Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Relationship Between Episodic Nocturnal Hypercapnia and History of Exacerbations in Patients with Advanced Chronic Obstructive Pulmonary Disease
Authors Kitajima T , Marumo S, Amimoto H, Shiraishi Y, Yamaki H, Shirata M, Inoue D, Fukui M
Received 10 February 2022
Accepted for publication 25 June 2022
Published 7 July 2022 Volume 2022:17 Pages 1553—1563
DOI https://doi.org/10.2147/COPD.S361914
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Russell
Takamasa Kitajima,1 Satoshi Marumo,1 Hisanori Amimoto,2 Yusuke Shiraishi,3 Haruka Yamaki,3 Masahiro Shirata,3 Daiki Inoue,1 Motonari Fukui1
1Respiratory Disease Center, Kitano Hospital, Tazuke Kofukai Medical Research Institute, Osaka, Japan; 2Department of Respiratory Medicine, Kobe City Medical Center West Hospital, Kobe, Japan; 3Department of Respiratory Medicine, Kyoto University, Graduate School of Medicine, Kyoto, Japan
Correspondence: Takamasa Kitajima, Respiratory Disease Center, Kitano Hospital, Tazuke Kofukai Medical Research Institute, 2-4-20 Ohgimachi, Kita-ku, Osaka, 530-8480, Japan, Tel +81-6-6312-8831, Fax +81-6-6361-8867, Email [email protected]
Purpose: An episodic increase in transcutaneous carbon dioxide pressure (PtcCO2) is often recognized in patients with advanced chronic obstructive pulmonary disease (COPD) by overnight PtcCO2 monitoring. This phenomenon, called episodic nocturnal hypercapnia (eNH), mainly corresponds to rapid eye movement (REM) sleep-related hypoventilation. However, it is unclear whether eNH is associated with the frequency of COPD exacerbation. We aimed to investigate whether a relationship exists between COPD exacerbation and eNH.
Patients and Methods: We enrolled consecutive patients with stable, severe, or very severe COPD with a daytime arterial carbon dioxide pressure (PaCO2) < 55.0 mmHg who underwent overnight PtcCO2 monitoring from April 2013 to January 2017. We retrospectively analyzed the prevalence of eNH and sleep-associated hypoventilation (SH) as defined by the American Academy of Sleep Medicine. Moreover, we compared the relationship between the frequency of COPD exacerbations in the previous year and eNH or SH.
Results: Twenty-four patients were included in this study. The study patients had a mean daytime PaCO2 and nocturnal PtcCO2 of 43.3 ± 6.8 mmHg and 42.9 ± 9.6 mmHg, respectively. Six (25.0%) and 11 (45.9%) of the 24 patients met the SH and eNH criteria, respectively. The odds ratios of SH and eNH for at least one annual exacerbation were 1.0 [95% confidence interval (CI): 0.16– 6.00] and 11.1 [95% CI: 1.39– 87.7], respectively. The odds ratios of SH and eNH for at least two annual exacerbations were 0.3 [95% CI: 0.04– 2.64] and 6.6 [95% CI: 1.06– 39.4], respectively.
Conclusion: In patients with advanced COPD and a daytime PaCO2 < 55.0 mmHg, eNH may be associated with a history of more frequent exacerbations than SH. Further studies are required to validate these findings.
Keywords: episodic nocturnal hypercapnia, sleep-associated hypoventilation, exacerbations, arterial carbon dioxide pressure, rapid eye movement
Introduction
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide.1 Exacerbations are common events that have a significant impact on COPD patients and healthcare services,2 affecting lung function, health status, and mortality.3,4 In addition, a history of exacerbations has been reported to be the best predictor of future exacerbations,5 and repeated severe exacerbations were associated with high future mortality.4
Certain studies have shown that daytime hypercapnia is associated with frequent exacerbation and poor prognosis in COPD patients.6–8 In particular, daytime hypoventilation is considered to be associated with repeated COPD exacerbation and a poor prognosis. In patients with advanced COPD, hypercapnic respiratory failure manifests earlier during sleep than during the awake state as a consequence of pathophysiological changes in ventilation.9 Therefore, sleep-related hypoventilation disorders may be related to COPD exacerbations before daytime hypercapnia becomes apparent. However, there are few reports showing the importance of sleep-related ventilation disorders on exacerbations in patients with COPD without remarkable daytime hypercapnia.
The American Academy of Sleep Medicine (AASM) defines hypoventilation during sleep as sleep-associated hypoventilation (SH),10 which needs to meet the following criteria: (1) an increase in the PaCO2 or transcutaneous carbon dioxide pressure (PtcCO2) to a value >55 mmHg for ≥10 min and (2) ≥10 mmHg increase in PaCO2 or transcutaneous carbon dioxide pressure (PtcCO2) during sleep (compared to the awake supine value) to a value exceeding 50 mmHg for ≥10 min. Unfortunately, no research has shown the relationship between SH and COPD exacerbation.
Aside from SH, we defined episodic nocturnal hypercapnia (eNH) as an episodic increase of ≥5 mmHg from baseline PtcCO2 for ≥5 min at least once during the night as reported in a previous study.11 eNH is more focused on rapid eye movement (REM) sleep-related hypoventilation than SH. Nocturnal hypercapnia often worsens during REM sleep9 because of the decreased activity of the respiratory muscles and diminished hypercapnic and hypoxic ventilatory response.12–14 REM sleep-related hypoventilation can be observed as episodic nocturnal increases in PtcCO2 during overnight PtcCO2 monitoring.12 We have shown that eNH seems to be related to exacerbation frequency in COPD patients with daytime PaCO2 <55 mmHg.11 eNH-targeted non-invasive positive pressure ventilation (NPPV) also reduced COPD exacerbation.
Next, we analyzed whether COPD exacerbations were associated with overall sleep-related hypoventilation or only eNH, ie, REM sleep-related hypoventilation. Thereafter, we added more cases to our analyses and retrospectively analyzed overnight PtcCO2 monitoring data and the frequency of COPD exacerbations during the previous year. We also evaluated the relationship between the history of exacerbations and eNH or SH in patients with stable, severe, or very severe COPD with daytime PaCO2 <55 mmHg.
Materials and Methods
Patients
We enrolled consecutive patients diagnosed with stable, severe, or very severe COPD who were admitted to Kitano Hospital, Tazuke Kofukai Medical Research Institute, from April 2013 to January 2017 for the evaluation of respiratory failure with overnight PtcCO2 monitoring. All patients who met the following criteria were retrospectively reviewed: age ≥40 years; baseline daytime PaCO2 <55.0 mmHg; no abnormalities of the thorax or lung other than COPD; no medical history of obstructive sleep apnea (OSA) body mass index (BMI) <25 kg/m2; no malignant comorbidities within the past 5 years; and no severe heart failure (New York Heart Association stage 3–4). Patients were judged to be clinically stable if they had no exacerbation (lasting ≥2 days and requiring any change in pharmacological treatment) during the past 3 weeks.
Measurements and Data Collection
Sociodemographic, clinical, and laboratory data were extracted from medical records. The BMI was calculated as kg/m2. Pulmonary function tests were performed by trained operators in accordance with the guidelines of the American Thoracic Society and European Respiratory Society.15
Arterial blood gas was measured during the daytime in the supine position using a RAPIDLAB 1200 System (Siemens Healthcare Diagnostic Incorporated, USA). At sampling, all patients were breathing room air, with the exception of those on long-term oxygen therapy who used their prescribed dose of supplementary oxygen. Polysomnography (PSG) was performed using PSG-1100 (Nihon Kohden, Tokyo, Japan), and evaluated by sleep laboratory technicians.
Peak Nocturnal PtcCO2 and eNH
PtcCO2 monitoring was performed using a SenTec Digital Monitor (SenTec, Therwil, Switzerland) or a TOSCA TCM4 (Radiometer, Copenhagen, Denmark), which are reported to show small difference in PtcCO2.16,17 Data on PtcCO2 monitoring were evaluated by two board-certified members of the Japanese Respiratory Society with over 10 years of clinical practice. In the present study, eNH was defined as a continuous episodic increase of ≥5 mmHg from baseline PtcCO2 for ≥5 min, at least once during the night, according to the criteria of a previous study11 (Figure 1A). The PtcCO2 increase range was measured as the difference between the baseline PtcCO2 and peak PtcCO2 for each hypoventilation event (Figure 1B). Furthermore, all patients with eNH were evaluated using PSG to rule out complications of OSA and episodic PtcCO2 increases corresponding to REM sleep. The nocturnal mean PtcCO2 and maximum PtcCO2 were also collected from the overnight PtcCO2 monitoring data.
Evaluation of Sleep-Associated Hypoventilation
According to the American Society of Sleep Medicine (ASSM) scoring manual for the scoring of sleep and associated events, SH was defined as an event that met the following criteria during sleep: SH criterion (1), which was an increase in the PaCO2 (or PtcCO2) to a value >55 mmHg for ≥10 min; or SH criterion (2), which was a ≥ 10 mmHg increase in PaCO2 (or PtcCO2) during sleep (compared to the awake supine value) to a value exceeding 50 mmHg for ≥10 min.10 SH and eNH were judged by two board-certified members of the Japanese Respiratory Society with over 10 years of clinical experience.
Definition of COPD Exacerbation
COPD exacerbations were defined as acute worsening of respiratory symptoms that resulted in additional therapy.18 In this study, we retrospectively counted the frequency of moderate and severe exacerbations in the previous year. Moderate exacerbations were defined as events requiring short-acting bronchodilators plus antibiotics and/or oral corticosteroids.18 Severe exacerbations were defined as those requiring hospitalizations or visits to the emergency room.18
Ethics and Statistics
The study was carried out in accordance with the ethical guidelines of the Japanese Ministry of Health, Labor, and Welfare and was approved by the Institutional Review Board of the Kitano Hospital Medical Research Institute Ethics Committee (ethics board approval number: P210101300). In addition, we focused on the protection of personal information based on ethical guidelines. Prior comprehensive written informed consent for the use of patients’ data for research purposes was obtained from the patients at their first visit to our hospital. Moreover, our hospital’s website stated that the study patients were free to opt out of the study. The study conforms to the Declaration of Helsinki. We examined the normality of our data using the Shapiro–Wilk test. Parametric data were presented as mean ± standard deviation and nonparametric data as median (interquartile range [IQR]). Data were expressed as odds ratios (ORs) with corresponding 95% confidence intervals (CIs). For all analyses, a p-value <0.05 was considered statistically significant. Data analyses were conducted using SPSS version 25 (IBM Corp., Armonk, NY, USA).
Results
Figure 2 shows the patient selection flowchart for this study. Finally, 24 patients with COPD (19 men and five women) met the inclusion criteria. Table 1 shows patient characteristics. Patients had a mean age of 73.5 (64.5–78.8) years and a very severe airflow limitation, with a mean FEV1 of 28.8 ± 10.4%. Supplemental oxygen was used in four patients. Daytime PaO2, PaCO2, and bicarbonate levels were 72.0 ± 9.5 mmHg, 43.3 ± 6.8 mmHg, and 29.3 ± 4.2 mmol/L, respectively. The modified Medical Research Council (mMRC) and COPD assessment test scores were 2.9 ± 0.6 and 22.4 ± 9.6 points, respectively.
 |
Table 1 Patient Characteristics |
COPD Exacerbation
Figure 3 shows the frequency distribution chart of COPD exacerbations in the analyzed population. The median frequency of COPD exacerbations was 1 (0–2.0) times/year. Although eight out of 24 (33.3%) patients were not diagnosed with COPD exacerbation during the previous year, eight (33.3%) patients developed COPD exacerbation ≥2 times during the previous year.
 |
Figure 3 Frequency distribution chart of exacerbations in the analyzed population. Abbreviation: COPD, chronic obstructive pulmonary disease. |
Overnight PtcCO2 and PaCO2 Analysis
Twenty-three patients were evaluated by Sentec and only one was evaluated by TOSCA. The nocturnal maximum PtcCO2, mean PtcCO2, and PtcCO2 increase was 48.6 ± 9.5 mmHg, 42.9 ± 9.2 mmHg, and 5.1 ± 3.3 mmHg, respectively (Table 1).
Of the 24 analyzed patients, six (25.0%) patients met the SH criteria, four patients met only SH criterion (1), one patient met only SH criterion (2), and one patient met SH criteria (1) and (2). Daytime PaCO2, bicarbonate level, nocturnal maximum PtcCO2, mean PtcCO2, and PtcCO2 increases were significantly higher range in patients with SH than in patients without SH (Table 2). On the other hand, there was no significant difference in daytime PaO2 between patients with SH and patients without SH (Table 2).
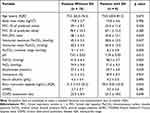 |
Table 2 Characteristics of Patients with and without Sleep-Associated Hypoventilation |
Of the 24 analyzed patients, 11 (45.9%) patients met the eNH criteria. Daytime PaCO2, bicarbonate levels, and PtcCO2 increases were significantly higher in patients with eNH than those without eNH (Table 3). There was no significant difference in daytime PaO2, nocturnal maximum PtcCO2, or mean PtcCO2 in patients with and without eNH (Table 3). In the PSG analysis of the patients with eNH, the mean total sleep time and sleep efficiency were 308 ± 80.7 min and 61.6 ± 15.5 min, respectively. REM sleep time accounted for 17.1 ± 6.0% of the sleep period. The apnea hypopnea index, central apnea index, and OSA index were 16.8 ± 8.0 episodes/h, 0.2 ± 0.3 episodes/h, and 1.6 ± 2.4 episodes/h, respectively. Most hypopneas were associated with alveolar hypoventilation during REM sleep.
 |
Table 3 Characteristics of Patients with and without Episodic Nocturnal Hypercapnia |
SH and COPD Exacerbation Relationship
The median frequency of COPD exacerbation was 1.0 (1.0–1.3) times/year in patients with SH. Table 4 represents the sensitivity, specificity, and OR of SH for a history of exacerbation. The OR of SH did not reach statistical significance.
The median frequency of COPD exacerbation was 1.0 (0–1.5) times/year in patients with SH criterion (1) and 1.0 (1.0–1.0) times/year in patients with SH criterion (2). Table 5 represents the sensitivity, specificity, and OR of SH criterion (1) or criterion (2) for a history of exacerbation. The OR of SH criterion (1) or criterion (2) did not reach statistical significance.
 |
Table 5 Sensitivity, Specificity, and Odds Ratio Values of Sleep-Associated Hypoventilation Criterion (1) and (2) for the Prediction of Chronic Obstructive Pulmonary Disease Exacerbations |
eNH and COPD Exacerbation History
The median frequency of COPD exacerbation was 2.0 (1.0–4.0) times/year in patients with eNH. Table 4 represents the sensitivity, specificity, and OR of eNH for a history of exacerbation. The OR of eNH reached statistical significance, with an OR of 11.1 [95% CI: 1.39–87.7] for at least one annual exacerbation and an OR of 6.6 [95% CI: 1.06–39.4] for two or more exacerbations per year.
Discussion
We have shown that eNH measured by overnight PtcCO2 is associated with a history of COPD exacerbations in the last year in patients with advanced COPD with baseline daytime PaCO2 <55.0 mmHg. Furthermore, eNH was more sensitive than SH in relation to the history of COPD exacerbation, while the specificity of eNH was similar to that of SH. There were no significant differences in daytime physiological parameters, excluding pH, daytime PaCO2, and bicarbonate levels, with or without eNH or SH (Tables 2 and 3).
The results of this study suggest that eNH, but not SH, is related to COPD exacerbation. The most important difference between SH and eNH is that eNH is exclusively focused on nocturnal episodic PtcCO2 increases, which corresponds to REM-related hypoventilation, as confirmed by PSG.11 This indicates that COPD exacerbations are closely associated with REM-related hypoventilation detected as eNH.
On the other hand, SH does not always correspond to episodic PtcCO2 increases, but also sustained hypercapnia during the night. The SH criterion (1) was defined as an increase in the arterial PaCO2 (or PtcCO2) to a value >55 mmHg for ≥10 min during sleep. Therefore, the SH criterion (1) theoretically includes not only REM-related hypoventilation but also hypoventilation during non-REM sleep. Therefore, for detection of REM-related hypoventilation, the sensitivity of eNH is better than that of SH.
In addition, the absolute value of PaCO2 is included in the SH criterion (1), although it is not easy to continuously measure PaCO2 in clinical practice.19 We used PtcCO2 as a surrogate marker for PaCO2 to evaluate sleep-related disorders in patients with chronic respiratory failure.19,20 However, the average difference between PaCO2 and PtCO2 is reported to be 4.6–6.1 mmHg,19,20 and changes in PtcCO2 are reportedly more reliable than the absolute values of PtcCO2.19,20 In the present study, in patients with SH, five out of six patients (83.3%) met the SH criterion (1), which depends on the uncertain absolute values of PtcCO2. Therefore, eNH could be a more reliable marker than SH because it focuses only on the change in PtcCO2 and not the absolute values of PtcCO2.
The SH criterion (2) was defined as a ≥ 10 mmHg increase in PtcCO2 during sleep (in comparison to an awake supine value) to a value exceeding 50 mmHg for ≥10 min. Therefore, SH criterion (2) focuses on the change in PtcCO2 and may be useful for specifically detecting REM-related hypoventilation, similar to eNH. In patients with a history of at least one exacerbation, the specificities of the SH criterion (2) and eNH were 94.1% and 87.5%, respectively. However, the sensitivity of the SH criterion (2) (12.5%) was lower than that of eNH (62.5%). In the SH criterion (2), the PtcCO2 increase of ≥10 mmHg during sleep seemed to be too high as a cut-off value for detecting REM-related hypoventilation. Eleven patients met the eNH criteria, but only two patients met the SH criterion (2) in the present study. In patients with COPD (average ratio of FEV1 to forced vital capacity was 42%), PaCO2 during the awake state, stage 2, stage 3–4, and REM sleep were reported 49.7 ± 1.59 mmHg, 53.4 ± 1.52 mmHg, 54.5 ± 1.94 mmHg, and 57.4 ± 1.71 mmHg, respectively.21 Namely, it is uncommon for PtcCO2 to increase to ≥10 mmHg during REM sleep.21 In contrast, the sensitivity was improved by the eNH criteria (PtcCO2 increase ≥ 5 mmHg) in the present study. Changing the criteria for PtcCO2 increase from ≥10 mmHg to ≥5 mmHg seemed to improve the sensitivity associated with a history of COPD exacerbation.
The reason why REM sleep-related hypoventilation is associated with exacerbation of COPD can be explained as follows. During REM sleep, respiratory activity relies almost exclusively on the diaphragm, whereas the activity of the intercostal and accessory muscles ceases.22 In patients with advanced COPD, the diaphragm flattens as pulmonary hyperinflation,23 causing inefficient contraction of the diaphragm, resulting in marked alveolar hypoventilation and episodic nocturnal hypercapnia during REM sleep. Surges in PaCO2 accompanied by episodic hypoventilation may have an important impact on pulmonary artery pressure, since even short-duration hypercapnia may cause pulmonary vasoconstriction,24 and respiratory acidosis also causes pulmonary artery hypertension, regardless of hypoxic pulmonary vasoconstriction.24 Repetition of episodic nocturnal hypoventilation and hypercapnia may result in permanent pulmonary hypertension (PH). In our previous study, COPD patients with eNH had significantly higher estimated pulmonary artery systolic pressure (47.0 ± 4.8 mmHg vs 33.6 ± 2.6 mmHg, p = 0.037) and pulmonary artery: aorta ratio (0.96 ± 0.05 vs 0.79 ± 0.03, p = 0.019) than those without eNH.11 REM-related hypoventilation with eNH may lead to PH. Namely, the patient group with eNH may be a subgroup with a high likelihood of pulmonary hypertension, including the patients with baseline daytime PaCO2 <55.0 mmHg. Pulmonary artery hypertension is known to be associated with COPD exacerbation and mortality.25 This hypothesis should be further verified by prospective large-scale studies with overnight PtcCO2 monitoring.
Fletcher et al proposed episodic nocturnal desaturation criteria (the patient’s SaO2 falls below a baseline of 90% for 5 ≥ min) to focus on episodic hypoventilation mainly during REM sleep and showed that patients with COPD based on Fletcher’s desaturation criteria had poor survival prognosis.26,27 However, we believe that evaluation by overnight PtcCO2 monitoring is more important than that by SpO2 monitoring. This is because hypoventilation may be overlooked as SpO2 is affected by oxygen therapy. In addition, episodic nocturnal desaturation may be misidentified as desaturation due to REM-related hypoventilation owing to its similarity to desaturation due to exertion, such as night urination, which is not always reported by the patient.
There is not enough evidence for the usefulness of long-term NPPV in COPD patients without marked elevation in daytime PaCO2. However, we previously demonstrated that eNH-targeted NPPV resulted in a significant decrease in daytime PaCO2 and COPD exacerbation frequency in COPD patients with daytime PaCO2 <55 mmHg.11 In the near future, nocturnal PtcCO2 monitoring could be a useful measure to detect frequent exacerbations among advanced COPD patients without marked daytime alveolar hypoventilation. Furthermore, we could select a more appropriate patient with daytime PaCO2 <55 mmHg for long-term NPPV therapy, resulting in a decreased frequency of COPD exacerbation.
The present study had some limitations. First, this study enrolled a relatively small number of patients with stable advanced COPD and daytime PaCO2 <55 mmHg in a single general hospital. However, to the best of our knowledge, this is the first report to compare the significance of eNH with SH in terms of the history of COPD exacerbations. Our findings may lead to new approaches for the detection of subgroups with frequent COPD exacerbations. Second, although we showed that eNH was associated with a history of COPD exacerbations, it remains unclear whether the presence of eNH can predict future exacerbations. A prospective study is needed to validate the relationship between eNH and COPD exacerbation. However, it is not easy to adjust the influence of treatment such as NPPV. Patients with COPD with eNH met the indication criteria of NPPV for stable COPD in Japanese Respiratory Society’s NPPV guidelines.28 Therefore, we treated the patients with eNH with NPPV in clinical practice, and eNH targeted NPPV reduced the frequency of exacerbations.11 Third, we could not correctly evaluate the history of mild COPD exacerbation. This is because we retrospectively counted the frequency of exacerbations from the medical records. Although we demonstrated the importance of eNH in moderate or severe COPD exacerbations, additional prospective studies are required to confirm our findings. Fourth, six of 24 patients could not be evaluated using polysomnography. We might not have completely excluded patients with OSA from the present study. However, we excluded patients with a history of OSA or BMI ≥ 25 kg/m2, and the mean BMI was 19.5 ± 3.7 kg/m2 in the present study. Moreover, the nocturnal continuous monitoring of SpO2 showed that the 3% and 4% oxygen desaturation indexes were 7.3 ± 3.8 episodes/h and 4.4 ± 3.3 episodes/h, respectively, in patients without polysomnography evaluation. All patients with eNH were evaluated using PSG, as described above. Our study showed that patients with COPD with low BMI are common in Japan.29 On the other hand, we should pay attention to apply the results of our study to patients of COPD in the west with high BMI.
Conclusion
In conclusion, we focused on the association between a history of COPD exacerbations and eNH in patients with advanced COPD and daytime PaCO2 <55 mmHg. eNH may be a better biomarker than SH defined by ASSM for detecting subgroups with frequent COPD exacerbations. Our research was a small observational study, and further studies are required to evaluate our findings.
Abbreviations
AASM, American Academy of Sleep Medicine; PaCO2, arterial carbon dioxide pressure; BMI, body mass index; COPD, chronic obstructive pulmonary disease; eNH, episodic nocturnal hypercapnia; mMRC, modified Medical Research Council; NPPV, non-invasive positive pressure ventilation; OSA, obstructive sleep apnea; PSG, polysomnography; PH, pulmonary hypertension; REM, rapid eye movement; SH, sleep-associated hypoventilation; PtcCO2, transcutaneous carbon dioxide pressure.
Acknowledgments
We thank Editage for English language editing.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval for the version to be published; and agreed to be accountable for all aspects of the work.
Disclosure
Dr Hisanori Amimoto reports personal fees from AstraZeneca, personal fees from CHUGAI PHARMACEUTICAL CO., LTD., personal fees from TAIHO PHARMACEUTICAL CO., LTD., during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/S0140-6736(12)61728-0
2. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J. 2017;49(3):1700214. doi:10.1183/13993003.00214-2017
3. Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418–1422. doi:10.1164/ajrccm.157.5.9709032
4. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931. doi:10.1136/thx.2005.040527
5. Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. doi:10.1056/NEJMoa0909883
6. Yang H, Xiang P, Zhang E, et al. Is hypercapnia associated with poor prognosis in chronic obstructive pulmonary disease? A long-term follow-up cohort study. BMJ Open. 2015;5(12):e008909. doi:10.1136/bmjopen-2015-008909
7. Almagro P, Barreiro B, Ochoa de Echaguen A, et al. Risk factors for hospital readmission in patients with chronic obstructive pulmonary disease. Respiration. 2006;73(3):311–317. doi:10.1159/000088092
8. Kessler R, Faller M, Fourgaut G, Mennecier B, Weitzenblum E. Predictive factors of hospitalization for acute exacerbation in a series of 64 patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;159(1):158–164. doi:10.1164/ajrccm.159.1.9803117
9. Böing S, Randerath WJ. Chronic hypoventilation syndromes and sleep-related hypoventilation. J Thorac Dis. 2015;7(8):1273–1285. doi:10.3978/j.issn.2072-1439.2015.06.10
10. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated Events. Deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597–619. doi:10.5664/jcsm.2172
11. Kitajima T, Marumo S, Shima H, et al. Clinical impact of episodic nocturnal hypercapnia and its treatment with noninvasive positive pressure ventilation in patients with stable advanced COPD. Int J Chron Obstruct Pulm Dis. 2018;13:843–853. doi:10.2147/COPD.S153200
12. O’Donoghue FJ, Catcheside PG, Ellis EE, et al. Sleep hypoventilation in hypercapnic chronic obstructive pulmonary disease: prevalence and associated factors. Eur Respir J. 2003;21(6):977–984. doi:10.1183/09031936.03.00066802
13. Marrone O, Salvaggio A, Insalaco G. Respiratory disorders during sleep in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulm Dis. 2006;1(4):363–372. doi:10.2147/copd.2006.1.4.363
14. Collop NA, Salas RE, Delayo M, Gamaldo C. Normal sleep and circadian processes. Crit Care Clin. 2008;24(3):449–460. doi:10.1016/j.ccc.2008.02.002
15. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
16. Bolliger D, Steiner LA, Kasper J, Aziz OA, Filipovic M, Seeberger MD. The accuracy of non-invasive carbon dioxide monitoring: a clinical evaluation of two transcutaneous systems. Anaesthesia. 2007;62(4):394–399. doi:10.1111/j.1365-2044.2007.04987.x
17. Storre JH, Magnet FS, Dreher M, Windisch W. Transcutaneous monitoring as a replacement for arterial PCO(2) monitoring during nocturnal non-invasive ventilation. Respir Med. 2011;105(1):143–150. doi:10.1016/j.rmed.2010.10.007
18. Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi:10.1016/S0140-6736(07)61382-8
19. Storre JH, Steurer B, Kabitz HJ, Dreher M, Windisch W. Transcutaneous PCO2 monitoring during initiation of noninvasive ventilation. Chest. 2007;132(6):1810–1816. doi:10.1378/chest.07-1173
20. Kelly AM, Klim S. Agreement between arterial and transcutaneous PCO2 in patients undergoing non-invasive ventilation. Respir Med. 2011;105(2):226–229. doi:10.1016/j.rmed.2010.11.010
21. Coccagna G, Lugaresi E. Arterial blood gases and pulmonary and systemic arterial pressure during sleep in chronic obstructive pulmonary disease. Sleep. 1978;1(2):117–124. doi:10.1093/sleep/1.2.117
22. Tabachnik E, Muller NL, Bryan AC, Levison H. Changes in ventilation and chest wall mechanics during sleep in normal adolescents. J Appl Physiol Respir Environ Exerc Physiol. 1981;51(3):557–564. doi:10.1152/jappl.1981.51.3.557
23. Ballard RD, Clover CW, Suh BY. Influence of sleep on respiratory function in emphysema. Am J Respir Crit Care Med. 1995;151(4):945–951. doi:10.1164/ajrccm.151.4.7697271
24. Dorrington KL, Balanos GM, Talbot NP, Robbins PA. Extent to which pulmonary vascular responses to PCO2 and PO2 play a functional role within the healthy human lung. J Appl Physiol. 2010;108(5):1084–1096. doi:10.1152/japplphysiol.90963.2008
25. Wells JM, Washko GR, Han MK, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367(10):913–921. doi:10.1056/NEJMoa1203830
26. Fletcher EC, Miller J, Divine GW, Fletcher JG, Miller T. Nocturnal oxyhemoglobin desaturation in COPD patients with arterial oxygen tensions above 60 mm Hg. Chest. 1987;92(4):604–608. doi:10.1378/chest.92.4.604
27. Fletcher EC, Donner CF, Midgren B, et al. Survival in COPD patients with a daytime PaO2 greater than 60 mm Hg with and without nocturnal oxyhemoglobin desaturation. Chest. 1992;101(3):649–655. doi:10.1378/chest.101.3.649
28. Akashiba T, Ishikawa Y, Ishihara H, et al. The Japanese Respiratory Society noninvasive positive pressure ventilation (NPPV) Guidelines (second revised edition). Respir Investig. 2017;55(1):83–92. doi:10.1016/j.resinv.2015.11.007
29. Tsuboi T, Oga T, Machida K, et al. PaCO2 six months after the initiation of long-term noninvasive ventilation in patients with COPD. Intern Med. 2011;50(6):563–570. doi:10.2169/internalmedicine.50.4310
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



