Back to Journals » Cancer Management and Research » Volume 11
Quality of life of patients with proximal humerus metastasis treated with cement spacer
Authors Guo W , Gao X, Wang D, Wang T, Tang L, Wang Y, Liu B
Received 12 June 2019
Accepted for publication 23 August 2019
Published 17 September 2019 Volume 2019:11 Pages 8499—8506
DOI https://doi.org/10.2147/CMAR.S219178
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Eileen O'Reilly
Wen Guo,1,* Xin Gao,2,* Dongsheng Wang,2,* Tao Wang,2 Liang Tang,2 Yao Wang,2 Bin Liu3,*
1Department of Orthopedics, Taizhou Peopleʼs Hospital, Taizhou 225300, Jiangsu, People’s Republic of China; 2Orthopaedic Oncology Center, Department of Orthopaedics, Changzheng Hospital, Second Military Medical University, Shanghai 200000, People’s Republic of China; 3Department of Bone and Soft Tissue Neurosurgery, Affiliated Tumor Hospital of Guangxi Medical University, Nanning 530021, Guangxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wen Guo
Department of Orthopedics, Taizhou People’s Hospital, No.366 Taihu Road, Taizhou 225300, Jiangsu, People’s Republic of China
Email [email protected]
Bin Liu
Department of Bone and Soft Tissue Neurosurgery, Affiliated Tumor Hospital of Guangxi Medical University, 71 He Di Road, Nanning 530021, Guangxi, People’s Republic of China
Email [email protected]
Purpose: The goal of this study was to determine whether the surgery using cement spacer could improve the quality of life of patients with proximal humerus metastasis.
Patients and methods: This is a retrospective study. The study included 34 patients who had been treated for proximal humerus metastasis between January 2010 and June 2014. The patients were divided into surgical and non-surgical group depending on whether they underwent cement spacer surgery. The patient’s quality of life (QOL) assessment is scheduled at five points—at the initial diagnosis (baseline) and at 1 month, 3 months, 6 months, and 9 months of follow-up. Evaluation tool is Functional Assessment of Cancer Therapy-General (FACT-G) questionnaire.
Results: A total of 34 patients, including 15 patients in the surgery group and 19 patients in the non-surgery group, were enrolled in this retrospective study. In the end, 22 patients finished all evaluations, including 11 patients in the surgical group and 11 patients in the non-surgery group. At the completion of the study, 22 patients had died, including 8 patients in the surgery group and 14 patients in the non-surgery group. After surgical using the cement spacer, the QOL scores of patients at each follow-up point were significantly higher than that of preoperative scores. These scores were also higher than those of the non-surgery group.
Conclusion: The current study indicated that surgical treatment using the cement spacer could upgrade and maintain quality of life for patients with proximal humerus metastasis in the 9-month assessment.
Keywords: cement spacer, proximal humerus metastasis, quality of life, palliative treatment
Introduction
The proximal humerus is a common site of bone metastasis. Lesions at this location often occur in the advanced stages of cancer.1 Pathological fractures of the proximal humerus are common, and usually require a long time to heal, while up to 50% of the cases never heal.3 This can lead to intractable pain, limb dysfunction, and serious physiological and psychological effects on these patients’ quality of life (QOL). Because metastasis of the proximal humerus (MPH) is incurable at current medical levels, and the expected survival time is relatively short, the development of treatment plans should be targeted at improving the QOL as much as possible.
Limb salvage has evolved to represent the preferred treatment method of bone metastases in the proximal humerus.2 Wide en bloc intra-articular excision and reconstruction of the defect with nail cement spacer is a traditional palliative therapy for MPH.3 The advantages of this method include a low cost, a relatively easy surgical procedure, rapid recovery of limb function, and easy patient management.4 While reconstruction of the defect with nail cement spacer improves functional outcome in patients with metastases of the proximal humerus, the impact on QOL and survival is not well established.
The notion of QOL was proposed in the 1970s to reflect the physical and emotional experience of the patients after treatment.5 From then on, the consensus has gradually formed that improving QOL is more important than traditional therapeutic objectives such as prolonged survival in most palliative treatments.6 QOL assessment of patients with a primary tumor has been successfully conducted through effective questionnaires.7,8 However, for proximal humerus metastasis (MPH), as far as we know, few studies have focused on the differences between surgical treatment using cement spacer and non-surgical treatment in improving the QOL. Therefore, we carried out a retrospective research to compare the impact on QOL between treatment with cement spacer and treatment with non-surgery therapy in order to offer an additional reference in clinical decision-making for these patients.
Materials and methods
Clinical data
A retrospective review was performed of proximal humerus metastasis that had been treated in our department between 2010 and 2014. A total of 45 patients with MPH were at our department in this time period. The inclusion criteria were: (1) pathologically confirmed MPH; (2) presence of a surgical indication including pathological fracture, impending fracture, which was evaluated with the Mirels scale9 or (3) intractable pain that is difficult to control with anesthesia or radiation therapy. (4) In addition, an expected survival time of 3–12 months according to the Katagiri scale10 was required. The expected survival of patients was estimated based on the primary tumor, previous chemotherapy, presence of multiple bone metastases, presence of visceral metastases, and performance status according to the ECOG scale.11 Of these 45 patients, 38 patients were eligible for analysis, 7 patients were excluded because 3 patients have no surgical indications, 3 patients’ expected survival time was less than 3 months, 1 patients’ survival time was larger than 12 months. Of the 38 patients, 4 patients had been lost for follow-up, and a total of 34 patients were included in this study (Figure 1). The clinical records, radiographic data and pathological reports of all patients were reviewed by two individual researchers. The FACT-G scores, Musculoskeletal Tumor Society scores (MSTS), visual analogy scores (VAS), Eastern Cooperative Oncology Group performance score (ECOG-PS) were used to evaluate the QOL, limb function, degree of pain and performance status, respectively. These data were recorded during hospitalization and follow-up. Patients were followed up at 1, 3, 6 and 9 months after surgery. The patient’s final state was obtained through an outpatient visit or a telephone follow-up. For the missing data, the relevant information was obtained by telephone communication. Surgical treatment is recommended for all patients who meet the selection criteria. After objectively emphasizing the importance of the operation and explaining in detail the risks and costs of the operation, it is up to the patients and the family members to decide whether to undergo surgical intervention. Fifteen patients who eventually opted for surgical intervention were included in the surgical group, and 19 cases of refusal of surgical intervention were included in the non-operative group. Adjuvant treatment of patients in both groups included radiotherapy (mean dose 30 Gy) and chemotherapy. Patients in the surgery group were administered by limb-sparing tumor excision. The proximal humerus was resected and reconstructed with antibiotic bone cement supported by intramedullary nails. The choice of adjuvant therapy was determined by the nature of the primary tumor and the specific circumstances of the disease. This retrospective study was approved by the Institutional Review Board of Taizhou People’s Hospital in Jiangsu Province. The written informed consent was not required by the Institutional Review Board due to the retrospective property. We are committed to protecting the confidentiality of patients, and the study was conducted in accordance with the Helsinki Declaration.
 |
Figure 1 Patient flow diagram. |
QOL questionnaire assessment
The Functional Assessment of Cancer Therapy-General (FACT-G) questionnaire is a patient self-assessment system evaluating different dimensions of QOL. This questionnaire is one of the most effective tools used to assess the QOL of cancer patients and has been confirmed to be applicable to the Chinese population. It contains four aspects: physical well-being (seven questions), social/family well-being (seven questions), emotional well-being (six questions), and functional well-being (seven questions). The score range for each specific item is 0–4 points. 0 stands for “not at all” and 4 for “extraordinary”. The highest score is 108 points. A higher total score represents a better QOL.
Statistical analysis
Baseline data comparisons between the surgical and non-operative groups were carried out through the T-test and Fisher’s exact tests. Difference in the same treatment group was analyzed by repeated measurement of variance. Differences between the two treatment groups were also analyzed using the same method. The comparison of scores at one, three, six, and nine months in each field between the groups was analyzed with paired t-tests.
Kaplan-Meier curves were plotted, and comparison of the overall survival between the two groups was carried out with the log-rank test. p<0.05 was considered statistically significant level in all analyses. All the statistical analyses were carried out by SPSS 22.0 (SPSS Inc., Chicago, Illinois).
Results
Demographic data
Baseline data for these 34 patients are listed in Table 1. There were no statistically significant differences in baseline parameters between both groups. After surgery, nine (60%) patients in the surgery group received radiotherapy, thirteen (86.7%) received chemotherapy, and eleven (73%) received bisphosphonate therapy, and the corresponding numbers (percentages) for the nonsurgery group were fifteen (78.9%), eighteen (94.7%), and fourteen (73.7%), respectively. One month after therapies, 75% of the patients in the surgical group achieved effective pain control, in comparison with only 45% of patients in the nonsurgery group.
 |
Table 1 Characteristics of the enrolled patients |
Quality of life
In this study, a total of 22 patients (11 in each group) completed the FACT-G scale data collection at all 5 time points. There was no statistically significant difference between both groups in any field of the FACT-G scale at baseline. At each follow-up point (1, 3, 6, and 9 months), the mean total QOL score of the surgical group was significantly higher than that of the non-surgical group, particularly at the 3 months follow-up evaluation (p<0.05).
Figure 2 shows the difference between the two groups of total QOL scores. The total QOL score of the surgical group increased gradually over time and reached its highest level at the 3rd month of follow-up, and then remained at a higher level. However, the total QOL score of the non-operative group showed a gradual downward trend. The magnitude of the change is also larger in the surgical group.
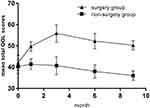 |
Figure 2 The differences between the two groups of total QOL scores are demonstrated from baseline to 9 months after diagnosis.Abbreviation: QOL, quality of life. |
Figure 3 shows the trend of physical well-being in both groups. A sharp rise in the physical score was observed for the surgery group, while an acute reduction was noticed in the nonsurgery group. Similar patterns were found for functional well-being (Figure 4) (p<0.001).
 |
Figure 3 The differences between the two groups of physical well-being QOL scores are demonstrated from baseline to 9 months after diagnosis.Abbreviation: QOL, quality of life. |
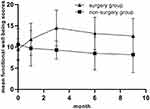 |
Figure 4 The differences between the two groups of functional well-being QOL scores are demonstrated from baseline to 9 months after diagnosis.Abbreviation: QOL, quality of life. |
Figure 5 shows the trend of emotional well-being, which shows a similar trend in the two sets of data, but the average level of the surgical group is higher (p<0.001).
 |
Figure 5 The differences between the two groups of emotional well-being QOL scores are demonstrated from baseline to 9 months after diagnosis.Abbreviation: QOL, quality of life. |
For the social/family well-being scores (Figure 6), the scores of the two groups did not vary substantially over time. This trend is similar with that of the emotional well-being, without a statistically significant difference (p=0.13).
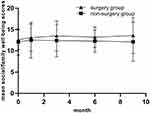 |
Figure 6 The differences between the two groups of social/family well-being QOL scores are demonstrated from baseline to 9 months after diagnosis.Abbreviation: QOL, quality of life. |
Survival analysis
At the completion of the study, 22 patients (64.7%) had died, including 8 patients (53.3%) in the surgery group and 14 patients (73.7%) in the non-surgery group. The mean survival time was 10.6 months (median, 12.0 months [95% confidence interval (CI), 6.4–17.6 months]) in the surgery group and 8.9 months (median, 10 months [95% CI, 6.3–13.7 months]) in the non-surgery group. There was no statistically significant difference in survival time between both groups (p=0.178) (Figure 7).
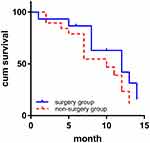 |
Figure 7 Kaplan-Meier curves demonstrating overall survival of the surgery and non-surgery groups (chi square =1.817, p=0.178, log-rank test). |
Discussion
The survival rate of patients with bone metastasis is very low, and the occurrence of complications related to bone tumors tends to worsen the prognosis of these patients.12 Patients with metastatic bone disease are not only concerned about whether the disease is curable, but also about the impact of treatment on their QOL. As a result, oncologists treat these patients with the aim of improving their QOL.1,13 In many clinical trials, a QOL assessment scale was used to evaluate the effectiveness of treatment, especially when it comes to incurable disease.14 Nevertheless, as far as we know, little is known on the QOL of patients with MPH. We performed a retrospective study to assess the effect of using a cement spacer on the QOL of patients with MPH.
The results suggest that, although surgical therapy did not prolong survival, it did significantly improve QOL. The total QOL score of MPH patients, evaluated with the FACT-G scale, was higher in the surgical group compared to the non-operative group. In the non-surgical group, the total QOL score showed a decreasing trend over time, reaching the lowest point at 9 months of follow-up, suggesting that non-surgical treatment does not improve QOL in these patients. Similar conclusions were reported by Yu Tang et al,6 who found that adjuvant therapy, including chemotherapy and radiotherapy, did not improve QOL in non-operated patients.
In China, the concept of family has Chinese characteristics. The traditional view is that the living, psychological dependence and financial burden of the sick family members, regardless of the severity of the disease, are borne by the family.15 These features will have an impact on the scores of the social/family well-being. In this study, the scores of the two groups in the field of the social/family well-being showed a steady trend of development over time. Due to the influence of the traditional concept, both patients in the two groups were able to obtain good life care and psychological comfort provided by their family members. However, the scores in the surgical group were slightly higher: due to the postoperative pain reduction and functional reconstruction in the surgical group, patients were given a certain amount of limb function, thus acquiring part of the ability to take care of themselves, which appropriately reduced the guilt of the patient due to increased family burden.
The purpose of limb preserving surgery is to resect the tumor, relieve pain, and preserve the affected limb function as much as possible. The relief of pain can improve ratings for specific items in the physical function field such as “I have pain” and “I feel ill”. Due to functional reconstruction, the functional ratings such as “I am able to work“ and “I am sleeping well” were improved. Therefore, a sharp rise in the physical score and the functional score was observed in the surgical group. In contrast, an acute reduction was noticed in the two fields due to the uncontrollable pain and deteriorating limb function in the non-surgical patients.
Although there are some advantages in functional scoring, this type of operation does not achieve the ideal shoulder function, which is in line with what Cannon et al16 indicated in their study. Most scholars believe that even with reconstruction after resection of proximal humerus tumor segment, shoulder function will be damaged to a certain extent.17 In our study, only a few (30%) patients who underwent active rehabilitation could reach 90 degrees of abduction. Even with optimal preservation of the deltoid and axillary nerves in type I resection of the Malawer classification,18 the range of active shoulder abduction can reach a maximum of 40–60 degrees. Although this surgical method does not achieve satisfactory shoulder function, it retains a comforting and painless distal limb function, which has been confirmed by several similar studies.19–22 Woong PJ et al21 reported that the pain was significantly relieved after carrying out joint-preserving palliative surgery for MPH in the advanced cancer patients. A study by Shi G et al22 found that the pain was relieved immediately and substantially after carrying out percutaneous osteoplasty in the humeral head metastases. The integrity of the anatomical structure at the proximal end of the humerus is a prerequisite for the preservation of elbows, forearm, and wrist functions. This is not only an improvement of daily living ability, but also a psychological comfort for patients with advanced cancer. Combined with the nursing support of family members, the satisfaction of patients with self-care ability in basic life can be improved. This will also improve psychological well-being of patients.
Emotional scores gradually increased during the months after operation but showed a downward trend in the last few follow-up points. However, the overall score was above the baseline level. There may be several reasons for this phenomenon: patients can clearly feel pain relief and functional recovery one or more months after surgery, resulting in an increase in such scores as “I am satisfied with how I am coping with my illness”. However, the continued deterioration of the condition of the primary tumor will have an adverse effect on such type of emotional score as “I worry about dying” and “I worry that my condition will get worse”. Therefore, more active and effective treatment of the primary tumor is an effective way to improve the situation. In the non-operative group, although there was a slight fluctuation in the emotional score, there was no obvious change over time. This may be caused by uncertainty about the effect of non-surgical treatment. In the first period of chemotherapy, the therapeutic effect can improve the patient’s confidence in treatment and thus improve the emotional score. However, drug resistance and chemotherapy side effects can have a negative impact on the patient’s mood and thus result in a lower emotional score.
From the economical perspective, because of China’s large population, insufficient financial investment, and unreasonable allocation of medical resources, patients have to pay high medical costs to treat disease such as malignant tumors. Meanwhile, the imbalance of input and return is a status of the treatment of malignant tumors. Fortunately, bone cement spacer is a cheap and effective method to treat MPH. In the current economic environment, this is a hope for families of advanced cancer patients who are already under great economic pressure. We did not observe any case of deep infection in our study because we used antibiotic cement in order to achieve a high concentration of local antibiotic.
This study has some limitations which should be noted. First, there are multiple other functional reconstruction methods for limb salvage. This study was confined to the use of bone cement spacer because of medical and economical limitations. Second, the number of patients was small, and large sample volumes and multi-center studies are needed in the future. Third, follow-up time was relatively short, which may influence the results of the survival analysis to a certain extent. Fourth, this analysis is based on China’s medical security system. Whether it is applicable in the environment of other countries has yet to be studied.
Conclusion
The results of this study show that the use of bone cement spacers for functional shoulder reconstruction improved the QOL of advanced cancer patients with MPH. This surgery method has the advantages of a low cost, simple operation and adequate analgesic effect after operation. Although it is not perfect in improving shoulder function, it preserves a painless and comforting distal limb function. At the same time, it is a reasonable solution for patients with poor economic conditions.
Abbreviations
QOL, quality of life; MPH, metastasis of the proximal humerus; FACT-G, The Functional Assessment of Cancer Therapy-General (FACT-G) questionnaire; VAS, visual analog scale; MSTS, Musculoskeletal Tumor Society scores; ECOG, Eastern Cooperative Oncology Group; PS, performance status.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rafalla AA, ESA A. Endoprosthetic replacement versus cement spacer in reconstruction of proximal humerus after tumor resection: cost and benefits. J Orthop Surg (Hong Kong). 2017;25(2):2309499017713937. doi:10.1177/2309499017713937
2. Sirveaux F. Reconstruction techniques after proximal humerus tumour resection. Orthop Traumatol Surg Res. 2019;105(1):S153–S164. doi:10.1016/j.otsr.2018.04.024
3. Clara-Altamirano MA, Garcia-Ortega DY, Martinez-Said H, Caro-Sánchez CHS, Herrera-Gomez A, Cuellar-Hubbe M. Surgical treatment in bone metastases in the appendicular skeleton. Rev Esp Cir Ortop Traumatol. 2018;62(3):185–189. doi:10.1016/j.recot.2017.12.001
4. Kundu ZS, Gogna P, Gupta V, Kamboj P, Singla R, Sangwan SS. Proximal humeral reconstruction using nail cement spacer in primary and metastatic tumours of proximal humerus. Strategies Trauma Limb Reconstr. 2013;8(3):149–154. doi:10.1007/s11751-013-0172-9
5. Lipscomb J, Gotay CC, Snyder CF. Patient-reported outcomes in cancer: a review of recent research and policy initiatives. CA Cancer J Clin. 2007;57(5):278–300. doi:10.3322/CA.57.5.278
6. Tang Y, Qu J, Wu J, et al. Effect of surgery on QOL of patients with spinal metastasis from non-small-cell lung cancer. J Bone Joint Surg Am. 2016;98(5):396–402. doi:10.2106/JBJS.O.00629
7. Holzner B, Kemmler G, Kopp M, et al. QOL in breast cancer patients – not enough attention for long-term survivors. Psychosomatics. 2001;42(2):117–123. doi:10.1176/appi.psy.42.2.117
8. Mols F, van de Poll-Franse LV, Vingerhoets AJ, et al. Long-term QOL among Dutch prostate cancer survivors: results of a population-based study. Cancer. 2006;107(9):2186–2196. doi:10.1002/cncr.22231
9. Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res. 1989;249:256–264.
10. Katagiri H, Okada R, Takagi T, et al. New prognostic factors and scoring system for patients with skeletal metastasis. Cancer Med. 2014;3(5):1359–1367. doi:10.1002/cam4.292
11. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–655.
12. Kong P, Yan J, Liu D, et al. Skeletal-related events and overall survival of patients with bone metastasis from nonsmall cell lung cancer – a retrospective analysis. Medicine (Baltimore). 2017;96(51):e9327. doi:10.1097/MD.0000000000009327
13. Huschka MM, Mandrekar SJ, Schaefer PL, Jett JR, Sloan JA. A pooled analysis of QOL measures and adverse events data in north central cancer treatment group lung cancer clinical trials. Cancer. 2007;109(4):787–795. doi:10.1002/cncr.22444
14. Cella D, Ivanescu C, Holmstrom S, Bui CN, Spalding J, Fizazi K. Impact of enzalutamide on QOL in men with metastatic castration-resistant prostate cancer after chemotherapy: additional analyses from the AFFIRM randomized clinical trial. Ann Oncol. 2015;26(1):179–185. doi:10.1093/annonc/mdu510
15. He L, Tang S, Yu W, Xu W, Xie Q, Wang J. The prevalence, comorbidity and risks of prolonged grief disorder among bereaved Chinese adults. Psychiatry Res. 2014;219(2):347–352. doi:10.1016/j.psychres.2014.05.022
16. Cannon CP, Paraliticci GU, Lin PP, Lewis VO, Yasko AW. Functional outcome following endoprosthetic reconstruction of the proximal humerus. J Shoulder Elbow Surg. 2009;18(5):705–710. doi:10.1016/j.jse.2008.10.011
17. Rödl RW, Gosheger G, Gebert C, Lindner N, Ozaki T, Winkelmann W. Reconstruction of the proximal humerus after wide resection of tumours. J Bone Joint Surg Br. 2002;84(7):1004–1008. doi:10.1302/0301-620x.84b7.12989
18. Malawer MM, Meller I, Dunham WK. A new surgical classification system for shoulder-girdle resections. Analysis of 38 patients. Clin Orthop Relat Res. 1991;267:33–44.
19. Yang Q, Li J, Yang Z, Li X, Li Z. Limb sparing surgery for bone tumours of the shoulder girdle: the oncological and functional results. Int Orthop. 2010;34(6):869–875. doi:10.1007/s00264-009-0857-3
20. Casadei R, Drago G, Di Pressa F, Donati D. Humeral metastasis of renal cancer: surgical options and review of literature. Revue de Chirurgie Orthopedique et Traumatologique. 2018;104(4):380. doi:10.1016/j.otsr.2018.03.009
21. Woong PJ, Yong-Il K, Guy KH. Joint-preserving palliative surgery using self-locking screws of intramedullary nail and percutaneous cementoplasty for proximal humeral metastasis in the advanced cancer patients. World J Surg Oncol. 2018;16(1):1–8. doi:10.1186/s12957-018-1397-3
22. Shi G, Liu Q, Chen H, et al. Percutaneous osteoplasty for the management of a humeral head metastasis: two case reports. Medicine (Baltimore). 2019;98(20):e15727. doi:10.1097/MD.0000000000015727
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
