Back to Journals » International Journal of General Medicine » Volume 15
Quality of Life Among Children with Inflammatory Bowel Disease in Saudi Arabia: A Cross-Sectional Study
Authors Alahmari AA , AlShawaf SH , Meshikhes HA , Aleid BA , Aldossari RM , Shafey MM , Aladsani AA, Al-ibraheem AA, AlRubia NM, AlQahtani SA
Received 30 October 2022
Accepted for publication 21 December 2022
Published 29 December 2022 Volume 2022:15 Pages 8775—8786
DOI https://doi.org/10.2147/IJGM.S394914
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abdulaziz A Alahmari,1 Sarah H AlShawaf,2 Huda A Meshikhes,2 Bedour A Aleid,2 Raghad M Aldossari,2 Marwa M Shafey,3 Ahmed A Aladsani,1 Abdulazeem A Al-ibraheem,4 Nawal M AlRubia,5 Saleh A AlQahtani1
1Department of Pediatrics, King Fahd Hospital of the University, Imam Abdulrahman Bin Faisal University, Dammam, Kingdom of Saudi Arabia; 2College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Kingdom of Saudi Arabia; 3Department of Family and Community Medicine, College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Kingdom of Saudi Arabia; 4Department of Pediatrics, Maternal and Children’s Hospital, Ministry of Health, Alhassa, Kingdom of Saudi Arabia; 5Department of Pediatrics, Maternal and Children’s Hospital, Ministry of Health, Dammam, Kingdom of Saudi Arabia
Correspondence: Abdulaziz A Alahmari, Department of Pediatrics, King Fahd Hospital of the University, Imam Abdulrahman bin Faisal University, Dammam, 34212, Kingdom of Saudi Arabia, Tel +966 59 884 0373, Email [email protected]
Purpose: The aim of this study was to investigate the quality of life in children and adolescents aged 7– 18 years with inflammatory bowel disease and identify the factors that influence it.
Patients and Methods: A multi-center cross-sectional study in which participants were recruited from 3 governmental hospitals in the Eastern Province of Saudi Arabia. A total of 61 children with inflammatory bowel disease were approached, 44 participants were included according to their age (7– 18 years), disease duration of at least 6 months, and without any other co-morbidities. A translated Arabic version of the IMPACT-III questionnaire was used to assess the quality of life of the participants with inflammatory bowel disease. In addition, disease-specific indices were used to measure their disease activity; Harvey Bradshaw for patients with Crohn’s disease and Pediatric Ulcerative Colitis Activity Index for ulcerative colitis patients.
Results: The mean age of the 44 participants was 13.36 ± 2.85. Crohn’s disease accounted for 56.8% of the sample, while 36.4% had ulcerative colitis and 6.8% had unclassified type. The majority were males and in disease remission. The mean total score of the questionnaire was 74.10 ± 12.21, where the domain of social functioning scored the highest and the domain of emotional functioning scored the lowest. Children who are 11 years or older scored significantly higher in emotional functioning and total mean scores. Statistical significance was also observed between the well-being domain and not having flare-ups in the past year, as well as disease severity with emotional functioning, body image, and total mean scores. It was found that corticosteroid utilization is a predictor of poorer quality of life and was statistically significant with the body image domain.
Conclusion: Measuring the quality of life in children with inflammatory bowel disease can aid in reducing its burden and help address its factors.
Keywords: quality of life, IMPACT-III, pediatrics, Crohn’s disease, ulcerative colitis
Introduction
Inflammatory bowel disease (IBD) is a chronic relapsing inflammatory disorder of the gastrointestinal tract of which its manifestations range widely on the spectrum of intestinal and extraintestinal manifestations. This disease entity encompasses two distinctive types: Crohn’s disease (CD) and ulcerative colitis (UC). A patient not fitting in any of the aforementioned types is diagnosed with the less common third type known as unclassified IBD. Approximately 20% to 30% of the patients are diagnosed during childhood or adolescence.1,2
The incidence and prevalence of this disease is on a continuous rise around the world.3 A variation in the incidence of IBD pediatric patients was observed in different regions of Saudi Arabia, and a notable increase of incidence was noticed in the years 2003–2007 and 2008–2012. The highest increase of incidence rate for both CD and UC was found in the Eastern Province of the Kingdom, where it increased from 0.23 to 0.7 per 100,000 persons per year and from 0.13 to 0.27 per 100,000 persons per year, respectively. The mean age of diagnosis in this region for UC was 9 years, while CD was at the age of 12.3 years.4
Because pediatric IBD peaks in late childhood, which is an important transitional age, the collective effect of the experienced intestinal and extraintestinal symptoms, complications, treatment course, and side effects can greatly affect them physically and psychologically, and impair their social, academic, and family functioning,5 leading to a reduction in their quality of life (QoL).6,7 Therefore, measuring the QoL of these patients plays a pivotal role in providing them with the best care, in addition to improving and measuring the efficacy of their treatment regimens.8 Since there is no ultimate cure for IBD, the current treatment goals for pediatric patients are to reduce the physical manifestations and complications, and improve their QoL.9
The QoL of IBD pediatric patients has been considerably explored globally using either generic tools like Pediatric QoL Inventory (PedsQL) and Child QoL Questionnaire, or disease-specific questionnaire by using IMPACT-III.10 The only documented disease-specific tool in the literature that is used in this population was IMPACT-III questionnaire. In addition, it was translated into various languages and employed on children with IBD in different countries and cultures.11,12 A single center study conducted in Saudi Arabia used an Arabic version of a different country on 38 IBD pediatric patients.13 The presenting study aims to investigate the QoL in children and adolescents aged 7–18 years with IBD in 3 hospitals and identify the factors that influence their QoL in the Eastern Province of Saudi Arabia.
Methods
Study Design, Setting and Sampling Technique
A cross-sectional descriptive study was conducted targeting children and adolescents aged 7–18 years with IBD of a duration at least 6 months. Researchers wanted to access all IBD cases registered in the 3 main largest governmental hospitals in the Eastern Province of Saudi Arabia serving gastroenterology pediatric IBD patients. Algorithm for the participant selection process is shown in Figure 1.
 |
Figure 1 Algorithm demonstrating the participant selection process. |
Data Collection
The Institutional Review Board (IRB) of Imam Abdulrahman bin Faisal University in Saudi Arabia granted the ethical approval to conduct the study, with the number (IRB-UGS-2021-01-343). In addition, to ensure data confidentiality, the principles of Declaration of Helsinki were followed. Due to the pandemic restrictions during the period of the data collection (November 2021 until January 2022), a Zoom meeting was arranged with the parents for their children to read and answer the questionnaire themselves.
Measurement Tools and Variables
Sociodemographic and Clinical Characteristics of IBD
The collected data included the age, gender, nationality, height, weight, age at diagnosis, type of disease, co-morbidities, family history of IBD, types of medications used, previous related colonic surgeries, history of relapses, hospitalization, and emergency room (ER) visit in the past year. Medical records of the participants were reviewed to extract the presence or absence of extraintestinal manifestations at the time of study recruitment.
QoL Assessment
The utilized measurement tool for assessing the QoL of children with IBD was IMPACT-III, a questionnaire developed by Dr. Anthony Otley.14 This is a 35-item English questionnaire of 4 domains that assess the social functioning (11 questions), emotional functioning (7 questions), wellbeing (12 questions), and body image (4 questions), all of which are perceived by the afflicted individual. Each of these items have a 5-likert scale. Scores were converted into values from 0 to 100, where a higher total score is interpreted by having a better QoL, and vice versa, and not by a defined cut-off point.
An Arabic translation of the IMPACT-III questionnaire was supervised and guided by the developers in the Pediatric IBD Working Group on QoL, of which the process of linguistic validation consisted of 3 steps.15 The steps were reported back to the original developing research team, to which the approval of the Arabic translation was granted and licensed to be used in Saudi Arabia. The questionnaire was tested for its internal consistency and the reliability Cronbach’s alpha was estimated at 0.89.
Disease Activity
Harvey-Bradshaw Index was used to assess the disease activity of CD patients. This includes the patients’ perception of their general well-being, abdominal pain, number of liquid stools within the last 24 hours and the presence of extra-intestinal manifestations (arthralgia, uveitis, erythema nodosum, aphthous ulcer, pyoderma gangrenosum, anal fissure, fistula, and abscess). The scoring of this index is as follows: remission <5, mild 5–7, moderate 8–16, and severe >16. Pediatric Ulcerative Colitis Activity Index (PUCAI) was used for UC and unclassified-IBD. This is composed of abdominal pain, rectal bleeding, consistency of most stools, number of stools in the last 24 hours, and nocturnal stools. PUCAI categorizes the disease as remission <10, mild 10–34, moderate 35–64, and severe 65–85.16
Data Analysis
Statistical Package for the Social Sciences (SPSS) program version 27 was utilized to process the collected data. The data were coded, entered, and analyzed according to the IMPACT-III tool kit which provides a scoring system for the QoL. As for the descriptive statistics, frequency and percentages were used for the categorical variables, while the mean, standard deviation and median were used for the continuous variables. QoL domains’ scores were tested using Shapiro–Wilk test and were not following a normal distribution. Relationships between QoL domains’ scores and different characteristics were tested using Mann–Whitney U and Kruskal–Wallis tests, while independent t-test and ANOVA test were used for for the normally distributed variables. Individual questions of the IMPACT-III were selected to be analyzed separately; question 2 (Perception of medications Positive/Negative), question 15 (Perception of one’s look Positive/Negative), and question 23 (Experience of bullying Yes/No). The relationship between these questions and various characteristics were tested using Chi2 test and Fisher’s Exact test (FET). Binary logistic regression was also conducted to identify predictors for these individual questions. A p-value <0.05 was considered significant.
Results
Sociodemographic and Clinical Characteristics
The total number of enrolled IBD pediatric patients was 44, with a mean age of 13.36 ± 2.85 years (7–18 years). UC and CD represented 36.4% and 56.8%, respectively, while the unclassified was only 6.8%. Males accounted for 56.8% and Saudis were the majority of the studied population (90.9%).
The mean height for the sample was 147.36 ± 16.98 cm (116–181 cm), while the mean weight was 42.97 ± 16.8 kg (19–104 kg), with a mean body mass index (BMI) of 19.28 ± 5.05 kg/m2 (11.11–33.16). Their BMI percentiles according to their age are shown in Table 1. The mean age of diagnosis was 9.61 ± 2.59 years (2–14 years), with a mean duration of 3.63 ± 2.20 years (1–9 years).
 |
Table 1 Distribution of Children with Inflammatory Bowel Disease According to Their Socioeconomic and Clinical Characteristics |
Approximately 18% had positive family history for IBD, and 45.5% had no flare-ups within the past year. Meanwhile, those who neither visited the ER nor admitted to the hospital in the previous year were 56.8% and 61.4%, respectively. Only 1 participant had previous colonic surgery.
Patients who were in remission represented 59.09%, while mild and moderate cases were 27.27% and 13.64%, respectively. No severe cases were reported in the study. At the time of data collection, 10 patients were exhibiting extraintestinal manifestations. These children were distributed as follows: arthralgia (n = 5), uveitis (n = 2), fistula (n = 2), aphthous ulcer (n = 1), erythema nodosum (n = 1), sacroilitis (n = 1), and thromboembolism (n = 1). Different medications were used by children with IBD; immunomodulators were used by 25 patients, followed by biologics (n = 19), 5-aminosalicylic acids (n = 13) and 7 participants took corticosteroids; summarized in Table 1.
QoL of Children with IBD
Table 2 shows descriptive values of different domains of QoL among children with IBD. It showed that the total QoL score was 74.10 ± 12.21. The highest domain score was reported in social functioning (78.67 ± 13.60) and the least was in the emotional functioning (65.83 ± 18.86). Whereas the body image (75.71 ± 16.35) and wellbeing domains (75.66 ± 16.04) scored nearly equal results.
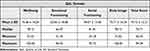 |
Table 2 Descriptive Values for Different Domains of IMPACT-III |
Factors Related to QoL
Table 3 demonstrates the relation between IMPACT-III domains and their total score with different sociodemographic and clinical characteristics. As demonstrated, no significant differences were observed in relation to gender, ER visits nor clinical type of IBD with the domains. Whereas mean domain scores and total scores were observed higher among age ≥11 years, significance was met with emotional functioning and total QoL scores, p < 0.05. Children with IBD who did not experience a flare-up in the past year had higher scores in all domains, to which statistical significance was observed in the wellbeing domain. Hospital admission was significantly different with only the total QoL mean scores. Regarding IBD severity, it was observed that scores were higher among children in remission than those who had mild or moderate severity, where differences were statistically significant in emotional functioning, body image and total mean scores. A boxplot (Figure 2) illustrates the total QoL scores according to the participants disease severity. The use of corticosteroids was significantly related to the body image domain. As shown in Figure 3, more than three-quarters of children with IBD were satisfied with their looks (79.54%) and with their medications (77.28%), and only 4.54% experienced bullying.
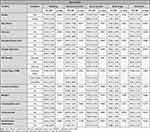 |
Table 3 Relation of Quality of Life Domains and Total Scores with Different Characteristics |
 |
Figure 2 The total quality of life scores across the disease severity categories. |
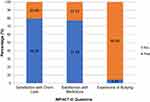 |
Figure 3 Distribution of children with inflammatory bowel disease in relation to individual questions on IMPACT-III. |
Association Between Individual QoL Questions and Children’s Characteristics
It is noted in Table 4 that higher percentages of children with IBD who were unsatisfied with their body image were seen among those who had a flare-up in the past year, not in disease remission, and in those who were using corticosteroid. Significance was only met with corticosteroid intake FET p = 0.002. Logistic regression confirms that those who do not take corticosteroid were 20.62 times more likely satisfied with their body image (p = 0.002).
 |
Table 4 Body Image Satisfaction with Inflammatory Bowel Disease Clinical Characteristics |
Regarding children’s experience with bullying, those who had moderate disease severity experienced bullying significantly higher than those in remission (FET p = 0.016). Higher percentages of children with IBD who were unsatisfied with their medications were observed among those taking corticosteroids and immunomodulators, although significance was only seen in the latter (FET p = 0.027).
Discussion
IBD is known to severely interfere with the lives of those who are afflicted with it, rendering them with a lesser perception of the quality of their lives. The World Health Organization (WHO) has defined QoL as “individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns”.17
In our study, the total mean score of the 4 QoL domains of our participants was found to be 74.10 ± 12.21, which is lower than that observed among Spanish children with IBD.18 The highest mean score in our report was observed in social functioning domain 78.67 ± 13.60, consistent with other studies.13,19,20 This may be noted that 95.46% of our participants were not bullied, as the majority of our participants were in remission. Therefore, they were bullied significantly less than those in moderate disease activity leading to higher social domain scores.
Regarding the sociodemographic factors, there was no statistical difference between genders and QoL scores, coinciding with several studies.13,19,21,22 Conversely, other studies reported that females scored lower in the total and some of the domain scores.23,24 Concerning age, it has been reported that adolescents scored significantly lower QoL than younger children.23 On the contrary, a Greek study illustrated a positive correlation between age and QoL, attributing it to the development of coping mechanisms as children grow into adolescence.25 This concurs with our findings as the older the child, the higher the total mean and emotional functioning scores. However, there are numerous studies that stated nonsignificant correlation between the age and QoL.19,21,22,24
The domain with the lowest mean score was attained in the emotional functioning 65.83 ± 18.86. One aspect related to this domain was how children were inconvenienced by their medications. When asked if their medications bothered them, 22.72% were troubled. Of that sample, 56.8% were using immunomodulators, to which it involves commuting all the way to the hospital to receive the dose through infusion for up to 6 hours. Lowe et al22 also found that this was one of the least scored questions among CD patients.
Regarding the domain of body image, there are a limited number of studies that measured body image dissatisfaction in IBD children. We illustrated higher significant percentages of body image dissatisfaction among children with moderate IBD severity. This goes in full accordance with Claytor et al,26 who elaborated that patients who were not in remission reported more body image dissatisfaction in contrast to their counterparts. The majority of IBD children who were not satisfied with their body image were taking corticosteroids (71.4%) with a p-value of 0.002. Our results did not show statistical significance between corticosteroid use and total QoL score, in contrary to that in the South Korean study which may be attributable to their use of different measurement tools.27 As our logistic regression results demonstrated, those who do not take corticosteroids were approximately 21 times more likely to have good perception of their body image than those who receive corticosteroids.
Our analysis showed that the wellbeing of pediatrics with IBD was significantly lower among those who experienced a flare-up within the past year, a factor that can be attributed to the endured symptoms during the relapses which was in line with the Italian study.23 Another major finding was seen in those who were admitted to the hospital within the past year, in which they displayed a significantly lower total mean score than those who did not. This is expected as those who do get admitted are warranted for having severe flare-ups that are in need for further medical interventions, management, and monitoring. On the contrary, a Greek study reported that hospitalizations in the previous 3 months did not correlate with the total mean score.25
Several reports demonstrated that the prevalence of extraintestinal manifestations among IBD patients is higher in children than in adults. Generally, the most common extraintestinal manifestation in IBD is musculoskeletal in the form of arthralgia,28–30 and this was seen to be the highest in our study. Regarding the correlation between the extraintestinal manifestations and the QoL in IBD patients, one study observed a negative association with the emotional and social functioning.25 Although individuals with extraintestinal manifestations had lower mean score in emotional functioning, there was no statistical significance in our results. This may be due to the low number of extraintestinal manifestations in our study.
Limitations
One of the study’s main advantages is that it was conducted in three cities in Saudi Arabia’s eastern region on a multicenter basis. However, our small sample size could be due to the rather low prevalence of IBD among pediatrics and some parents refusing to allow their children to participate. QoL is a subjective issue that is regarded differently by each individual, which could result in self-reported bias. In addition, some questions were dependent on participants’ memories leading to recall bias.
Recommendations
Nonetheless, our findings brought light to critical aspects of IBD’s psychological, social, and emotional effects on children and their families in Saudi Arabia. The significance of these findings is likely to be meaningful in the development of a system that incorporates psychosocial support for those who are in need. This highlights the role which IMPACT-III may play as a periodical screening tool in the clinical practice to pinpoint the issues that IBD may cause for these children and their families throughout their disease course. A larger sample with variations in disease severity as well as the inclusion of patients from all regions of Saudi Arabia is needed to demonstrate a more representative result that is applicable to the population. Furthermore, conducting interviews with the patients for qualitative research can help explore and probe on the factors that impact their lives.
Conclusion
In conclusion, the QoL of IBD pediatrics is highly influenced by the severity of the disease, and the type of medication used, specifically corticosteroids and immunomodulators. The highest and lowest domain scores were observed in social functioning and emotional functioning, respectively. Early detection of physical and psychological issues may help to alleviate the burden of the disease on the children and their families. It is important to conduct further research to measure the QoL of IBD children on a larger scale and to identify further factors that may interfere with the lives of IBD pediatric patients in Saudi Arabia.
Abbreviations
IBD, Inflammatory bowel disease; CD, Crohn’s disease; UC, Ulcerative colitis; QoL, Quality of life; PedsQL, Pediatric QoL Inventory; SPSS, Statistical Package for the Social Sciences; FET, Fisher’s Exact test; ER, Emergency room; BMI, Body mass index; WHO, World Health Organization.
Ethics Approval and Consent
The ethical approval was acquired from Institutional Review Board (IRB) of Imam Abdulrahman bin Faisal University in Saudi Arabia, with the number (IRB-UGS-2021-01-343). Informed consent was obtained from the guardians and children. The participants were informed that the data will be anonymized.
Acknowledgment
The authors would like to acknowledge the contributions of all the following for their assistance in the research process: Bradley MacIntyre, Anthony Otley, Sarah Itani, Abdullah AlMusharraf and all the patients and their guardians that participated in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis. 2010;17(1):423–439. doi:10.1002/ibd.21349
2. Malaty HM, Fan X, Opekun AR, Thibodeaux C, Ferry GD. Rising incidence of inflammatory bowel disease among children: a 12-year study. J Pediatr Gastroenterol Nutr. 2010;50(1):27–31. doi:10.1097/MPG.0b013e3181b99baa
3. Alatab S, Sepanlou SG, Ikuta K, et al. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(1):17–30. doi:10.1016/S2468-1253(19)
4. El Mouzan MI, AlEdreesi MH, Hasosah MY, Al-Hussaini AA, Al Sarkhy AA, Assiri AA. Regional variation of pediatric inflammatory bowel disease in Saudi Arabia: results from a multicenter study. World J Gastroenterol. 2020;26(4):416–423. doi:10.3748/wjg.v26.i4.416
5. Bramuzzo M, De Carlo C, Arrigo S, et al. Parental psychological factors and quality of life of children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2020;70(2):211–217. doi:10.1097/mpg.0000000000002548
6. Greenley RN, Hommel KA, Nebel J, et al. A meta-analytic review of the psychosocial adjustment of youth with inflammatory bowel disease. J Pediatr Psychol. 2010;35(8):857–869. doi:10.1093/jpepsy/jsp120
7. Mackner LM, Greenley RN, Szigethy E, Herzer M, Deer K, Hommel KA. Psychosocial issues in pediatric inflammatory bowel disease: report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2013;56(4):449–458. doi:10.1097/MPG.0b013e3182841263
8. Haraldstad K, Wahl A, Andenæs R, et al. A systematic review of quality of life research in medicine and health sciences. Quality Life Res. 2019;28(10):2641–2650. doi:10.1007/s11136-019-02214-9
9. Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr. 2015;169(11):1053–1060. doi:10.1001/jamapediatrics.2015.1982
10. Grant A, Otley A. Measurement of quality of life in pediatric inflammatory bowel disease. In: Mamula P, Grossman AB, Baldassano RN, Kelsen JR, Markowitz JE, editors. Pediatric Inflammatory Bowel Disease. Springer International Publishing; 2017:625–638.
11. Chen XL, Zhong LH, Wen Y, et al. Inflammatory bowel disease-specific health-related quality of life instruments: a systematic review of measurement properties. Health Qual Life Outcomes. 2017;15(1):177. doi:10.1186/s12955-017-0753-2
12. Conrad MA, Rosh JR. Pediatric Inflammatory Bowel Disease.
13. Alhadab AA, AlMahamed SN, Hassan IE, Hammo AH. The impact of inflammatory bowel diseases on the quality of life of Saudi pediatric patients: a cross-sectional study. Saudi J Gastroenterol. 2022;28(6):448–455. doi:10.4103/sjg.sjg_162_22
14. Otley A, Smith C, Nicholas D, et al. The IMPACT questionnaire: a valid measure of health-related quality of life in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2002;35(4):557–563. doi:10.1097/00005176-200210000-00018
15. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–3191. doi:10.1097/00007632-200012150-00014
16. Shaoul R, Day AS. An overview of tools to score severity in pediatric inflammatory bowel disease. systematic review. Front Pediatrics. 2021;9. doi:10.3389/fped.2021.615216
17. Kim S. The World Health Organization Quality of Life (WHOQOL) User Manual. World Health Organization; 2012.
18. Navas-López VM, Martel LC, Martín-Masot R, et al. The effect of the inflammatory bowel disease classroom in nature on the quality of life of patients with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2020;71(2):243–245. doi:10.1097/mpg.0000000000002746
19. Gallo J, Grant A, Otley AR, et al. Do parents and children agree? Quality-of-life assessment of children with inflammatory bowel disease and their parents. J Pediatr Gastroenterol Nutr. 2014;58(4):481–485. doi:10.1097/mpg.0000000000000236
20. Malik BA, Gibbons K, Spady D, Lees G, Otley A, Huynh HQ. Health-related quality of life in pediatric ulcerative colitis patients on conventional medical treatment compared to those after restorative proctocolectomy. Int J Colorectal Dis. 2013;28(3):325–333. doi:10.1007/s00384-012-1561-0
21. Grant A, MacIntyre B, Kappelman MD, Otley AR, New Domain A. Structure for the IMPACT-III Health-related Quality of life Tool for Pediatric Inflammatory Bowel Disease. J Pediatr Gastroenterol Nutr. 2020;71(4):494–500. doi:10.1097/mpg.0000000000002824
22. Lowe W, Kenwright D, Wyeth J, Blair N. Crohn disease: effect on children’s lifestyles. J Pediatr Gastroenterol Nutr. 2012;54(3):397–400. doi:10.1097/MPG.0b013e318231cf17
23. Gatti S, Del Baldo G, Catassi G, et al. Factors associated with quality of life in Italian children and adolescents with IBD. Sci Rep. 2021;11(1):18076. doi:10.1038/s41598-021-97661-1
24. Kim S, Park S, Kang Y, et al. Can we estimate quality of life in pediatric inflammatory bowel disease patients? An Asian multicenter study. J Pediatr Gastroenterol Nutr. 2019;68(1):45–49. doi:10.1097/mpg.0000000000002119
25. Chouliaras G, Margoni D, Dimakou K, Fessatou S, Panayiotou I, Roma-Giannikou E. Disease impact on the quality of life of children with inflammatory bowel disease. World J Gastroenterol. 2017;23(6):1067–1075. doi:10.3748/wjg.v23.i6.1067
26. Claytor JD, Kochar B, Kappelman MD, Long MD. Body image dissatisfaction among pediatric patients with inflammatory bowel disease. J Pediatr. 2020;223:68–72.e1. doi:10.1016/j.jpeds.2020.04.045
27. Kum DJ, Bang K-S. Body image, self-esteem, and quality of life in children and adolescents with inflammatory bowel disease in a tertiary hospital in South Korea. Child Health Nurs Res. 2021;27(2):181–189. doi:10.4094/chnr.2021.27.2.181
28. Aloi M, Cucchiara S. Extradigestive manifestations of IBD in pediatrics. Eur Rev Med Pharmacol Sci. 2009;13(Suppl 1):23–32.
29. Jose FA, Garnett EA, Vittinghoff E, et al. Development of extraintestinal manifestations in pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(1):63–68. doi:10.1002/ibd.20604
30. Rogler G, Singh A, Kavanaugh A, Rubin DT. Extraintestinal manifestations of inflammatory bowel disease: current concepts, treatment, and implications for disease management. Gastroenterology. 2021;161(4):1118–1132. doi:10.1053/j.gastro.2021.07.042
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
