Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Quality of Life Differences in Pre- and Post-Educational Treatment in Type 1 Diabetes Mellitus During COVID-19
Authors Rochmah N , Faizi M, Hisbiyah Y , Triastuti IW, Wicaksono G, Endaryanto A, Soetjipto
Received 30 March 2021
Accepted for publication 10 June 2021
Published 28 June 2021 Volume 2021:14 Pages 2905—2911
DOI https://doi.org/10.2147/DMSO.S313575
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ming-Hui Zou
Nur Rochmah,1,2 Muhammad Faizi,1,2 Yuni Hisbiyah,1,2 Ike Wahyu Triastuti,2 Garindra Wicaksono,2 Anang Endaryanto,1,2 Soetjipto1,3
1Doctoral Program of Medical Science, Faculty of Medicine, Universitas Airlangga, Surabaya, East Java, Indonesia; 2Department of Child Health, Dr. Soetomo General Hospital, Faculty of Medicine, Universitas Airlangga, Surabaya, East Java, Indonesia; 3Department of Biochemistry, Faculty of Medicine, Universitas Airlangga, Surabaya, East Java, Indonesia
Correspondence: Nur Rochmah
Department of Child Health, Dr. Soetomo General Hospital, Faculty of Medicine, Universitas Airlangga, Jl. Mayjend Prof. Dr. Moestopo No. 6-8, Airlangga, Gubeng, Surabaya, East Java, 60286, Indonesia
Tel +62 81703501118
Email [email protected]
Purpose: The coronavirus-19 (COVID-19) pandemic requires the use of online media to ensure monitoring of type 1 diabetes mellitus (T1DM) in children. Thus, this study aims to determine whether online education effectively improves the quality of life (QoL) in children with T1DM during the coronavirus-19 pandemic.
Patients and Methods: The study, conducted from March to October 2020, utilized the paired t-test before and after online education. Moreover, it adopts the recommended Pediatric Quality of Life Inventory (PedsQL) 3.2 diabetes module for the 33 patients registered in the Pediatric Endocrine Outpatient Clinic of Dr. Soetomo Hospital, Surabaya, Indonesia.
Results: The QoL of all children (p = 0.011), parents (p = 0.001), and both children and parents (overall; p = 0.002) have shown significant improvement after the treatment. The QoL of parents, as a subcriterion, improved after the treatment. However, the improvement in the children in subcriterion treatment II (p = 0.186) was not significant.
Conclusion: Online education has proven to create a better QoL almost in all children with T1DM during the coronavirus-19 pandemic.
Keywords: T1DM, COVID-19, children, online education, PedsQL
Introduction
The coronavirus-19 (COVID-19) pandemic was declared by the World Health Organization (WHO) Emergency Committee as a global health emergency.1 This pandemic has inadvertently impacted health systems in that the primary health services have given up for a long time. It has also influenced health, physical, psychological, and socioeconomic sectors in many countries.2–6 Especially for the psychological aspect, COVID-19 pandemic on pediatric patients with chronic diseases, particularly type 1 diabetes, are more vulnerable and at higher risk for developing dangerous feelings, such as uncertainties, distraction, irritability, and fear. Also, They are at risk of acute stress disorder, adjustment disorder, and grief.7 Thus, quality of life (QoL) will be impaired.3 Moreover, the American Diabetes Association recommends that patients with type 1 diabetes mellitus (T1DM) and their families be given comprehensive education and support.8
T1DM is the most common chronic disease, with approximately 70,000 children diagnosed worldwide each year. It has an incidence rate of <1 case/year/100 individuals in the Asian population, which is relatively lower than in the Caucasian population.9 A rise of approximately 40% (70 children) in new T1DM visits was recorded in Indonesia from 2002 to 2014 according to the data from Dr. Soetomo General Hospital, Surabaya.10 On one hand, the China Center for Disease Control reported 2143 infections <18 years old as of August 2020.11 On the other hand, a report from the COVID-19 task force in Indonesia shows that the infection rate in children is 11.4%, with 3.2% mortality. This mortality rate is relatively the highest compared to other countries, including America, Italy, and Korea.12
Many patients have impaired glucose control during the pandemic period.13 Consequently, children with T1DM are vulnerable to COVID-19 infection.14 However, studies have shown that education is the key to successful diabetes management.15 Thus, the healthcare system needs to explain the condition of this pandemic, management for prevention, and the importance of continuing diabetes treatment during the pandemic. The effect of lockdown in some countries restricts individual movement. Therefore, daily activities are affected, which can influence the QoL in some aspects.16 Several components in the Pediatric Quality of Life Inventory (PedsQL), such as diabetes symptoms, treatment barrier, treatment adherence, worry, and communication, are at risk of worsening during the pandemic.17 Therefore, several studies have stated that pandemic conditions can cause a decrease in QoL in T1DM patients, especially children and adolescents.13,18
It has been previously reported that online education can promote relationship quality and knowledge improvement.17,19 Especially in pandemic conditions, it could lead to lack of doctor and patient contact which results in a reduction of parent’s motivation to care their child’s condition which results in a further decrease in QoL.20 Consequently, this study aims to determine whether online education is effective in improving QoL in children with T1DM during the COVID-19 pandemic.
Patients and Methods
Sample
This study involved children and adolescents, as well as their parents, diagnosed with T1DM according to the International Society for Pediatric and Adolescent Diabetes guidelines. The patients were registered at the Pediatric Endocrinology Outpatient Clinic of Dr. Soetomo Hospital, Surabaya, Indonesia. The inclusion criteria for this study were age (5–18 years), diagnosed with T1DM, registered at the Pediatric Endocrinology Outpatient Clinic of Dr. Soetomo Hospital, treatment status (already started treatment), and hospital visits (visited the hospital with parents). The sample was randomly obtained after we share the information in mobile application. Those who willing to join our interactive session were our sample population. Consequently, 33 patients (18 boys and 15 girls) were included in this study.
Community Treatment
Treatment activities were in the form of knowledge sharing through online education with the preparation of educational manuals and videos using Zoom web conference. In addition, parents were given learning materials such as educational videos and powerpoint presentations about the guide and treatment of T1DM during the COVID-19 pandemic. Online education was about the COVID-19 infection, the importance of continuing proper diabetes treatment during the pandemic, and the equipment for personal prevention. The online meeting began with explaining the T1DM child care method at home and advice to be applied at home, presented by a pediatric diabetes specialist. Followed by a one by one sharing session of experiences from each participant regarding the process of nursing for the children during the COVID-19 pandemic period. After sharing the experience, a pediatric diabetes specialist reviewed whether the actions taken by each family and motivated the family. This meeting session is conducted only once in about 120 minutes. Post-test evaluation applied after education is done. Post-intervention QoL data were obtained two months intervals. Then, we collect some feedback on satisfaction with participants by personal chat on a mobile application. All participants were satisfied with the sharing session because they can share their problems and find solutions in the sharing session.
Data Collection
This study used a cross-sectional design and was performed from March to October 2020. Retrospective data were taken from medical records, and the subjects were interviewed to collect data based on PedsQL. Before the interview, the subject’s consents were obtained. This process was carried out during their visit to the Pediatric Endocrine Outpatient Clinic of Dr. Soetomo Hospital, Surabaya, Indonesia.
The Personal Characteristic Form
The children’s form consisted of demographics (eg, gender, weight, age, and illness-related topics such as diabetes duration, age at diagnosis, and glycated hemoglobin levels). The parent’s form consists of questions about marital status, educational background, and family income.
Nutritional Status
Nutritional status was classified according to the World Health Organization (WHO), Body Mass Index (BMI) for age values defined for children and adolescents (5–18 years old): severe malnutrition (z < −3), moderate malnutrition (−3 < z < −2), normal (−2 < z ≤ 1), overweight (1 < z < 2), and obese (z > 2).17 The subjects were grouped into four groups (severe malnutrition, moderate malnutrition, normal, and overweight/obese).
Educational Background
The educational background was classified based on the government program of 9-year compulsory education; hence, the governmental program of our country divided it into three groups: <9 years, 9–12 years, and >12 years.
Socioeconomic Status
The socioeconomic status was defined based on the world bank scale of Indonesia, which is middle-low and regional minimum wage from the government of each city. We divided into three groups based on the regional minimum wage: low, medium, and high.
Pediatric Quality of Life Inventory
The patient’s QoL was assessed using the PedsQL 3.2 diabetes module by Varni et al for children based on the patient’s age.21 The PedsQL questionnaire has been translated by a credible sworn translator into Bahasa Indonesia that used to assess the quality of life of the children with T1DM. It assessed the aspects of diabetes (15 items; diabetes symptoms), treatment barriers (evaluated the obstacles or problems during treatment; treatment I, 5 items), treatment adherence (treatment II, six items), worry (3 items), and communication (4 items) with reverse-scored items. Five- and three-point scales exist for the Child Report for Young Children (5–7 years old). In the 5-point scale, 0, 1, 2, 4, and 4 never represented, almost never, sometimes, often, and almost always, respectively. However, in the 3-point scale, 0, 2, and 4 represented not at all, sometimes, and a lot, respectively. These scores were transformed to a 0–100 scale, where 0 = 100, 1 = 75, 2 = 50, and 4 = 0. Lower scores demonstrate more diabetes symptoms and management problems. This PedsQL has tested its validity and reliability by showing good results in the study by Varni et al.22 In addition, validity is assessed by predicting the morbidity and disease burden of the patients and their parents. Consequently, reliability is when results were consistent after several tests.21 Moreover, the validity and reliability of the PedsQL questionnaire have been tested by Statistics of Universitas Airlangga and it has been reported to be valid. The questionnaire was shared online with the participants by the same team during the study.
Data Evaluation
The SPSS 17.0 software (IBM SPSS; Armonk, NY, USA) was used to analyze data. The mean and standard deviation of each element were used to obtain the baseline and clinical characteristics data. The normality test was done using the Shapiro–Wilk test because the subject was <50. The data were normally distributed so that we continued to the paired t-test based on the statistic journal from Kim K. T., 2015.23 Moreover, we have already consult to the statistician of Universitas Airlangga, the paired t-test was used to test the comparison test. P < 0.05 was considered statistically significant.
Results
This cross-sectional study included 33 children with T1DM (18 boys and 15 girls; 11.97 ± 2.91 years old). The baseline characteristics and history of the patients with T1DM are presented in Table 1. The average diabetes duration was 3.33 years, compared to the Asian demographic average was 5.48 years. The average age at diagnosis in our study was 67.75 months or 5.64 years old, similar to a study of Asian children population from Khanolkar et al 2016,24 stated that the average age at diagnosis was 6.60 years old. The average HbA1c in our study was 10.06%, while the average in Asian children population was 9.1%, based on Khanolkar et al 2016. The participant’s socioeconomic status was majority low, as well as a study of Khanolkar et al 2016 in Asia population.
 |
Table 1 Baseline Characteristics of Patients with T1DM |
The scores of the parents were in line with the scores of the children. On the one hand, the mean QoL scores for parents before and after online education were 75.29 and 76.51, respectively. On the other hand, the mean QoL scores for children before and after online education were 75.66 and 76.80, respectively. These results showed that linearity exists between the scores of the parents and children. The results of the treatment effect on the QoL of the subjects showed a significant PedsQL score before and after an online video conference (p = 0.002), and the mean difference was as high as 1.21 of the PedsQL score. Moreover, the most significant impact was observed in the scores of the parents (p = 0.001) and children (p = 0.011), with a difference of 1.22 and 1.14 of the PedsQL scores, respectively.
The improvement in the scores of the parents (1.22) was more significant than the increase in the scores of the children (1.14). However, a significant increase in PedsQL score was shown overall. The PedsQL subcriteria are presented in Table 2. An increased result was found in all criteria except for treatment adherence for children (p = 0.186). Meanwhile, diabetes, treatment barrier, worry, and communication criteria significantly improved after the treatment (p < 0.05).
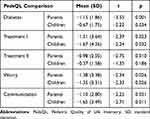 |
Table 2 Comparison of PedsQL Scores Before and After Online Education for Each Subcriteria |
Discussion
This study found that online education is effective in improving the QoL in children with T1DM during the COVID-19 pandemic. The average of parents, and children’s scores were increased. An increased mean score QoL before and after intervention showed that online education was clinically meaningful and improved QoL among the parents and children with T1DM. It is clinically meaningful because the parents feel satisfied with this interactive session and their worry reduced (worry aspect), for the treatment barrier aspect, their parents more courageous to control with the doctor in hospital, for the diabetes symptoms, complaints from patients are also reduced due to their routine control, for the adherence treatment, each patient has a glucose report book before and after meals, so parents are more obedient to the insulin dosage and insulin schedule, for the communication aspect, parents and children build more communication at home, their parents told us when they came to clinic to control. This study is consistent with a study from Dudley et al 2014 which stated that the way the health care team works together and implements technology and education dramatically affects the client’s success. In that study, participants completed an initial semi-structured interview.25 Another study from Algahtani et al 2021 stated that Community-based interventions are needed to mitigate the pandemic’s negative effects and enhance the health and QoL of the general population. The online survey was the most feasible way to access the target population in light of the social-distance protocols implemented during the COVID-19 pandemic.26 A significant improvement in each of the subcriteria was also found except for the treatment adherence criterion in children. This could be due to the child’s lower ability to understand speech and writing compared to adults. Moreover, children are more likely to be visual and psychomotor learners.27,28 Online education has been studied in a systematic review by Giustini et al.29 This research pointed out that evaluating health promotion through social media is tricky. However, benefits were noted from the existence of psychosocial support and psychological functioning. Online education is also safe during a pandemic.30 The knowledge of T1DM and its management significantly affects metabolic control and patient adherence to medical advice. Children with T1DM are vulnerable to COVID-19 infection. Many patients have impaired glucose control during the pandemic period because of their fear of going to hospital to see the doctor and have a routine control.31 Thus, many researchers want to evaluate the education of patients regarding T1DM.32,33 They conclude that education is needed to control T1DM in children, adolescents, and adults.
Abdul-Rasoul et al stated that patients with T1DM, especially children and adolescents, had lower QoL evaluated by PedsQL.34 Similarly, parents had lower QoL compared with children. This result is consistent with the current study that parents had lower PedsQL scores than children, which may be caused by the parent’s burden to guide and maintain the child and adolescent patients with T1DM. Thus, educating patients with T1DM is essential to maintain patient adherence and its effect on patient QoL.32 However, the study evaluating the efficacy of education to the improvement of the PedsQL score has not yet been conducted. This study found that QoL improvement was significant in all groups (parents and children). Moreover, the best improvement was shown by the treatment barrier score. Treatment barrier was related to patient–parent motivation and acceptance of the disease.20 It is also related to doctor–patient contact, which has been significantly reduced due to social distancing during the COVID-19 pandemic.35 Moreover, online education could be the solution to improve the treatment barrier component of the treatment.
The smallest improvement observed in this study was in treatment adherence score (Table 2). Consistent with the study by Vimalavathini et al, education only improves knowledge and attitude but is not a practical component that composes adherence.32 Treatment adherence is the most difficult to improve because it needs practical demonstration and mirroring from the doctor, which is limited due to the modularity of online education.36
This study found that most patients were in the 8–12 years old group, which is consistent with other studies.28–30 Moreover, the T1DM incidence rate is lower in younger children (5–7 years old).37 Table 1 shows that boys were more prevalent in this study, which is similar to a study by Redondo et al.38 The patient socioeconomic status of this study is similar to the study by Mackey et al.39 In addition, the socioeconomic status correlates with diet, activity, and doctor’s compliance, thus affecting QoL. Another study demonstrated that socioeconomic inequalities, measured as low education and occupational levels, were associated with an increased risk of complication T1D and worsening the disease.40,41
Nevertheless, this study has a limitation. The number of T1DM cases in this study is lower than that in Caucasians although the study was conducted at a referral hospital in East Indonesia. Another limitation, this study is single-center, so that it is also difficult to conduct a controlled trial study for this case. Moreover, the challenge of handling T1DM is quite complicated in Indonesia because of limited resources. Thus, online education, besides maintaining routine control in pediatric endocrine outpatient clinics, will improve treatment. Consequently, QoL will also be improved. Moreover, no studies exist about online education during the COVID-19 pandemic. It is believed that this is the first online education that determines the differences between QoL in patients with T1DM before and after online education.
Conclusion
Online education during the COVID-19 pandemic has a good impact on promoting the QoL of patients with T1DM with the increment of PedsQL observed in parents and children. Although a face-to-face conference is limited due to the risk of COVID-19 transmission, the online video conference could substitute for education in some parts. Nevertheless, meeting sessions (eg, workshops or demonstrations) are essential for health promotion which cannot be substituted.
Data Sharing Statement
All subject data in our study are available upon request.
Ethical Approval
This study’s ethical approval was granted by the ethics committee overseeing health research at Dr. Soetomo Hospital, Surabaya, Indonesia (Ref. No. 0123/LOE/301.4.2/IX/2020). All participants and their parents provided informed consent, and this study was conducted in accordance with the Declaration of Helsinki.
Informed Consent
Participants have received an explanation regarding the following research. The patient’s personal data will be kept confidential. Participants who were willing to take part in the research filled out and send back the consent form via email. A parent of participant that consented will be interviewed with questionnaire based on PedsQL regarding the age.
Acknowledgments
The authors wish to thank the patients and their caregivers who participated in the study. We also acknowledge the support of the endocrine team of Dr. Soetomo Hospital, Surabaya, Indonesia.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors received no financial support for the research.
Disclosure
The authors declare that no conflicts of interest in this work.
References
1. Velavan TP, Meyer CG. The COVID-19 epidemic. Trop Med Int Heal. 2020;25(3):278–280. doi:10.1111/tmi.13383
2. Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):300–302. doi:10.1016/S2215-0366(20)30073-0
3. Cui K, Han Z. Association between disaster experience and quality of life: the mediating role of disaster risk perception. Qual Life Res. 2019;28(2):509–513. doi:10.1007/s11136-018-2011-4
4. Dube A, Moffatt M, Davison C, Bartels S. Health outcomes for children in haiti since the 2010 earthquake: a systematic Review. Prehosp Disaster Med. 2018;33(1):77–88. doi:10.1017/S1049023X17007105
5. Shieh V, Huang JJ, Wu TEG, et al. Rate of psychiatric disorders and associations with quality of life among community members following the Kaohsiung gas explosion: an 18-month cross-sectional follow-up study. Health Qual Life Outcomes. 2019;17(1):7. doi:10.1186/s12955-018-1076-7
6. Papanikolaou V, Adamis D, Kyriopoulos J. Long term quality of life after a wildfire disaster in a rural part of Greece. Open J Psychiatr. 2012;02(02):164–170. doi:10.4236/ojpsych.2012.22022
7. Passanisi S, Pecoraro M, Pira F, et al. Quarantine due to the COVID-19 pandemic from the perspective of pediatric patients with type 1 diabetes: a web-based survey. Front Pediatr. 2020;8:491. doi:10.3389/fped.2020.00491
8. Chiang JL, Maahs DM, Garvey KC, et al. Type 1 diabetes in children and adolescents: a position statement by the American Diabetes Association. Diabetes Care. 2018;41(9):2026–2044. doi:10.2337/dci18-0023
9. Park YJ, Yoo SA, Kim WU. Role of endoplasmic reticulum stress in rheumatoid arthritis pathogenesis. J Korean Med Sci. 2014;29(1):2–11. doi:10.3346/jkms.2014.29.1.2
10. RSUD Dr Soetomo. Medical Records Data of outpatient clinic Dr. Soetomo Hospital; n.d.
11. Dong Y, Dong Y, Mo X, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6):e20200702. doi:10.1542/peds.2020-0702
12. Tugas G COVID-19. data sebaran kasus positif; 2020.
13. d’Annunzio G, Maffeis C, Cherubini V, et al. Caring for children and adolescents with type 1 diabetes mellitus: Italian society for pediatric endocrinology and diabetology (ISPED) statements during COVID-19 pandemia. Diabetes Res Clin Pract. 2020;168:168. doi:10.1016/j.diabres.2020.108372
14. Chowdhury S, Goswami S. COVID-19 and type 1 diabetes: dealing with the difficult duo. Int J Diabetes Dev Ctries. 2020;40(3):315–320. doi:10.1007/s13410-020-00846-z
15. Verma A, Rajput R, Verma S, Balania VKB, Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 diabetes mellitus. Diabetes Metab Syndr Clin Res Rev. 2020;14(5):1213–1216. doi:10.1016/j.dsx.2020.07.016
16. Phelan S, Hart C, Phipps M, et al. Maternal behaviors during pregnancy impact offspring obesity risk. Exp Diabetes Res. 2011;2011:1–9. doi:10.1155/2011/985139
17. Tornese G, Ceconi V, Monasta L, Carletti C, Faleschini E, Barbi E. Glycemic control in type 1 diabetes mellitus during COVID-19 quarantine and the role of in-home physical activity. Diabetes Technol Ther. 2020;22(6):462–467. doi:10.1089/dia.2020.0169
18. Tejera- Perez C, Moreno-Pérez Ó, Rios J, Reyes-García R. People living with type 1 diabetes point of view in COVID-19 times (COVIDT1 study): disease impact, health system pitfalls and lessons for the future. Diabetes Res Clin Pract. 2021;171:108547. doi:10.1016/j.diabres.2020.108547
19. Franc S, Borot S, Ronsin O, et al. Telemedicine and type 1 diabetes: is technology per se sufficient to improve glycaemic control? Diabetes Metab. 2014;40(1):61–66. doi:10.1016/j.diabet.2013.09.001
20. Saoji N, Palta M, Young HN, Moreno MA, Rajamanickam V, Cox ED. The relationship of Type 1 diabetes self-management barriers to child and parent quality of life: a US cross-sectional study. Diabet Med. 2018;35(11):1523–1530. doi:10.1111/dme.13760
21. Varni JW, Burwinkle TM, Jacobs JR, Gottschalk M, Kaufman F, Jones KL. The pedsQLTM in type 1 and type 2 diabetes: reliability and validity of the pediatric quality of life inventoryTM generic core scales and type 1 diabetes module. Diabetes Care. 2003;26(3):631–637. doi:10.2337/diacare.26.3.631
22. Varni JW, Seid M, Kurtin PS. PedsQLTM 4.0: reliability and validity of the pediatric quality of life inventoryTM version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812. doi:10.1097/00005650-200108000-00006
23. Kim TK. T test as a parametric statistic. Korean J Anesthesiol. 2015;68(6):540. doi:10.4097/kjae.2015.68.6.540
24. Khanolkar AR, Amin R, Taylor-Robinson D, Viner RM, Warner JT, Stephenson T. Young people with Type 1 diabetes of non-white ethnicity and lower socio-economic status have poorer glycaemic control in England and Wales. Diabetic Med. 2016;33(11):1508–1515. doi:10.1111/dme.13079
25. Dudley B, Heiland B, Kohler-Rausch E, Kovic M. Education and technology used to improve the quality of life for people with diabetes mellitus type II. J Multidiscip Healthc. 2014;7:147–153. doi:10.2147/JMDH.S52681
26. Algahtani FD, Hassan SU, Alsaif B, Zrieq R. Assessment of the quality of life during COVID-19 pandemic: a cross-sectional survey from the kingdom of saudi arabia. Int J Environ Res Public Health. 2021;18(3):847. doi:10.3390/ijerph18030847
27. Friedman D, Nessler D, Cycowicz YM, Horton C. Development of and change in cognitive control: a comparison of children, young adults, and older adults. Cogn Affect Behav Neurosci. 2009;9(1):91–102. doi:10.3758/CABN.9.1.91
28. Luna B. Developmental changes in cognitive control through adolescence. Adv Child Dev Behav. 2009;37:233–278.
29. Giustini DM, Ali SM, Fraser M, Boulos MNK. Effective uses of social media in public health and medicine: a systematic review of systematic reviews. Online J Public Health Inform. 2018;10(2). doi:10.5210/ojphi.v10i2.8270
30. Mukhtar K, Javed K, Arooj M, Sethi A. Advantages, limitations and recommendations for online learning during covid-19 pandemic era. Pak J Med Sci. 2020;36:S27–31.
31. Alonso Martín DE, Roldán Martín MB, Álvarez Gómez MÁ, et al. Impact of diabetes education on type 1 diabetes mellitus control in children. Endocrinol Nutr. 2016;63(10):536–542. doi:10.1016/j.endonu.2016.08.004
32. Vimalavathini R, Agarwal B, Gitanjali B. Educational program for patients with type-1 diabetes mellitus receiving free monthly supplies of insulin improves knowledge and attitude, but not adherence. Int J Diabetes Dev Ctries. 2008;28(3):86–90. doi:10.4103/0973-3930.44079
33. Mouslech Z, Somali M, Sarantis L, et al. Significant effect of group education in patients with diabetes type 1. Hormones. 2018;17(3):397–403. doi:10.1007/s42000-018-0054-0
34. Abdul-Rasoul M, Alotaibi F, Abdulla A, Rahme Z, Alshawaf F. Quality of life of children and adolescents with type 1 diabetes in Kuwait. Med Princ Pract. 2013;22(4):379–384. doi:10.1159/000347052
35. Datye KA, Moore DJ, Russell WE, Jaser SS. A Review of adolescent adherence in type 1 diabetes and the untapped potential of diabetes providers to improve outcomes. Curr Diab Rep. 2015;15(8):1–9. doi:10.1007/s11892-015-0621-6
36. Gandhi K, Vu B-MK, Eshtehardi SS, Wasserman RM, Hilliard ME. Adherence in adolescents with Type 1 diabetes: strategies and considerations for assessment in research and practice. Diabetes Manag. 2015;5(6):485–498. doi:10.2217/dmt.15.41
37. Harjutsalo V, Sjöberg L, Tuomilehto J. Time trends in the incidence of type 1 diabetes in Finnish children: a cohort study. Lancet. 2008;371:1777–1782.
38. Redondo MJ, Eisenbarth GS. Genetic control of autoimmunity in Type I diabetes and associated disorders. Diabetologia. 2002;45(5):605–622. doi:10.1007/s00125-002-0781-1
39. Mackey ER, O’Brecht L, Holmes CS, Jacobs M, Streisand R. Teens with type 1 diabetes: how does their nutrition measure up? J Diabetes Res. 2018;2018:5094569. doi:10.1155/2018/5094569
40. Gregory JM, Slaughter JC, Duffus SH, et al. COVID-19 severity is tripled in the diabetes community: a prospective analysis of the pandemic’s impact in type 1 and type 2 diabetes. Diabetes Care. 2021;44(2):526–532. doi:10.2337/dc20-2260
41. Singh K, Kondal D, Mohan S, et al. Health, psychosocial, and economic impacts of the COVID-19 pandemic on people with chronic conditions in India: a mixed methods study. BMC Public Health. 2021;21(1):1–5. doi:10.1186/s12889-021-10708-w
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
