Back to Journals » International Journal of General Medicine » Volume 9
Quality-of-life indicators and falls due to vitamin D deficiency
Authors Cheema MR , Chaudhry A
Received 24 October 2014
Accepted for publication 13 January 2015
Published 22 February 2016 Volume 2016:9 Pages 21—25
DOI https://doi.org/10.2147/IJGM.S76360
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Muhammad Raza Cheema, Ahmad Yar Chaudhry
Department of Geriatrics, University Hospitals Coventry and Warwickshire, NHS Hospitals, Coventry, UK
Objective: To determine whether the number of falls and quality-of-life indicators relate to serum levels of vitamin D, parathyroid hormone (PTH), and calcium levels.
Design: A prospective study.
Participants: Patients being admitted with a fall with or without sustaining a fragility fracture post fall.
Measurements: Measured frequency of falling, SF-12 questionnaire, serum concentrations of 25-hydroxyvitamin D, calcium, and PTH levels before and after treatment with vitamin D supplementation.
Results: The mean age (N=38) of the cohort was 80.2±12. In all, 76.3% of the cohort had sustained a fragility fracture after the fall. The cohort was vitamin D deficient with the pretreatment mean value of 24.2±17 nmol/L and posttreatment mean value of 99±40 nmol/L with a statistically significant mean difference of 74.7 nmol/L (confidence interval [CI] 61.27–88.3), P=0.001. The levels of calcium and PTH were statistically significant after treatment with a mean difference of 0.16 (CI 0.1–0.2), P=0.001, and 3.7 (CI –4.8 to –2.5), P=0.001, respectively. After treatment, the mean difference of physical component score (PCS) and mental component score for the whole cohort was 2.9 (CI –0.69 to 6.6), P=0.10, and 1.05 (CI –2.6 to 4.7), P=0.56, respectively. However, a subgroup analysis for cohort aged ≤70 years provided a statistically significant effect on PCS with a mean difference of 8.9 (CI 1.3–16.4), P=0.03, but a statistically insignificant improvement in mental component score with a mean difference of 6.0 (CI –17 to –5.0), P=0.20. However, a statistically significant improvement in PCS SF-12 was observed in patients ≤70 years of age 2.9 (1.3–16.4), P=0.03. The mean number of falls for the whole cohort pre- and posttreatment was 1.11±0.92 vs 0.97±0.99 (P=0.68), respectively.
Conclusion: Patients who had fallen and sustained fragility fracture had lower serum 25-dihydroxyvitamin D and higher serum PTH levels. Our study demonstrates that there is no statistically significant improvement in the number of falls after treatment with vitamin D. Overall, vitamin D levels improved significantly, this is despite quality-of-life indicators showing a mean increase in PCS but not a statistically significant improvement. However, statistically significant improvement in PCS was observed in group aged ≤70 years after vitamin D supplementation.
Keywords: vitamin D, calcium, SF-12 questionnaire, parathyroid hormone
Introduction
Falls in the elderly population remains one of the most common presentations in emergency departments and is a common cause for admissions in UK hospitals.1 There is a minimum of one fall per year in 30% and 50% of population older than 65 years and 80 years, respectively. In the National Health Service UK, the cost of admissions associated with falls mounts to >£2.3 billion every year.1 With progressively increasing geriatric population, it has been projected that in the USA, annual cost from all fall-related injuries in persons older than the age of 65 will increase to $32.4 billion in 2020.2 Falls are a substantial cause of fractures and result in significant morbidity and mortality in the elderly population, and consequently, increases the risks of fractures.2 The etiology of falls in elderly population is often multifactorial and warrants a multidisciplinary approach for management and prevention to treat the consequences and prevent falls.
Vitamin D is known to exert a wide range of effects in our bodies, including those relating to musculoskeletal development and sustenance. Studies have shown that most tissues in our body contain receptors for 1,25-dihydroxyvitamin D.3 For example, receptors are present in muscle tissues and bones, hence, explaining the myopathy, muscle weakness, and muscle pains associated with vitamin D deficiency.3 Having low levels of vitamin D also decreases the bone mineral density and the strength of the bones, hence, increasing the chances of instability on mobility and increasing the chances of falls.3
Vitamin D deficiency is common in elderly population due to various risk factors, including decreased dietary intake, diminished sunlight exposure, reduced skin thickness, impaired intestinal absorption, and impaired hydroxylation in the liver and kidneys.4 Vitamin D supplementation is a fairly easy and cost-effective intervention that may result in or potentiate positive outcomes, regarding fall prevention.
Previous literature indicates that low levels of vitamin D in elderly population have been associated with increased risks of falls and reduction in muscle strength and muscle mass. These have resulted in the widespread and popular concept that vitamin D supplementation may be helpful in preventing fall. The results of trials and meta-analyses that have investigated the relationship between vitamin D and falls have been varied. It still remains unclear how vitamin D supplements might prevent falls.
Considering the importance of controlling and preventing this growing epidemic of falls in elderly population, we performed a prospective 3-month follow-up study on patients who were admitted with falls to assess the impact on quality of life and its relationship to vitamin D levels.
Materials and methods
Ethical approval was given from the University Hospitals Coventry and Warwickshire, UK local ethical committee. After verbal informed consent, 38 consecutive patients being admitted with falls were assessed on parameters of serum levels of 25-hydroxyvitamin D, calcium, parathyroid hormone (PTH), number of falls, and number of fragility fractures (new or previous). They completed SF-12 questionnaire for assessment of quality of life. Hypovitaminosis D was defined as plasma serum concentration of 25-hydroxyvitamin D of <25 nmol/L (10 ng/mL) as per Department of Health Recommendation.5 Patients suffering from hypovitaminosis D were identified and were administered appropriate treatment. As per hospital protocol, patients were administered 60,000 IU of cholecalciferol weekly for 8 weeks followed by maintenance regimen of 400 IU of vitamin D3 and 600 mg elemental calcium.
All 38 patients were found to have a low vitamin D level. These patients were then followed up in “Falls Clinic” for >3 months post-fall. Repeat serum concentrations of 25-hydroxyvitamin D, calcium, and PTH were performed at that stage and were reassessed using SF-12 health questionnaires to assess the impact of vitamin D supplementation on their quality of life and frequency of falls 3 months posttreatment.
SF-12 questionnaire is a validated questionnaire used globally to assess the impacts on physical and mental health. Separate scores are obtained for physical component score (PCS) and mental component score (MCS). We chose this questionnaire to ascertain whether vitamin D supplementation can affect physical and/or mental quality of life. Pre- and posttreatment serum concentration of vitamin D, calcium, and PTH and SF-12 questionnaire values (PCS and MCS) were compared using paired Student’s t-test, confidence intervals (CIs), and P-values. Student’s t-test was used to test for significant differences in the results before and after treatment with vitamin D.
Results
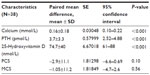
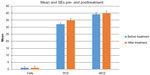
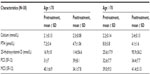
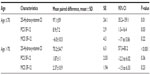
The mean age (N=38) of the cohort was 80.2±12. The mean age of the subjects older than 70 years (n=32) was 84 (SD=7.4) and the mean age of the subjects younger than 70 years (n=6) was 58±9. In all, 76.3% of the cohort had sustained a fragility fracture after the fall and 23.6% sustained a fall but did not have any fractures. Characteristic baseline demographics of the cohort are shown in Table 1. The cohort was 25-hydroxyvitamin D deficient with pretreatment mean value of 24.2±17 nmol/L and posttreatment mean value of 99±40 nmol/L with a statistically significant mean difference of 74.7 nmol/L (CI 61.27–88.3), P=0.001 (Table 2). The levels of calcium and PTH were statistically significant after treatment with a mean difference of 0.16 mmol/L (CI 0.1–0.2), P=0.001 and 3.7 pmol/L (CI −4.8 to −2.5), P=0.001, respectively. The mean difference of PCS and MCS for the whole cohort after treatment was 2.9 (CI −0.69 to 6.6), P=0.10, and 1.05 (CI −2.6 to 4.7), P=0.56, respectively (Table 3 and Figure 1). However, a subgroup analysis for cohort aged ≤70 years provided a statistically significant effect on PCS with a mean difference of ±SD of 8.9±7.2 (95% CI 1.3–16.4), P=0.03, but a statistically insignificant improvement in MCS with a mean difference ±SD of –6.0 ±10.5 (95%CI–17–5.06), P=0.20 (Table 5).
  | Table 1 The baseline characteristics of the cohort including medical comorbidities in the cohort |
The mean ± SD pre- and posttreatment for calcium was 2.23mmol/L ±–0.14 and 2.4 mmol/L ± 0.12, 25-hydroxyvitamin D 24.2 nmol/L ±17 and 99nmol/L ±–40, PTH 7.9 pmol/L± 3.7 and 4.2 ± 0.12, PCS 32.3 ± 7.5 and 35 ± 7.9 and MCS 39.2 ± 8.9 and 40 ± 6.5, respectively.
The number of falls for the whole cohort pre- and posttreatment with a mean of 1.11±0.92 vs 0.97±0.99 (P=0.68) did not improve, despite a clinical increase in the mean value of PCS for the whole cohort (32.3±7.5 vs 35±7.9) but was statistically insignificant P=0.10. The number of nonfallers increased from 31.5% to 42% after 3 months of treatment.
Discussion
Falls constitute a significant number of admissions in the UK hospitals. Functional decline with age is often followed by gait instability and falls, which can often result in significant morbidity. Adjunct medical comorbidities that can independently contribute to increase in falls also increase with age.6 This relationship of falls to worsening health status has led to numerous studies to find the “perfect cure” for this dilemma. The present study adds to a growing body of literature, in search for treatable causes and to help reduce the burden of falling, especially in the elderly population.
One of the first randomized controlled trials looking at the effects of vitamin D and calcium supplements on falls showed that the number of falls reduced by 49% per person, improved musculoskeletal function within 3 months of treatment.7 In our study, the number of nonfallers increased by 10.5% but we did not see a significant difference in the number of fallers after treatment, which might be caused by lack of a large sample size. The study revealed an increase in physical state of patients, especially in the cohort aged 70 years or younger; however, the authors acknowledge that the sample size is not completely reflective of the general population. Cohort aged 70 years or younger had multiple comorbidities and gait instability well before admission to hospital.
A more recent systematic review and meta-analysis found that vitamin D use was associated with statistically significant reduction in the risk of falls odds ratio 0.86 (95% CI 0.77–0.96).8 These studies have shown robust evidence in successful decline in the number of falls with vitamin D supplementations. However, recent evidence has been contradictory. Recent meta-analysis, which incorporated data from 29,535 people, demonstrated that vitamin D with or without calcium supplements does not reduce falls by 15% or more.9
However, previously a meta-analysis looking at the effect of vitamin D on falls in ambulatory and institutionalized older individuals showed that vitamin D reduced the corrected odds ratio by 22% and number needed to treat was 15 (95% CI 8–53). This would mean 15 patients would need to be treated with vitamin D to prevent one person from falling.10 Interestingly, a meta-analysis looking at five randomized controlled trials in prophylactic use of vitamin D in older people showed a decrease in the number of falls in group receiving prophylactic vitamin D with needed to treat =15 (95% CI 9–52).11
In the present study, there is little evidence for a reduction in the number of falls with vitamin D supplementation, although an increase in PCS has been seen throughout the cohort but significant increase was observed in cohort aged ≤70 years. This may perhaps be contributed to the younger age population having more physical reserve than people aged >70 years and even slight improvements in muscle power/activity would be beneficial enough to improve their quality of life. In the current study, the authors recognize the lack of large sample size that could contribute to lack of identification of significant differences before and after treatment. Further studies would be required to look at more direct physical measurements, such as bone mineral density, lean body mass, and bone resorption markers.
Most of the studies in literature comprise relatively older population, including mostly institutionalized individuals or individuals with significant mobility-limiting comorbidities, therefore, the influence of vitamin D supplementation may be confounded or be minimally conspicuous. This emphasizes a need for further studies specifically targeted to examine the effects of muscle changes and quality-of-life indicators, particularly in individuals aged between 50 years and 70 years.
Our study indicates the following:
- There is minimal effect of vitamin D supplementation with regard to fall prevention, despite a mean increase in vitamin D levels post supplementation.
- In spite of this, vitamin D supplementation has shown a beneficial effect on PCS.
- Younger patients responded better to vitamin D supplementation with a significant rise in PCS, indicating a better physical outcome.
Despite the vast amount of work that has been conducted in this direction, there are still some points of ambiguity, which warrant further research. A few of these are as follows:
- Is there a significant beneficial effect of vitamin D supplementation in fall prevention? If so, what is the target population and preferred age for onset of supplementation?
- Would it be beneficial to institute vitamin D supplementation at an earlier age when it may help to sustain a relatively better physical condition vs at a later age when there is preexisting musculoskeletal degeneration age related or otherwise?
- Does the recommended dose of vitamin D supplementation need to be revisited?
- Are there any factors that may have confounded the effect of vitamin D supplementation in studies focusing on the elderly/institutionalized population?
Conclusion
Our study shows that the exogenous supplementation of vitamin D increases the vitamin D levels and improves the physical quality of life in the younger sect of the cohort (aged ≤70), although did not show a significant difference in the number of falls. The older population of the cohort showed a moderate mean increase in PCS (however, statistically insignificant) but no significant difference in the number of falls. This generates an interesting hypothesis whether vitamin D supplementation may be more beneficial for patients aged ≤70 years; however, further robust and prospective data will be required to test this hypothesis.
Acknowledgment
This article has been presented as a poster presentation at the Annual Conference of Royal College of General Practitioners, 2013. No financial support was undertaken by any external/internal units.
Disclosure
The authors report no conflicts of interest in this work.
References
NICE [webpage on the Internet]. Falls: Assessment and Prevention of Falls in Older People. NICE Guidelines. 2013. Available from: http://www.nice.org.uk/guidance/CG161/chapter/Introduction. Accessed December 29, 2015. | |
Englander F, Hodson TJ, Terregrossa RA. Economic dimensions of slip and fall injuries. J Forensic Sci. 1996;41:733–746. | |
Perez-Lopez FR. Vitamin D and its implications for musculo-skeletal health in women: an update. Maturitas. 2007;58:117–137. | |
Hollick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–1930. | |
Department of Health (DoH). Dietary Reference Values for food energy and nutrients for the United Kingdom. Report on Health and Social Subjects No 41. London: Her Majesty’s Stationery Office. 1991. | |
Autier P, Gandini S. Vitamin D supplementation and total mortality. A meta-analysis of randomized controlled trials. Arch Intern Med. 2007;176(16):1730–1737. | |
Bischoff HA, Stahelin HB, Dick W, et al. Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Res. 2003;18(2):343–351. | |
Murad MH, Elamin KB, Abu Elnour NO, et al. The effect of vitamin D on falls: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2011;96(10):2997–3006. | |
Bolland MJ, Grey A, Gamble GD, Reid IR. Vitamin D supplementation and falls: a trial sequential meta-analysis. Lancet Diabetes Endocrinol. 2014;2(7):573–580. | |
Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-anlysis. JAMA. 2004;291(16):1999–2006. | |
Monaghan H. Review: prophylactic use of vitamin D reduces falls in older people. Evid Based Nurs. 2004;7(4):119. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.