Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 15
Quantitative and Qualitative Correlation of Mandibular Lingual Bone with Risk Factors for Third Molar Using Cone Beam Computed Tomography
Authors Halder M, Chhaparwal Y , Patil V, Smriti K, Chhaparwal S, Pentapati KC
Received 25 July 2023
Accepted for publication 15 September 2023
Published 30 October 2023 Volume 2023:15 Pages 267—277
DOI https://doi.org/10.2147/CCIDE.S428908
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Christopher E. Okunseri
Mehuli Halder,1 Yogesh Chhaparwal,1 Vathsala Patil,1 Komal Smriti,1 Shubha Chhaparwal,2 Kalyana C Pentapati3
1Department of Oral Medicine and Radiology, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, 576104, India; 2Department of Conservative Dentistry and Endodontics, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, 576104, India; 3Department of Public Health Dentistry, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, 576104, India
Correspondence: Yogesh Chhaparwal, Department of Oral Medicine and Radiology, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, 576104, India, Tel +91 9986454730, Email [email protected]
Background: Lingual plate thickness, density, and proximity to the tooth are linked as risk factors for various complications associated with third molar extraction. The present study aimed to assess the lingual plate thickness, and density in the mandibular third molar region using cone beam computed tomography and to estimate its correlation with type and level of impaction, number of roots, age, and gender as the risk factors
Methods: This was a retrospective study on CBCT images of 648 mandibular third molars. The lingual plate thickness at three different root levels – cervical, mid-root, and apex along with the position of the tooth, number of roots, density of lingual plate, age, and gender were evaluated. The measurements were done on Invivo 5-Anatomage software. Statistical comparison of the categorical variables was done by Chi-square test, and Fisher’s exact test, and univariate and multivariate analysis were done using binomial logistic regression.
Results: Lingual plate thickness of the third molars at the cervical, mid root, and apex were 1.28 mm, 1.42 mm and .01 mm (mean). A significantly higher proportion of subjects with thin lingual plates at mid-root (p-value=0.01) and apex (p-value=0.05) were in the 21– 30 age group. Lingual bone density was significantly associated with the thickness of the lingual plate at the mid-root. A significantly higher proportion of thinner lingual plates at the mid-root level were associated with mesioangularly placed third molars (p-value=0.002).
Conclusion: Our study presented that lingual plate thickness has a strong association with age, angulation, and the number of roots. Knowledge about these risk factors is imperative during the management of third molar impactions.
Keywords: lingual plate, third molar, bone density, mandible, cone-beam computed tomography
Introduction
The most consistently impacted tooth in the oral cavity is mandibular third molar. Its extraction can lead to diverse surgical difficulties like pain, swelling, or trismus which are the most common and minor ones, while nerve damage, lingual plate fracture and accidental displacement of root into fascial tissue spaces are more unusual and critical that can lead to permanent paraesthesia, hypoesthesia, altered sensation, speech or chewing disabilities. Hence, assessment of surgical difficulties and risks is fundamental prior to extraction of these teeth. Risk factors can be assessed using dental factors on radiographs pre-operatively, assessing the surgical site during surgery and also by relating clinical variables like age, gender etc.1
Various studies have reported the correlation between the lingual plate and its connection to the mandibular third molar. Tolstunov et al2 addressed that in the majority of cases, the lingual plate fractures were seen during the extraction of mesioangular and horizontally impacted mandibular third molars wherein the lingual bone thickness at the apical third was less than 1mm. However, another study showed that vertically impacted teeth were more critical in comparison to mesioangular impacted.3 Approximation of the apex of the tooth to the lingual cortical plate is also associated with higher intra and post-operative difficulties.4,5 Poor surgical skills, thinner lingual cortical plate, and configuration of the impacted teeth are risks for lingual plate fracture and lingual nerve injury. Likewise, patient age, duration of the procedure, depth of impaction, and expertise of the surgeon are other risk factors.6–8 Lingual bone quantity and quality are the two main factors associated with third molar extraction. Quantity of lingual bone is the amount of cortical bone in terms of thickness of the bone and quality is the density of the cortical and medullary bone. Panoramic radiographs and Lateral Cephalograms in the dry sectioned mandibles have been used to measure the quality and quantity of bones. However, the measurements of 2-Dimensional imaging modalities are less reliable in comparison to real mandible due to their inherent magnification and distortion and use of dry sectioned mandibles is a complex procedure. Hence, three-dimensional imaging modality like Cone Beam Computed Tomography is a preferable choice as it is non-invasive and provides good-quality images with higher resolution which can be visualized on all three sections.9–11
Hence, the present study aimed to assess the lingual plate thickness along with bone density in the mandibular third molar region using cone beam computed tomography and to estimate its correlation with the type of impaction, level of impaction, number of third molar roots, age, and gender as risk factors.
Materials and Methods
This retrospective observational study was reviewed and approved by Institutional Ethics Committee (IEC 772-2020) in compliance with the declaration of Helsinki. The radiographic study was conducted retrospectively using CBCT images of mandibular third molars that were compiled during the time period of January 2017 to January 2020 from 590 patients from the archives of the Department of Oral Medicine and Radiology. The patients who had undergone CBCT scanning for several reasons like third molar removal, endodontic treatment, and implant surgeries were only considered for the study.
CBCT images of good quality with complete visibility of the mandibular third molar in any configuration (whether teeth erupted fully or partially, or impacted teeth) with the adjoining alveolar bone were included CBCT images of poor quality that hinder the evaluation of anatomic structures, mandibular third molars with incomplete root formation and root resorption, third molars with large carious lesions and periapical bony changes and anatomical changes secondary to surgical treatment about third molars were excluded. The images were obtained using an i-CAT FLX Cone Beam 3D system with a suitable FOV size operated at 1 kV and 5mA. The thickness of the slice was 0.5mm and images were evaluated using i-CAT ViSiONTM and Invivo 5 ver.5.3 Anatomage software. Images were analyzed in appropriate Axial, Sagittal, and Coronal planes.
Radiographic Measurements
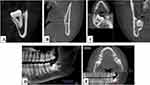
The CBCT images were categorized age-wise into 4 groups ≤20 years, 21–30 years, 31–40 years, and >41 years, respectively. Images were assessed for the following parameters as shown in Figure 1.
- Position of the third molar (left/right side of the mandible);
- Number of third molar roots (one-rooted, two-rooted, or multirooted);
- The depth of impaction of third molars was classified according to the Pell-Gregory classification as Level A (high), Level B (middle), or Level C (low)9 as shown in Figures 2 and 3.
- Level A: When the occlusal plane of the impacted tooth is at the same level as the occlusal plane of the adjacent second molar.
- Level B: When the occlusal plane of the impacted tooth is between the occlusal plane and the cervical line of the adjacent second molar.
- Level C: When the impacted tooth is below the cervical line of the adjacent second molar;
- Measurement of thickness at the root apex.
- The mesiodistal angulation of the third molar, which was calculated by measuring the angle between the imaginary central axis (beginning at the central fossa up to the middle of the pulp chamber) of the third molar through to the imaginary central axis of the adjoining second molar in the coronal section. This was done according to Winter’s classification9 and then marked as either “distoangular”, “vertical”, “mesioangular” or “horizontal” Figure 4.
- The buccolingual angulation, was to determine whether the tooth was buccally or lingually aligned as compared to the mandibular second molar. For teeth that were more mesioangular/horizontally erupted third molars the angle was determined from the imaginary central axis bisecting the pulp chambers of the first molar and second molar in the middle, on the Axial section. Lingual angulation was assigned a negative value (-) and buccal angulation of the crown was assigned a positive value (+). A line parallel to the line bisecting the second molar was marked and measurement of the difference in the lingual or buccal angulation was done. Buccolingual angulation >5 degrees was considered as “buccal”, < – 5 degrees was considered as “lingual”. The remaining were considered to be “central”.
- The lingual plate thickness of each tooth was assessed at three different root levels - cervical, mid-root, and at apex. A relevant coronal slice of the tooth was selected and the cervical third, mid-root, and apex were identified and measurements were made from different root levels to the outer lingual cortical plate. Bone width of more than 1mm was considered as thicker and the width of lesser than 1 mm was considered as thinner. In cases where the outer lingual plate was perforated, the width of the lingual bone was considered to be 0mm.
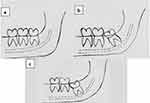 |
Figure 2 Pell and Gregory classification (Impaction Depth) (a) Level A. (b) Level B. (c) Level C. |
 |
Figure 3 Pell and Gregory Classification. (A) Class 1. (B) Class 2. (C) Class 3. |
 |
Figure 4 Winters classification. (A) Vertical impaction. (B) Mesioangular impaction. (C) Horizontal impaction. (D) Distoangular impaction. (E) Bucco-lingual impaction. (F) Others. |
All the parameters were evaluated by single observer (Post-Graduate Student – Oral and Maxillofacial Radiologist with 4 years of experience in the field). This was done after arriving at consensus with a trained Oral and Maxillofacial Radiologist with 14 years of experience in the field. A ten percent of the sample size was evaluated 2nd time by the first observer itself after a gap of 2 weeks for evaluating the intra observer reliability. To evaluate inter-observer variability, 10% of the sample size were analysed by second observer (Oral and Maxillofacial Radiologist with 7 years of experience). The intraclass correlation coefficient was used to ensure inter and intra-observer agreement and reproducibility of measurements.
Statistical Analysis
All the data were analysed using SPSS software (version 18). A p-value of ≤0.05 was considered to be statistically significant. The comparison of the categorical variables was done using the Chi-square test or Fisher’s exact test based on the distribution of the test. The mean bone density at the mid-root level was compared between thin and thick lingual plates at the mid-root level using the Mann–Whitney U-test. Univariate and multivariate analysis was done using Binomial logistic regression with lingual plate thickness at cervical, middle, and apical levels as the dependent variable for significant independent variables in bivariate analysis. Independent variables used were age, gender, mesiodistal and buccolingual angulation, number of roots, side, bone density, and impaction depth.
Cohen κ test was used to estimate inter and intra-observer agreements wherein κ showed perfect agreements with the Wilcoxon signed rank test showing no significant difference between the Lingual plate thickness at the cervical, mid-root, and apex along with the Lingual plate density at the mid-root level.
Results
The study sample comprised 648 third mandibular molars. A maximum number of mandibular third molars (437) belonged to the 21–30 age group and the minimum number of mandibular third molars (17) belonged to the age group of more than 40. The mean age was 24.25 years (standard deviation 5.502; range, 17–54 years). Three hundred and thirty-three mandibular third molars belonged to males (51.4%) and 315 to females (48.6%). Out of the 648 mandibular third molars, 35 were single-rooted (5.4%), 504 teeth had two roots (77.8%) and 109 had more than two roots (16.8%).
The level of impaction, mesiodistal angulation, and buccolingual angulation of mandibular third molars is depicted in Table 1. Out of 648 third molars, 251 (38.7%) had the highest portion above or parallel to the occlusal plane of the adjacent second molar ie, Level A; 87 third molars (13.4%) had the highest portion between the occlusal plane and cervical line of the adjacent second molar ie, Level B and 310 third molars (47.8%) had the highest portion below the cervical line of adjacent second molar-Level C according to the Pell-Gregory classification. The mesiodistal angulation was recorded as per the Winters classification which showed 382 third molars to be mesioangularly placed (59%), 138 were vertically angulated (21.3%), 78 were horizontally placed (12%) and 45 were distoangular third molars (6.9%). There were 388 third mandibular molars (59.9%) that were lingually angulated, 203 third mandibular (31.3%) were buccally angulated, and 57 third mandibular (8.8%) were centrally placed.
 |
Table 1 Table Shows the Impaction Depth, Mesiodistal Angulation, and Buccolingual Angulation of the 648 Mandibular Third Molars |
Lingual plate thickness of the mandibular third molar at the cervical level was 1.28 mm (mean); at the mid-root level was 1.42 mm (mean); at the apex was 1.01 mm (mean). The mean density of the Lingual cortical plate was 1198.04 HU (SD 231.24 HU). The thickness of the lingual plate based on age wise and gender is described in Table 2. Third molars belonging to the age group of 21–30 years showed thinner lingual plate at the cervical (71.3%), mid-root (71.7%), and apex (69.8%). A significantly higher proportion of subjects with a thin lingual plate at the apex belonged to the 21–30 age group when compared to the thick lingual plate (p-value 0.05). A significantly higher proportion of subjects with thin lingual plates at the mid-root were in the 21–30 age group when compared to the thick lingual plate (p-value 0.01). No significant difference in the distribution of lingual plate thickness at the cervical level among the various age groups and lingual plate thickness at all three levels among sexes was noted.
 |
Table 2 Age Groups and Gender with Lingual Plate Thickness at Cervical, Mid-Root, and Apex Along with p-values |
Lingual plate thickness varies according to the right and left side of the mandible and the number of roots was also evaluated (Table 3). A significantly higher proportion of subjects with thick lingual plates at the mid-root level had an association with the number of roots (p-value 0.05). No significant difference in the distribution of lingual plate thickness at the cervical level and the apex among the number of roots and lingual plate thickness at all 3 levels with the tooth number noted.
 |
Table 3 Lingual Plate Thickness at Cervical, Mid-Root, and Apex with the Position ie, Whether Right or Left Along with the Number of Roots of the Mandibular Third Molars |
Lingual plate thickness based on the impaction depth, mesioangular angulation, and buccolingual angulation showed that a significantly higher proportion of subjects with thin lingual plates at a mid-root level were associated with mesiodistal angulation. (p-value 0.002) and no significant difference in the distribution of lingual plate thickness at the cervical level and apex with the mesiodistal angulation noted.
A significantly higher proportion of subjects with a similar proportion of lingual plate thickness at the apex were associated with buccolingual angulation. (p-value 0.054) and no significant difference in the distribution of lingual plate thickness at the cervical and mid-root level with the buccolingual angulation noted. No significant difference in the distribution of lingual plate thickness at all 3 levels with the impaction depth noted (Table 4).
 |
Table 4 Compares the Lingual Plate Thickness at the Cervical, Mid-Root, and Apex with the Impaction Depth, Mesioangular Angulation, and Buccolingual Angulation |
Lingual plate density at the mid-root level for the 209 teeth with thinner (less than 1mm) lingual cortical plates was found to be 1121.86 (SD 248.29) and the mean for the 439 teeth with thicker (more than 1mm) lingual plates was 1222.81 (SD 220.07). Lingual plate density is significantly associated with lingual plate thickness at mid-root (P value of <0.001).
Univariate analysis showed that the age group of patients more than 40 years had a higher Odds ratio of the thick cortical plate at the mid-root level (OR 5.9, p-value of 0.007) Table 5. Multivariate analysis of lingual plate thickness at the mid-root had a significant association with the 21–30 age group. Univariate analysis showed that the double and multi-rooted teeth had a significant association with lingual plate thickness at the mid-root (OR 2.4, 2.2; p-value 0.01, 0.04 respectively). Multivariate analysis showed double and multi-rooted teeth had retained the significant association that was seen with the univariate analysis Table 6.
 |
Table 5 Univariate and Multivariate Analysis of the Lingual Plate Thickness at a Mid-Root Level Compared with Variables of Age, Mesiodistal Angulation, Number of Roots, and Lingual Plate Density |
 |
Table 6 Univariate and Multivariate Analysis of the Lingual Plate Thickness at the Apex Compared with Variables of Age and Buccolingual Angulation |
Discussion
Third molars are the most commonly impacted teeth. These often result in recurrent pericoronitis, cystic changes, swellings, and resorption of adjacent teeth. The most opted treatment modality for third molars is extractions which can be associated with numerous complications. The anatomy and morphology of the third molar and its surrounding bone contribute significantly as risk factors for surgical complications. Studies have reported lingual plate morphology, its thickness, and density along with the type of impaction angulation and depth of impaction are the risk factors associated with third molar extraction complications.5 Therefore, complete understanding and analysis of the anatomy of the lingual plate and its relation with the third molar is beneficial to prevent such complications and also for communicating with patients about the risks before surgery. Panoramic radiographs are the routinely used screening radiograph for visualization of impacted third molars. It is a two-dimensional imaging modality with inherent magnification which precludes accurate information about the third molar region. Cone Beam Computed Tomography (CBCT), is a 3-dimensional imaging modality with high definition, higher spatial resolution, and better quality images in all three sections; axial, coronal, and sagittal. Therefore, in the present study, all the measurements were done on CBCT images and it has shown good intra and inter-observer reliability.7
The study encompassed 648 mandibular third molars of 333 males and 315 females. The sample size was higher compared to previous studies.5,10,11 The present study did not show any significant correlation between the thickness] of a lingual plate with gender. But the findings of the study were not by the previous research12 which showed an increase in cortical bone thickness in women with age compared to men. This non-consensus could be due to our sample size belonging to different ethnicity than previous studies.
The present study analysed the association between lingual plate thickness and age. We noted that lingual plate thickness was significantly thinner at the apical and, mid root in 3rd molars belonging to younger age groups (21–30 years). This finding was in agreement with the study done by Aksoy et al13 wherein they also reported, the 15–25 years’ age group had significantly thinner/perforated cortical plates when compared with the 46–76 years’ age group. Similar observations were reported by Wang et al5 that the incidence of perforation decreases with age. However, in contrast to these findings, the study by Huang et al14 did not record any significant difference between age groups.
Previous studies have reported the lingual plate thickness in the region of root apex on CBCT images ranged from 0.99 to 3.38mm.4,5 The present study also showed a similar value with the mean lingual plate thickness of the mandibular third molar at the apex as 1.01mm and lesser than that measured at the middle third and cervical third of the root. On the contrary, a study by Huang et al14 Mallick et al10 and Emes et al,4 was not in agreement with this, as they reported lingual plate thickness at the level of mid-root to be thinner than that at the apical third of the root. This difference might be attributed to different measurement methods, different groups of population and differences in case selection. The findings of our study further warrant that the root apex of the impacted third molar is spatially close to the lingual plate of the mandible, which represents an anatomic risk factor.
The mean density of the Lingual cortical plate at the mid-root level was 1198.04 HU with Lingual plate density significantly associated with the thickness of the lingual plate at mid-root level. To the best of our knowledge, this is the first study to evaluate and correlate the density calculated using the Hounsfield unit on CBCT with lingual plate thickness on impacted third molars.
The majority of the third molars in our study were at Level C impaction (47.8%) which was similar to the studies done by Huang et al14 and Nguyen et al15 59% were mesioangularly impacted and 21.3% were vertically angulated and 12% were horizontally impacted and 6.9% were distoangular third molars. This was in accordance with Huang et al.14 Tolstunov et al reported that erosion in the lingual plate was more at the third molar apex region and was significantly associated with the angulation of the impacted third molar.2
Among Bucco lingual angulation 59.9% of mandibular third molars were lingually angulated, 31.3% were buccally angulated and 8.8% were centrally positioned whereas in research conducted by Huang et al and Ge et al,12,14 amongst the deeply impacted third molars, the lingually impacted belonged to largest group followed by the centrally placed and buccally placed.
Deeper impactions are at higher risk of complications due to thinner surrounding bone.10 In our study, a significantly higher proportion of thinner lingual plates at mid-root level were associated with mesioangularly placed third molars. Huang et al14 reported that at the mid-root mesiodistal angulation was significantly associated with an increased probability of a thinner and perforated lingual plate. Tolstunov et al2 stated that bone around horizontal and mesioangularly impacted third molars was 3.6 times more likely to be thinner than the width of the same bone around vertically and distoangularly impacted teeth at the level of the mid-root. However, Menziletoglu et al3 found that at the mid-root level, thinner lingual bone was noted in the horizontally impacted teeth. A study by Wang et al5 revealed that the root apex had the possibility of perforations beyond the cortical plate border in teeth with horizontal and mesial impaction. This can be attributed to the anatomic structure of the mylohyoid ridge, the internal oblique ridge present on the lingual aspect of the mandible. The ridge coincides with the apical region of the root and it might strengthen the lingual cortex around the root apex mandibular third molar.11
The limitation of the present study is that there is minimal evidence of a correlation of Hounsfield Unit (HU) in CBCT compared to CT for standardized quantification of bone density. Further validation is required. Also, our sample comprised Indian subpopulations with a lack of other ethnic and geographical backgrounds, hence extrapolation of the results needs multi-centric studies with a larger sample size.
Conclusion
Lingual bone is a natural hard tissue barrier between the impacted mandibular third molars and other vital structures on the mandibular lingual aspect. Lingual plate thickness had a strong association at the mid-root level in the age group of 21–30 years, mesio-distal angulation, double and multi-rooted teeth. Also, lingual plate thickness at the apex showed a significant association in the age group above 40 years and centrally angulated teeth. Good awareness about these risk factors during the management of third molar impactions will help to avoid complications.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki. It was approved by the Ethics Committee of Kasturba Hospital and Kasturba Medical College institutional ethics committee (IEC 772-2020), exempting informed consent due to the retrospective study design. All the patient records were delinked and anonymized before recording data for this study to ensure the confidentiality of the participants.
Acknowledgement
We are grateful to the Department of Oral and Maxillofacial Radiology, Manipal College of Dental Sciences, Manipal for providing us with all the scans and other technical support during the conduct of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Gbotolorun OM, Arotiba GT, Ladeinde AL. Assessment of factors associated with surgical difficulty in impacted mandibular third molar extraction. J Oral Maxillofac Surg. 2007;65(10):1977–1983. doi:10.1016/j.joms.2006.06.285
2. Tolstunov L, Brickeen M, Kamanin V, Susarla SM, Selvi F. Is the angulation of mandibular third molars associated with the thickness of lingual bone? Br J Oral Maxillofac Surg. 2016;54(8):914–919. doi:10.1016/j.bjoms.2016.07.004
3. Menziletoglu D, Tassoker M, Kubilay-Isik B, Esen A. The assessment of the relationship between the angulation of impacted mandibular third molar teeth and the thickness of lingual bone: a prospective clinical study. Med Oral Patol Oral Cir Bucal. 2019;24(1):e130–e135. doi:10.4317/medoral.22663
4. Emes Y, Öncu B, Aybar B, et al. Measurement of the lingual position of the lower third molar roots using cone-beam computed tomography. J Oral Maxillofac Surg. 2015;73(1):13–17. doi:10.1016/j.joms.2014.09.008
5. Wang D, He X, Wang Y, et al. Topographic relationship between root apex of mesially and horizontally impacted mandibular third molar and lingual plate: cross-sectional analysis using CBCT. Sci Rep. 2016;6:38955. doi:10.1038/srep38955
6. Parada C, Chai Y. Mandible and tongue development. Curr Top Dev Biol. 2015;115:31–58. doi:10.1016/bs.ctdb.2015.07.023
7. Guerrero ME, Jacobs R, Loubele M, Schutyser F, Suetens P, van Steenberghe D. The diagnostic efficacy of cone beam computed tomography for impacted teeth and associated features: a systematic review. J Oral Rehabil. 2011;38(3):208–216. doi:10.1111/j.1365-2842.2010.02141.x
8. Pauwels R, Araki K, Siewerdsen JH, Thongvigitmanee SS. Technical aspects of dental CBCT: state of the art. Dentomaxillofac Radiol. 2015;44(1):20140224. doi:10.1259/dmfr.20140224
9. Yilmaz S, Adisen MZ, Misirlioglu M, Yorubulut S. Assessment of third molar impaction pattern and associated clinical symptoms in a Central Anatolian Turkish population. Med Princ Pract. 2016;25(2):169–175. doi:10.1159/000442416
10. Mallick A, Vidya KC, Waran A, Rout SK. Measurement of lingual cortical plate thickness and lingual position of lower third molar roots using cone beam computed tomography. J Int Soc Prev Community Dent. 2017;7(7):S8–12. doi:10.4103/jispcd.JISPCD_106_17
11. Sathapana S, Forrest A, Monsour P, Naser-Ud-Din S. Age-related changes in maxillary and mandibular cortical bone thickness in relation to temporary anchorage device placement. Aust Dent J. 2013;58(1):67–74. doi:10.1111/adj.12018
12. Ge J, Zheng JW, Yang C, Qian WT. Variations in the buccal-lingual alveolar bone thickness of impacted mandibular third molar: our classification and treatment perspectives. Sci Rep. 2016;6(1):16375. doi:10.1038/srep16375
13. Aksoy U, Orhan K. Risk factor in endodontic treatment: Topographic evaluation of mandibular posterior teeth and lingual cortical plate using cone beam computed tomography (CT). Med Sci Monit. 2018;24(11):7508–7516. doi:10.12659/MSM.908869
14. Huang C, Zhou C, Xu M, Zou D. Risk factors for lingual plate fracture during mandibular third molar extraction. Clin Oral Investig. 2020;24(11):4133–4142. doi:10.1007/s00784-020-03286-5
15. Nguyen DP‐A, Le SH, Nguyen CTK, Dien VHA, Nguyen LT‐B, et al. The vulnerability of lingual plate of the mesioangular impacted mandibular third molars: A measurement on CBCT images. Oral Surg. 2020;14(2):106–112. doi:10.1111/ors.12543
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.