Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Real-Time Hemodynamic Changes in the Prefrontal and Bilateral Temporal Cortices During Intradermal Acupuncture for Major Depressive Disorder: A Prospective, Single-Center, Controlled Trial Protocol
Authors Xiong S, Tu M , Wu X, Qu S, Chen N, Jin J, Rong H, Pei S, Fang J, Shao X
Received 16 August 2023
Accepted for publication 17 November 2023
Published 1 December 2023 Volume 2023:19 Pages 2627—2638
DOI https://doi.org/10.2147/NDT.S435617
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Taro Kishi
Sangsang Xiong,1,* Mingqi Tu,1,* Xiaoting Wu,1 Siying Qu,1 Nisang Chen,1 Junyan Jin,1 Haiqin Rong,1 Shuangyi Pei,2 Jianqiao Fang,1 Xiaomei Shao1
1Key Laboratory for Research of Acupuncture Treatment and Transformation of Emotional Diseases, Key Laboratory of Acupuncture and Neurology of Zhejiang Province, The Third Clinical Medical College, Zhejiang Chinese Medical University, Hangzhou, People’s Republic of China; 2The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaomei Shao; Jianqiao Fang, Zhejiang Chinese Medical University, No. 548, Binwen Road, Binjiang District, Hangzhou City, Zhejiang Province, People’s Republic of China, Tel +86 189 5713 0287, Email [email protected]; [email protected]
Background: Major depressive disorder (MDD) is highly prevalent, affecting more than 300 million individuals worldwide, and its occurrence may be related to the abnormality of the prefrontal cortex and bilateral temporal cortex. Acupuncture, rooted in the theories of acupoints and meridians, has demonstrated its efficacy in regulating cortical blood flow (CBF) in the brains of MDD patients. As one form of acupuncture, intradermal acupuncture (IA) can alleviate clinical symptoms such as depressive mood and insomnia in MDD patients. However, it remains unknown whether IA will have a specific effect on the prefrontal cortex and bilateral temporal cortex in MDD patients.
Methods: In total, 60 participants will be recruited: 20 healthy control participants and 40 MDD patients. All healthy control participants will be allocated to the control group, whereas the 40 MDD patients will be randomly divided into two groups: the gallbladder meridian acupoint (GBA) group and the non-acupoint (NA) group, at a 1:1 allocation ratio. All groups will undergo a one-time IA intervention while their cortical activity is monitored using functional near-infrared spectroscopy (fNIRS). Total hemoglobin, oxygenated hemoglobin, and deoxygenated hemoglobin of the prefrontal and bilateral temporal cortices will be measured by fNIRS during the test procedure.
Discussion: This trial aims to use fNIRS to compare real-time hemodynamic changes in the prefrontal and bilateral temporal cortices of healthy individuals and MDD patients during IA. The primary objective is to investigate whether MDD patients exhibit specific real-time responses to IA stimulation in these brain regions. The findings from this study will provide clinical data and a possible theoretical basis for the assumption that stimulation of IA may treat MDD by modulating the relevant brain regions.
Trial Registration: The study protocol has been registered in the clinicaltrials.gov with the code NCT05707299.
Keywords: major depressive disorder, intradermal acupuncture, functional near-infrared spectroscopy, prefrontal cortex, temporal cortex
Introduction
Major depressive disorder (MDD) is a prevalent psychiatric condition that is distinguished by a prolonged and pronounced state of low mood, decreased interest, slowed thinking, and, in severe cases, self-harm and even suicide.1 In accordance with the World Health Statistics Report, over 300 million individuals are estimated to suffer from MDD worldwide, and its incidence is showing a year-on-year increase.2
From the perspective of modern medicine, more and more research has explored functional and structural brain abnormalities related to MDD.3 Research implicates dysfunction and structural changes in the prefrontal cortex and temporal lobe, critical areas governing complex cognitive processes, emotions, and language comprehension.4–6 Furthermore, the various elements of MDD exhibit a strong correlation with modifications in cerebral perfusion in the frontal-temporal cortex.7 These results indicate that the structural changes in the prefrontal cortex and bilateral temporal cortex are related to the occurrence of MDD.
From the perspective of traditional Chinese medicine (TCM), acupuncture therapy is founded on the acupoints and meridians theory and has been an effective treatment for MDD to date. At the core of TCM lies the concept of “qi”, a term not conventionally used in western scientific discourse, which refers to the vital energy or life force within the body. Acupuncture is considered to regulate qi and blood by stimulating acupoints, thereby improving physiological functions. Qi and blood are the fundamental substance constituting human body and affects people’s mental state. In modern medicine, qi is the equivalent term for “energy”. Acupuncture achieves clinical efficacy through the excitation of qi in the meridians, and this process is known as deqi. A trial has shown that a single session of acupuncture demonstrated a tendency to enhance the activation of the frontopolar area in patients with severe depression.8 Meanwhile, one case report has shown the mechanism of acupuncture’s efficacy is related to the regulation of cortical blood flow (CBF) in the brain of MDD patients, and the functional near-infrared spectroscopy (fNIRS) test showed an increased CBF in the prefrontal area after 3 months of acupuncture treatment in this patient.9 Therefore, it is highly likely that acupuncture may treat MDD by modulating the prefrontal cortex and bilateral temporal cortex.
Meanwhile, intradermal acupuncture (IA), as one form of acupuncture, can alleviate clinical symptoms such as depressive mood and insomnia in MDD patients.10 IA is an approach that involves the prolonged insertion of needles. It has the advantages of no obvious pain and discomfort, small and lasting stimulation, simple operation, ease of acceptance, and high safety. However, the mechanism of the immediate brain effect of IA remains unknown.
Therefore, it is possible that patients with MDD have a specific response to IA stimulation, and that this response would be reflected in hemodynamic changes in the prefrontal and bilateral temporal cortices, but there have been no studies on this.
The current mature fNIRS technology provides a reliable method for such studies. fNIRS refers to near-infrared spectroscopy (NIRS) for functional neuroimaging purposes. NIRS can use near-infrared (NIR) light to constantly and non-invasively track changes in tissue chromophore concentrations, which in turn can calculate changes in hemoglobin concentrations. In the past 20 years, fNIRS has been increasingly used to investigate cerebral hemodynamic changes in the cerebral cortex during acupuncture stimulation. A systematic review shows that many studies have utilized fNIRS signals for the purposes of diagnosing MDD, establishing correlations with depression symptomatology, and monitoring treatment response.11
In summary, this study intends to use fNIRS as the detection technique and the cortical hemodynamics of the prefrontal cortex and bilateral temporal cortex as the clinical observation index to investigate whether both cortices in patients with MDD respond specifically to IA stimulation.
Method and Analysis
Study Design
The study is designed as an interventional, prospective, controlled, single-center clinical trial. In total, 60 participants will be recruited: 20 healthy control participants and 40 MDD patients. All healthy control participants will be allocated to the control group, whereas the 40 MDD patients will be randomly divided into two groups: the gallbladder meridian acupoint (GBA) group and the NA group, at a 1:1 allocation ratio. The flow chart of the study process is shown in insert Figure 1. The schedule of enrolments, interventions and assessments is displayed in Table 1. The present protocol has been formulated in accordance with the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) 2010 checklist and the SPIRIT reporting guidelines.12,13
 |
Table 1 Schedule of Enrolment, Detection, and Assessments |
Participant Enrollment
MDD patients will be enrolled from the Third Affiliated Hospital of Zhejiang Chinese Medical University, and healthy participants will be enrolled from the community. Enrollment methods will mainly include advertisements and referrals from doctors in the psychology department clinics. Participant eligibility will be assessed by the researcher based on the following criteria.
Inclusion and Exclusion Criteria
The inclusion and exclusion criteria are summarized in detail in Table 2.
 |
Table 2 The Inclusion Criteria and Exclusion Criteria of Two Groups |
Discontinuation Criteria
- Subjects who develop serious complications or other serious illnesses during the study that require emergency measures.
- Subjects who experience significant adverse reactions during the course of the trial and are evaluated by a specialist to determine whether to continue or terminate the trail.
- Subjects who have other reasons for not being able to continue the study.
- Accidents such as equipment malfunction during the operation, which prevent the continuation of the trial or have a significant impact on the trail results.
Elimination Criteria
- Subjects with poor compliance during the study period, which may affect the validity and accuracy of data acquisition.
- Subjects who fail to meet the predetermined inclusion criteria or meet the established exclusion criteria and are inadvertently enrolled should be promptly excluded.
- Those whose detected fNIRS images are incomplete or have abnormal signal shadows due to various reasons.
- Those who were unable to complete the study for personal reasons after enrollment and voluntarily withdrew from the trial.
- Subjects who develop a sudden illness during the study and need to receive other treatments.
- Subjects who experience significant adverse reactions during the course of the trial and are deemed unsuitable to continue their participation.
Randomization and Allocation Concealment
In this study, MDD patients will receive randomized sequences generated by the SPSS software (version 26.0) random number generator program and distributed in a 1:1 ratio to GBA group and NA group. The 20 healthy control participants will be allocated to the control group.
Blinding
The recruitment of participants, administration of acupuncture procedures, evaluation of outcomes, and statistical analysis will be performed by different researchers independently. Only subject recruiter will know the allocation information, subject recruiter will not participate in all subsequent sessions. Acupuncture manipulators will only know the subject’s name, age, and gender and will be prohibited from asking the subject any other relevant information. Assessors who are not aware of the allocation specifics will perform the outcome assessment. Statistics will be performed by statisticians who are not aware of the allocation information.
Intervention
Three groups will accept the interventions as follows.
Acupoint Selection
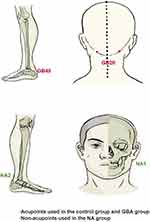
The location standard of acupoints is based on the National Standard Nomenclature and Location of Acupuncture Points 2021 (GB/T 12346-2021). Bilateral Fengchi (GB20) and Qiuxu (GB40) will be chosen for both the control group and GBA group, whereas the NA Group will receive IA at bilateral non-acupoints designated as NA1 and NA2. Locations of acupoints are summarized in Figure 2 and Table 3, and locations of non-acupoints are summarized in Figure 2 and Table 4.
 |
Table 3 The Location of Acupoints |
 |
Table 4 The Location of Non-Acupoints |
Selection of Experimental Equipment
Figure 3 shows the structure of the equipment used in this study. Figure 3a shows the structure of fNIRS, and Figure 3b and c are the front and back of IA. The tack needles (PYONEX, diameter of 0.2m, length of 1.5mm; Seirin Corporation, Shizuoka, Japan) will be used. The oxygenation data will be collected by the Hitachi ETG-4100 fNIRS instrument (52CH). The instrument consists of one set of the main body of the Optical Topographer Measurement Device, three sets of detachable transceiver optical fibers, and one silicone probe holder. It utilizes a 2-wavelength NIR semiconductor laser diode as the NIR light source and an avalanche photomultiplier tube as the detector. It measures the absorption of NIR light at two wavelengths (695 nm and 830 nm) and calculates the related hemoglobin and deoxyhemoglobin density using the modified Beer-Lambert Law.
 |
Figure 3 The structure of the equipment. Notes: (a) shows the structure of fNIRS, and (b and c) are the front and back of IA. |
Operation
Participants will receive IA stimulation at specified acupoints based on their assigned group. The subject will put on a headgear before signal gathering that is covered in numerous NIR light sensors that encompass the prefrontal area and both temporal regions. The NIR light sensors will be positioned on the head in accordance with the 10–20 international system. There are 11S-D channels in the prefrontal lobe and 20S-D channels in the right and left temporal lobes.
After acupoint localization and routine disinfection, press IA to insert the acupoints and hold them in the skin. Participants will be requested to maintain their eyes closed and silent throughout the intervention, and to prevent bodily activity as much as possible. All subjects will receive the IA in the same order, and follow the steps of “resting- stimulating-preparing-stimulating-resting” to complete the IA operation alternately.
Subjects will wear the headgear throughout the procedure and the fNIRS signal will be collected throughout. Before IA, the signals will be recorded for 60s to establish the baseline and then stimulate the bilateral head acupoints (GB20/NA1) for 2 mins. After stopping stimulation, wait for fNIRS signals to return to the resting level (ie, the preparation period), then stimulate the bilateral lower limb acupoints (GB40/NA2) for another 2 mins, and finally stop the NIR scanning when the image of fNIRS returns to the resting level. After the intervention, the needle will be removed. The whole process is summarized in insert Figure 4.
 |
Figure 4 Study Procedures. |
Outcome Measures
- Oxygenated hemoglobin (Oxy-Hb)
Oxy-Hb is the combination of hemoglobin plus oxygen. The cerebral oxygenation variables at each channel are determined through the utilization of fNIRS signals in accordance with the Beer-Lambert law. This methodology enables the characterization of alterations in the levels of oxy-hemoglobin.
Deoxy-Hb is the unbound form of hemoglobin with oxygen. The cerebral oxygenation variables at each channel are determined through the utilization of fNIRS signals in accordance with the Beer-Lambert law, in order to characterize the alterations in deoxy-Hb concentrations.
The calculation of Total-Hb involves the summation of the levels of both Oxy-Hb and Deoxy-Hb [The sum of Deoxy-Hb and Oxy-Hb is equal to Total-Hb]. The distributions of total-Hb are used as measures of cortical activation.
Outcome measures will be assessed during the whole IA operation.
Evaluation
To guarantee a smooth workflow, all instruments, equipment, and reagents used in clinical trials for the different tests will meet strict quality standards. Each member of the research team will undergo a training workshop prior to recruitment. All personnel must follow the study protocol and understand the clinical trial management procedure. The acupuncturist performing the treatment must have a certified medical practitioner certificate from the People’s Republic of China’s Ministry of Health and at least three years of actual clinical experience. To guarantee the accuracy of data, every observation and abnormal finding in studies will be meticulously confirmed and recorded in a timely manner. The research assistant will oversee data gathering and ensure that the data is of high quality. The unprocessed information from clinical studies must be used to draw a variety of conclusions. To reduce patient withdrawals, study processes should be simplified, excellent communication with participants must be maintained, and allowances must be disbursed on time. The reasons for withdrawal should be provided, and the withdrawal rate should be statistically assessed no matter when it happens.
Sample Size Estimation
In comparison to clinical studies, this is a fundamental study of IA combined with fNIRS, so there is no universal norm or formula for determining sample size. Three groups will each contain 20 cases, taking into account previous studies of fNIRS combined with acupuncture at home and abroad and the pre-test situation.14–16
Statistical Analysis
Our study follows the intention-to-treat (ITT) principle, which guides our analytical approach. Under this framework, any participants who withdraw from the study prior to completion will remain grouped according to their original assignment, regardless of compliance with the intervention protocol. The statistical analysis will be performed by third-party statisticians using SPSS 17.0 for Windows (SPSS Inc., Chicago, IL, USA). To determine whether there were any variations in the two groups’ baseline characteristics, the chi-square test was applied. For categorical data, chi-square tests will be used for between-group comparisons. Data with a skewed distribution will be presented as the median with 95% confidence intervals, while data with a normal distribution will be presented as the mean ± standard deviations. One-way Analysis of variance will be used to assess differences in groups of data that had a normal distribution, and a nonparametric test will be employed if the data does not conform to a normal distribution or exhibits non-uniform variance. Statistical significance will be deemed to be present when the two-tailed tests yield a P value of less than 0.05, while a high level of statistical significance was observed when P < 0.01 or P < 0.001.
Discussion
The available data indicates that the lifetime prevalence of MDD in China during the year 2019 has reached a significant proportion of 6.8%, with a total number of more than 95 million.16 Furthermore, MDD serves as a primary indicator of suicidal tendencies, resulting in a decrease in life span and contributing to premature mortality rates.17
In our experiment, the acupoint prescription is meticulously planned, and all acupoints in GBA group and control group are taken from gallbladder meridian (GB). According to TCM, “gallbladder dominating decision” is one of the significant theories derived from the “Huangdi’s Internal Classic”, “decision” refers to the final decision of people’s various emotional activities. When the gallbladder loses control over the dominant decision, it can lead to qi stagnation. Energy metabolism in the living body is said to become stagnant under the state known as qi stagnation, which is intricately linked to the pathogenesis of MDD. The GB circles the lateral head, and the area of the GB on the head corresponds to the body surface projection of the prefrontal cortex and temporal cortex. These two brain regions are known to play a significant role in MDD.
Based on a research and analysis of modern acupuncture articles as well as previous clinical studies, acupoint GB20 and GB40 are used more frequently in clinical practice among the GB acupoints. The pathogenesis of MDD remains unclear and various hypotheses have been proposed to date. The monoamine hypothesis is a primary hypothesis of depression, positing that depression arises from changes in monoamine levels, with a particular emphasis on the reduction of 5-HT in the pathophysiology of depression.18 According to a literature review, neuroreceptor PET imaging has shown that MDD is linked with reduced 5-HT(1A) binding potential in the medial prefrontal cortex and medial temporal lobe.19 According to the TCM theory that “the meridians pass through and the main treatment reaches”, stimulation of GB20 and GB40 can increase central 5-HT levels, and abnormal reduction of 5-HT is pathophysiologically linked to depression.20 Thus, GB20 and GB40 from both sides are selected.
To eliminate potential confounding factors caused by the IA needles, we implement NA group in this experiment. After reviewing traditional Chinese medicine reference books and modern acupuncture articles, we exclude acupoints known to impact real-time hemodynamic changes in the prefrontal cortex and bilateral temporal cortex as well as those demonstrating clinical efficacy in treating MDD.21 Following exclusion of these acupoints, Quanliao (SI18) located on the head and Shuiquan (KI5) on the lower limbs are selected, and locations 3mm away from each of these points are defined as NA used in the NA group.
fNIRS is a non-invasive modality that enables clear visualization of cerebral hemodynamic changes of interest. It is frequently employed in studies pertaining to depression or subthreshold depression to ascertain effectiveness. In addition, the diagnosis of MDD and the evaluation of its efficacy are usually subjective indicators and lack an objective indicator. From the technical standpoint, this study constitutes an invaluable addition to the investigation of prefrontal cortex and bilateral temporal cortex functionality in individuals diagnosed with MDD. From the perspective of the study results, it can provide clinical data and a possible theoretical basis for the assumption that stimulation of GB acupoints may treat MDD by modulating the relevant brain regions.
The development of brain structures involved in regulating emotions persists until the mid-twenties. However, there is a paucity of research that has investigated the crucial age bracket of 15–22, during which some of the most advanced high-level neurodevelopment takes place, a cohort comprising individuals aged between 15 and 22 years was chosen.22 To avoid the effects of drugs on the brain, enrolled participants also should not take antidepressants or antipsychotic drugs for at least 4 weeks before enrollment.23 In a similar vein, not all patients’ language centers are found in the left hemisphere. Although the language centers of most left-handed people are in the left hemisphere, some do have them in the right. As a result, we have only included right-handed patients in this investigation.
Limitations
First of all, this study is a basic one that uses IA combined with fNIRS technology for a short time and with a small sample size. In subsequent studies, the sample size will be increased to further investigate the differences in cortex response to IA in MDD patients in different evidence types, genders, and age levels and to more thoroughly reveal the real-time hemodynamic changes in the prefrontal cortex and bilateral temporal cortex during IA in MDD patients through fNIRS technology.
Secondly, this study mostly focuses on real-time hemodynamic changes in the prefrontal cortex and bilateral temporal cortex during IA in MDD patients. However, MDD is a type of disease with a long course and multiple attacks. This study focuses on whether a single IA stimulation can cause changes in the prefrontal cortex and bilateral temporal cortex. And such a short and single session of IA stimulation maybe not be enough to induce clinical improvement in dysfunction. In follow-up studies, the relationship between the clinical efficacy of IA and MDD-related brain regions will be investigated through the long-term IA course so as to explore the central mechanism of IA treatment for MDD patients and to evaluate the MDD symptoms before and after therapy.
Conclusion
This prospective, controlled, single-center clinical trial will utilize fNIRS to assess the real-time hemodynamic changes in the prefrontal cortex and bilateral temporal cortex during IA intervention in both healthy participants and MDD patients. By analyzing the response patterns in these cortices, this trial aim to investigate whether MDD patients have specific real-time responses to IA stimulation, which will hopefully provide new insights into the therapeutic mechanisms of IA and will contribute to the diagnosis and treatment of MDD.
Abbreviations
MDD, Major depressive disorder; CBF, Cortical blood flow; IA, Intradermal acupuncture; fNIRS, Functional near-infrared spectroscopy; TCM, Traditional Chinese medicine; NIRS, Near-infrared spectroscopy; NIR, Near-infrared; STRICTA, Standards for Reporting Interventions in Clinical Trials of Acupuncture; GB20, Fengchi; GB40, Qiuxu; Oxy-Hb, Oxygenated hemoglobin; Deoxy-Hb, Deoxygenated hemoglobin; Total-Hb, Total hemoglobin; GB, Gallbladder meridian; SI18, Quanliao; KI5, Shuiquan; NA, non-acupoints.
Trial Status
Participant recruitment started in February 2023 and is still recruiting patients.
Data Sharing Statement
Datasets obtained during this study can be provided by the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The current version was created in accordance with the SPIRIT Statement and approved on December 08, 2022. Ethics approval (No. ZSLL-ZN-2022-037-01) has been obtained from the Ethics Committee of the Third Affiliated Hospital of Zhejiang Chinese Medical University. Prior to implementation, protocol revisions will be submitted for approval by institutional review board. This trial will be carried out in compliance with the Declaration of Helsinki and Chinese clinical research norms and regulations. Before the enrollment of any participant, informed consent will be signed. The findings will be disseminated at international conferences and submitted to scholarly journals for peer-review on a global level.
Acknowledgments
We acknowledge the help and contributions from Key Laboratory of Acupuncture and Neurology of Zhejiang Province, Department of Neurobiology and Acupuncture Research. We also acknowledge the support from Key Laboratory for Research of Acupuncture Treatment and Transformation of Emotional Diseases.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The trial was supported by the Zhejiang Provincial TCM Science and Technology Program - Zhejiang Provincial TCM Modernization Special Project (2022ZX010).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sun J, Du Z, Ma Y, et al. Altered functional connectivity in first-episode and recurrent depression: a resting-state functional magnetic resonance imaging study. Front Neurol. 2022;13:922207. doi:10.3389/fneur.2022.922207
2. Collins PY, Patel V, Joestl SS, et al. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi:10.1038/475027a
3. Dean J, Keshavan M. The neurobiology of depression: an integrated view. Asian J Psychiatry. 2017;27:101–111. doi:10.1016/j.ajp.2017.01.025
4. Wang L, Dai W, Su Y, et al. Amplitude of low-frequency oscillations in first-episode, treatment-naive patients with major depressive disorder: a resting-state functional MRI study. PLoS One. 2012;7(10):e48658. doi:10.1371/journal.pone.0048658
5. Pu S, Nakagome K, Yamada T, et al. The relationship between the prefrontal activation during a verbal fluency task and stress-coping style in major depressive disorder: a near-infrared spectroscopy study. J Psychiatric Res. 2012;46(11):1427–1434. doi:10.1016/j.jpsychires.2012.08.001
6. Donix M, Haussmann R, Helling F, et al. Cognitive impairment and medial temporal lobe structure in young adults with a depressive episode. J Affect Disorders. 2018;237:112–117. doi:10.1016/j.jad.2018.05.015
7. Romero K, Black SE, Feinstein A. Differences in cerebral perfusion deficits in mild traumatic brain injury and depression using single-photon emission computed tomography. Front Neurol. 2014;5:5. doi:10.3389/fneur.2014.00005
8. Zhang T, Zhang J, Huang J, Zheng Z, Wang P. Neural activation via acupuncture in patients with major depressive disorder: a functional Near-Infrared Spectroscopy Study. Front Psychiatry. 2021;12:669533. doi:10.3389/fpsyt.2021.669533
9. Chen JK, Tsai WT, Lin SZ, et al. Using radial pulse wave as hemodynamic measurements to quantify effects of acupuncture therapy for patients with traumatic brain injury and ischemia stroke. J Trad Complement Med. 2022;12(6):594–598. doi:10.1016/j.jtcme.2022.08.005
10. Hu R, Tan Q, Chi S, et al. Progress in clinical research on characteristic acupuncture for treating depression. Chin J Pract Integr Tradit West Med. 2022;38(11):2023–2026.
11. Csh H, Lim LJH, Lim AQ, et al. Diagnostic and predictive applications of functional near-infrared spectroscopy for major depressive disorder: a systematic review. Front Psychiatry. 2020;11:378. doi:10.3389/fpsyt.2020.00378
12. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340(1):c869. doi:10.1136/bmj.c869
13. Chan AW, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200. doi:10.7326/0003-4819-158-3-201302050-00583
14. Fernandez Rojas R, Liao M, Romero J, Huang X, Ou KL. Cortical network response to acupuncture and the effect of the hegu point: an fNIRS study. Sensors. 2019;19(2):394. doi:10.3390/s19020394
15. Liu Y, Sun N, Xiong J, et al. Modulation of cerebral cortex activity by acupuncture in patients with prolonged disorder of consciousness: an fNIRS study. Front Neurosci. 2022;16:1043133. doi:10.3389/fnins.2022.1043133
16. Xiang XY. Immediate Responses of Left Dorsolateral Prefrontal Cortex to Acupuncture in Generalized Anxiety Disorder: An fNIRS Study. [master’s thesis]. Chengdu University of Traditional Chinese Medicine; 2017. Available from: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201901&filename=1018954364.nh&v=17.
17. Wang HZ, Luo WL, Zeng NX, et al. Cerebrospinal fluid proteomics reveal potential protein targets of JiaWeiSiNiSan in preventing chronic psychological stress damage. Pharm Biol. 2021;59(1):1063–1074. doi:10.1080/13880209.2021.1954666
18. Wong YK, Wu JM, Zhou G, et al. Antidepressant monotherapy and combination therapy with acupuncture in depressed patients: a Resting-State Functional Near-Infrared Spectroscopy (fNIRS) Study. Neurotherapeutics. 2021;18(4):2651–2663. doi:10.1007/s13311-021-01098-3
19. Bhatt S, Devadoss T, Manjula SN, Rajangam J. 5-HT3 receptor antagonism: a potential therapeutic approach for the treatment of depression and other disorders. Curr Neuropharmacol. 2021;19(9):1545–1559. doi:10.2174/1570159X18666201015155816
20. Florea I, Lindsten A, Baldwin DS, Baldwin DS. Efficacy of vortioxetine on the physical symptoms of major depressive disorder. J Psychopharmacol. 2018;32(10):1086–1097. doi:10.1177/0269881118788826
21. Tu M, Xiong S, Lv S, et al. Acupuncture for major depressive disorder: a data mining-based literature study. NDT. 2023;19:1069–1084. doi:10.2147/NDT.S405728
22. Ekbäck E, Granåsen G, Svärling R, et al. Clinical effectiveness of training for awareness resilience and action online compared to standard treatment for adolescents and young adults with depression: study protocol and analysis plan for a pragmatic, multi-center randomized controlled superiority trial. Front Psychiatry. 2021;12:674583.
23. Haroon E, Daguanno AW, Woolwine BJ, et al. Antidepressant treatment resistance is associated with increased inflammatory markers in patients with major depressive disorder. Psychoneuroendocrinology. 2018;95:43–49. doi:10.1016/j.psyneuen.2018.05.026
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.