Back to Journals » Orthopedic Research and Reviews » Volume 14
Radiological Outcomes of Reduction Surgery for Degenerative Lumbar Spondylolisthesis Using Long Arm Pedicle Screws
Authors Saleh I, Librianto D , Dilogo IH , Supriadi S, Indriatmi W, Octaviana F, Prasetyo M, Noor Z
Received 18 July 2022
Accepted for publication 18 October 2022
Published 28 October 2022 Volume 2022:14 Pages 365—372
DOI https://doi.org/10.2147/ORR.S382232
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Clark Hung
Ifran Saleh,1 Didik Librianto,2 Ismail Hadisoebroto Dilogo,3 Sugeng Supriadi,4 Wresti Indriatmi,5 Fitri Octaviana,6 Marcel Prasetyo,7 Zairin Noor8
1Orthopaedic Spine Surgeon, Department of Orthopaedic and Traumatology, Faculty of Medicine Universitas Indonesia – Cipto Mangunkusumo Hospital, Jakarta Pusat, Indonesia; 2Orthopaedic Spine Surgeon, Department of Orthopaedic and Traumatology, Faculty of Medicine Universitas Indonesia – Fatmawati Hospital, Jakarta Pusat, Indonesia; 3Orthopaedic Surgeon, Consultant of Hip and Knee, Department of Orthopaedic and Traumatology, Faculty of Medicine Universitas Indonesia – Cipto Mangunkusumo Hospital, Jakarta Pusat, Indonesia; 4Department of Mechanical Engineering, Faculty of Engineering, Universitas Indonesia, Depok City, Indonesia; 5Consultant Dermatologist, Department of Dermatology and Venerology, Faculty of Medicine Universitas Indonesia – Cipto Mangunkusumo Hospital, Jakarta Pusat, Indonesia; 6Consultant Neurologist, Department of Neurology, Faculty of Medicine Universitas Indonesia – Cipto Mangunkusumo Hospital, Jakarta Pusat, Indonesia; 7Consultant Radiologist, Department of Radiology, Faculty of Medicine Universitas Indonesia – Cipto Mangunkusumo Hospital, Jakarta Pusat, Indonesia; 8Orthopaedic Spine Surgeon, Department of Orthopaedic and Traumatology, Faculty of Medicine Universitas Lambung Mangkurat, Jakarta Pusat, Indonesia
Correspondence: Ifran Saleh, Department of Orthopaedic & Traumatology, Faculty of Medicine Universitas Indonesia, Cipto Mangunkusumo Hospital, Jakarta Pusat, Indonesia, Tel +62 811111221, Email [email protected]
Objective: Until now, the spondylolisthesis reduction technique has relied on posterior instrumentation using long arm pedicle screws. In this way, the segments will be brought into alignment with the other vertebrae with the pedicle mats being tightened. The aim of this study is to acknowledge whether reduction surgery for degenerative lumbar spondylolisthesis (DLS) using long arm pedicle screws is able to correct the listhesis and spinopelvic parameters.
Methods: We carried out a retrospective study of patients with degenerative lumbar spondylolisthesis who went through reduction surgery using long arm pedicle screws in our institutions from January 2019 to March 2022. Preoperative and postoperative radiological outcomes consisting of listhesis and spinopelvic parameters were assessed.
Results: We found a statistical difference between the magnitude of listhesis immediately after surgery and preoperatively (p< 0.001), with a successful correction of 85.85%. There was significant decrease in the value of pelvic tilt (p=0.044) and increase in the value of sacral slope (p=0.008) after surgery.
Conclusion: Reduction surgery using long arm pedicle screws for DLS was able to reduce the listhesis effectively up to 85.5%, and also to restore the parts of spinopelvic parameters, the pelvic tilt and sacral slope, approaching normal values.
Keywords: degenerative lumbar spondylolisthesis, long arm pedicle screws, listhesis, spinopelvic parameters, radiological outcomes
Introduction
Spondylolisthesis is forward slippage of one vertebrae against the vertebra below it, which is associated with degenerative changes without vertebral ring defects or disorders.1,2 Degenerative lumbar spondylolisthesis (DLS) occurs in the elderly group. This disease is more common in women because of ligament flexibility and hormonal effects: the ratio of women to men is 2–3:1.2. The global prevalence of DLS is 24.8%: prevalence in segments L3-4 is 4.5%, segment L4-5 is 12%, and L5-S1 is 8.3%.3 Risk factors in the form of anatomical conditions also determine the progression of this disease, including pelvic anatomy, inclination of the fourth lumbar vertebra, vertebral size, and facet orientation in the sagittal section, which results in facet joint degeneration. The vertebrae that are susceptible to spondylolisthesis are the fourth and fifth lumbar, with vertebral translation most often at >30%.
Even if the displacement is small, if it is accompanied by ligamentous flavum hypertrophy or intervertebral disc protrusion, narrowing of the spinal canal is likely to occur easily. The narrowing causes neurological symptoms in the form of neurogenic claudication or sensory and motor disturbances. The spinal canal then narrows again with posterior joint subluxation exacerbated by osteophyte growth. In addition, the exiting L5 nerve can also experience the “guillotine effect”, ie compression by the pedicle and corporotransverse ligament from above.4–6
Spondylolisthesis management can be non-operative and operative. The main goals of therapy are to relieve pain, restore function, restore flexibility of nervous tissue, and strengthen the spine. Surgery is performed to partially remove the bone pressing on the nerves, followed by fusion of the vertebral bodies to repair.2 These procedures are performed simultaneously by reducing the displaced bone. Several researchers have tried various tools to facilitate reduction. Examples of these techniques are skeletal traction in the hip flexion position, distraction using halo-femoral traction, distraction using a Harrington rod, and placing a cast. The results of therapy vary widely, some being very good and others unsatisfactory. In addition, there is a high risk of neurologic injury.7,8
Until now, the spondylolisthesis reduction technique has relied on posterior instrumentation, namely, bolts of the vertebral segment that has undergone listhesis and then in the final stage using a special reduction, called long arm pedicle screws.9 Long-arm pedicle screw is a multi-axial pedicle screw with a long U-shaped screw head. In this way, the spondylolisthesis segment will be brought into alignment with the other vertebrae when the pedicle nuts and rods are being tightened.7,8 The use of this long arm pedicle screw had been described in the literature; however, its use in our country is still limited, owing to its more expensive cost compared to ordinary pedicle screws. In our country, we had limited budget due to the National Insurance. For the above reason, we were not much using this long arm pedicle screw. Measurement of the degree of correction required is based on the measurement of radiological parameters. For the case of degenerative spondylolisthesis, there are various parameters used, ranging from the degree of displacement of the two vertebrae involved, to the spinopelvic and sagittal balance parameters, all of which can be obtained from the lumbosacral lateral projection radiograph. This study was then performed to evaluate whether reduction using long arm pedicle screws is able to correct the listhesis.
Method
We carried out a retrospective study of patients with degenerative lumbar spondylolisthesis (DLS) who carried out reduction surgery using long arm pedicle screws in our academic Fatmawati Hospitals from January 2019 to March 2022. Reduction surgery using these long arm pedicle screws was the standard method of surgery in these institutional hospitals. Ethics approval was attained from institutional review board of local faculty and the engaging hospitals. The institutional hospitals where the study was held were Cipto Mangunkusomo and Fatmawati Hospitals. The eligibility criteria for this study were diagnosis of DLS with persistent symptoms after 6 weeks of non-operative measures. Patients with another spinal surgery or loss to follow-up were excluded. All patients were assessed for preoperative and postoperative radiological outcomes consistent with listhesis and spinopelvic parameters. Figure 1 presents the glow chart of this study. Postoperatively, patients were allowed to return to previous sport or activity after 3 months.
 |
Figure 1 Flowchart of Eligibility Criteria. |
Research data was analyzed using IBM SPSS version 22 statistical software. For comparing study groups for mean equality of preoperative and postoperative outcomes, independent T or Mann–Whitney tests were used. P-value of <0.05 was considered to be statistically significant.
Intervention
Surgical Technique
The surgeries were held at two academic hospitals, performed by either one of two senior spine orthopaedic surgeons using long arm pedicle screws. The steps of surgery were as follows: midline incision until exposure of the listhesis levels, bilateral facetectomies, instrumentation of vertebrae using pedicle screws (the listhetic vertebrae were instrumented using long arm pedicle screws). Fusion using transforaminal of posterior lumbar interbody fusions was then followed, as shown in Figure 2. Thereafter, the vertebral segments will be brought into alignment with the other vertebrae with the pedicle mats being tightened. The final construct of the instrumentation was confirmed using intraoperative image intensifier. All surgeries were monitored by intraoperative neuro monitoring (IONM) by neurologists.
Non-sutured surgical drain was left in place until two to three days postoperatively. Patients then were encouraged to ambulate progressively as tolerated, without external support. Daily activities were gradually increased. Return to sports was restricted for at least 6 months after surgery.
Radiological Outcomes
The radiological outcomes were assessed preoperatively and immediately postoperatively using HOROS® application by the DICOM images (Figure 3). The radiological outcomes measured include listhesis and spinopelvic parameters. The spinopelvic parameters measured were pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), and lumbar lordosis (LL). The listhesis was measured as millimeters (mm) of the forward slippage of the vertebrae. PI is the angle formed by a line drawn from the center of the femoral heads to center of the sacral endplate. PT is the angle between the line from the sacral endplate to the center of the femoral heads and a vertical line, while SS is defined as the angle between the sacral endplate and a horizontal line. Lumbar lordosis is the angle between the sacral endplate and upper end of the first lumbar vertebrae.10
 |
Figure 3 Figure Describing the Difference between Preoperative and Postoperative Radiologic Measurements. |
Results
A total of 17 patients had reduction surgery for DLS in our study. The follow-up was immediate postoperative. The results were compared to preoperative values. Figure 3 shows the result sof radiologic measurements.
Mean age of the patients was 57.82 ± 7.77 years. Only one patient was a male, 16 were female. Most of the patients were suffering from listhesis at the L4-L5 vertebrae, followed by L3-4 and L4-5 equally. Most patients were in Meyerding grade I of the listhesis. Baseline characteristics of the patients are depicted in Table 1.
 |
Table 1 Subject Characteristics |
Summary of radiological outcome is depicted in Table 2. As seen, there was a significant difference between the magnitude of listhesis immediately after surgery and preoperatively (p<0.001), with a successful correction of 85.85%. Based on the measurements, there was no significant difference between after surgery and before surgery in the measurement of pelvic incidence (p=0.550) and lumbar lordosis (p=0.089). However, there was a significant difference in decreasing the value of pelvic tilt (p=0.044) and increasing the value of sacral slope (p=0.008) after surgery.
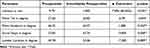 |
Table 2 Differences in Preoperative and Postoperative Radiological Values |
Discussion
The average age of occurrence of lumbar degenerative spondylolisthesis was 57.15, with an age range of 45.00–68.00 years. This finding is in line with the epidemiological research conducted by Deng et al,11 which found that the prevalence of degenerative lumbar spondylolisthesis was strongly influenced by age: prevalence was highest above 50 years of age and only a small number of cases occurred before the age of 50. Most of the subjects in this study were female, with a male to female ratio of 3:35. This finding is in line with the epidemiological findings of Yi Xiang et al,11 who found that the prevalence of degenerative lumbar spondylolisthesis was strongly influenced by gender. This study and other studies also stated that the percentage of women who experienced complaints of spondylolisthesis and underwent surgery for its treatment was higher than that of men due to the fact that women had lower pain thresholds than men, and that women had a higher tendency to experience pain.12,13 Physiologically, a greater proportion of women than men experience spondylolisthesis as a result of the greater laxity of their ligaments and the hormonal effects on women.2
The most frequent location for listhesis in this study was the L4-L5 segment. Lumbar degenerative spondylolisthesis can occur in any lumbar segment, but is most common in the L4-5 segment. The L5-S1 segment may also have listhesis, but with a small presentation.2 This finding was reflected in this study, where most of the listhesis occurred in the L4-5 segment, followed by the L3-4 and L5-S1 segments. As previously described, spondylolisthesis is defined as forward slippage of the vertebral bodies with respect to the vertebral bodies below at least 5% (3 mm) of the body length.11
The standard of surgery for spondylolisthesis is posterior stabilization using reduction screws. If the spondylolisthesis segment can be fully mobilized after adequate discectomy and annulus removal, the correction of the sagittal alignment depends only on the screw which will reduce the listhesis segment.14 This study, using long arm pedicle screws, successfully showed that the use of long arm pedicle screws was able to significantly reduce the spondylolisthesis, as high as 85.5%. A long arm pedicle screw consists of a long U-shaped screw head. The thread in the long arm screw makes the reduction of spondylolisthesis possible when the pedicle along with its rod are tightened. Long arm pedicle screw promotes more controlled and gradual anatomical reduction.
Our study showed that, postoperatively, there was reduction of PT value and increase of SS value. There was no alteration in other spinopelvic parameters, which may be due to the fact that the correction of spinopelvic parameters depends not only on the reduction of listhesis; factors other than vertebral displacement contribute to the resulting spinopelvic parameters. Yamaguchi et al15 found that there was an increase in lumbar lordosis after vertebral fusion. They revealed that the improvement in one of the spinopelvic parameters was not only caused by changes in postoperative anatomy, but rather the return of spinopelvic parameters to normal values due to complaints of back and leg pain having improved postoperatively. Another study, by Chumnanvej et al,16 assessed spinopelvic parameters in post-fusion spondylolisthesis patients and found that, postoperatively, only the lumbar lordosis parameters improved.
As previously noted, the basic deformities in spondylolisthesis are listhesis or slippage of the vertebral bodies, loss of disc height, and segmental kyphosis. With forward slippage, the center of gravity shifts to the anterior, the pelvis tilts backward, the upper vertebral segments hyperextend to balance the shift, and the lumbar lordosis is reduced because the disc also degenerates and the pelvis tilts toward the side back.17 The deformity correction operation will affect the spinopelvic parameters. Several studies explain why the effect of spondylolisthesis surgery on correction of spondylolisthesis parameters can occur spontaneously. With reduced listhesis, it is expected that the center of gravity will move to posterior, the pelvis will tilt to anterior, the sacral slope will be greater because the endplate of the sacrum is more vertical, and the LL will be increased. In a study conducted by Kong et al,17 who performed surgical correction of degenerative spondylolisthesis, it was found that, after surgery, there were changes in all spinopelvic parameters. They found that the PT decreased and the SS and LL increased. These findings are in line with our study findings, where there was a decrease in pelvic tilt and an increase in sacral slope values immediately after surgery. Based on the literature, the cause of changes in the spinopelvis that are not too prominent in cases of lumbar degenerative spondylolisthesis is because usually, in lumbar degenerative spondylolisthesis, the listhesis that occurs is low-grade (Meyerding I–II), so the magnitude of the reduction after surgery is usually not great. Also, most patients can achieve a satisfactory reduction in listhesis or slippage and, therefore, it will be difficult to find a correlation between spondylolisthesis and the spinopelvic parameters.17
Study Limitation
The sample size could be larger for this common DLS. Furthermore, the method of fusion was not the same for all subjects because some patients were treated using posterolateral interbody fusion while others transforaminal interbody fusion.
Conclusion
This study showed that reduction surgery using long arm pedicle screws was able to reduce the listhesis effectively up to 85.5%, and able to restore parts of spinopelvic parameters, namely, pelvic tilt and sacral slope approaching normal values.
Ethical Clearance
Ethical approval was obtained from the hospital and educational institution. The ethics committee did not require the patients to review their medical records as the surgery performed was the standard treatment in this hospital. The patients’ data were kept confidentially by the hospital and the information yielded from the medical records was used for research purposes only, which complied with the Declaration of Helsinki.
Acknowledgment
The authors would like to thank Cipto Mangunkusumo Hospital and Fatmawati General Hospital for providing the sources and chance to perform this research.
Funding
This research received no grant from any parties.
Disclosure
The authors declare that there is no conflict of interest for this study.
References
1. Matz PG, Meagher RJ, Lamer T, et al. Guideline summary review: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine J. 2016;16(3):439–448. doi:10.1016/j.spinee.2015.11.055
2. Garfin S, Eismont F, Bell G, Fischrund J, Bono C. Rothman-Simeone and Herkowitz the Spine Seventh Edition. Philadelphia: Elsevier; 2018.
3. Mesfin A, Sherif SM, Liu AY, Liu SE, Ba PJ, Menga EN. 197. Prevalence of isthmic and degenerative lumbar spondylolisthesis: analysis of 882 CT scans. Spine J. 2019;19(9):18–19. doi:10.1016/j.spinee.2019.05.214
4. Farfan HF. The pathological anatomy of degenerative spondylolisthesis: a cadaver study. Spine. 1980;5(5):412–418. doi:10.1097/00007632-198009000-00004
5. Simmonds AM, Rampersaud YR, Dvorak MF, Dea N, Melnyk AD, Fisher CG. Defining the inherent stability of degenerative spondylolisthesis: a systematic review. J Neurosurg Spine. 2015;23(2):178–189. doi:10.3171/2014.11.SPINE1426
6. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356(22):2257–2270. doi:10.1056/NEJMoa070302
7. Bradford DS. Treatment of severe spondylolisthesis: a combined approach for reduction and stabilization. Spine. 1979;4(5):423–429. doi:10.1097/00007632-197909000-00006
8. Scaglietti O, Frontino G, Bartolozzi P. Technique of anatomical reduction of lumbar spondylolisthesis and its surgical stabilization. Clin Orthop Relat Res. 1976:164???175. doi:10.1097/00003086-197606000-00021
9. Saleh I, Librianto D. Surgical treatment of spondylolisthesis using long arm screw: a literature review. Ann Med Surg. 2022;73:103200. doi:10.1016/j.amsu.2021.103200
10. Bhosale S, Pinto D, Srivastava S, Purohit S, Gautham S. Journal of clinical orthopaedics and trauma measurement of spinopelvic parameters in healthy adults of Indian origin e A cross sectional study. J Clin Orthop Trauma. 2019;3–8. doi:10.1016/j.jcot.2019.07.013
11. Deng M, Xiang Y, Wang J, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: a systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Transl. 2016;2016:1–14.
12. Manchikanti L, Singh V, Datta S, Cohen S, Hirsch J. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12:E35e70.
13. Rollman GB, Ph D, Lautenbacher S, Ph D. Sex differences in musculoskeletal pain. Clin J Pain. 2001;17(1):20–24. doi:10.1097/00002508-200103000-00004
14. Hitchon PW, Mahoney JM, Harris JA, et al. Biomechanical evaluation of traditional posterior versus anterior spondylolisthesis reduction in a cadaveric grade I slip model. J Neurosurg Spine. 2019:1–9. doi:10.3171/2019.2.SPINE18726
15. Yamaguchi H, Nojiri H, Miyagawa K, Inoue N, Kaneko K. Segmental coupling effects during correction of three-dimensional lumbar deformity using lateral lumbar interbody fusion. Eur Spine J. 2020;29(4):879–885. doi:10.1007/s00586-020-06310-0
16. Chumnanvej S. Determination of spinopelvic parameters in degenerative lumbar spondylolisthesis patients undergoing lumbosacral spine fusion surgery: the lesson learnt. Turk Neurosurg. 2018;29:0–6.
17. Kong L-D, Zhang Y-Z, Wang F, Kong F-L, Ding W-Y, Shen Y. Radiographic restoration of sagittal spinopelvic alignment after posterior lumbar interbody fusion in degenerative spondylolisthesis. J Spinal Disord Tech. 2022;29:E87–E92.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

