Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Real-life data on antibiotic prescription and sputum culture diagnostics in acute exacerbations of COPD in primary care
Authors Bathoorn E, Groenhof F, Hendrix R, van der Molen T, Sinha B, Kerstjens HA , Friedrich AW , Kocks JW
Received 24 August 2016
Accepted for publication 21 October 2016
Published 13 January 2017 Volume 2017:12 Pages 285—290
DOI https://doi.org/10.2147/COPD.S120510
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Erik Bathoorn,1 Feikje Groenhof,2 Ron Hendrix,1,3 Thys van der Molen,2,4 Bhanu Sinha,1 Huib AM Kerstjens,5 Alex W Friedrich,1 Janwillem WH Kocks2,4
1Department of Medical Microbiology, University of Groningen, University Medical Center Groningen, Groningen, the Netherlands; 2Department of Primary Care, University of Groningen, University Medical Center Groningen, Groningen, the Netherlands; 3Department of Pulmonary Diseases and Tuberculosis, University of Groningen, University Medical Center Groningen, Groningen, the Netherlands; 4Department of Medical Microbiology, Certe – Laboratory for Infectious Diseases, Groningen, the Netherlands; 5GRIAC Research Institute, Groningen, University of Groningen, University Medical Center Groningen, the Netherlands
Background: Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) are generally treated with optimization of bronchodilation therapy and a course of oral corticosteroids, mostly without antibiotics. The Dutch guidelines recommend prudent use of antibiotics, with amoxicillin or doxycycline as first choice. Here we evaluate adherence to these guidelines with regard to antibiotic prescription in AECOPD in primary care and the use of sputum cultures.
Methods: We retrospectively analyzed a longitudinal cohort of patients in three primary care practices in the north-eastern region of the Netherlands from 2009 to 2013 (n=36,172 subjects) participating in the Registration Network Groningen. Antibiotics prescribed for AECOPD -10/+28 days from the start date of corticosteroid courses were evaluated. In addition, we assessed regional data on the susceptibility of respiratory pathogens from COPD patients.
Results: We identified 1,297 patients with COPD. Of these, 616 experienced one or more exacerbations, resulting in a total of 1,558 exacerbations, for which 1,594 antibiotic courses were prescribed. The recommended antibiotics doxycycline and amoxicillin accounted for 56% of the prescribed antibiotics overall and for 35% in subsequent antibiotic courses. The alternative choices were not based on culture results because only in 67 AECOPD events (2.9%) sputum samples were taken. Regional data including 3,638 sputum samples showed that pathogens relevant in AECOPD were detected in 19% of cultures.
Conclusion: Our study shows that guidelines regarding the prescription of antibiotics are poorly followed, particularly in recurrent exacerbations. Sputum cultures were performed in a small minority of cases. Performing sputum diagnostics in patients with early treatment failure or a repeated exacerbation when antibiotic treatment is started may further rationalize antibiotic treatment.
Keywords: COPD, exacerbation, antimicrobial stewardship, bacteria, sputum cultures
Introduction
Antimicrobial resistance is a worldwide threat to health. Antimicrobial stewardship programs are essential to withstand the emerging resistance and gain time for the development of new antibiotics. The aims of antimicrobial stewardship are to optimize antibiotic therapy in patients with a bacterial infection with an antibiotic drug that has a spectrum as narrow as possible and to avoid using antibiotics in nonbacterial causes of disease. Acute exacerbations of chronic obstructive pulmonary disease (AECOPD) in primary care are an important field for antimicrobial stewardship because the disease burden is high. In 2009, the average COPD-related hospital admission rate in European Union (EU) member states was 184 per 100,000 population aged ≥15 years.1 The origin of an exacerbation in mild COPD is often nonbacterial.2 In addition, exacerbations, where bacteria are present, are often self-limiting.3 Finally, the treatment of exacerbations with antibiotics is especially evidence based in hospitalized patients showing a limited, short-lived effect on clinical outcome. Antibiotic treatment did not have a beneficial effect on clinical success on day 30 in the inpatient setting.4 Outpatient antibiotic prescription has been associated with the development of resistance, also in Streptococcus pneumoniae, the most important respiratory pathogen.5,6 Nonetheless, antibiotics are widely prescribed for AECOPD in primary care.7
Guidelines by a joint taskforce of European Respiratory Society and European Society for Clinical Microbiology and Infectious Diseases taskforce state that
An antibiotic should be given in exacerbations of COPD in patients with all three of the following symptoms: increased dyspnea, sputum volume, and sputum purulence. In addition, antibiotics should be considered for exacerbations in patients with severe COPD.8
In the Dutch primary care guideline for the treatment of AECOPD restrictive usage of antibiotics is recommended. The guidelines of 2007 state that AECOPD can be treated with oral corticosteroids and optimizing bronchodilator therapy.9 Antibiotics should be used only in patients who have signs of infection (temperature >38°C), in combination with forced expiratory volume in 1 second (FEV1) <30% of predicted, and no recovery after 4 days of prednisolone and proper bronchodilation. In patients with severe COPD and recurrent hospital admission, antibiotics can be started immediately. Both guidelines consider amoxicillin or doxycycline as first choices of antibiotics. This study evaluates antibiotic prescription in COPD exacerbations by primary care physicians based on a real-life data analysis. We assess adherence to local guideline recommendations in choices of antibiotics prescribed for AECOPD and differences in antibiotic prescription between recurrent exacerbations and single exacerbation. In addition, we provide more rationale behind the choices of antibiotics by evaluating the regional epidemiology of respiratory pathogens in sputum from COPD patients.
Methods
We retrospectively analyzed anonymized electronic patient data of a longitudinal cohort of patients in three primary care practices in the north-eastern region of the Netherlands, participating in the Regional Network Groningen, from 2009 to 2013 (n=36,172 subjects). COPD patients were identified by ICPC code R95, which is an international classification system of reason for patient encounter in primary care. Prescription of antibiotics for respiratory indication was identified by disease-specific Anatomical Therapeutic Chemical (ATC) codes R02, R05, R74, R78, R81, R95, and R96. We identified exacerbation episodes in patients aged >40 years diagnosed with COPD based on prescription of a course of oral corticosteroids by ATC code H02. Antibiotic courses were compared to the first day of corticosteroid course. Antibiotic prescriptions for respiratory indications from 10 days before to 28 days after the date of corticosteroid prescription were analyzed. Recurrent exacerbations were defined by prescription of subsequent courses of corticosteroids within 60 days of the first course.10 Patients who suffered from two or more exacerbations in 1 year were characterized as frequent exacerbators.11 Sputum cultures performed in routine practice of the identified COPD patients during exacerbation episodes were assessed for a bacterial etiology as described previously.12 Doxycycline and amoxicillin were considered recommended treatments as per the Dutch primary care guideline for the treatment of AECOPD.
In addition, we assessed the regional epidemiology of antibiotic susceptibility of respiratory pathogens of the north-eastern part of the Netherlands. We analyzed culture results of 3,639 sputum samples from in- and outpatients with COPD from 2014 to 2015 tested in a routine diagnostic laboratory (Certe – Laboratory for Infectious Diseases, Groningen, the Netherlands). Susceptibility patterns of Haemophilus influenzae, S. pneumoniae, and Moraxella catharralis were assessed. Antibiotic susceptibility results were interpreted according to the EUCAST guidelines.13
The Medical Ethics Review Board of the University Medical Center Groningen ascertained that no ethical approval or patient informed consent was required.
Results
We identified 1,297 patents with COPD and at least one exacerbation defined by prescription of a systemic corticosteroid course (Table 1). In total, 1,558 exacerbations were identified, of which 1,135 were single and 423 recurrent exacerbations. Exacerbations were treated with one or more courses of antibiotics in 70% of all exacerbation episodes, adding up to a total of 1,594 courses of antibiotics. Antibiotics for respiratory indications were more often prescribed in recurrent exacerbations compared to single exacerbations (87% versus 64%, respectively; Table 2). Doxycycline was most often prescribed (46% of antibiotic courses), followed by amoxicillin/clavulanic acid (17%), amoxicillin (11%), azithromycin (11%), and clarithromycin (9%). Thus, the recommended antibiotic regimens (doxycycline or amoxicillin) only accounted for 57% of all antibiotics prescribed. When this was subdivided into first course of antibiotics (n=1,081) and subsequent courses (n=513) during an exacerbation episode, recommended regimens accounted for 67% and 35% of antibiotic prescriptions, respectively.
  | Table 1 Patient characteristics and exacerbations |
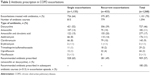  | Table 2 Antibiotic prescription in COPD exacerbations |
Only 74 sputum samples were taken in 67 (4.3%) exacerbation episodes. Of these, in only 24/74 (32% of sputum cultures) potentially pathogenic microorganisms were cultured. H. influenzae was most frequently cultured (n=10) and was tested susceptible to doxycycline in 10/10 and to amoxicillin in 8/10 isolates. Pseudomonas aeruginosa was isolated in five cultures, Enterobacteriaceae aceae in four, Staphylococcus aureus in two, and non-influenzae Haemophilus spp. in two. All P. aeruginosa and E. cloacae were resistant to the initiated antibiotic treatment. However, in none of these cases, antibiotics were adjusted based on culture results. No S. pneumoniae were cultured, which may, in part, be due to the fact that 44% of patients had been treated with antibiotics within 10 days prior to sampling.
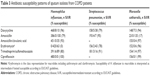
Table 3 shows the results of 3638 sputum cultures from COPD patients in our region. We found that in 19% of cultures, the most relevant pathogens in AECOPD H. influenzae, S. pneumoniae, and/or M. catharralis were isolated. Pathogens of which their role in COPD exacerbations are less well-established as S. aureus, P. aeruginosa, E. cloacae, and Candida spp. were isolated in 31% of cultures. In 50% of cultures, no potential pathogens were found.
Susceptibility results of H. influenzae (n=486) showed that 96% of isolates were susceptible to doxycycline, 79% to amoxicillin, 93% to amoxicillin/clavulanic acid, and 80% to sulfamethoxazole/trimethoprim. Of 204 S. pneumoniae isolates, 79% were susceptible to doxycycline, 95% to amoxicillin, 100% to amoxicillin/clavulanic acid, 91% to sulfamethoxazole/trimethoprim, and 78% to azithromycin. M. catharralis was susceptible to doxycycline in 94% of 158 isolates. Beta-lactamase production is common in M. catharralis, which explains the poor susceptibility to amoxicillin of 17%. M. catharralis showed good susceptibility to amoxicillin/clavulanic acid, macrolides, and sulfamethoxazole/trimethoprim; all were >95%.
Discussion
Real-life data analysis is a valuable tool to evaluate clinical practice and adherence to guidelines in a real-life setting, which cannot be performed in randomized controlled trials (RCTs). This study shows that antibiotics are rather widely prescribed for COPD exacerbations, and that guidelines regarding antibiotic prescription are poorly followed. The reason for the poor adherence is not entirely clear. Nonadherence to first-line antibiotic recommendations cannot be justified by existing sputum culture data since these were collected only in 4.3% of cases.
We found an overall prescription rate of antibiotics for AECOPD of 70%. A cross-sectional study showed prescribing rates of 92.9% in Russia, 81.1% in Spain, 80.6% Lithuania, and only 48.9% in Denmark.14 Since we detected pathogens in only a limited percentage of cultures, our local data suggest that the role of bacteria in AECOPD in primary care is limited. Evidence that antibiotics are not needed in mild exacerbations of COPD in primary care is helpful, not only to support physicians, but also to educate patients in their claim for antibiotics. A randomized double-blinded study in outpatients showed that antibiotics added to an oral course of corticosteroids did not accelerate recovery of exacerbations.15 In addition, a multicenter RCT addressing this question has recently started in Germany.16
In severe AECOPD, it is difficult to differentiate between a bacterial and nonbacterial cause of exacerbation. Sputum purulence is associated with bacterial cause of exacerbations but the prediction is far from perfect.17,18 Treating all AECOPD with antibiotics based on sputum purulence alone would result in over-treatment.19,20 Point-of-care diagnostics may be supportive in the decision not to prescribe antibiotics.17 C-reactive protein (CRP) and procalcitonin tests have been evaluated for this purpose, and both allow for strategies to successfully reduce treatment with antibiotics in AECOPD.21 CRP as point of care test is already feasible and in use by general practitioners in the Netherlands. The addition of CRP testing during AECOPD showed a strong reduction in antibiotic prescription in patients with AECOPD with purulent sputum, and antibiotic prescription rates were 26% lower in general practitioners using CRP tests.14 The guidelines of Norway and Denmark recommend the use of biomarkers for treatment with antibiotics of outpatients with AECOPD.20 Future studies may aim to compare the usefulness of procalcitonin to CRP to reduce antibiotic prescription in AECOPD in primary care.
Following the data analysis of this study, the Dutch guidelines were revised in 2015.22 The updated version states that severe AECOPD can be treated with oral corticosteroids and optimizing bronchodilator therapy. In patients with FEV1 >50%, there is no need for antibiotics, unless patients have signs of infection (temperature >38°C) or there is no response within 2–4 days of treatment. CRP point of care assessment can be used to support the decision not to prescribe antibiotics. If CRP is <20 mg/L, there is no indication for antibiotic treatment. If CRP is >20 mg/L, the decision to start antibiotics depends on the clinical state of the patient. If CRP is above 100 mg/L, start of antibiotics is indicated.14,17 In patients with FEV1 30%–50% and signs of infection, start of antibiotics is recommended independently of CRP determinations. In patients with FEV1 <30%, antibiotics are recommended with or without signs of infection. Amoxicillin or doxycycline for 7–10 days is recommended as first choice antibiotics.
The role of sputum diagnostics is often underexposed in guidelines on the treatment of AECOPD.
Sputum gram stains may provide useful information in the decision not to prescribe antibiotics. If there is no suggestion of a single microorganism, or abundance of potential pathogenic microorganisms in the stain, this was found to be 100% predictive of a nonbacterial cause of AECOPD in combination with a nonclinical decrease in lung function, and <2 exacerbations in the previous year.23
Next, local or regional susceptibility data of respiratory pathogens on a population level are important for empiric choice of antibiotic treatment. On an individual level, patients may benefit from targeted treatment based on sputum culture results in case of recurrent exacerbations due to resistance to antibiotics. Our data shows that resistance of H. influenzae to amoxicillin is abundant, but uncommon to doxycycline. In contrast, S. pneumoniae may be resistant to doxycycline, but resistance to amoxicillin is rare. Thus, in case of no improvement on treatment, a switch between these first choice antibiotics seems reasonable. In patients with severe AECOPD who are at immediate risk of being hospitalized, amoxicillin with clavulanic acid seems to be the best choice based on our susceptibility data.
Our study shows that the current situation of antibiotic prescription in repeated exacerbations is suboptimal. To reduce inappropriate use of antibiotics, we agree with the updated guidelines making the prescription of antibiotics less routine, and introducing a quest for point of care testing of a biomarker (CRP). We suggest that performing sputum diagnostics prior to antibiotic treatment in patients with early treatment failure or a repeated exacerbation will further rationalize antibiotic treatment (or abstinence thereof). Empiric antibiotic treatment based on local epidemiology could immediately be started if necessary and adapted based on culture results. Differences in epidemiology and antimicrobial treatment between countries should be further analyzed in order to understand the cause and implement good-practice. Cross-border collaboration, for example, between the Netherlands and Germany could help implementation of better care in COPD patients.
Acknowledgments
The authors would like to thank Heske Bathoorn from the University Medical Center Groningen and Matthijs Berends from Certe – Laboratory for Infectious Diseases, Groningen for their help with the data collection.
This work was supported by the Interreg IVa-funded project EurSafety Heath-net (III-1-02=73), part of a Dutch–German cross-border network supported by the European Commission, the German Federal States of Nordrhein-Westfalen and Niedersachsen, and the Dutch provinces of Overijssel, Gelderland, and Limburg.
Disclosures
TvdM is a member of the board of trustees of Certe – Laboratory for Infectious Diseases, Groningen during the conduct of the study. HAMK reports that his institution has received grants and consultancy fees from Novartis, Almirall, GlaxoSmithKline, Fluidda, AstraZeneca, and Boehringer Ingelheim outside the submitted work. The other authors report no conflicts of interest in this work.
References
OECD. Health at a glance: Europe 2012.Organisation for Economic Co-operation and Development. Paris, France: OECD publishing; 2012. | ||
Seemungal T, Harper-Owen R, Bhowmik A, et al. Respiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164(9):1618–1623. | ||
Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106(2):196–204. | ||
Daniels JM, Snijders D, de Graaff CS, Vlaspolder F, Jansen HM, Boersma WG. Antibiotics in addition to systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;181(2):150–157. | ||
Goossens H, Ferech M, Vander Stichele R, Elseviers M; ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579–587. | ||
Hicks LA, Chien YW, Taylor TH Jr, Haber M, Klugman KP; Active Bacterial Core Surveillance (ABCs) Team. Outpatient antibiotic prescribing and nonsusceptible Streptococcus pneumoniae in the United States, 1996–2003. Clin Infect Dis. 2011;53(7):631–639. | ||
Vollenweider DJ, Jarrett H, Steurer-Stey CA, Garcia-Aymerich J, Puhan MA. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;12:CD010257. | ||
Woodhead M, Blasi F, Ewig S, et al. Guidelines for the management of adult lower respiratory tract infections–full version. Clin Microbiol Infect. 2011;17(Suppl 6):E1–E59. | ||
Smeele IJM, Weel C van, Schayck CP van, et al. NHG-Standaard COPD (tweede herziening) [NHG-Standard COPD {second revision}]. Huisarts Wet. 2007; 50(8):362–379. Dutch. | ||
Hurst JR, Donaldson GC, Quint JK, Goldring JJ, Baghai-Ravary R, Wedzicha JA. Temporal clustering of exacerbations in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2009;179(5):369–374. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. | ||
Bathoorn E, Liesker JJ, Postma DS, et al. Change in inflammation in out-patient COPD patients from stable phase to a subsequent exacerbation. Int J Chron Obstruct Pulmon Dis. 2009;4:101–109. | ||
www.eucast.org. European Committee on Antimicrobial Susceptibility Testing; version 6.0 [valid from 2016 Jan 1, cited 2016 Jul 8]. Available from: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_6.0_Breakpoint_table.pdf. Accessed September 28, 2016. | ||
Llor C, Bjerrum L, Munck A, et al. Predictors for antibiotic prescribing in patients with exacerbations of COPD in general practice. Ther Adv Respir Dis. 2013;7(3):131–137. | ||
Sachs AP, Koeter GH, Groenier KH, van der Waaij D, Schiphuis J, Meyboom-de Jong B. Changes in symptoms, peak expiratory flow, and sputum flora during treatment with antibiotics of exacerbations in patients with chronic obstructive pulmonary disease in general practice. Thorax. 1995;50(7):758–763. | ||
Rohde GG, Koch A, Welte T; ABACOPD study group. Randomized double blind placebo-controlled study to demonstrate that antibiotics are not needed in moderate acute exacerbations of COPD–the ABACOPD study. BMC Pulm Med. 2015;15:5. | ||
Miravitlles M, Moragas A, Hernandez S, Bayona C, Llor C. Is it possible to identify exacerbations of mild to moderate COPD that do not require antibiotic treatment? Chest. 2013;144(5):1571–1577. | ||
Soler N, Torres A. Significance of sputum purulence to guide antibiotic therapy in exacerbations of COPD. Eur Respir J. 2013;41(1):248–249. | ||
Brusse-Keizer MG, Grotenhuis AJ, Kerstjens HA, et al. Relation of sputum colour to bacterial load in acute exacerbations of COPD. Respir Med. 2009;103(4):601–606. | ||
Laue J, Reierth E, Melbye H. When should acute exacerbations of COPD be treated with systemic corticosteroids and antibiotics in primary care: A systematic review of current COPD guidelines. NPJ Prim Care Respir Med. 2015;25:15002. | ||
Brightling CE. Biomarkers that predict and guide therapy for exacerbations of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10(Suppl):S214–S219. | ||
Snoeck-Stroband JB, Schermer TRJ, Van Schayck CP, et al. NHG-Standaard COPD (tweede herziening) [NHG-Standard COPD {second revision}]. Huisarts Wet. 2015;58(4):198–211. Dutch. | ||
van der Valk P, Monninkhof E, van der Palen J, Zielhuis G, van Herwaarden C, Hendrix R. Clinical predictors of bacterial involvement in exacerbations of chronic obstructive pulmonary disease. Clin Infect Dis. 2004;39(7):980–986. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.