Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 9 » Issue 1
Reduction of exacerbation frequency in patients with COPD after participation in a comprehensive pulmonary rehabilitation program
Authors van Ranst D , Stoop WA, Meijer J, Otten HJ, van de Port IG
Received 17 June 2014
Accepted for publication 31 July 2014
Published 3 October 2014 Volume 2014:9(1) Pages 1059—1067
DOI https://doi.org/10.2147/COPD.S69574
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
D van Ranst, WA Stoop, JW Meijer, HJ Otten, IG van de Port
Revant, Pulmonary Rehabilitation Center "Schoondonck," Breda, the Netherlands
Background: Pulmonary rehabilitation (PR) is an important treatment option for chronic obstructive pulmonary disease (COPD) patients and might contribute to a reduction in exacerbation and exacerbation-related hospitalization rate.
Methods: In this prospective study, all COPD patients that completed a comprehensive pulmonary rehabilitation program (PRP) between June 2006 and December 2012 were included. Self-reported exacerbation and hospitalization frequency 1 year before PR was retrospectively recorded. During the year following PR, exacerbation and hospitalization frequency was recorded with questionnaires.
Results: For 343 patients, complete information on exacerbation and hospitalization rate was obtained. The mean number of exacerbations decreased significantly after participating in a PRP by 1.37 exacerbations/year (95% confidence interval 1.029 to 1.717) from 4.56±3.26 exacerbations in the year preceding PR to 3.18±2.53 in the year following PR (P<0.0005). The number of hospitalizations due to exacerbations decreased significantly by 0.68 hospitalizations/year (95% confidence interval 0.467 to 0.903) from 1.48±1.84 in the year preceding PR to 0.80±1.31 hospitalizations/year in the year following PR (P<0.0005). The proportion of patients with a frequent exacerbation type (more than two exacerbations/year) was reduced by 24%. Multivariate regression analysis to explore determinants that might predict reduction in exacerbation frequency or change in exacerbation pattern did not reveal clinically useful predictors, although patients with more exacerbations before PR had the highest potential for reduction.
Conclusion: In a large population of severely impaired COPD patients with high exacerbation rates, a significant reduction in exacerbation and hospitalization frequency was observed after participation in a comprehensive PRP.
Keywords: health status, health care utilization, hospitalization, disease management, self-management
Introduction
Pulmonary rehabilitation (PR) has become an integral component in the treatment of chronic obstructive pulmonary disease (COPD) patients. The short-term effects on improving symptoms, exercise tolerance, and health-related quality of life (HRQoL)were demonstrated by numerous randomized studies and meta-analyses.1
This was confirmed by a recent study from our group, showing positive short-term results of a comprehensive PR program (PRP) in a large group of COPD patients with severely impaired health status.2 We were able to show statistically significant and clinically relevant positive effects on 6-minute walking distance (6MWD), muscle force, cycle exercise endurance time, and HRQoL. Studies investigating long-term effects are more scarce and show less clear results. Although the majority of studies reported positive results on exercise performance and HRQoL, only half of the studies that investigated exacerbation rate and/or use of health care resources reported statistically significant positive effects.3 The studies published varied considerably in sample size, severity of disease, type and duration of the program offered, follow-up time, and whether or not patients participated in a maintenance program. Reducing exacerbation frequency and subsequent health care utilization is considered to be an important outcome target in the treatment of COPD.4,5 Exacerbations lead to increased complaints, reduced HRQoL, and reduced physical activity.6 This can lead to reduced exercise tolerance and muscle dysfunction.7,8 Furthermore, frequent exacerbations are related to accelerated lung function decline and are associated with increased mortality.9–13 PR might decrease exacerbation and hospitalization rates by improving physical condition and physical activity in daily life. Recent studies show that less active persons have a higher risk for hospital admission.14,15 Moreover, the improvement of knowledge of the disease, awareness of body symptoms, and self-management skills might lead to earlier recognition and treatment of exacerbations.16
The purpose of this study was, therefore, 1) to evaluate the effect of a PRP on self-reported exacerbation and hospitalization frequency during 1 year after PR compared with 1 year before PR, and 2) to explore determinants (at baseline and after completing a PRP) that might predict a change in exacerbation and hospitalization frequency.
Materials and methods
Study design
A prospective, observational study of patients enrolled in a comprehensive PRP in a tertiary referral center in the Netherlands was performed. The study was institutional review board exempt because all procedures and measurements were part of the usual care in our institute, and only deidentified, preexisting data were used.
Participants
All patients with COPD who participated in the comprehensive program of the “Schoondonck” Center for Pulmonary Rehabilitation, Breda, the Netherlands, between June 2006 and December 2012 were included in this study. Referral criteria and contraindications for participation in the program have been described and discussed extensively in a previous article.2 Patients were referred by pulmonologists from the southwest region of the Netherlands to this tertiary referral center for PR. Reasons for referral were a high impact of the disease on health status, with no satisfactory response to prior medical and nonmedical treatment, including rehabilitation in primary care and hospital-based rehabilitation. The patients who were referred and enrolled typically had at least three of the following features: 1) severe to very severe airway obstruction, 2) a markedly limited exercise performance with a maximal power output on a cycle ergometer (Wmax) of less than 50% predicted, 3) a severely impaired quality of life as measured with the St George’s Respiratory Questionnaire (SGRQ) total score of more than 50%, and 4) a relatively high annual, self-reported exacerbation rate (more than three in the preceding year) and markedly high health care utilization (more than two exacerbation-related hospitalizations in the preceding year).
Intervention
The indication for participation in a comprehensive PRP was based on evaluation of the impact of the chronic respiratory disorder on different dimensions of health status, that is, physiological functioning, symptoms, activities, quality of life, and health care utilization during an assessment.17 The measurement instruments are consistent with markers that have previously been identified as appropriate for measuring clinically relevant outcomes in COPD.18 Pulmonary function tests, incremental exercise test, and 6MWD were obtained according to American Thoracic Society/European Respiratory Society guidelines.19–21 Cycle exercise endurance was determined with a constant work rate test on a cycle ergometer at a work rate equal to 75% of Wmax obtained in a preceding incremental test performed in the same week.22 The Medical Research Council scale for dyspnea was recorded, and the BODE index (Body mass index, airway Obstruction, Dyspnea, and Exercise capacity) was calculated.23,24 HRQoL was measured with the SGRQ and the Medical Outcomes Study short-form survey, version 2 (SF-36, version 2).25,26
Patient characteristics, program components, and outcome measurements have been described extensively earlier.2
The initial assessment was followed by an individually tailored comprehensive PRP of 12 weeks duration, which was carried out in fixed groups of 8–10 persons.27 Patients participated in the program 5 days a week, for a weekly average of 20–25 hours, either as an in- or outpatient. Besides group sessions, patients received interventions on an individual basis: for example, counseling by psychologist or social worker, art therapy sessions, and educational conversations with a dietician or respiratory nurse. Indication for individual therapy sessions was determined by the healthcare professionals during the assessment week. To improve self-management skills, all patients made an individualized written action plan for exacerbations, under the supervision of a respiratory nurse and pulmonary physician. This was done by offering educational group sessions covering exacerbation management (three sessions, 30 minutes each) and individual counseling by a respiratory nurse (up to five sessions, 30 minutes each). Weekly group sessions of 1 hour on training in body awareness were an important instrument to teach the participants how to correctly recognize symptoms of exacerbation.
At discharge, the participants were instructed to continue training with a local physiotherapist for 30–60 minutes, twice weekly, for which the participants received written training instructions. These physiotherapists were trained in treating COPD patients. Participants were instructed to make an appointment with their referring pulmonary physician or respiratory nurse or both in the first 2–3 months after discharge.
Outcomes
Exacerbation frequency in the year preceding participation in the PRP was recorded by asking the participant about the exacerbation frequency in the previous year. An exacerbation was defined as an increase in or new onset of more than one symptom of COPD (cough, sputum, wheezing, dyspnea, or chest tightness), with at least one symptom lasting 3 days or more and leading the patient’s attending physician to initiate treatment with systemic glucocorticoids, antibiotics, or both.28 Participants were also asked about the frequency of hospitalizations as a result of exacerbations in the previous year. Exacerbations that were initially treated outside the hospital but resulted eventually in hospitalization, without interruption of the treatment, were considered as hospitalizations. The total number of exacerbations consisted of both exacerbations in and out of hospital.
During the year following PR, questionnaires were sent to the participants at fixed intervals (3, 6, and 12 months after completing PR). Patients were asked to record the number of exacerbations and exacerbation-related hospitalizations during the previous period.
Data were collected by an administrative assistant who tried to contact the participants by phone if data were missing to ensure a maximal retrieval of data. Data were collected in an SPSS database, which was anonymized for research purposes.
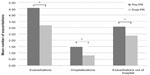
Patients were classified as having infrequent or frequent exacerbations. Infrequent exacerbations were defined as zero to two exacerbations per year, and frequent exacerbations were defined as more than two exacerbations per year.29 The percentage of patients having infrequent or frequent exacerbations 1 year before and 1 year after PR was reported. The percentage of patients that changed to a different exacerbation type was calculated. Four patterns of change were defined: unchanged infrequent, unchanged frequent, frequent to infrequent (decreased), and infrequent to frequent (increased).
Statistical analysis
Statistical analysis was done using IBM SPSS version 19. Baseline characteristics and changes in exacerbation and hospitalization frequency were assessed for normality using visual inspection of normal quantile–quantile plots and histograms.
Differences in baseline characteristics between completers, dropouts, and deaths were analyzed with an ANOVA test or a Kruskal–Wallis test for categorical data or depending on the criteria for normality. Data are reported as the mean ± standard deviation unless otherwise specified. Changes in exacerbation and hospitalization frequency 1 year before compared with 1 year after were tested with a paired-samples t-test. A P-value of less than 0.05 was considered significant. Change in exacerbations frequency type before and after PR was analyzed with a McNemar test.
Logistic regression
A hierarchical logistic regression analysis was performed to ascertain effects of baseline characteristics on the likelihood to change from frequent exacerbation type 1 year before PR to infrequent exacerbation type 1 year after PR (1 =change from frequent to infrequent; 0 =unchanged or change from infrequent to frequent). Four blocks of baseline parameters were tested: age, sex, body mass index (block one); forced expiratory volume in 1 second (percent predicted [% pred]), quadriceps force (% pred), Wmax (% pred) (block two); SGRQ total score (block three); and exacerbation frequency in the year preceding PR (block four). These parameters were chosen because they are commonly tested before PR and because they represent different domains of the disease. Another similar hierarchical logistic regression analysis was done, with the same baseline characteristic but with reduction in exacerbation frequency (at least one exacerbation less in the following PR compared to the year preceding PR) (=1) or no reduction in exacerbation frequency as dependent variable (=0). Finally, a logistic regression analysis was performed with change from frequent to infrequent exacerbation pattern as dependent variable and change in SGRQ total score, constant work rate test, and 6MWD after PR as independent variables.
Results
Patient characteristics
In total, 537 patients completed the initial program of 12 weeks and were eligible for follow-up. During the 1-year follow-up period after PR, 38 patients died (7%) (deaths). In addition, 156 patients (29%) did not answer the questionnaire regarding exacerbation and hospitalization frequency sufficiently and were considered as lost to follow-up (dropouts). For 343 patients, complete data on exacerbation and hospitalization frequency was available during the 1-year follow-up and were eligible for analysis (completers). Patient characteristics for completers, dropouts, and deaths are shown in Table 1.
Compared with patients that completed the follow-up, patients that were lost to follow-up were more often female, were younger, and had a lower score on the mental component scale the SF-36. When comparing participants that died during follow-up with completers and dropouts, they had a higher Medical Research Council scale and BODE index, more hyperinflation, lower Wmax (% pred), and lower 6MWD than the survivors. In addition, patients who died during follow-up had a lower diffusion capacity and higher SGRQ total score compared with completers.
Reduction of exacerbation and hospitalization frequency
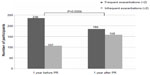
The mean number of exacerbations decreased significantly after participating in a PRP by 1.37 exacerbations/year (95% confidence interval 1.029 to 1.717) from 4.56±3.26 exacerbations in the year preceding PR to 3.18±2.53 in the year following PR (t[342]=7.847, P<0.0005, d=0.42).
The number of hospitalizations due to exacerbations decreased significantly by 0.68 hospitalizations/year (95% confidence interval 0.467 to 0.903) from 1.48±1.84 in the year preceding PR to 0.80±1.31 hospitalizations/year in the year following PR (t[342]=6.184, P<0.0005, d=0.33).
The mean number of exacerbations, hospitalizations, and exacerbations out of hospital 1 year before and 1 year after PR are presented in Table 2 and in Figure 1.
  | Table 2 Exacerbations and hospitalizations 1 year before and 1 year after pulmonary rehabilitation (paired samples t-test) |
  | Figure 1 Mean number of exacerbations (total), hospitalizations, and exacerbations out of hospital 1 year before and 1 year after PR. |
One hundred and ninety-seven of 343 participants (57.4%) experienced a reduction in total exacerbation frequency of at least 1 exacerbation, and 163 participants experienced a reduction of at least 1 hospitalization (47.5%). For 56 (16.3%) participants, total exacerbation frequency was unchanged, and for 118 (34.4%) participants, hospitalization frequency was unchanged. Exacerbation and hospitalization frequency was increased for 90 (26.2%) and 62 (18.1%) participants, respectively.
Of the 343 participants, 236 (69%) had frequent exacerbations and 107 (31%) had infrequent exacerbations 1 year before PR. During the year after PR, 185 (54%) participants had frequent exacerbations and 158 (46%) had infrequent exacerbations. This change was a consequence of 85 frequent exacerbators becoming infrequent exacerbators and 34 infrequent exacerbators becoming frequent exacerbators. A McNemar test determined that the difference in the proportion of frequent exacerbators pre- and post-PR was statistically significant (X2[1]=21.008, P<0.0005). The proportion of frequent and infrequent exacerbation type before and after PR is graphically presented in Figure 2.
Prediction of change in exacerbation frequency
A hierarchical logistic regression analysis was performed to ascertain effects of baseline characteristics on the likelihood to change from frequent exacerbator 1 year before PR to infrequent exacerbator 1 year after PR, testing four blocks of baseline parameters (age, sex, body mass index [block one]; forced expiratory volume in 1 second [% pred], quadriceps force [% pred], Wmax [% pred] [block two]; SGRQ total score [block three]; and exacerbation frequency in the year preceding PR [block four]). Although this model was statistically significant (X2[8]=15.576, P=0.049), only a very small percentage of 6.6% of the variance could be explained. Two variables (SGRQ total score and exacerbation frequency preceding PR) contributed statistically significantly to the effect, with exacerbations in the year preceding PR accounting for the majority of the effect, with an increase of explained variance from 2.8% to 6.6% after adding the variable to the model with the previous blocks of variables.
When a similar procedure was performed to ascertain the effect of the same baseline characteristics on the likelihood that participants would have at least one exacerbation less in the year following PR compared to the year preceding PR, the model was statistically significant (X2[8]=99.419, P<0.005), and a larger proportion of the variance was explained (34.1%). In this model, only exacerbation frequency in the year preceding PR contributed statistically significantly, showing an increase of explained variance from 5.3% to 34.1% after adding the variable to the previous blocks of variables.
A logistic regression model with change from frequent to infrequent exacerbator as dependent variable and variables that represent change after PR as independent variables (change in 6MWD, cycle endurance time, SGRQ total score) did not reveal any statistically significant variables that might predict a change from frequent to infrequent exacerbation type.
Discussion
This study demonstrates a significant reduction in exacerbation and hospitalization frequency after PR. This reduction largely exceeds the suggested minimal clinically important difference.30 Not only was the mean number of exacerbations reduced but there was also a significant reduction in the proportion of patients that were classified as frequent exacerbator. Baseline characteristics and change during the program are not very useful to predict a change in exacerbation frequency. However, at baseline, higher exacerbation frequency in the year preceding PR predicts a larger reduction in exacerbation frequency in the year after PR. Patients with a frequent exacerbation phenotype seem to have the largest potential for reducing the exacerbation frequency and may have greater benefits from participation in the PRP on that long-term outcome. Change in outcome measurements after completing the PRP did not significantly predict effects on exacerbation rate.
One of the main advantages of this study is the large number of severely disabled patients with COPD, with high impact on physical performance and HRQoL. In a publication in 2012, Ochmann et al3 reviewed 20 studies performed between 2000 and 2010 that described exacerbation rate and/or COPD-related health care utilization after PR, with the number of participants ranging between 24 and 522. Only three of the 20 studies had more than 200 participants. These reviewed studies varied considerably in patient characteristics, components of the PRP, and outcome measurements. About half of the 20 studies showed a reduction in exacerbation rate and/or health care utilization. The number of hospitalizations preceding PR in these studies is lower than in our group, ranging from 0.3 to 2 per year whereas, in our study, the exacerbation rate before PR is higher, with a mean of 4.56 exacerbations per year. This finding, combined with low HRQoL, indicates that our population is a severely disabled group.
Long-term improvement in this population will only be possible by offering an intensive PRP, where integrated care is the cornerstone of the program. The importance of reduction of exacerbation frequency cannot be underestimated; it might contribute to preservation of quality of life and even survival. By influencing exacerbation frequency, we might influence the natural course of the disease since frequent exacerbations are associated with more rapid lung function decline.9 We believe that the reduction in exacerbation frequency is influenced by the improvement of self-management and alterations in health behavior.31,32 Because individualized action plans without a PRP do not always improve exacerbation rates and health care utilization, the integration of self-management improvement in the PRP seems to be a key factor to improve health care utilization.33,34 Increased awareness of body symptoms and knowledge of symptoms related to exacerbations was an important part of the program. Earlier recognition and subsequent treatment of exacerbations can lead to earlier recovery and probably less recurrence of exacerbation.35 Although it could also be expected that an increased awareness of symptoms related to exacerbations might lead to an increase in exacerbation treatment, this was not observed. This might indicate that the PRP has caused a sustained improvement in health-related behavior, possibly by improving self-management skills and physical activity in daily life.36 In the present study, we do not have data on pulmonary function or physical performance at 1 year following PR, so we do not know whether these parameters are associated with a reduction of exacerbation frequency. The identification of factors that might be associated with reduction in exacerbation frequency is an interesting area for future research.
The reduction seen in exacerbation frequency subsequently seems to lead to a very significant reduction in exacerbation-related hospitalization frequency, which has the potential to reduce health care costs dramatically. We know that the majority of the costs incurred in chronic respiratory patients are associated with the costs of hospitalization.37–39 In our study, the total number of hospitalizations for the whole group decreased from 535 hospitalizations to 344, or a reduction of 191 hospitalizations.
Baseline characteristics and their change after participation in the PRP are not very useful predictors for change in exacerbation frequency. A recent study by Donaldson et al40 also found that a change in exacerbation frequency seems difficult to predict. This lack of predictors could be explained because of the heterogeneity of COPD and because the program components are individually tailored according to the observations during the assessment. Because, in the present study, we did not record the content and duration of individual components, it is not possible to correct for this.
One of the limitations of our study is the absence of a control group. However, because in a Cochrane review, PR has been proven to be effective, at least on the short term, this eliminates the need for randomized studies.1 Our population is very severely impaired and experiences a major impact on quality of life, so we believe it is unethical not to offer a proven intervention to these patients. This also points to another possible limitation: our population is a selected group for which the high rate of exacerbation and hospitalization frequency is one of the main reasons for referral to our center. The increase in exacerbation and hospitalization rate in the year before PR might be incidental, and we do not know what the natural course of the disease in these patients might be. However, there are indications that patients with frequent exacerbations have a more rapid deterioration in health status, so it seems unlikely that, without intervention, the exacerbation rate would be spontaneously reversed.31
The number of dropouts during the follow-up period is significant but can be expected in a long-term observational study, with the majority of the participants experiencing a severely impaired health status. Significant differences in patient characteristics at baseline between completers and dropouts that might predict dropout are limited. Specifically, there are no significant differences in comorbidity or in exacerbation or hospitalization frequency in the year preceding PR. Differences in change in outcome during the PRP between completers and dropouts are limited, which means that the absence of improvement is unlikely to predict dropout.
The recorded exacerbations and hospitalizations are self-reported, which might lead to under or overreporting. Data regarding the year preceding PR were retrospectively recorded by asking the participants about the frequency of these events at initial assessment, after informing the participants of the definition of exacerbation. This information was verified again by a respiratory nurse at the start of the PRP. Because the definition of exacerbations was treatment based, and information was verified twice, we believe that potential bias is limited. In case there would be a bias, we would rather expect an undercount of events pre-PR since participants have to recall information over a year. Despite this, there is a significant reduction in events post-PR. The data in the year following PR were collected prospectively by asking the participants to record the exacerbation and exacerbation-related hospitalization frequency on a questionnaire sent to the participants at 3, 6, and 12 months post-PR. Because participants were informed that they would be asked about the occurrence of these events, the potential for underreporting seems to be limited.
Conclusion
In conclusion, participation in a comprehensive PRP is associated with a significant reduction in self-reported exacerbation rate and exacerbation-related hospitalization rate in the year following PR. This might positively influence the progression of the disease, despite severely impaired health status of the participants at inclusion. The observed reduction in exacerbation rate might lead to a substantial reduction in health care utilization, with positive effects on health care costs. Future research should be directed to an evaluation of factors that might be associated with reduction in exacerbation and hospitalization frequency. This could lead to development of more specific PR components and maintenance strategies, in order to further improve long-term outcomes in this group of patients.
Acknowledgments
The authors would like to acknowledge Mrs M Groenestijn and Mr M Westerman for their valuable contributions to data collection and management.
Disclosure
The authors report no conflicts of interest in this work.
References
Lacasse Y, Goldstein R, Lasserson TJ, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2006;(4):CD003793. | |
van Ranst D, Otten H, Meijer JW, van ‘t Hul AJ. Outcome of pulmonary rehabilitation in COPD patients with severely impaired health status. Int J Chron Obstruct Pulmon Dis. 2011;6:647–657. | |
Ochmann U, Jörres RA, Nowak D. Long-term efficacy of pulmonary rehabilitation: a state-of-the-art review. J Cardiopulm Rehabil Prev. 2012;32(3):117–126. | |
Bourbeau J. Activities of life: the COPD patient. COPD. 2009;6(3):192–200. | |
Marchetti N, Criner GJ, Albert RK. Preventing acute exacerbations and hospital admissions in COPD. Chest. 2013;143(5):1444–1454. | |
Miravitlles M, Anzueto A, Legnani D, Forstmeier L, Fargel M. Patient’s perception of exacerbations of COPD – the PERCEIVE study. Respir Med. 2007;101(3):453–460. | |
Cote CG, Dordelly LJ, Celli BR. Impact of COPD exacerbations on patient-centered outcomes. Chest. 2007;131(3):696–704. | |
Spruit MA, Gosselink R, Troosters T, et al. Muscle force during an acute exacerbation in hospitalised patients with COPD and its relationship with CXCL8 and IGF-I. Thorax. 2003;58(9):752–756. | |
Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847–852. | |
Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931. | |
Soler-Cataluña JJ, Martínez-García MA, Sánchez LS, Tordera MP, Sánchez PR. Severe exacerbations and BODE index: two independent risk factors for death in male COPD patients. Respir Med. 2009;103(5):692–699. | |
Burtin C, Decramer M, Gosselink R, Janssens W, Troosters T. Rehabilitation and acute exacerbations. Eur Respir J. 2011;38(3):702–712. | |
Halpin DM, Decramer M, Celli B, Kesten S, Liu D, Tashkin DP. Exacerbation frequency and course of COPD. Int J Chron Obstruct Pulmon Dis. 2012;7:653–661. | |
Esteban C, Arostegui I, Aburto M, et al. Influence of changes in physical activity on frequency of hospitalization in chronic obstructive pulmonary disease. Respirology. 2014;19(3):330–338. | |
Zanoria SJ, ZuWallack R. Directly measured physical activity as a predictor of hospitalizations in patients with chronic obstructive pulmonary disease. Chron Respir Dis. 2013;10(4):207–213. | |
Bourbeau J, Saad N, Joubert A, et al. Making collaborative self-management successful in COPD patients with high disease burden. Respir Med. 2013;107(7):1061–1065. | |
Vercoulen JH, Daudey L, Molema J, et al. An Integral assessment framework of health status in chronic obstructive pulmonary disease (COPD). Int J Behav Med. 2008;15(4):263–279. | |
Glaab T, Vogelmeier C, Buhl R. Outcome measures in chronic obstructive pulmonary disease (COPD): strengths and limitations. Respir Res. 2010;11:79. | |
Miller MR, Hankinson J, Brusasco V, et al; ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. | |
Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–522. | |
Macintyre N, Crapo RO, Viegi G, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26(4):720–735. | |
O’Donnell DE, Travers J, Webb KA, et al. Reliability of ventilatory parameters during cycle ergometry in multicentre trials in COPD. Eur Respir J. 2009;34(4):866–874. | |
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. | |
Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. | |
Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation. The St George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–1327. | |
Mahler DA, Mackowiak JI. Evaluation of the short-form 36-item questionnaire to measure health-related quality of life in patients with COPD. Chest. 1995;107(6):1585–1589. | |
Nici L, Donner C, Wouters E, et al; ATS/ERS Pulmonary Rehabilitation Writing Committee. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med. 2006;173(12):1390–1413. | |
Decramer M, Celli B, Tashkin DP, et al. Clinical trial design considerations in assessing long-term functional impacts of tiotropium in COPD: the UPLIFT trial. COPD. 2004;1(2):303–312. | |
Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418–1422. | |
Chapman KR, Bergeron C, Bhutani M, et al. Do we know the minimal clinically important difference (MCID) for COPD exacerbations? COPD. 2013;10(2):243–249. | |
Spencer S, Calverley PM, Burge PS, Jones PW. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Respir J. 2004;23(5):698–702. | |
Bourbeau J, Ford G, Zackon H, Pinsky N, Lee J, Ruberto G. Impact on patients’ health status following early identification of a COPD exacerbation. Eur Respir J. 2007;30(5):907–913. | |
Walters JA, Turnock AC, Walters EH, Wood-Baker R. Action plans with limited patient education only for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2010CD005074. | |
Trappenburg JC, Monninkhof EM, Bourbeau J, et al. Effect of an action plan with ongoing support by a case manager on exacerbation-related outcome in patients with COPD: a multicentre randomised controlled trial. Thorax. 2011;66(11):977–984. | |
Chandra D, Tsai CL, Camargo CA Jr. Acute exacerbations of COPD: delay in presentation and the risk of hospitalization. COPD. 2009;6(2):95–103. | |
Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Antó JM. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. 2006;61(9):772–778. | |
Wedzicha JA, Wilkinson T. Impact of chronic obstructive pulmonary disease exacerbations on patients and payers. Proc Am Thorac Soc. 2006;3(3):218–221. | |
D’Souza AO, Shah M, Dhamane AD, Dalal AA. Clinical and economic burden of COPD in a medicaid population. COPD. 2014;11(2):212–220. | |
Pasquale MK, Sun SX, Song F, Hartnett HJ, Stemkowski SA. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–764. | |
Donaldson GC, Müllerova H, Locantore N, et al. Factors associated with change in exacerbation frequency in COPD. Respir Res. 2013;14:79. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.