Back to Journals » International Journal of General Medicine » Volume 11
Received care compared to ADP-guided care of patients admitted to hospital with chest pain of possible cardiac origin
Authors Perera M, Aggarwal L, Scott IA , Logan B
Received 25 February 2018
Accepted for publication 22 May 2018
Published 3 September 2018 Volume 2018:11 Pages 345—351
DOI https://doi.org/10.2147/IJGM.S166570
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Michael Perera,1 Leena Aggarwal,1 Ian A Scott,2,3 Bentley Logan1
1Medical Assessment and Planning Unit, Princess Alexandra Hospital, Brisbane, QLS, Australia; 2Department of Internal Medicine and Clinical Epidemiology, Princess Alexandra Hospital, Brisbane, QLS, Australia; 3School of Clinical Medicine, University of Queensland, Brisbane, QLS, Australia
Purpose: To assess the extent to which accelerated diagnostic protocols (ADPs), compared to traditional care, identify patients presenting to emergency departments (EDs) with chest pain who are at low cardiac risk and eligible for early ED discharge.
Patients and methods: Retrospective study of 290 patients admitted to hospital for further evaluation of chest pain following negative ED workup (no acute ischemic electrocardiogram [ECG] changes or elevation of initial serum troponin assay). Demographic data, serial ECG and troponin results, Thrombolysis in Myocardial Infarction (TIMI) score, cardiac investigations, and outcomes (confirmed acute coronary syndrome [ACS] at discharge and major adverse cardiac events [MACEs]) over 6 months of follow-up were analyzed. A validated ADP (ADAPT-ADP) was retrospectively applied to the cohort, and processes and outcomes of ADP-guided care were compared with those of care actually received.
Results: Patients had mean (±SD) TIMI score of 1.8 (±1.7); six (2.0%) patients were diagnosed with ACS at discharge. At 6 months, one patient (0.3%) re-presented with ACS and two (0.6%) died of non-coronary causes. The ADAPT-ADP defined 97 (33.4%) patients as being at low risk and eligible for early ED discharge, but who instead incurred mean hospital stay of 1.5 days, with 40.2% in telemetry beds, and 21.6% subject to non-invasive testing with only one positive result for coronary artery disease. None had a discharge diagnosis of ACS or developed MACE at 6 months.
Conclusion: Compared to traditional care, application of the ADAPT-ADP would have allowed one-third of chest pain patients with initially negative investigations in ED to have been safely discharged from ED.
Keywords: chest pain, accelerated diagnostic protocol, investigation, coronary outcomes
Plain language summary
Chest pain accounts for about 1 in 12 presentations to emergency departments (EDs). In ruling out acute coronary events and preventing any complications after discharge, most patients have traditionally either had prolonged stays in ED or been admitted for further evaluation. But most will be shown to have a non-coronary condition. Accelerated diagnostic protocols (ADPs) can identify low-risk patients eligible for safe, early discharge from ED. But do hospitals actually use these protocols, and if not, how many patients may be subject to unnecessary overnight stays and low-yield investigations? We analyzed care received by 290 patients presenting to ED with chest pain who did not have coronary events confirmed on arrival. They compared care actually received with care patients would have received if an ADP had been followed. They found that only 2% of these patients had a coronary event diagnosed by the time of hospital discharge, and none died from a coronary event up to 6 months later. If the ADP had been applied, a third of these patients could have been discharged from ED. Instead, they incurred an average stay in hospital of 1.5 days and a fifth underwent tests for coronary artery disease (CAD) which were negative in 99% of cases. This study indicates that for patients presenting to ED with chest pain, decisions to admit them to rule out coronary disease should not rely on clinical judgment alone but incorporate ADPs in reducing unnecessary hospital stays and investigations.
Introduction
Presentations with chest pain for further evaluation are one of the most common reasons for hospital admission from emergency departments (EDs).1 In Australia, around 500,000 patients present each year with possible cardiac chest pain to EDs nationwide, accounting for around 8% of all ED presentations.2 The majority will incur a hospital stay to undergo further assessment,3 with up to half being admitted overnight to inpatient wards.4 While chest pain may be the first manifestation of an acute coronary syndrome (ACS), no more than 15% of such patients will have this diagnosis subsequently confirmed.4,5 However, clinical findings alone cannot definitively rule out ACS,6 and discharging patients from ED, in the absence of more extensive investigation, raises anxiety about missing a diagnosis of ACS and incurring the clinical and medicolegal risk of subsequent major adverse cardiac events (MACEs). On the other hand, unnecessary inpatient cardiac workup in patients with low-risk chest pain delays discharge from hospital, causing congestion in ED and receiving medical wards, such as medical assessment and planning units (MAPUs), and incurring costs.4
Studies indicate that accelerated diagnostic protocols (ADPs), several of which use the Thrombolysis in Myocardial Infarction (TIMI) score to stratify risk,7 can reliably identify low-risk patients who do not require inpatient investigations and can be rapidly discharged from ED.8–10 These patients demonstrate 30-day MACE rates less than 1% – a figure most ED physicians11 and patients12 accept as the safety threshold for early discharge with investigations performed, as necessary, as an outpatient. Such protocols have been endorsed in Australian,13 United States,14 and European15 clinical practice guidelines, but the extent to which they have been adopted is unclear. One ADP, named ADAPT (2-hour Accelerated Diagnostic Protocal to Access Patients with Chest Pain Symtoms Using Contemporary Troponins as the Only Biomarkers), which used the TIMI score and results of sensitive troponin assays performed at least 2 hours apart from the time of ED presentation, was shown in a prospective trial to be more than 99% sensitive in identifying the 10–20% of patients who are at low risk (<1%) of 30-day MACE among all patients presenting with possible ACS to ED of study hospitals.9
The aim of this study was to determine the clinical characteristics, risk level, investigations performed, and medium-term outcomes of consecutive patients with possible ACS admitted to a MAPU of a large tertiary hospital (received care) and to compare care processes and outcomes with those that may have transpired if the same cohort had been subjected to the ADAPT-ADP (ADP-guided care).
Patients and methods
This retrospective study included all consecutive patients with chest pain admitted for further evaluation to the MAPU at Princess Alexandra Hospital between February 1, 2012 and June 1, 2012 in whom initial investigations in ED were not confirmatory for ACS. The hospital has 640 acute beds and services a catchment population of 600,000. During this period, hospital practice was to admit patients with unconfirmed but possible ACS (no ischemic changes on initial electrocardiogram [ECG] and non-elevated initial serum troponin in ED) to the MAPU under a cardiologist or general physician following consultation between an emergency physician and cardiology/general medical registrar. Excluding patients with clear cut evidence of myocardial infarction or other diagnoses on presentation, around a third of patients with undifferentiated chest pain are discharged from ED after sole review by emergency physicians, and the remainder are admitted for further evaluation (Dr James Collier, Co-director of Emergency Medicine, personal communication, March, 2012). During the study period, hospital guidelines stipulated that all patients undergo at least two serial ECGs and two troponin assays within the first 6 hours of ED presentation. However, guidelines did not mandate calculation and documentation of TIMI scores on patients, or recommend how patients should be managed in terms of cardiac investigations or use of telemetry. Such decisions were left to the discretion of the treating cardiologist/general physician.
Data were collected from medical notes, discharge summaries, and electronic pathology (Auslab) and radiological (WEB1000) databases and comprised demographic details, initial description of chest pain (being either atypical or typical for ischemia based on history), results of serial ECGs and troponin assays, cardiac investigations performed (including exercise stress ECG test, rest or stress echocardiogram, myocardial perfusion scan, computerized tomographic coronary angiography [CTCA], and invasive coronary angiography), use of telemetry, and length of hospital stay. TIMI scores were retrospectively calculated for all patients, with a range of 0–7.7
Outcomes during the index admission were diagnosis of ACS and all-cause death, yield of diagnostic tests, and frequency of coronary revascularization (either percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG]). Outcomes at 6-month follow-up were MACE defined as all-cause death and readmission for ACS, new-onset arrhythmia, or congestive heart failure to any public hospital throughout the state, as ascertained using state-wide public hospital electronic databases via Viewer software. As access to death registries was not available, entries in Viewer reporting deaths within 6 months or confirming survival by any clinical encounter beyond 6 months were used to ascertain all deaths.
The ADAPT-ADP, as described in Table 1,9 was applied retrospectively to the same cohort in identifying low-risk patients whose clinical characteristics, investigations, and outcomes at 6 months were evaluated and then compared to those of the remaining non-low-risk patients.
  | Table 1 ADAPT-ADP score Note: Data from Than M, Cullen L, Aldous S, et al. A 2-hour Accelerated Diagnostic Protocol to Assess Patients with Chest Pain Symptoms Using Contemporary Troponins as the Only Biomarker: the ADAPT Trial. J Am Coll Cardiol. 2012;59(23):2091–2098.9 Abbreviations: ED, emergency department; ECG, electrocardiogram; TIMI, Thrombolysis in Myocardial Infarction; ADP, accelerated diagnostic protocol. |
Chi-square/Fisher’s exact test and Student’s t-tests were used to compare proportions and normally distributed means involving binary or continuous variables, respectively. As this study was originally intended as a quality assurance review and retrospectively analyzed routinely collected data on completed episodes of care with reporting of anonymized data and no need for informed patient consent or patient contact, need for ethical approval was waivered by the Director of Clinical Governance.
Results
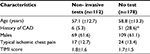
A total of 290 patients with initially negative cardiac workup in ED (no ischemic changes on ECG and non-elevated initial troponin assay) were included in the study. Their characteristics are summarized in Table 2. Mean age was 58.6 (±SD 14.4) years and 168 (58.0%) patients were male. All patients underwent two serial ECGs and two serial troponin assays within 6 hours of ED presentation. One hundred seventy-one (59.0%) patients were admitted under cardiologists and the remainder under general physicians. The mean length of hospital stay was 1.6 (±SD 1.2) days and 121 (41.3%) were admitted to telemetry beds. Sixty-seven (23.1%) patients had a previous diagnosis of CAD, of whom 16 (5.5%) had undergone previous PCI and 30 (10.3%) previous CABG. The mean (±SD) TIMI score was 1.8 (±1.7).
Received care analysis
Of the 290 patients, six (2.0%) were subsequently confirmed as having ACS at discharge as a result of elevated troponin assays performed within 6 hours following the initial non-elevated assay in ED (n=4), new ischemic ECG changes and elevated troponin (n=1), and one patient diagnosed with unstable angina who underwent coronary angiogram and PCI.
Non-invasive testing
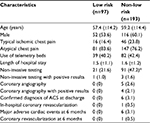
A total of 112 patients (38.6%) underwent non-invasive testing: 53 (18.3%) underwent exercise stress ECG tests of whom only two (3.8%) showed positive results (Figure 1). Other dynamic tests performed in 16 patients included exercise stress echocardiograms (n=5), dobutamine stress echocardiograms (n=9), and myocardial perfusion scans (n=2), none of which were positive for CAD. CTCA was performed in 45 (15.5%) patients with two (4.5%) returning a positive result. Two patients had non-conclusive exercise stress ECG tests, with one undergoing myocardial perfusion scan and the other CTCA, both of which were negative. Of all 114 tests performed (two patients had more than one test), only four (3.5%) were positive for CAD. Comparing baseline characteristics of the112 patients who underwent testing with the 178 who did not (Table 3), the only significant difference was a higher prevalence of past history of CAD among those not tested (28.6% vs 5.3%, p<0.001).
Invasive testing and management
Five (1.5%) underwent coronary angiography, with one undergoing PCI and none referred for CABG. Of the six patients diagnosed with ACS, four demonstrated CAD on angiography, one of whom had prior history of PCI. Mean TIMI score for all patients undergoing invasive coronary interventions was 3.4 (±2.7). The remaining patients with ACS presumptively diagnosed during their hospital stay received medical management, as did the two patients with positive CTCA.
Follow-up period
All 290 patients were followed up for a 6-month period after discharge. Two patients (0.7%) subsequently died, one receiving palliative care for advanced multi-morbidity and the other from long-standing refractory congestive heart failure. Forty-seven of 290 (16.2%) patients were readmitted, one with confirmed diagnosis of ACS (0.3%) who underwent urgent PCI (TIMI score =4), and 46 with non-ACS diagnoses which included stable angina (n=4), atypical chest pain (n=22), gastro-esophageal reflux (n=4), musculoskeletal chest pain (n=8), and other non-cardiac causes (n=7). One patient underwent a second PCI as an elective procedure for known CAD.
ADP-guided care analysis
All patients in our cohort met the first two criteria of the ADAPT-ADP (Table 1) which stipulate that the initial ECG in ED shows no ischemic changes and the initial and subsequent troponin assays were not elevated. The third criteria required TIMI score of 0, and all three criteria were met in 97 (33.4%) patients. The characteristics, management, and outcomes of these 97 patients are listed in Table 4 and compared with those of patients with a TIMI score of 1 or more. The majority (81 [83.6%]) presented with atypical chest pain, almost half (39 [40.2%]) were admitted to telemetry beds, and a fifth (21; 21.6%) underwent non-invasive testing during a mean length of stay of 1.5 days, of whom only one returned an equivocally positive stress ECG test. None of these patients, including the latter, had a discharge diagnosis of ACS, underwent coronary angiography, or developed MACE at 6 months of follow-up. Compared to non-low-risk patients (TIMI score of 1 or more), low-risk patients were more often admitted to telemetry beds (52.6% vs 37.3%, p=0.03) but underwent fewer non-invasive tests (21.6% vs 47.2%, p<0.001).
Discussion
This review of consecutive patients admitted to a tertiary hospital MAPU with chest pain following initially negative investigations in ED yielded several key findings. Only 2% were subsequently confirmed as having ACS, less than 4% returned positive results for CAD on non-invasive testing, only 2% demonstrated CAD at coronary angiography, and less than 1% underwent coronary revascularization during the hospital stay. There were no in-hospital deaths and all subsequent deaths over the following 6 months were from non-coronary causes; less than 1% re-presented with ACS.
If the ADAPT-ADP had been applied, a third of these patients could have been safely discharged from ED following a non-elevated 2-hour troponin level. Instead, they incurred an overnight hospital stay of 1.5 days on average, occupied a telemetry bed in almost half the cases, and underwent investigations at a rate of 1 in 5. Several studies have documented the very low incidence of MACE in patients with chest pain deemed to be at low to intermediate risk, ranging from less than 1% to no more than 1.7%, respectively, at 30 days of follow-up.5,16,17 Our study involved longer follow-up with no further increase in MACE rates above 1% at 6 months.
More evidence is emerging of the utility and safety of ADPs which identify patients at low risk (<1%) of MACE at 30 days. Combining the ADAPT-ADP with a clinical risk score based on patient characteristics and presenting symptoms, the Emergency Department Assessment of Chest Pain Score identifies as many as 50% of patients presenting with possible cardiac chest pain as being at low risk (<1%) for MACE at 30 days.18 More recently, substituting high-sensitivity troponin assays for sensitive assays at 0 and 2 hours after presentation identified 40% of patients with TIMI scores of either 0 or 1 as being at low risk and eligible for early discharge.19
Adoption of ADPs helps to decongest EDs and MAPUs, reduces patient inconvenience, and avoids adverse events incurred by unnecessary and, in some cases, invasive management. A study of over 11,000 patients in the United States identified a 15-fold risk of care-related complications compared to benefits realized in terms of prevented MACE among low-risk patients who were admitted for investigation.5 In addition, 40% of patients in our study occupied the limited number of telemetry beds, despite definitive evidence of the low utility of telemetry in low-risk patients in whom less than 1% develop arrhythmias.20–24
In hospitals in Queensland, Australia, initiatives aimed at systematizing the use of ADPs have shown increased numbers of low-risk patients being discharged more quickly from ED. A study done in one hospital showed that with the introduction of an accelerated chest pain pathway, 19% of patients with undifferentiated chest pain who were discharged from ED within 3 hours (average of 163 minutes ED length of stay) over a 7-month period suffered no MACE during a 4-week follow-up period.25 A more recent and extensive interrupted time series evaluation of the use of the ADAPT-ADP across 16 Queensland hospitals showed that, over 12 months after ADP implementation, 21% of patients presenting to ED with chest pain were categorized as being at low risk and eligible for early discharge.26 Change in practice resulted in a decrease in hospital admission rate from 68.3% to 54.9% and decrease in mean hospital length of stay from 57.7 to 47.3 hours (p<0.01 for both comparisons). Use of an ADP in three EDs in the state of Victoria, which adopted TIMI score <3 as low risk, allowed 83% of 1547 patients with low-risk chest pain to be discharged from ED, with only one (0.09%) suffering from MACE at 30 days, compared to discharge of only 31% of 747 similar low risk patients who were managed using a traditional care pathway.27 In a prospective observational study, use of a similar ADP in a regional hospital in New Zealand resulted in early and safe discharge of 70% of patients presenting to ED with undifferentiated chest pain.28
Among patients classified as being at non-low risk, the optimal and most cost-effective means of non-invasive testing for stratifying risk of CAD remains unclear, as each testing modality (stress ECG, CTCA, stress imaging) has its strengths and limitations. Same-day exercise stress ECG testing in patients who can exercise and have an interpretable ECG, combined with an ADP, is widely available, safe and efficient, and has high negative predictive value.29 Exercise stress ECG testing can also be safely deferred to outpatient settings in low-to-intermediate risk patients.30 However, recent randomized trials suggest CTCA, in patients with no contrast allergies or significant renal disease, is superior to stress ECG in ruling out ACS and enabling more rapid discharge from ED.31,32 Guidelines for CTCA in the ED have been developed,33 and recent reviews suggest CTCA may be the more cost-effective testing option, although in low-risk patients (TIMI score of 0), a no-testing strategy may be preferred.34 In this study, exercise stress ECG (a dynamic test) and CTCA (an anatomical test) were used in roughly equal numbers of patients. However, irrespective of the test used, the positive yield for CAD of all non-invasive tests combined was less than 5%, and the only predictor of non-testing was a known history of CAD. The reasons why clinicians chose to test or not test were not able to be ascertained from chart documentation.
This study has some limitations. It was a retrospective analysis reliant on accuracy of medical notes, and diagnoses of troponin-negative unstable angina made by treating clinicians, in the absence of objective verification, may have been incorrect, although this applied to only one patient. Similarly, rise and fall in elevated troponin levels were not scrutinized by the authors to confirm myocardial infarction; instead we accepted the discharge diagnosis assigned by the treating consultant. The study focused on patients admitted to MAPU of a tertiary hospital with access to a range of testing modalities, and our results cannot be generalized to other hospitals with different testing modalities and admission policies. While we were unable to ascertain in-hospital deaths or readmissions of patients presenting to private hospitals or hospitals outside of Queensland, all patients were Queensland residents lacking private health insurance.
Study strengths included the detailed analysis of patient characteristics and investigations performed and the long follow-up of 6 months, with ascertainment of survival status in every patient, providing further confirmation of the very low medium-term mortality, or MACE rates in low-risk patients.
Conclusion
This study demonstrates that the majority of patients with chest pain admitted to a MAPU after initially negative investigations in ED are at low risk for ACS, either in hospital or following discharge. Testing procedures for ruling out CAD in such patients can be deferred to outpatient settings but need to be highly selective, as current testing patterns are associated with very low rates of positive results. If the ADAPT-ADP had been applied, at least a third of patients could have been safely discharged from ED. Contemporary evidence and guidelines argue for a more systematic application of ADPs centered on TIMI scores and initial ECGs and troponin assays in identifying patients at low risk who can be spared admission to MAPUs and subsequent low-yield in-hospital cardiac testing.
Author contributions
MP and LA conceived the concept and design of the study; MP, LA, and BL collected and analyzed the data; MP, LA, and IAS interpreted the data; IAS drafted the manuscript which was critically reviewed and revised by MP, LA, and BL. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Nawar E, Niska RW, Xu J. National hospital ambulatory medical care survey: 2005 emergency department summary. Adv Data. 2007;386:1–32. | ||
Australian Institute of Health and Welfare. Australian Hospital Statistics 2011–12: Emergency Department Care. Health Services Series No. 45. Cat. no. HSE 126. Canberra, Australia: AIHW, 2012. | ||
Goodacre S, Cross E, Arnold J, et al. The health care burden of acute chest pain. Heart. 2005 91(2):229–230. | ||
Cullen L, Greenslade J, Merollini K, et al. Cost and outcomes of assessing patients with chest pain in an Australian emergency department. Med J Aust. 2015;202(8):427–432. | ||
Weinstock MB, Weingart S, Orth F, et al. Risk for clinically relevant adverse cardiac events in patients with chest pain at hospital admission. JAMA Intern Med. 2015;175(7):1207–1212. | ||
Fanaroff AC, Rymer JA, Goldstein SA, et al. Does this patient with chest pain have acute coronary syndrome?: the rational clinical examination systematic review. JAMA. 2015;314(18):1955–1965. | ||
Hess EP, Agarwal D, Chandra S, et al. Diagnostic accuracy of the TIMI risk score in patients with chest pain in the emergency department: a meta-analysis. CMAJ. 2010;182(10):1039–1044. | ||
Than M, Cullen L, Reid CM, et al. A 2-h diagnostic protocol to assess patients with chest pain symptoms in the Asia-Pacific region (ASPECT): a prospective observational validation study. Lancet. 2011;377(9771):1077–1084. | ||
Than M, Cullen L, Aldous S, et al. A 2-hour accelerated diagnostic protocol to assess patients with chest pain symptoms using contemporary troponins as the only biomarker: the ADAPT Trial. J Am Coll Cardiol. 2012;59(23):2091–2098. | ||
Than M, Aldous S, Lord SJ, et al. A 2-hour diagnostic protocol for possible cardiac chest pain in the emergency department: a randomized clinical trial. JAMA Intern Med. 2014;174(1):51–58. | ||
Than M, Herbert M, Flaws D, et al. What is an acceptable risk of major adverse cardiac event in chest pain patients soon after discharge from the emergency department? A clinical survey. Int J Cardiol. 2013;166(3):752–754. | ||
Hess EP, Hollander JE, Schaffer JT, et al. Shared decision making in patients with low risk chest pain: prospective randomized pragmatic trial. BMJ. 2016;355:i6165. | ||
Chew DP, Scott IA, Cullen L, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Heart Lung Circ. 2016; 25(9):895–951. | ||
Amsterdam EA, Kirk JD, Bluemke DA, et al. American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Cardiovascular Nursing, and Interdisciplinary Council on Quality of Care and Outcomes Research. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010;122(17):1756–1776. | ||
Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267–315. | ||
Mitchell AM, Garvey JL, Chandra A, et al. Prospective multicenter study of quantitative pre-test probability assessment to exclude acute coronary syndrome for patients evaluated in emergency department chest pain units. Ann Emerg Med. 2006;47(5):447. | ||
Napoli AM. The association between pretest probability of coronary artery disease and stress test utilization and outcomes in a chest pain observation unit. Acad Emerg Med. 2014;21(4):401–407. | ||
Than M, Flaws D, Sanders S, et al. Development and validation of the Emergency Department Assessment of Chest Pain Score and 2 h accelerated diagnostic protocol. Emerg Med Australas. 2014;26(1):34–44. | ||
Cullen L, Mueller C, Parsonage WA, et al. Validation of high-sensitivity troponin I in a 2-hour diagnostic strategy to assess 30-day outcomes in emergency department patients with possible acute coronary syndrome. J Am Coll Cardiol. 2013;62(14):1242–1249. | ||
Durairaj L, Reilly B, Das K, et al. Emergency department admissions to inpatient cardiac telemetry beds: a prospective cohort study of risk stratification and outcomes. Am J Med. 2001;110(1):7–11. | ||
Snider A, Papaleo M, Beldner S, et al. Is telemetry monitoring necessary in low-risk suspected acute chest pain syndromes? Chest. 2002;122(2):517–523. | ||
Hollander JE, Sites FD, Pollack CV, Shofer FS. Lack of utility of telemetry monitoring for identification of cardiac death and life-threatening ventricular dysrhythmias in low-risk patients with chest pain. Ann Emerg Med. 2004;43(1):71–76. | ||
Grossman SA, Shapiro NI, Mottley JL, et al. Is telemetry useful in evaluating chest pain patients in an observation unit? Intern.Emerg Med. 2011;6(6):543–546. | ||
Syed S, Gatien M, Perry JJ, et al. Prospective validation of a clinical decision rule to identify patients presenting to the emergency department with chest pain who can safely be removed from cardiac monitoring. CMAJ. 2017;189(4):E139–145. | ||
George T, Ashover S, Cullen L, et al. Introduction of an accelerated diagnostic protocol in the assessment of emergency department patients with possible acute coronary syndrome: the Nambour Short Low-Intermediate Chest pain project. Emerg Med Australas. 2013;25(4):340–344. | ||
Parsonage WA, Milburn T, Ashover S, et al. Implementing change: evaluating the Accelerated Chest pain Risk Evaluation (ACRE) project. Med J Aust. 2017;207(5):201–205. | ||
Meek R, Braitberg G, Cullen L, et al. Outcome at 30 days for low-risk chest pain patients assessed using an accelerated diagnostic pathway in the emergency department. Emerg Med Australas. 2016;28(3):279–286. | ||
Munro AR, Jerram T, Morton T, Hamilton S. Use of an accelerated diagnostic pathway allows rapid and safe discharge of 70% of chest pain patients from the emergency department. N Z Med J. 2015;128(1408):62–71. | ||
Soremekun OA, Hamedani A, Shofer FS, et al. Safety of a rapid diagnostic protocol with accelerated stress testing. Am J Emerg Med. 2014;32(2):124–128. | ||
Rahman F, Mitra B, Cameron PA, Coleridge J. Stress testing before discharge is not required for patients with low and intermediate risk of acute coronary syndrome after emergency department short stay assessment. Emerg Med Australas. 2010;22(5):449–456. | ||
Litt HI, Gatsonis C, Snyder B, et al. Safety of CT angiography for rapid “rule-out” of acute coronary syndrome. N Engl J Med. 2012;366:1393–1403. | ||
Hoffmann U, Truong QA, Schoenfeld DA, et al; ROMICAT-II Investigators. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367:299–308. | ||
Raff GL, Chinnaiyan KM, Cury RC, et al; Society of Cardiovascular Computed Tomography Guidelines Committee. SCCT guidelines on the use of coronary computed tomographic angiography for patients presenting with acute chest pain to the emergency department: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr. 2014;8(4):254–271. | ||
Goodacre S, Thokala P, Carroll C, et al. Systematic review, meta-analysis and economic modelling of diagnostic strategies for suspected acute coronary syndrome. Health Technol Assess. 2013;17(1):v-vi, 1–188. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.