Back to Journals » Infection and Drug Resistance » Volume 16
Refractory Palmoplantar Pustulosis Successfully Treated with JAK Inhibitor Tofacitinib: A Case Series
Authors Xu Q , Wang X, Yang A, Wei G
Received 9 June 2023
Accepted for publication 1 August 2023
Published 9 August 2023 Volume 2023:16 Pages 5165—5172
DOI https://doi.org/10.2147/IDR.S421299
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Qingqing Xu,1 Xiaochen Wang,2 Anbo Yang,3 Guo Wei1
1Department of Dermato-Venereology, the Second Hospital of Shandong University, Jinan, 250033, People’s Republic of China; 2Clinical Laboratory of Qingdao Municipal Hospital, Qingdao, 266000, People’s Republic of China; 3Department of Dermato-Venereology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, 250021, People’s Republic of China
Correspondence: Anbo Yang; Guo Wei, Email [email protected]; [email protected]
Background: Palmoplantar pustulosis (PPP) is a common chronic and recurrent skin disease of the palms and soles with significant pain, mental distress, and functional disability. PPP is challenging to treat and usually requires prolonged management. Therapy resistance and frequent relapse discourages patients from follow-up. No unified standard and no published therapeutic guidelines have yet been defined on PPP treatment. In general, all therapeutic options known for autoimmune diseases, psoriasis in particular, have been tested in PPP. Tofacitinib, an oral JAK inhibitor, has been approved for the treatment of rheumatoid arthritis and shows promise in the treatment of moderate-to-severe plaque psoriasis. However, no clinical trials or case reports have been conducted to confirm the efficacy of tofacitinib in palmoplantar pustulosis.
Methods: Six in total with 6 PPP patient, aged 42– 58 years were recruited according to the inclusion and exclusion criteria. Patient characteristics, including triggering factors, concomitant diseases, and previous therapeutic drugs, were investigated. All patients experienced a lack of response to topical drugs and at least one systemic agent. During treatment, visits were scheduled at the start of treatment and at 2, 4, and 12 weeks, and efficacy was assessed using the PPP ASI and PPP PGA.
Results: Our six patients showed an excellent response to tofacitinib as all patients did achieve at least 50% reduction and half of our patients with more than 80% reduction in PPPASI after 4 weeks treatment; at week 12, 5 (83.3%) patients had 80% reduction in PPPASI with no serious adverse events were reported.
Conclusion: The JAK inhibitor tofacitinib is a promising treatment for refractory palmoplantar pustulosis that requires further clinical observation and research.
Keywords: refractory palmoplantar pustulosis, tofacitinib, palmoplantar pustular psoriasis area and severity index
Introduction
Palmoplantar pustulosis (PPP) is a common chronic and recurrent dermatosis characterized by aseptic pustules on the palms and soles, which often causes disproportionate pain, pruritus, and functional disability. The prevalence of PPP ranges from 0.01 to 0.05%.1 The mean patient age ranged from 40 to 58 years.2 Smoking is one of the important inducing factor2 in PPP, and tonsillar streptococcal3 or dental infections4 may exacerbate PPP. Other triggering factors, including dental metal allergies5 and some drugs, especially anti-TNF agents6 may induce or exacerbate PPP.
PPP usually occurs concomitantly with various other diseases. Autoimmune thyroid disease is often observed in PPP patients.7 Obesity (BMI > 25 mg/m2), T2DM, hyperlipidemia, allergic diseases (such as asthma, atopic dermatitis, and rhinitis allergica) and joint pain frequently accompanies PPP lesions.7,8
PPP is challenging to treat and usually requires prolonged management. Therapy resistance and frequent relapse discourage patients from follow-up. To date, no therapeutic standards or published guidelines have been defined for PPP treatment. In general, all known therapeutic options for autoimmune diseases, psoriasis in particular, have been tested in patients with PPP. Therapeutic recommendations for PPP are mainly based on case reports and dermatologist’ own long-term clinical experience. Topically potent glucocorticosteroids, retinoids, vitamin D derivatives, keratolytic agents and emollients are first-line agents for PPP treatment.9 In practice, however, refractory or severe PPP patients often require systemic therapy. Current systemic treatment options include retinoids, immunosuppressant (such as methotrexate, cyclosporine and mofetil) and biological agents that are approved for psoriasis Vulgaris.9
Janus kinases (JAKs) family consisting of 4 members: JAK1, JAK2, JAK3, and TYK, belongs to non-receptor tyrosine protein kinases. When cytokines (IL-6, IL-22, IL-23, or IFN-γ) bind to their receptors, JAKs are recruited to phosphorylate and activate STAT family proteins. Activated STAT proteins undergo dimerization and translocate into the nucleus to modulate gene expression.10 Dysregulation of the JAK/STAT pathway is associated with various autoimmune diseases. JAK inhibitors directly target Janus kinases to block JAK/STAT pathway to regulate the expression of inflammatory factors like IL-6, IL-17A, or IFN-γ.11 Currently, multiple JAK inhibitors are approved by FDA for skin diseases, like alopecia areata,12 atopic dermatitis13 and vitiligo.14 Also, JAK inhibitors are investigated as a new treatment for various skin diseases.15
This paper reports a series of six cases of refractory palmoplantar pustulosis treated with the JAK inhibitor tofacitinib, which quickly improve the severity of skin lesions, including erythema, aseptic pustules and desquamation. All our patients experienced a lack of response to at least one systemic agent.
Methods
Patients
Inclusion Criteria were as follows: We included patients aged 18–65 years who were diagnosed with palmoplantar pustulosis with active pustules (yellow pustules) for at least 1 year and a history of lack of response to at least one systemic agent.
The exclusion criteria were as follows: 1. palmoplantar pustulosis (ppp) with psoriasis vulgaris lesions; 2. palmoplantar pustulosis treated with systemic therapy <8 weeks and/or topical agents or phototherapy <2 weeks prior to the study; 3. active or latent Mycobacterium tuberculosis infection without inadequate treatment; and 4. evidence of hepatitis B/C or HIV infection, disseminated or recurrent herpes zoster infection; 5. infections requiring hospitalization <3 months before the study; infections requiring oral or topical antibiotic <4 weeks before the study; 6. evidence of active or inadequately treated malignancies or lymphoproliferative disorders (except completely excised non-metastatic squamous cell skin cancer, basal cells, or cervical carcinoma) and 7. history of previous treatment with oral tofacitinib.
Study Design and Objectives
Before treatment, all patients were informed that tofacitinib was not specifically used for PPP treatment in the production instruction but was effective in treating moderate-to-severe plaque psoriasis with minimal adverse effects.16 Routine blood tests, liver and kidney function tests, virus series, T-spots, and tumor markers were screened to exclude contraindications.
During treatment, patients usually received tofacitinib at a dosage of 5 mg twice daily for 12 weeks. Visits were scheduled at the start of the treatment and at 2, 4, and 12 weeks. When patients achieved a physician’s Global Assessment of “clear” or “almost clear” (PGA response), tofacitinib was decreased to 5 mg once daily. During the study period, patients were forbidden to use immunosuppressants and other anti-inflammatory agents such as ibuprofen. The medication will be terminated once patients show adverse events, such as vital signs, abnormalities in laboratory indexes, confirmed malignancies, physical examinations, blood pressure abnormalities, pulse abnormalities, electrocardiogram (ECG) abnormalities, and judgemental cardiovascular problems. All patients signed informed consent prior to the study.
Efficacy was assessed using the Palmoplantar Pustular Psoriasis Area and Severity Index (PPP ASI) and the Palmoplantar Pustulosis Physician Global Assessment (PPP PGA). The achievement of a response in PPP ASI and PPP PGA from the baseline was assessed in this study. The PPP ASI is calculated as a weighted sum of the scores obtained for erythema (E), pustules (P), desquamation (D), and percent of body surface area affected (Table S1): PPPASI = [(E+P+D) × A × 0.2 (right palm)] + [(E+P+D) × A × 0.2 (left palm)] + [(E+P+D) × A × 0.3 (right sole)] + [(E+P+D) × A × 0.3 (left sole)]. PPP PGA was graded on a scale of 0 to 4 based on skin lesion, with 0/1 indicating clear/almost clear skin and 4 indicating very severe lesions (Table S2). Ethical approval was obtained from the Ethics Committee of the Second Hospital of Shandong University (KYLL-2021 [KJ]P-0358). The study was complied with the Declaration of Helsinki.
Result
Our study included six patients, including four men and two women, aged 42–58 years. Disease duration ranged from 2 to 9 years. The body mass index ranged from 23.6 to 34.6. The details of the patients are summarized in Table 1. The average age of our patients was 49.8 ± 6.4 years. The mean age at disease was 45.2 ± 7.9 years, and the mean disease was 4.8 ± 2.6 years. Among these six patients, three had a history of smoking, four frequently consumed alcohol, and one had tonsil infections. All these patients had concomitant diseases: Patient 1 suffered from obesity, hyperlipidemia, and urticaria; Patient 2 suffered from Obesity, T2DM, and atopic dermatitis; Patients 3 and 5 only suffered from obesity; Patient 4 suffered from obesity, T2DM, urticaria, and rhinitis allergica; and Patient 6 suffered from hyperlipidemia and joint pain. All patients experienced a lack of response to topical agents and at least one systemic agent. All patients received systemic retinoids, two received methotrexate, two received Cyclosporine and 1 patient have Mycophenolate mofetil without biological agents.
 |
Table 1 Characteristics of Patients with Palmoplantar Pustulosis (PPP) Treated with Tofacitinib |
At the start of the treatment, PPP ASI ranged from 14.2 to 30.4 (Table 2). We noticed a rapid onset of tofacitinib, evidenced by almost complete clearance of PPP lesions without visible active pustules (Figures 1 and 2) within 2–4 weeks in three of our patients, with more than 80% reduction in PPPASI. Another 3 patients had a 50–75% reduction in PPPASI at 4 weeks visit, and further improvement was observed after that. At week 12, three of our patients had more than 90% reduction in PPPASI, two patients had 80–85% reduction, and only one patient had less than 75% reduction in PPPASI. After 12 weeks, the tofacitinib dose was decreased to 5 mg once daily in five patients with a PGA score of 0/1, and the original dosage was maintained in the remaining patient for 4 weeks. Above all, our six patients showed an excellent response to tofacitinib, as all six patients achieved a 50% reduction and 3 patients had more than 80% reduction in PPPASI within 4 weeks of treatment, and at week 12, 5 (83.3%) patients had an 80% reduction in PPPASI. During the 12-week medication period, no serious adverse events, such as vital infections, malignancies, or abnormalities in laboratory safety data, were reported.
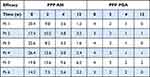 |
Table 2 The Change of PPP ASI and PPP PGA in All 6 Patients at 0, 2, 4, and 12 Weeks After Tofacitinib Treatment |
 |
Figure 1 Clinical images of patient 1 at 0, 2, 4, and 12 weeks after tofacitinib treatment. |
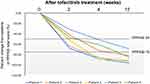 |
Figure 2 Percent change from baseline in PPP ASI over time in all 6 patients. |
Discussion
The pathogenesis of palmoplantar pustulosis is complex. In addition to the genetic background and microbiome, both interleukin (IL)-17 pathway and IL-36 pathway (with IL-8 overexpression) play a significant role in PPP pathogenesis.9 Some consider PPP to be a localized form or acral variant of pustular psoriasis, whereas others regard PPP as a nosological entity distinct from psoriasis.17–19 However, PPP is closely linked to psoriasis, and clinical studies have been conducted to evaluate the effectiveness of biological therapies which have been approved for psoriasis or psoriatic arthritis in PPP treatment.20 In a multicenter, randomized, double-blind clinical study involving over 200 PPP patients, 300 mg and 150 mg secukinumab (IL‑17 inhibitors) were compared with placebo for PPP treatment. At week 52, only 41.8% of patients receiving 300 mg secukinumab treatment achieved PPPASI 75.21 Compared with placebo, the IL-12/23 p40 antagonist ustekinumab displayed weak clinical efficacy in treating PPP.22 The efficacy of IL-23/IL-17 targeted therapies in PPP is weaker than that in psoriasis vulgaris. In addition to blockade of the IL-23/IL-17 pathway, the biological treatment focuses on blocking the IL-8 or IL-36 pathways have been investigated. In an open-label multicenter trial involving 31 PPP patients with a single-dose and dose-escalation administration, the anti-IL-8 monoclonal antibody HuMab 10F8, which effectively blocks IL-8-dependent neutrophil activation and migration,16 was evaluated for the treatment of PPP.23 About 37% of the patients at week 4 and 61% of the participants at week 8 had a clinical response with at least a 50% reduction in the number of active pustules. Furthermore, all seven patients receiving high-dose HuMab 10F8 showed more than 50% reduction in the number of active pustules, and four patients had a 75% reduction from baseline at week 8. In a IIa phase, multicenter, double-blind, randomized, placebo-controlled clinical trial, anti-IL-36R monoclonal antibody spesolimab 900 mg and 300 mg were compared with placebo by intravenous administration per 4 weeks until week 12 for the treatment of PPP. At week 16, only 31.6% of subjects receiving 900 mg or 300 mg spesolimab achieved PPP ASI 50 versus 23.8% of subjects receiving placebo treatment (p = 0.338), with good tolerance but limited efficacy.24 The efficacy of the above biological treatments for palmoplantar pustulosis is less than satisfactory, and new effective methods are still being explored.
Tofacitinib inhibits JAK signaling in the form of homodimers or heterodimeric receptors, with the repression of JAK1/JAK3 being the best, followed by JAK1 or JAK3 paired with JAK2, and JAK2/JAK2 being the worst. These receptors inhibition blocks IL‐2, IL‐4, IL‐7, IL‐9, IL‐13, IL‐15 and IL‐21 signal transduction25 which are integral to lymphocyte function and adaptive immune response. The therapeutic potential of the JAK inhibitor tofacitinib in dermatological conditions such as alopecia areata,26 psoriasis, atopic dermatitis,27 vitiligo,28 and dermatomyositis has shown promising results in clinical trials that are well tolerated. Common adverse effects include increased risk of infection and thromboembolic events. Tofacitinib has been approved for psoriatic arthritis by the FDA and EMA and shows promise for treating moderate-to-severe plaque psoriasis. However, the FDA has declined approval for psoriasis due to issues of clinical efficacy and long-term safety. In a long-term safety analysis of tofacitinib up to 9.5 years in rheumatoid arthritis patients, tofacitinib 5 and 10 mg twice daily showed similar safety except an increased risk of infection (eg, herpes zoster), compared with anti-rheumatic biological drugs and other JAK inhibitors.29
In this clinical observation, tofacitinib, a pan-JAK inhibitor, was evaluated in refractory PPP treatment, not selective JAK inhibitors like upadacitinib or other biologic, mainly because of the price. The cost of tofacitinib during the treatment period per 4 weeks is 110 RMB, while upadacitinib or IL-17 inhibitors needs more than 2000 RMB. In the current clinical results, we showed that tofacitinib 5mg twice daily could quickly improve the signs and symptoms of refractory PPP without serious adverse events including infection during the treatment period. Therefore, we believe that tofacitinib may be an effective treatment option for refractory disease, but the condition of decreasing dosage (equal to or less than once daily) or stopping medication still require further follow-up, also long-term efficacy and safety of tofacitinib compared with traditional systemic immunosuppressants or biologics in PPP treatment need to be evaluated.
Consent for Publication
Informed consent has been signed by the patients to publish the case details and relational images.
Acknowledgments
This study was supported by the Natural Science Foundation of Shandong Province (Grant No. ZR2020QH195).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors declare that there are no conflicts of interest in this work.
References
1. Mrowietz U, van de Kerkhof PC. Management of palmoplantar pustulosis: do we need to change? Br J Dermatol. 2011;164(5):942–946. doi:10.1111/j.1365-2133.2011.10233.x
2. Misiak-Galazka M, Wolska H, Galazka A, Kwiek B, Rudnicka L. General characteristics and comorbidities in patients with palmoplantar pustulosis. Acta Dermatovenerologica Croatica: ADC. 2018;26(2):109–118.
3. Nozawa H, Kishibe K, Takahara M, Harabuchi Y. Expression of cutaneous lymphocyte-associated antigen (CLA) in tonsillar T-cells and its induction by in vitro stimulation with alpha-streptococci in patients with pustulosis palmaris et plantaris (PPP). Clin Immunol. 2005;116(1):42–53. doi:10.1016/j.clim.2005.01.009
4. Kouno M, Nishiyama A, Minabe M, et al. Retrospective analysis of the clinical response of palmoplantar pustulosis after dental infection control and dental metal removal. J Dermatol. 2017;44(6):695–698. doi:10.1111/1346-8138.13751
5. Kato M, Oiso N, Yanagihara S, Kawada A. Long-lasting allergic patch test reactions to dental metal allergens in a patient with palmoplantar pustulosis and pustulotic arthro-osteitis. J Dermatol. 2020;47(9):e324–e5. doi:10.1111/1346-8138.15471
6. Bae JM, Lee HH, Lee BI, et al. Incidence of psoriasiform diseases secondary to tumour necrosis factor antagonists in patients with inflammatory bowel disease: a nationwide population-based cohort study. Aliment Pharmacol Ther. 2018;48(2):196–205. doi:10.1111/apt.14822
7. Atas H, Gonul M. Insulin resistance, diabetes mellitus and thyroid dysfunction in patients with palmoplantar pustulosis: a case-controlled study. Postepy Dermatol Alergol. 2017;34(3):268–272. doi:10.5114/pdia.2016.61630
8. Trattner H, Bluml S, Steiner I, Plut U, Radakovic S, Tanew A. Quality of life and comorbidities in palmoplantar pustulosis - a cross-sectional study on 102 patients. J Eur Acad Dermatol Venereol. 2017;31(10):1681–1685. doi:10.1111/jdv.14187
9. Misiak-Galazka M, Zozula J, Rudnicka L. Palmoplantar Pustulosis: recent Advances in Etiopathogenesis and Emerging Treatments. Am J Clin Dermatol. 2020;21(3):355–370. doi:10.1007/s40257-020-00503-5
10. O’Shea JJ, Schwartz DM, Villarino AV, Gadina M, McInnes IB, Laurence A. The JAK-STAT pathway: impact on human disease and therapeutic intervention. Annu Rev Med. 2015;66:311–328. doi:10.1146/annurev-med-051113-024537
11. Hu X, Li J, Fu M, Zhao X, Wang W. The JAK/STAT signaling pathway: from bench to clinic. Signal Transduct Target Ther. 2021;6(1):402. doi:10.1038/s41392-021-00791-1
12. Lensing M, Jabbari A. An overview of JAK/STAT pathways and JAK inhibition in alopecia areata. Front Immunol. 2022;13:955035. doi:10.3389/fimmu.2022.955035
13. Nakashima C, Yanagihara S, Otsuka A. Innovation in the treatment of atopic dermatitis: emerging topical and oral Janus kinase inhibitors. Allergol Int. 2022;71(1):40–46. doi:10.1016/j.alit.2021.10.004
14. Cunningham KN, Rosmarin D. Vitiligo Treatments: review of Current Therapeutic Modalities and JAK Inhibitors. Am J Clin Dermatol. 2023;24(2):165–186. doi:10.1007/s40257-022-00752-6
15. Solimani F, Meier K, Ghoreschi K. Emerging Topical and Systemic JAK Inhibitors in Dermatology. Front Immunol. 2019;10:2847. doi:10.3389/fimmu.2019.02847
16. Valenzuela F, Korman NJ, Bissonnette R, et al. Tofacitinib in patients with moderate-to-severe chronic plaque psoriasis: long-term safety and efficacy in an open-label extension study. Br J Dermatol. 2018;179(4):853–862. doi:10.1111/bjd.16798
17. Misiak-Galazka M, Wolska H, Rudnicka L. Is palmoplantar pustulosis simply a variant of psoriasis or a distinct entity? J Eur Acad Dermatol Venereol. 2017;31(7):e342–e3. doi:10.1111/jdv.14136
18. Brunasso AMG, Massone C. Psoriasis and palmoplantar pustulosis: an endless debate? J Eur Acad Dermatol Venereol. 2017;31(7):e335–e7. doi:10.1111/jdv.14131
19. Brunasso AM, Massone C. Can we really separate palmoplantar pustulosis from psoriasis? J Eur Acad Dermatol Venereol. 2010;24(5):619–621. doi:10.1111/j.1468-3083.2010.03648.x
20. Sanchez IM, Sorenson E, Levin E, Liao W. The Efficacy of Biologic Therapy for the Management of Palmoplantar Psoriasis and Palmoplantar Pustulosis: a Systematic Review. Dermatol Ther (Heidelb). 2017;7(4):425–446. doi:10.1007/s13555-017-0207-0
21. Mrowietz U, Bachelez H, Burden AD, et al. Secukinumab for moderate-to-severe palmoplantar pustular psoriasis: results of the 2PRECISE study. J Am Acad Dermatol. 2019;80(5):1344–1352. doi:10.1016/j.jaad.2019.01.066
22. Bissonnette R, Nigen S, Langley RG, et al. Increased expression of IL-17A and limited involvement of IL-23 in patients with palmo-plantar (PP) pustular psoriasis or PP pustulosis; results from a randomised controlled trial. J Eur Acad Dermatol Venereol. 2014;28(10):1298–1305. doi:10.1111/jdv.12272
23. Skov L, Beurskens FJ, Zachariae CO, et al. IL-8 as antibody therapeutic target in inflammatory diseases: reduction of clinical activity in palmoplantar pustulosis. J Immunol. 2008;181(1):669–679. doi:10.4049/jimmunol.181.1.669
24. Mrowietz U, Burden AD, Pinter A, et al. Spesolimab, an Anti-Interleukin-36 Receptor Antibody, in Patients with Palmoplantar Pustulosis: results of a Phase IIa, Multicenter, Double-Blind, Randomized, Placebo-Controlled Pilot Study. Dermatol Ther (Heidelb). 2021;11(2):571–585. doi:10.1007/s13555-021-00504-0
25. O’Shea JJ. Targeting the Jak/STAT pathway for immunosuppression. Ann Rheum Dis. 2004;63(Suppl 2):ii67–ii71. doi:10.1136/ard.2004.028290
26. Ibrahim O, Bayart CB, Hogan S, Piliang M, Bergfeld WF. Treatment of Alopecia Areata With Tofacitinib. JAMA Dermatol. 2017;153(6):600–602. doi:10.1001/jamadermatol.2017.0001
27. Szalus K, Trzeciak M, Nowicki RJ. JAK-STAT Inhibitors in Atopic Dermatitis from Pathogenesis to Clinical Trials Results. Microorganisms. 2020;8(11):1743. doi:10.3390/microorganisms8111743
28. Song H, Hu Z, Zhang S, Yang L, Liu Y, Wang T. Effectiveness and safety of tofacitinib combined with narrowband ultraviolet B phototherapy for patients with refractory vitiligo in real-world clinical practice. Dermatol Ther. 2022;35(11):e15821. doi:10.1111/dth.15821
29. Cohen SB, Tanaka Y, Mariette X, et al. Long-term safety of tofacitinib up to 9.5 years: a comprehensive integrated analysis of the rheumatoid arthritis clinical development programme. RMD Open. 2020;6(3):e001395. doi:10.1136/rmdopen-2020-001395
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
