Back to Journals » Infection and Drug Resistance » Volume 12
Rational use of antibiotics in an intensive care unit: a retrospective study of the impact on clinical outcomes and mortality rate
Authors Ali M, Naureen H , Tariq MH , Farrukh MJ , Usman A , Khattak S, Ahsan H
Received 17 September 2018
Accepted for publication 16 January 2019
Published 26 February 2019 Volume 2019:12 Pages 493—499
DOI https://doi.org/10.2147/IDR.S187836
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Joachim Wink
Muhammad Ali,1 Humaira Naureen,1 Muhammad Haseeb Tariq,2,3 Muhammad Junaid Farrukh,4,5 Abubakar Usman,3 Shahana Khattak,1 Hina Ahsan1
1Faculty of Pharmaceutical Sciences, Riphah International University, Islamabad, Pakistan; 2Pharmaceutical Evaluation and Registration Division, Drug Regulatory Authority of Pakistan, Islamabad, Pakistan; 3Department of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia; 4Department of Clinical Pharmacy, Faculty of Pharmaceutical Sciences, UCSI University, Kuala Lumpur, Malaysia; 5Department of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Background: Intensive care units (ICUs) are specialized units where patients with critical conditions are admitted for getting specialized and individualized medical treatment. High mortality rates have been observed in ICUs, but the exact reason and factors affecting the mortality rates have not yet been studied in the local population in Pakistan.
Aim: This study was aimed to determine rational use of antibiotic therapy in ICU patients and its impact on clinical outcomes and mortality rate.
Methods: This was a retrospective, longitudinal (cohort) study including 100 patients in the ICU of the largest tertiary care hospital of the capital city of Pakistan.
Results: It was observed that empiric antibiotic therapy was initiated in 68% of patients, while culture sensitivity test was conducted for only 19% of patients. Thirty-percent of patients developed nosocomial infections and empiric antibiotic therapy was not initiated for those patients (P<0.05). Irrational antibiotic prescribing was observed in 86% of patients, and among them, 96.5% mortality was observed (P<0.05). The overall mortality rate was 83%; even higher mortality rates were observed in patients on a ventilator, patients with serious drug–drug interactions, and patients prescribed with irrational antibiotics or nephrotoxic drugs. Adverse clinical outcomes leading to death were observed to be significantly associated (P<0.05) with irrational antibiotic prescribing, nonadjustment of doses of nephrotoxic drugs, use of steroids, and major drug–drug interactions.
Conclusion: It was concluded that empiric antibiotic therapy is beneficial in patients and leads to a reduction in the mortality rate. Factors including irrational antibiotic selection, prescribing contraindicated drug combinations, and use of nephrotoxic drugs were associated with high mortality rate and poor clinical outcomes.
Keywords: clinical outcomes, mortality rate, intensive care unit, rational use of antibiotics, nosocomial infections, medication review
Introduction
Intensive care units (ICUs), also known as intensive therapy units or critical care units, are special hospital wards that provide treatment and monitoring for critically ill patients. Since patients with critical infectious diseases are also managed in ICUs, they can become a major source of spreading infectious organisms which may lead to nosocomial infections. Such nosocomial infections are associated with increased morbidity, mortality, and health care costs.1 Nosocomial infections are a serious patient safety concern in modern health care system, since it is the fifth leading cause of death among hospitalized patients. ICU patients are five to ten times more likely to acquire nosocomial infections than those in general ward.2 Nosocomial infections occur worldwide and affect both developing and developed countries.3
Empiric antibiotic administration is required in majority of ICU patients, but extensive use of both broad- and narrow-spectrum antibiotics may lead to development of resistant strains of bacteria and other pathogens.4 The extensive and irrational use of antibiotics has also been reported to increase the risk of toxicity and drug interactions.5
This study was aimed to determine the rational use of antibiotic therapy in ICU patients, its impact on clinical outcomes, and mortality rate. The study was also focused to identify factors affecting mortality rate in ICU patients undergoing antibiotic therapy.
Patients and methods
Ethical approval
Ethical approval was taken from the Ethics Review Board of Pakistan Institute of Medical Sciences, Hospital. Since this was a retrospective study in which all patients were either discharged after recovery or died during treatment, taking individual patient consent was not possible. Therefore, the Ethics Review Board waived the requirement of patient consent form. Patient data confidentiality and its compliance with the Declaration of Helsinki were ensured by the Ethics Review Board.
Study settings and design
This was a retrospective longitudinal (cohort) study including patients admitted in either medical or surgical ICU of the largest tertiary care hospital of the capital city of Pakistan.
Study sample
The study sample included all patients fulfilling the inclusion criteria and who were admitted and subsequently discharged/died between September 2016 and April 2017 in the ICU of the largest tertiary care hospital of capital of Pakistan. Patients aged 2–60 years with <30 days of ICU stay were included in the study, since the accurate renal function cannot be determined using Cockroft–Gault (equation) method for patients <2 and >60 years of age.
Clinical evaluation
Daily clinical evaluation was performed for each patient using standard methods and approved guidelines. The difference in values of all studied variables was determined before and after the start of any therapy. The clinical outcomes were determined on the last day in terms of “discharge” or “death” after treatment. Renal function was determined using Cockroft–Gault equation,6 and the need for dose adjustment and required dose after adjustment was determined using guidelines from the Physician Desk Reference,7 British National Formulary,8 and Renal Pharmacotherapy.9 The adverse events for every administered drug were enlisted from clinical drug literatures approved by the US Food and Drug Administration, the Medicine and Healthcare Products Regulatory Agency, UK and the European Medicine Agency. Drug–drug interactions were determined by Stockley’s drug interaction.10 The control of infection was determined using reduction in white blood cell (WBC) count and fever, and the appropriateness of the antibiotic therapy was determined using the results of culture sensitivity test (CST) and the American Society of Infectious Diseases (IDSA) guidelines.
Study tool (evidence-based clinical checklist)
An evidence-based clinical checklist was adapted from an already developed clinical checklist.11 The variables included in the checklist were also compared with previous reported studies and discussed among a focus group of clinical researchers and practitioners. The finally developed checklist was also subjected to content validity through a pilot study on 20 patients and to focus group discussion to identify any missed variable or clinical scenario. After validation, the final version of the checklist was used during the study.
Statistical analysis
All the data collected through clinical checklist were transcribed on a spreadsheet in SPSS after carefully defining all the variables under study. The analysis was performed in two steps including a descriptive analysis in which patient clinical situation and various variables were studied for their respective frequencies, percentages, and measure of central tendencies. Later, in the second step, inferential statistics was employed to determine the associations among patient- and therapy-related variables, clinical outcomes, and mortality rate using Pearson’s chi-squared test, and P-value <0.05 was considered statistically significant.
Results
This study involved 100 patients which fulfilled the inclusion criteria and were discharged from the ICU between September 2016 and April 2017, including both males (43%) and females (57%). Twenty patients were between 2 and 20 years age, while 44 patients were between 21 and 40 years old and 36 patients were in the age group of 41–60 years. The length of the ICU stay for all the patients under investigation was from 2 to 30 days.
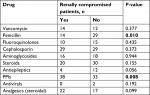
In our study, 68% patients were being administered empiric therapy with broad-spectrum antibiotics; among them, samples for CST were drawn in only 7% of the patients (P=0.001). Antibiotic therapy was changed in 13% patients (P=0.000) after the CST reports were received. The concept of de-escalation therapy12 was not followed in this hospital, and none of the initiated antibiotics were de-escalated or stopped; instead, new antibiotics were added after the CST results. The results are presented in Table 1 and Figure 1.
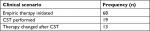  | Table 1 Frequency of various scenarios while prescribing empiric antibiotics Abbreviation: CST, culture sensitivity test. |
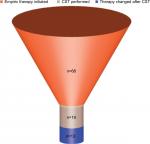  | Figure 1 Funnel graph showing the frequency (n) of changes in antibiotic therapy after initiation of empiric therapy. Abbreviation: CST, culture sensitivity test. |
During our investigation period, 30% of the patients developed infections 3 days after their admission in hospital ICU, and therefore, it was declared that they had nosocomial infection.13 The pattern of nosocomial infection was statistically insignificant among the gender and age groups. It was observed that nosocomial infection developed in every patient who was not administered empiric antibiotic therapy (P=0.0002), as shown in Table 2. In our study, 29 patients were on ventilator, and among them, 10 (34.5%) patients developed nosocomial infections with very high mortality rate (89.7%). Other than the common broad-spectrum antibiotics, some narrow-spectrum antibiotics were also prescribed (Table 3).
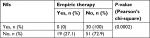  | Table 2 Cross-tabulation of development of NIs against initiation of empiric antibiotic therapy Abbreviation: NI, nosocomial infection. |
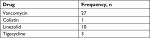  | Table 3 Frequency of prescription of narrow-spectrum antibiotics |
Since the study was carried out in ICU where patients are brought due to multiple reasons, one of the important factors while selecting a drug therapy to be prescribed is the route of metabolism and excretion of the drug and the renal/hepatic profile of the patients.14 Since a majority of the drugs are excreted through kidneys, assessing the kidney function is a key factor in ensuring administration of safe and effective therapy.15
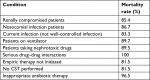
In our study, it was determined that 41% of the patients were renally compromised, and they needed careful administration of renally excreted drugs.16 The use of nonsteroidal anti-inflammatory drugs was not seen in any of the patient, and instead, steroidal analgesics were used. Use of vancomycin, aminoglycoside, steroids, and proton pump inhibitors (PPIs) was observed, which need to be avoided or administered carefully among renally compromised patients. The use of PPI was high (P=0.008) in renally compromised patients as compared to those with normal renal function. The results of the frequency of nephrotoxic drugs prescribed are provided in Table 4.
  | Table 4 Frequency of prescribing potentially nephrotoxic drugs among renally compromised patients Note: Bold P-values are statistically significant: P<0.05. Abbreviation: PPI, proton pump inhibitor. |
Out of 41 renally compromised patients, 38 were being prescribed with nephrotoxic drugs for which dose adjustments were required. No renal dose adjustments were made in any of the patients and among the 41 renally compromised patients, 85.4% died at the end of the study.
In our study, only 14% patients were prescribed antibiotics as per the recommendations of IDSA and all these patients were discharged after recovery. Also, among the 86% patients in whom IDSA recommendations were not followed, statistically significant (P=0.000) mortality rate (96.5%) was observed. The results are presented in Table 5.
  | Table 5 Association of various clinical variables with appropriateness of antibiotic therapy Note: Bold P-values are statistically significant: P<0.05. |
Among patients having recurrent infection even after antibiotic administration, 85% of them were initially prescribed with in appropriate antibiotics. Appropriate antibiotic therapy was not administered in majority (26 [89.7%]) of the ventilator patients. One hundred percent mortality rate was observed among all such patients on ventilator for whom appropriate antibiotic therapy had not been administered.
The signs of infection including raised WBC count and/or fever17 were observed in 60% of patients already on antibiotic therapy, with a mean WBC count of 41.6 in the infected patient group. The fever was well controlled in most of the patients, with only 15 patients having a temperature >100°F and only 2 patients having above 102°F, with a mean value of 98.54°F.
The associations of various factors affecting the end outcome in ICU patients were determined using chi-squared test. These associations are provided in Table 6.
It was found that patients treated with appropriate antibiotics were discharged from the hospital. CST was performed in 19 patients; but due to various other factors including renally compromised state of the patients, 17 (89.5%) died at the end of treatment. Renal dose adjustment is necessary in renally compromised patients, but it was not performed in 77 (89.5%) patients and all of them died at the end. Steroids should be used with caution in renally compromised patients,18 and in our study, 52 (91.2%) patients who were on steroid therapy died.
It was observed that major drug–drug interactions including fatal particulate precipitation occurred in the lungs due to co-administration of ceftriaxone along with calcium-containing intravenous solutions.19 Since drug therapy was not reviewed by any specialized clinical pharmacist, drug–drug interactions could not be reported, thus leading to high mortality rate.
An overall 83% mortality rate was observed in this study, while the mortality rate among various specified clinical conditions is provided in Table 7 and Figure 2.
  | Table 7 Mortality rate in various clinical scenarios Abbreviation: CST, culture sensitivity test. |
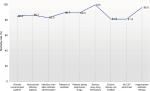  | Figure 2 Mortality rate (%) in various clinical scenarios. Abbreviation: CST, culture sensitivity test. |
It was observed that the mortality rate was affected by inappropriate use of antibiotics, failure to perform renal dose adjustments, presence of major drug–drug interactions, and use of nephrotoxic drugs without any control or dose adjustments.
Discussion
In the current study, empiric therapy with broad-spectrum antibiotics was administered in 68% of the patients. Since all ICU patients are at high risk for developing infections due to intense pathological/surgical conditions, all measures are usually taken to prevent the spread of infection.20 The hospital under study caters for the medical needs of ~6–7.5 million population,21 and due to high patient influx, the hygienic conditions were poor and proper sterilization and disinfection could not be attained at all levels.22,23 Certain previous studies have also reported the use of empiric antibiotic therapy in the ICU when the hygienic conditions are poor.24–26 Before initiation of empiric antibiotic therapy, samples for CST were drawn in very few, that is, only 7%, patients. CST samples can give false results if empiric antibiotic therapy has been initiated. After the results of CST were obtained, antibiotic therapy was modified in only 13% of patients, that too, without following the principles of de-escalation, which are very important to consider while treating patients with acute infections.12 The frequency of nosocomial infections in our study was found to be 30%, with the highest number of infections (ie, 34.5%) associated with ventilator since they are most difficult to manage.27,28 The frequency of ventilator-acquired nosocomial infection in our study was quite similar with previously reported data in Pakistan.29 The practice of initiating empiric antimicrobial therapy among ICU patients was found to be associated with reduction in incidence of nosocomial infections, since none of the patients undergoing empiric therapy developed nosocomial infection. This practice was in accordance with previously reported benefits from initiation of empiric therapy in reducing nosocomial infection.24 Since there was no antibiotic control or stewardship program in this hospital and none of the prescribed therapy was reviewed by infectious disease specialist or clinical pharmacist specialized in infectious diseases, appropriate therapy was prescribed in only 14% of patients, which is very low as compared to already reported data,30 while the drug therapy in the remaining 86% of patients had errors such as inappropriate drug or dose selection, serious interactions, and unwanted adverse reactions.
In this study, overall, 83% mortality rate was observed, which is very high as compared to previously reported literature.31 Mortality rate among patients with nosocomial infection was found to be 89.7%, which is quite high as compared to previous literature data.32,33 Very high mortality rate (85.4%) was observed in renally compromised patients prescribed with potentially nephrotoxic drugs as compared to previously reported studies.34,35 Among patients for whom appropriate antibiotics were not prescribed in adequate doses, a mortality rate of 96.5% was observed, which is very high as compared to previous study reports.36 This high mortality rate, especially with inappropriate use of antibiotics, is a point of concern and should be addressed with appropriate measures by the concerned authorities.
High mortality rates, poor clinical outcomes, and poor hygienic conditions were observed among ICU patients of the largest tertiary care hospital of the capital city of Pakistan, which indicates lack of interest and commitment of higher officials and policymakers. Regardless of such high mortality rates, no measures for infection control have been taken and no protocols for antibiotic prescribing have been developed. The spread of infections and resistant strains is also putting health care providers at risk.
Conclusion
Empiric antibiotic therapy is beneficial in patients and leads to reduction in mortality rate. Irrational antibiotic prescribing along with co-administration of contraindicated drugs and use of nephrotoxic drugs without dose adjustments were found to be associated with high mortality rate and poor clinical outcomes. Medication review under the supervision of clinical pharmacist specialized in intensive care can help reduce various factors affecting mortality rate. Antibiotic control programs including stewardship and prescribing under the supervision of infectious disease specialist can further help to improve clinical outcomes and reduce mortality. It is time that health authorities of the capital of Pakistan take serious measures to control the mortality rate by implementing stewardship program, hiring competent infectious disease specialist and clinical pharmacists specialized in infectious disease, and training the medical staff regarding use and de-escalation of antibiotic therapy.
Disclosure
The authors report no conflicts of interest in this work.
References
Jarvis WR. Selected aspects of the socioeconomic impact of nosocomial infections: morbidity, mortality, cost, and prevention. Infect Control Hosp Epidemiol. 1996;17(8):552–557. | ||
Mauldin PD, Salgado CD, Hansen IS, Durup DT, Bosso JA. Attributable hospital cost and length of stay associated with health care-associated infections caused by antibiotic-resistant gram-negative bacteria. Antimicrob Agents Chemother. 2010;54(1):109–115. | ||
Ducel G, Fabry J, Nicolle L. Prevention of Hospital-Acquired Infections: A Practical Guide. 2nd ed. Geneva: World Health Organization; 2002. | ||
Sarraf D, Phunyalb M, Mandals M, Rauniar G. Utilization pattern of antimicrobial agents and its culture sensitivity pattern in intensive care units in a tertiary care center in eastern Nepal. Nepal Med Coll J. 2015;17(3–4):107–112. | ||
Emmerson M. Antibiotic usage and prescribing policies in the intensive care unit. Intensive Care Med. 2000;26(1):S026–S030. | ||
Cockcroft DW, Gault H. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. | ||
Staff PDR. Physicians’ Desk Reference. 66th ed. New York: Thomson Healthcare; 2011. | ||
Royal Pharmaceutical Society. MedicinesComplete [homepage]. Available from: https://about.medicinescomplete.com/. Accessed June 7, 2016. | ||
Golightly LK. Renal pharmacotherapy. In: Dosage Adjustment of Medications Eliminated by the Kidneys. New York: Springers; 2003. | ||
Preston CL. Stockley’s drug interaction. In: Royal Pharmaceutical Society. London: Pharmapress; 2015. | ||
Farrukh MJ, Hisham SA, Bin Zainal ZA. Pharmaceutical care issues in patients with atrial fibrillation receiving thromboprophylaxis. Am J Pharmacol Sci. 2014;5B:12–16. | ||
Masterton RG. Antibiotic de-escalation. Crit Care Clin. 2011;27(1):149–162. | ||
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16(3):128–140. | ||
Udy AA, Roberts JA, Lipman J. Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med. 2013;39(12):2070–2082. | ||
Roberts JA, Lipman J. Antibacterial dosing in intensive care. Clin Pharmacokinet. 2006;45(8):755–773. | ||
Mahmood I. Interspecies scaling of renally secreted drugs. Life Sci. 1998;63(26):2365–2371. | ||
High KP, Bradley SF, Gravenstein S, et al. Clinical practice guideline for the evaluation of fever and infection in older adult residents of long-term care facilities: 2008 update by the infectious diseases Society of America. Clin Infect Dis. 2009;48(2):149–171. | ||
Pazhayattil GS, Shirali AC. Drug-induced impairment of renal function. Int J Nephrol Renovasc Dis. 2014;7:457. | ||
Murney P. To mix or not to mix – compatibilities of parenteral drug solutions. Aust Prescr. 2008;31(4):98–101. | ||
Eroglu A. Factors impacting the likelihood of death in patients in intensive care unit. Int J Anesthesiol Res. 2016;4(4):225–228. | ||
6th Population & Housing Census 2017, Bureau of Statistics Pakistan. Available from: http://www.pbscensus.gov.pk/. Accessed March 15, 2018. | ||
Ikram A, Hussain Shah SI, Naseem S, et al. Status of hospital infection control measures at seven major tertiary care hospitals of northern Punjab. J Coll Physicians Surg Pak. 2010;20(4):266–270. | ||
Akhtar N. Hospital acquired infections in a medical intensive care unit. J Coll Physicians Surg Pak. 2010;20(6):386–390. | ||
Kollef M. Appropriate empirical antibacterial therapy for nosocomial infections: getting it right the first time. Drugs. 2003;63(20):2157–2168. | ||
Bor C, Demirag K, Okcu O, Cankayali I, Uyar M. Ventilator-associated pneumonia in critically ill patients with intensive antibiotic usage. Pak J Med Sci. 2015;31(6):1441. | ||
Malik MI. Antimicrobial susceptibility pattern of bacteria isolated from tracheal secretions in intensive care units admitted patients of Lahore General Hospital. Pak J Chest Med. 2018;24(2):72–77. | ||
Kalanuria AA, Ziai W, Zai W, Mirski M. Ventilator-associated pneumonia in the ICU. Crit Care. 2014;18(2):208. | ||
Maqbool M, Shabir A, Naqash H, Amin A, Koul RK, Shah P. Ventilator associated pneumonia – incidence and outcome in adults in medical intensive care unit of a tertiary care hospital of North India. Int J Sci Study. 2017;4(10):73–76. | ||
Shaikh JM, Devrajani BR, Shah SZ, Akhund T, Bibi I. Frequency, pattern and etiology of nosocomial infection in intensive care unit: an experience at a tertiary care hospital. J Ayub Med Coll Abbottabad. 2008;20(4):37–40. | ||
Baqi S, Damani NN, Shah SA, Khanani R. Infection control at a government hospital in Pakistan. Int J Infect Control. 2009;5(1):1–7. | ||
Rosenthal VD, Guzman S, Orellano PW. Nosocomial infections in medical–surgical intensive care units in Argentina: attributable mortality and length of stay. Am J Infect Control. 2003;31(5):291–295. | ||
Pittet D, Tarara D, Wenzel RP. Nosocomial bloodstream infection in critically ill patients, excess length of stay, extra costs, and attributable mortality. J Am Med Assoc. 1994;271(20):1598–1601. | ||
Bueno-Cavanillas A, Delgado-Rodríguez M, López-Luque A, Schaffino-Cano S, Gálvez-Vargas R. Influence of nosocomial infection on mortality rate in an intensive care unit. Crit Care Med. 1994;22(1):55–60. | ||
Mandelbaum T, Scott DJ, Lee J, et al. Outcome of critically ill patients with acute kidney injury using the acute kidney injury network criteria. Crit Care Med. 2011;39(12):2659–2664. | ||
Ostermann M, Chang R; Riyadh ICU Program Users Group. Renal failure in the intensive care unit: acute kidney injury compared to end-stage renal failure. Crit Care. 2008;12(5):432. | ||
Pradhan NP, Bhat SM, Ghadage DP. Nosocomial infections in the medical ICU: a retrospective study highlighting their prevalence, microbiological profile and impact on ICU stay and mortality. J Assoc Physicians India. 2014;62(10):18–21. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

