Abdulmajeed I, Al-Ghamdi SH, Al-Shamrani AM, Al-Qahtani NS. Daytime sleepiness and academic performance among Arab medical students. J Thorac Dis. 2016;8(2):AB006. | ||
Huang CF, Yang LY, Wu LM, Liu Y, Chen HM. Determinants of daytime sleepiness in first-year nursing students: a questionnaire survey. Nurse Educ Today. 2014;34(6):1048–1053. | ||
Rodrigues RN, Viegas CA, Abreu E Silva AA, Tavares P. Daytime sleepiness and academic performance in medical students. Arq Neuropsiquiatr. 2002;60(1):6–11. | ||
Surani AA, Zahid S, Surani A, Ali S, Mubeen M, Khan RH. Sleep quality among medical students of Karachi, Pakistan. J Pak Med Assoc. 2015;65(4):380–382. | ||
Zailinawati AH, Teng CL, Chung YC, Teow TL, Lee PN, Jagmohni KS. Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia. 2009;64(2):108–110. | ||
Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38(4):438–444.. | ||
Angelone AM, Mattei A, Sbarbati M, Di Orio F. Prevalence and correlates for self-reported sleep problems among nursing students. J Prev Med Hyg. 2011;52(4):201–208. | ||
Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2010;14(3):179–189. | ||
Regestein Q, Natarajan V, Pavlova M, Kawasaki S, Gleason R, Koff E. Sleep debt and depression in female college students. Psychiatry Res. 2010;176(1):34–39. | ||
Taher YA, Samud AM, Ratimy AH, Seabe AM. Sleep complaints and daytime sleepiness among pharmaceutical students in Tripoli. Libyan J Med. 2012;7:18930. | ||
Morrison I, Riha RL. Excessive daytime sleepiness and narcolepsy – an approach to investigation and management. Eur J Intern Med. 2012;23(2):110–117. | ||
Buboltz WC, Soper B, Brown F, Jenkins S. Treatment approaches for sleep difficulties in college students. Couns Psychol Q. 2002;15:229–237. | ||
Alsaggaf MA, Wali SO, Merdad RA, Merdad LA. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years. Relationship with stress and academic performance. Saudi Med J. 2016;37(2):173–182. | ||
Berto de Spinola BR, De Spinola H, De Spinola H, de Oliveira BR, Witte H, Spinola H. Rendimiento académico y factores psicosociales en los ingresantes a la carrera de medicina – UNNE [Academic performance and psychosocial factors in those entering the medical career–UNNE]. 1990;78:143–67. Spanish [with English abstract]. | ||
Shilo L, Sabbah H, Hadari R, et al. The effects of coffee consumption on sleep and melatonin secretion. Sleep Med. 2002;3(3):271–273. | ||
Genzel L, Ahrberg K, Roselli C, et al. Sleep timing is more important than sleep length or quality for medical school performance. Chronobiol Int. 2013;30(6):766–771. | ||
Seun-Fadipe CT, Mosaku KS. Sleep quality and psychological distress among undergraduate students of a Nigerian university. Sleep Health. 2017;3(3):190–194. | ||
Johns MW, Dudley HA, Masterton JP. The sleep habits, personality and academic performance of medical students. Med Educ. 1976;10(3):158–162. | ||
Sohail N. Stress and academic performance among medical students. J Coll Physicians Surg Pak. 2013;23(1):67–71. | ||
Kumar M, Sharma S, Gupta S, Vaish S, Misra R. Effect of stress on academic performance in medical students – a cross sectional study. Indian J Physiol Pharmacol. 2014;58(1):81–86. | ||
Dendle C, Baulch J, Pellicano R, et al. Medical student psychological distress and academic performance. Med Teach. Epub 2018 Jan 21. | ||
Grandner MA. Sleep, health, and society. Sleep Med Clin. 2017;12(1):1–22. | ||
Silva M, Chaves C, Duarte J, Amaral O, Ferreira M. Sleep quality determinants among nursing students. Procedia Soc Behav Sci. 2016;217 (Suppl C):999–1007. | ||
AlFakhri L, Sarraj J, Kherallah S, Kuhail K, Obeidat A, Abu-Zaid A. Perceptions of pre-clerkship medical students and academic advisors about sleep deprivation and its relationship to academic performance: a cross-sectional perspective from Saudi Arabia. BMC Res Notes. 2015;8:740. | ||
Mahendran R, Subramaniam M, Chan YH. Medical students’ behaviour, attitudes and knowledge of sleep medicine. Singapore Med J. 2004;45(12):587–589. | ||
Azad MC, Fraser K, Rumana N, et al. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. 2015;11(1):69–74. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.