Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Real-World Experience of Treating Chronic Obstructive Pulmonary Disease with Triple Therapy
Authors Liao KM , Wang JJ, Ho CH
Received 8 January 2023
Accepted for publication 28 May 2023
Published 7 June 2023 Volume 2023:18 Pages 1057—1066
DOI https://doi.org/10.2147/COPD.S404039
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Zhang
Kuang-Ming Liao,1 Jhi-Joung Wang,2,3 Chung-Han Ho2,4,5
1Department of Internal Medicine, Chi Mei Medical Center, Chiali, Taiwan; 2Department of Medical Research, Chi Mei Medical Center, Tainan, Taiwan; 3Department of Anesthesiology, Tri-Service General Hospital and National Defense Medical Center, Taipei, Taiwan; 4Department of Information Management, Southern Taiwan University of Science and Technology, Tainan, Taiwan; 5Cancer Center, Wan Fang Hospital, Taipei Medical University, Taipei, Taiwan
Correspondence: Chung-Han Ho, Department of Medical Research, Chi Mei Medical Center, No. 901, Zhonghua Road, Yongkang District, Tainan, 710, Taiwan, Email [email protected]
Background: Double-blind randomized controlled trials have compared patients with chronic obstructive pulmonary disease (COPD) taking triple therapy, which can improve lung function, dyspnea, and quality of life and reduce acute exacerbation and mortality, with those taking long-acting muscarinic antagonist/long-acting β 2-agonist; however, the real-word treatment scenario may be different from that of a strict and well-designed study. The aim of our study was to assess long-term outcomes among patients with COPD who received triple therapy in real-world practice.
Methods: Data from Taiwan’s National Health Insurance Research Database (NHIRD) from 2005 and 2016 were used to identify COPD patients who were over 40 years of age with diagnosis codes 490– 492, 496 (ICD-9-CM) or J41-44 (ICD-10-CM). After matching for age, sex, and COPD exacerbations, COPD patients who did and did not receive triple therapy were enrolled in this study. Cox proportional regression was used to estimate the mortality risk between smoking status and COPD patients with and without triple therapy.
Results: A total of 19,358 patients with COPD who did or did not receive triple therapy were enrolled in this study. The prevalence rates of some comorbidities were higher among patients with COPD who received triple therapy than among those who did not receive triple therapy. These comorbidities included lung cancer, thoracic malignancies, bronchiectasis, and heart failure. The risk of mortality was higher among patients who received triple therapy than among those who did not receive triple therapy after matching for age, sex, and COPD exacerbations, with a crude hazard ratio, fully adjusted model hazard ratio and stepwise approach reduced hazard ratio of 1.568 (95% CI, 1.500– 1.639), 1.675 (95% CI, 1.596– 1.757), and 1.677 (95% CI, 1.599– 1.76), respectively.
Conclusion: Over 5 years of observation, patients with COPD who received triple therapy did not show a survival benefit compared with those who did not receive triple therapy in a real-world scenario.
Keywords: chronic obstructive pulmonary disease, mortality, real-world study, triple therapy
Introduction
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, patients with COPD who have already been treated with an inhaled corticosteroid (ICS)/long-acting β2-agonist (LABA) or a long-acting muscarinic antagonist/long-acting β2-agonist (LAMA/LABA) and still have significant dyspnea symptoms (COPD assessment test score >10 or Modified Medical Research Council Dyspnea Scale score ≥2) and a history of exacerbations can benefit from triple therapy. Triple therapy can improve pulmonary function, breathlessness, dyspnea, and quality of life and lower the risk of exacerbations compared to LAMA alone, LABA/LAMA and LABA/ICS1–6
Triple therapy can be prescribed as an “open triple”, defined as the addition of an ICS to LAMA/LABA or the addition of a LAMA to ICS/LABA. Single-inhaler triple therapy is also called closed triple therapy or fixed-dose triple therapy, such as the combination of beclomethasone dipropionate/formoterol fumarate/glycopyrronium, budesonide/glycopyrrolate/formoterol fumarate, or fluticasone furoate/umeclidinium/vilanterol. Two large one-year randomized controlled trials (IMPACT and ETHOS) showed that triple therapy not only reduced acute exacerbations but also improved dyspnea symptoms, lung function, and quality of life and showed a beneficial effect in reducing mortality compared with LAMA/LABA.7,8
In a real-world study of COPD treatment, triple therapy initiation was not more effective than dual bronchodilator use in reducing mortality.9 Another real-world study enrolled a cohort of patients with COPD from 2002 through 2015 from the UK’s Clinical Practice Research Datalink and showed that triple therapy was generally as effective as dual bronchodilators, but their study did not mention mortality.10 Suissa et al9 used the United Kingdom’s Clinical Practice Research Datalink and found that triple therapy for patients with COPD was not more effective than dual bronchodilators in reducing all-cause mortality. Our study used real-world data from Taiwan.
Patients in double-blind randomized controlled trials tend to have higher treatment adherence than those in clinical practice, and they agree with some aspect of the treatment; in addition, such patients have fewer comorbidities to limit the implication of competing risks. The effectiveness of treatment as evaluated in the real world can supplement results from conventional randomized controlled trials by providing a broad overview of therapy in a usual clinical practice setting.11
Therefore, the aim of this real-world study was to assess the impact of triple inhaled therapy on mortality compared with no triple therapy, which means that those patients received LABA/LABA, LABA/ICS, only LAMA, or only LABA. We also showed the characteristics of patients with COPD who received triple inhaled therapy and analyzed their mortality risk.
Methods
Data Source
Data from patients with COPD were collected from Taiwan’s National Health Insurance Research Database (NHIRD). The NHIRD includes more than 99% of Taiwan’s 23 million citizens from Taiwan’s single-payer population insurance program. The diagnosis codes in the NHIRD are based on the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) before 2015 and the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) after 2016. Patients’ sex, age, payments for consultations, and prescription details are also included in this claims database. The NHIRD is managed by the Health and Welfare Data Science Center (HWDC) to integrate health-related databases. For research purposes, the HWDC releases the databases to the public in a deidentified and anonymized format. This study was conducted in compliance with the Declaration of Helsinki of 1964 and was approved by the Ethics Committee of the Institutional Review Board of Chi-Mei Hospital. The requirement for informed consent was waived by the Research Ethics Committee of Chi Mei Hospital.
Study Population
Patients with new-onset COPD (ICD-9-CM codes 490–492 and 496 or ICD-10-CM codes J41-J44) from January 2005 to December 2016 were enrolled in this study. These diagnosis codes included chronic bronchitis (ICD-9-CM codes 490–491; ICD-10-CM codes J41-J42), emphysema (ICD-9-CM code 492; ICD-10-CM code J43), and other chronic obstructive pulmonary disease (ICD-9-CM code 496; ICD-10-CM code J44). To identify patients with COPD in this study, patients over 40 years of age were included, and those patients without any diagnosis records in inpatient or outpatient claims before the index date (COPD diagnosis) were excluded. Patients with missing data were excluded to avoid incomplete information from the claims data. All study subjects were divided into two groups: COPD patients who received triple therapy (study cohort) and those who did not (comparison cohort). Triple therapy was defined according to the Anatomical Therapeutic Chemical (ATC) Classification System, in which drugs are divided into different groups according to the organ or system on which they act and their main therapeutic use and pharmacological and chemical properties.12 The inception time for the case cohort was defined as the date when COPD patients started receiving triple therapy in the database. To ensure proper matching and avoid potential bias, the inception date for the controls was assigned based on the date when matched COPD patients started receiving triple therapy.
The comparison cohort included COPD patients who did not receive triple therapy, which means that they may have received LABA/LABA, LABA/ICS, only LAMA, or only LABA. All patients were followed up until death or the end of the study date, 2016/12/31. The median follow-up time was 32.56 months for patients who did not receive triple therapy and 29.26 months for those who did receive triple therapy.
To reduce potential selection effects between the study cohort and comparison cohort, each patient who received triple therapy was one-to-one matched according to age, sex, and COPD exacerbations to each patient who did not receive triple therapy. COPD exacerbations were defined as having one or more COPD diagnosis codes for emergency visits, outpatient visits or inpatient admission within the 12-month period before the index COPD diagnosis date. The flowchart of the study subject selection process is illustrated in Figure 1.
 |
Figure 1 Flowchart showing the patient selection process for analysis. |
Outcome and Measurements
The primary outcome of this study was mortality, which was identified using Taiwan’s cause-of-death database. All patients were classified into three age groups: 40–59 years, 60–74 years, and ≥75 years. The comorbidities among these COPD patients were identified by the ICD-9-CM or ICD-10-CM, and the comorbidities of interest included acute respiratory failure, pneumonia, lung cancer, thoracic malignancies, bronchiectasis, hypertensive diseases, ischemic heart disease, heart failure, stroke, myocardial infarction, cancer (except lung and thoracic), diabetes mellitus, renal diseases, and dementia/Alzheimer’s disease. All ICD-9-CM and ICD-10-CM codes for the listed comorbidities are presented in Supplementary Table 1.
Statistical Analysis
The differences in continuous variables and categorical variables between the COPD patients who received triple therapy and those who did not were evaluated using Student’s t test and Pearson’s chi-square test, respectively. The trend in mortality was plotted by the Kaplan–Meier method with the Log rank test to compare the difference between COPD patients who received triple therapy and those who did not. Cox proportional regression was used to estimate the relative risk of mortality with hazard ratios (HRs) and 95% confidence intervals (CIs) after adjusting for the selected variables. SAS statistical software version 9.4 (SAS Institute, Inc., Cary, NC, USA) was used to conduct all analyses. Statistical significance was set at a p value < 0.05.
Results
Study Subjects
Initially, 1,335,247 COPD patients who were regularly followed up for more than 1 year prior to the index date were identified from the databases. We excluded patients who used triple therapy before the index date and who were matched by age, sex, and exacerbations from the index date to the initiation of triple inhaled therapy for COPD. A total of 19,358 COPD patients were included in this study. Figure 1 shows the flowchart of this study.
Among the patients, 5044 (26.06%) were between 40–59 years old, and 9618 (49.68%) and 4696 (24.26%) patients were between 60–74 years old and ≧ 75 years old, respectively. Males accounted for 84.89%, and patients with a history of exacerbations accounted for 73.78%. Patients who received triple therapy had higher mortality and incidence rates of acute respiratory failure and pneumonia than those who did not receive triple therapy, with 24.96% vs 16.89%, 3.16% vs 2.47, and 25.59% vs 23.91%, respectively. The prevalence rates of certain comorbidities were also higher among COPD patients who received triple therapy than among those who did not receive triple therapy. These comorbidities included lung cancer, thoracic malignancies, bronchiectasis, and heart failure (Table 1).
 |
Table 1 Characteristics of Patients with COPD with or Without Triple Therapy |
Mortality Risk Between Patients with and without Triple Therapy
The risk of mortality was higher among COPD patients who received triple therapy than among those who did not receive triple therapy, with crude hazard ratios, fully adjusted model hazard ratios and stepwise approach reduced hazard ratios of 1.568 (95% CI, 1.500–1.639), 1.675 (95% CI, 1.596–1.757), and 1.677 (95% CI, 1.599–1.76), respectively. A history of acute respiratory failure and pneumonia also increased the risk of mortality, and the fully adjusted model hazard ratios were 1.797 (95% CI, 1.632–1.978) and 1.275 (95% CI, 1.211–1.342), respectively. In the fully adjusted model, some comorbidities were associated with a higher risk of mortality among COPD patients who received triple therapy than among those who did not receive triple therapy. These comorbidities included thoracic malignancies, hypertension, ischemic heart disease, heart failure, stroke, cancer (except lung and thoracic cancer), diabetes mellitus, renal diseases, and dementia/Alzheimer’s disease (Table 2).
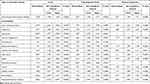 |
Table 2 The Mortality Risk Ratio Between COPD Patients Who Received Triple Therapy and Those Who Did Not |
Mortality Risk Among Patients with Triple Therapy
Among COPD patients who received triple therapy, a history of acute respiratory failure and pneumonia increased the risk of mortality in the fully adjusted model, and the hazard ratios were 1.48 (95% CI, 1.294–1.693) and 1.275 (95% CI, 1.192–1.363), respectively. In the fully adjusted model, comorbidities, including thoracic malignancies, hypertensive diseases, heart failure, stroke, cancer (except lung and thoracic cancer), renal diseases, and dementia/Alzheimer’s disease, were associated with a higher risk of mortality among COPD patients who received triple therapy (Table 3).
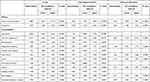 |
Table 3 COPD Patients Who Received Triple Therapy Only |
Kaplan‒Meier Curve
Figure 2 shows the Kaplan‒Meier curve and estimated survival function by plotting estimated survival probabilities against the time trend of mortality between COPD patients who received triple therapy and those who did not receive triple therapy.
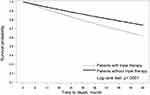 |
Figure 2 The trend in mortality between COPD patients who received triple therapy and patients who did not receive triple therapy. |
Discussion
This retrospective cohort study evaluated the risk of mortality among patients with COPD who received triple therapy compared with those who did not receive triple therapy. After matching for age, sex and history of exacerbations, we found that patients who received triple therapy had an increased risk of mortality compared with those who did not receive triple therapy during a real-world 5-year observation period. A history of acute respiratory failure and pneumonia had a significant effect on mortality among patients with COPD who received triple therapy.
A randomized trial (IMPACT)7 involving patients with COPD who used a once-daily combination of triple therapy showed that all-cause mortality was significantly lower in the groups that received fluticasone furoate. Patients in the triple therapy group had a lower mortality rate than those in the umeclidinium/vilanterol group, with a hazard ratio of 0.58 (95% CI, 0.38 to 0.88; P=0.01).7 However, the Study to Understand Mortality and Morbidity in COPD (SUMMIT)13 enrolled moderate COPD patients with heightened cardiovascular risk and did not show a significant difference in the reduction in mortality among patients who received fluticasone furoate/vilanterol. Why did the IMPACT study show improved survival among patients with COPD? It is possible that the IMPACT study enrolled patients with more severe lung function and a higher risk of exacerbations than did the SUMMIT study. Patients in the IMPACT study had a forced expiratory volume in 1 second (FEV1) < 50% of the predicted normal value and a history of at least one moderate or severe exacerbation or an FEV1 of 50 to 80% of the predicted normal value and at least two moderate exacerbations or one severe exacerbation during the previous year. Inhaled corticosteroids were beneficial in the population with severe airway obstruction and frequent exacerbations. In addition, the peripheral blood eosinophil count was an important guide for prescribing ICSs for COPD patients.14 The significantly better efficacy of regimens containing ICSs in lowering rates of moderate and severe exacerbations than that of a LAMA/LABA bronchodilator was directly proportional to blood eosinophil count.15
Another study, ETHOS (Efficacy and Safety of Triple Therapy in Obstructive Lung Disease), showed that all-cause mortality in the 320-μg budesonide triple therapy group was significantly lower than that in the glycopyrrolate–formoterol group, but there was no statistically significant difference between the 320-μg budesonide triple therapy group and the budesonide–formoterol group.8 The study showed reduced mortality among COPD patients on triple therapy, but the results were somewhat questionable, as the sample sizes were insufficient for detecting a statistically significant difference between the triple therapy and LAMA/LABA groups, indicating that the evidence for mortality was relatively weak.16 The low mortality rate among COPD patients who received triple therapy should be interpreted with caution, and it is possible that these findings were weak. Further studies are needed to investigate the reasons for this finding.
There are some possible reasons to explain why patients with COPD who received triple therapy had higher mortality rates than those who did not receive triple therapy. First, patients with COPD who receive triple therapy may have severe or very severe airflow obstruction. FEV1 can be used to quantify COPD severity and has been reported in previous COPD guidelines.17 A decreased FEV1 is related to mortality in the general population18 and among patients with COPD.19 Lung function can be used not only to measure COPD staging but also to predict mortality among patients with COPD.20,21 Second, patients who received triple therapy in our study had higher prevalence rates of lung cancer, thoracic malignancy and heart failure than those who did not receive triple therapy. These comorbidities may have contributed to the high mortality rates. Previous studies showed that only 58% of patients with COPD had COPD listed on their death certificates,22 and the cause of death may have been related to underlying patient comorbidities. COPD is a systemic inflammatory disease, and patients are likely to have multiple comorbidities, particularly cancer and coronary artery disease, which may lead to death. In the TORCH trial of 6184 patients with moderate-to-severe COPD, there were 911 deaths during the study period, with respiratory disease (35%), cardiovascular disease (26%) and cancer (21%, most commonly lung cancer) accounting for the three most common causes of death.23 In our study, lung cancer, thoracic cancer and heart failure may have contributed to the high mortality rate among patients with COPD who received triple therapy.
The strength of this study was the inclusion of a large real-world COPD population, which provided data from different people on a very important and hot topic: mortality among patients with COPD.
There are also some limitations of our study. First, in the NHIRD, pulmonary function, mMRC (Modified Medical Research Council) Dyspnea Scale and eosinophil data were lacking and could not be used to further analyze the relationship between pulmonary function, the mMRC Dyspnea Scale, blood eosinophils and mortality.
Second, this was an observational study, which could establish only that associations were present between COPD treated with triple therapy and mortality but could not prove that the associations represented cause-and-effect relationships. Confounding factors that are present in health care databases and observational studies are not always evident, and statistics cannot be adjusted for these variables. Confounding by indication may have occurred in this study when a patient’s condition was an indication for the use of triple therapy. Patients with more severe COPD are likely to receive triple therapy, and compared with other treatments, COPD treated with triple therapy appears to result in poorer outcomes. To avoid this bias, we adjusted for age, sex, and exacerbations among patients with COPD. Third, some of the COPD patients may have been misclassified as having no COPD. The addition of ICSs to bronchodilators improved cardiovascular mortality in randomized controlled trials. In this study, the triple therapy group had more cardiovascular comorbidities. Nevertheless, even after adjusting for comorbidities, triple therapy was associated with increased mortality. This suggests that the potential benefits of triple therapy observed in previous RCTs may not necessarily translate to real-world settings, and further research is needed to better understand the underlying mechanisms and potential factors that contributed to the observed associations. Finally, although we employed matching techniques to reduce the potential impact of confounding factors, such as differences in baseline characteristics between the triple therapy group and the control group, it is still possible that some unmeasured confounding variables may exist. For instance, the triple therapy group may have had a higher proportion of symptomatic patients with poor exercise capacity, which could have potentially affected the study outcomes. In future research, additional variables can be included in the analysis to more comprehensively evaluate the differences between these two groups.
In conclusion, our study provided real-world data regarding COPD patient characteristics in triple therapy usage and their mortality risk derived from large administrative databases over a 5-year period; this study showed an association of triple therapy with increased mortality.
Acknowledgment
The abstract for this paper was presented at a 2022 Annual Congress of Taiwan Society of Pulmonary and Critical Care Medicine conference.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–1084.
2. Vestbo J, Papi A, Corradi M, et al. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomised controlled trial. Lancet. 2017;389(10082):1919–1929.
3. Singh D, Papi A, Corradi M, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting beta2- agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388(10048):963–973.
4. Frith PA, Thompson PJ, Ratnavadivel R, et al. Glycopyrronium once-daily significantly improves lung function and health status when combined with salmeterol/fluticasone in patients with COPD: the GLISTEN study, a randomised controlled trial. Thorax. 2015;70(6):519–527.
5. Lipson DA, Barnacle H, Birk R, et al. FULFIL Trial: once-Daily Triple Therapy for Patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2017;196(4):438–446.
6. Siler TM, Kerwin E, Singletary K, Brooks J, Church A. Efficacy and Safety of Umeclidinium Added to Fluticasone Propionate/Salmeterol in Patients with COPD: results of Two Randomized, Double-Blind Studies. COPD. 2016;13(1):1–10.
7. Lipson DA, Barnhart F, Brealey N, et al.; IMPACT Investigators. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378:1671–1680.
8. Rabe KF, Martinez FJ, Ferguson GT, et al.; ETHOS Investigators. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383:35–48.
9. Suissa S, Dell’Aniello S, Ernst P. Triple Inhaler versus Dual Bronchodilator Therapy in COPD: real-World Effectiveness on Mortality. COPD. 2022;19(1):1–9.
10. Suissa S, Dell’Aniello S, Ernst P. Comparative Effects of LAMA-LABA-ICS vs LAMA-LABA for COPD: cohort Study in Real-World Clinical Practice. Chest. 2020;157(4):846–855.
11. Kim HS, Lee S, Kim JH. Real-world Evidence versus Randomized Controlled Trial: clinical Research Based on Electronic Medical Records. J Korean Med Sci. 2018;33(34):e213.
12. Gerhard N. Anatomical Therapeutic Chemical Classification System (ATC). Dictionary of Pharmaceutical Medicine. Vienna: Springer; 2009:8.
13. Vestbo J, Anderson JA, Brook RD, et al. Fluticasone furoate and vilanterol and survival in chronic obstructive pulmonary disease with heightened cardiovascular risk (SUMMIT): a double-blind randomised controlled trial. Lancet. 2016;387:1817–1826.
14. Ashdown HF, Smith M, McFadden E, Pavord ID, Butler CC. Mona Bafadhel. ERJ Open Res. 2022;8:00606–2021.
15. Pascoe S, Barnes N, Brusselle G, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med. 2019;7(9):745–756.
16. Rogliani P, Calzetta L. Mortality in ETHOS: a Question of “Power”. Am J Respir Crit Care Med. 2021;203(7):926–927.
17. Rabe KF, Hurd S, Anzueto A, et al.; Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555.
18. Bang KM, Gergen PJ, Kramer R, Cohen B. The effect of pulmonary impairment on all-cause mortality in a national cohort. Chest. 1993;103(2):536–540.
19. Mannino DM, Buist AS, Petty TL, Enright PL, Redd SC. Lung function and mortality in the United States: data from the First National Health and Nutrition Examination Survey follow up study. Thorax. 2003;58(5):388–393.
20. Anthonisen NR, Wright EC, Hodgkin JE. Prognosis in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1986;133(1):14–20.
21. Traver GA, Cline MG, Burrows B. Predictors of mortality in chronic obstructive pulmonary disease. A 15-year follow-up study. Am Rev Respir Dis. 1979;119(6):895–902.
22. Drummond MB, Wise RA, John M, Zvarich MT, McGarvey LP. Accuracy of death certificates in COPD: analysis from the TORCH trial. COPD. 2010;7(3):179–185. doi:10.3109/15412555.2010.481695
23. McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA. Ascertainment of cause-specific mortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax. 2007;62(5):411–415.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
