Back to Journals » International Journal of Women's Health » Volume 15
Quality of Life After Treatment for Pelvic Organ Prolapse: Vaginal Pessary versus Surgery
Authors Aimjirakul K, Pumtako M, Manonai J
Received 26 January 2023
Accepted for publication 11 July 2023
Published 12 July 2023 Volume 2023:15 Pages 1017—1025
DOI https://doi.org/10.2147/IJWH.S406048
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Komkrit Aimjirakul, Mintita Pumtako, Jittima Manonai
Department of Obstetrics & Gynaecology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Jittima Manonai, Email [email protected]
Background: Pelvic organ prolapse (POP) is quite common and has an impact on quality of life (QoL). The evaluation of QoL after treatment for prolapse is important. The objective was to compare patient’s prolapse symptoms, functional outcomes, and quality of life between pessary and surgery using standardized questionnaires at 1 and 6 months after treatment.
Methods: We conducted a prospective study including women with symptomatic POP who chose pessary or surgery as the first-line treatment. We evaluated QoL using the International Consultation on Incontinence Questionnaire-Vaginal Symptoms and Prolapse Quality of Life questionnaires.
Results: Seventy-two participants were enrolled, with 36 in each group. Body mass index, menopausal status, marital status, number of vaginal deliveries, and stage of pelvic organ prolapse were not significantly different between the groups. At 1 and 6 months after treatment, participants in both groups reported significant improvement in prolapse symptoms, functional outcomes, and overall quality of life. At 1 month after treatment, absolute changes in vaginal symptom scores in the pessary and surgery groups were − 16.67 and − 19.03, respectively (p > 0.05); at 6 months, the absolute changes were − 19.21 and − 19.25, respectively (p > 0.05). Significant improvement was only found in role limitation and physical and social domains at both follow-up times after surgery.
Conclusion: At 1 and 6 month(s) after treatment, women with symptomatic POP reported substantial improvement in prolapse symptoms and functional outcomes when treated with pessary or surgical correction.
Keywords: quality of life, pelvic organ prolapse, pessary, surgery
Introduction
Pelvic organ prolapse (POP) is a condition with high prevalence among older women. It is widely accepted that 50% of women will develop prolapse.1 The prevalence rate reported among postmenopausal Thai women is approximately 43%.2 Complaints of feeling or seeing a bulge, increased heaviness, and abnormal vaginal bleeding are common in affected women.3 Additionally, prolapse-related lower urinary tract symptoms, anorectal dysfunction, and sexual dysfunction are also reported. Consequently, POP can negatively affect a woman’s quality of life (QOL) by decreasing confidence, limiting activities and other restrictions including sexual, social, emotional, and sleep aspects.4,5
The aim of POP treatment is to improve a woman’s symptoms, functioning, and QOL. Generally, the options for treating symptomatic POP are physiotherapy, pessary and surgical treatment. The advantages of using a pessary are an immediate effect on prolapse-specific QOL and non-invasiveness whereas disadvantages may comprise discomfort, vaginal discharge, and the need for regular cleaning and clinic visits.6,7 Most choices of surgery for POP are obliterative procedures and reconstructive procedures.8 These procedures can eliminate prolapse symptoms and do not require long-term follow-up: however, they can be associated with surgical complications or recurrence. The individual treatment option depends on a woman’s treatment goals and preferences. Several studies have shown that both surgery and pessary can improve POP symptoms, and the clinical outcomes of treatment are not different between groups.9–15 However, a previous study demonstrated substantial inconsistencies between POP symptom scores in physician interviews and patient-reported responses to a questionnaire. Those authors recommended the use of a validated questionnaire to evaluate functional outcomes, for a more realistic assessment.16 There are few well-designed comparative studies focusing on functional outcomes and QOL after undergoing these two treatment options using validated questionnaires. We aimed to conduct a study among a prospective cohort of women with symptomatic POP. The objective was to compare the effects of vaginal pessary and surgery on QOL, vaginal symptoms, and functional outcomes using the International Consultation on Incontinence Questionnaire-Vaginal Symptoms (ICIQ-VS)17 and Prolapse Quality of Life (P-QOL) questionnaires18 at 1 and 6 month(s) after treatment.
Materials and Methods
We conducted a prospective, observational study among women with symptomatic POP at an academic hospital in Bangkok between May 2019 and June 2020. This study was approved by our institutional review board, Faculty of Medicine Ramathibodi Hospital (No. MURA2019/239) and complied with the Declaration of Helsinki. We included women with POP at least stage II using the Pelvic Organ Prolapse Quantification (POP-Q) system.19 Women with symptomatic POP were methodically evaluated and comprehensively counseled about the treatment options, including pessary and surgery. We excluded women with unsuccessful fitting from the study. Women with cognitive impairment who were unable to complete the questionnaires, those who refused to participate, were pregnant, and those who had undergone prior treatment with either pessary or surgery were also excluded. Participants who started in the pessary group but subsequently requested surgery were excluded from the analysis in both the surgery and pessary groups. After women had made their treatment decision, the second author (MP) consecutively identified eligible participants, adequately explained the study, distributed the participant information sheet, and recruited an adequate sample. Written informed consent was obtained from all participants before entering in the study. At the initial visit, demographic data were obtained. All participants were asked to read the baseline questionnaires and record their responses themselves, which were the validated Thai version of the ICIQ-VS questionnaire20 and the P-QOL questionnaire.21 Afterward, participants were scheduled for follow-up appointments at 1 and 6 months according to the routine clinical appointments and completed the same questionnaires. The primary outcome was changes in functional outcomes and overall QOL after treatment. Changes in prolapse-related impact were measured using domain 2 (sexual matters subscale) of the ICIQ-VS and domains 3–7 (role limitations, physical and social limitations, personal relationships, emotional problems, and sleep or energy disturbance) of the P-QOL. Improvement in overall QOL was evaluated using domain 3 (QOL subscale) of the ICIQ-VS and domain 2 (prolapse impact) of the P-QOL. The secondary outcome was improvement in prolapse symptoms after treatment measured using domain 1 (vaginal symptoms subscale) of the ICIQ-VS and domain 8 (severity measures) of the P-QOL. Based on both questionnaires used, lower scores indicate a lesser impairment of quality of life. The sample size was calculated for QOL as evaluated using the validated ICIQ-VS as the primary endpoint. A difference between the interventions of 17.5 points in the domain of vaginal symptoms of the ICIQ-VS at 6 months after treatment was considered clinically relevant.6 We used IBM SPSS version 21.0 (IBM Corp., Armonk, NY, USA) for the statistical analysis. Continuous data are described using mean (SD). The Student’s t-test and Pearson chi-square test were used to compare continuous and categorical baseline demographic parameters, respectively. The pairwise comparison test was used to assess change in symptoms and impact scores from baseline to 1 and 6 month(s) in each of the two groups. A p-value < 0.05 was considered to be statistically significant in the analysis.
Results
We approached a total of 80 women with symptomatic prolapse. Women who experienced unsuccessful pessary fitting were excluded, resulting in 72 women who participated in the study; 36 women preferred the pessary and 36 opted for surgery. As shown in Figure 1, five participants discontinued using a pessary; the reasons were inconvenience of use (80.0%) and abnormal vaginal discharge (20.0%). Two patients were lost to follow-up. A ring with support pessary had been used in all pessary users. The list of surgeries included 14 vaginal hysterectomies with anterior colporrhaphy with posterior colpoperineorrhaphy, 8 vaginal hysterectomies with anterior colporrhaphy, 1 vaginal hysterectomy with posterior colpoperineorrhaphy, 3 anterior colporrhaphy with posterior colpoperineorrhaphy, 2 anterior colporrhaphy, 1 posterior colpoperineorrhaphy, 5 vaginal hysterectomies with colpocleisis and 5 colpocleisis procedures.
 |
Figure 1 Participants’ flow diagram. |
The demographic and clinical characteristics of all participants are presented in Table 1. The two groups were not significantly different with respect to age, BMI, menopausal status, marital status, number of vaginal deliveries, and stage of POP. Only 3/36 (8.3%) participants in the pessary group and 4/36 (11.1%) in the surgery group were sexually active, which would not be unexpected according to our cultural context. The surgical-case and pessary-care protocols of our institute includes follow-up visits with urogynecologists and/or specialized nurses at 1 to 2 weeks, 1 month, 3 and 6 months after surgery or pessary fitting.
 |
Table 1 Demographic and Clinical Characteristics of All Participants (N = 72) |
Baseline scores for prolapse symptoms, functional outcome, and QOL of all participants are shown in Table 2. ICIQ-VS vaginal symptom scores were not significantly different between the pessary (22.7 ± 11.5) and surgery (23.7 ± 12.3) groups (p > 0.05). P-QOL severity scores were also comparable, with 40.0 ± 18.0 and 49.1 ± 16.7, respectively (p > 0.05). Regarding functional outcomes and QOL using ICIQ-VS and P-QOL scores in the role limitation, physical and social limitations, and emotional problems domains were clearly higher in the surgery group (p < 0.05).
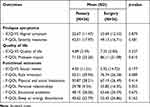 |
Table 2 Baseline Scores of Prolapse Symptoms, Quality of Life, and Functional Outcomes of Participants Who Underwent Pessary or Surgery Treatment (N = 72) |
Findings regarding improvement in prolapse symptoms and impact on QOL after pessary and surgical treatment are presented in Figure 2. Considering ICIQ-VS scores, participants in both groups reported significant improvement in overall QOL subscales at 1 month and 6 months after treatment (p < 0.05). In view of functional outcomes using the P-QOL questionnaire, scores for role limitation, physical and social limitations, and emotional problems were significantly decreased in both treatment groups (p < 0.05). However, improvement in sleep or energy was only observed in the surgery group (p < 0.05).
Table 3 shows the results of comparing absolute changes in scores regarding prolapse symptoms, overall QOL, and improvement in functional outcomes between the two groups at 1 and 6 month(s). There were no significant differences in ICIQ-VS scores between the two groups at 1 and 6 month(s) after treatment (p > 0.05). Considering P-QOL severity score, participants in the surgery group reported greater symptom improvement than the pessary group at 1 month (p = 0.040) whereas the improvement was comparable at 6 months (p > 0.05). Regarding functional outcomes, there was greater improvement in the surgery group for role limitation and physical and social domains at both follow-ups, as compared with the pessary group (p < 0.05).
Percent changes in ICIQ-VS and P-QOL for the two groups at 1 and 6 month(s) are shown in Table 4. Greater percent changes in P-QOL severity scores were demonstrated in the surgery group versus the pessary group at 1 month (p = 0.007) but not at 6 months (p > 0.033). There were statistically significant differences noted between the pessary and surgery groups at 1 and 6 month(s) after treatment in physical and social domains according to P-QOL scores (p < 0.05). The percent changes in P-QOL role limitation and emotional problems scores were higher in the surgery group at 1 month (p = 0.004) and 6 months (p = 0.035).
 |
Table 4 % Changes of Prolapse Symptoms, Quality of Life Scores and Functional Outcome After 1 Month and 6 Months of Treatment in Participants Who Underwent Pessary or Surgery (N = 61) |
Discussion
The current study was a direct comparison study to assess the effect of two treatment options on functional outcomes of POP. We found improvement in the main outcome measures (prolapse symptoms, functional outcomes and overall QOL) after 1 and 6 month(s) of treatment. Although vaginal symptoms after treatment decreased equally, the negative impact of prolapse symptoms on QOL perceived by women was greatly reduced after a surgical procedure compared with pessary use. Surgical treatment also offered better improvement in terms of role limitation, physical and social limitations, and emotional problems among women with symptomatic POP.
Women who choose surgical treatment commonly describe more severe and bothersome symptoms and have a more advanced stage of prolapse than women who choose pessary.10,22 We did not find that age, prolapse stage, or severity of prolapse symptoms noticeably affected how patients made treatment choices. Participants’ perspectives were focused on their QOL including role limitation, physical and social ability, and emotional problems, as captured in patient-reported outcome measures, and these evidently had important roles.
Primary Outcomes (Functional Outcomes and Overall QOL)
From the patient’s perspective, the most important outcome after treatment is the resolution of vaginal or bulge symptoms.23 Functional outcomes of treatment for POP also include physical (physical function and participation), social (social function, relationships, sexual function), and mental (emotional distress, preoccupation, body image) health. Functional outcomes may be an indicator of important alterations to how the patient functions or feels after treatment.16 Therefore, functional outcomes are becoming increasingly relevant for patient well-being and quality of care.24,25 Our findings are consistent with previous studies regarding the positive effect of both pessary and surgical procedures for POP in terms of prolapse symptoms and overall QOL.12–15 However, in a previous study, women who underwent surgery reported significantly greater improvement in physical function, social roles, and depression compared with pessary users.13
Considering the impact of pessary use and surgery on functional outcomes, we found better improvement in role limitations, physical and social limitations, and emotional problems according to the P-QOL among women who had surgical treatment. Those domains are evidently important for treatment success from the patient’s perspective.23 Long-term pessary care and follow-up might explain the lower effect on some functional outcomes after treatment. The pessary-related complications such as vaginal discharge, bleeding, rubbing, and foul odor may outweigh patient benefits from pessary treatment.7 From a clinical point of view, during the preoperative counseling process, clinicians should explore patient’s experience and expectations regarding treatment success. Focusing only on vaginal bulge and associated discomfort might not be sufficient to determine and evaluate patient-reported outcomes after POP treatment. Providing essential information and discussing functional outcomes regarding both treatments can be helpful for shared decision-making among patients with POP.
Secondary Outcome (Prolapse Symptoms)
Using the ICIQ-VS and severity measure in P-QOL, we found a significant improvement in vaginal symptoms at 1- and 6-month follow-up among women who opted for pessary use as well as those who chose surgery. Additionally, both treatment options were equally effective in alleviating prolapse symptoms according to score changes after treatment. These results resemble findings from previous studies reporting that both pessary and surgery are effective treatment options for the management of women with symptomatic POP particularly the prolapse symptom.9,26 Therefore, choosing a pessary or surgery as the first option for treatment of POP can improve prolapse symptoms at 1 and 6 month(s).
The strengths of this study include the pragmatic, comparative design focusing on functional outcomes and QOL after undergoing two treatment options, and validated questionnaires were used for outcome evaluation. The findings of this study provide further information regarding comprehensive functional outcomes of treatment for POP. Nevertheless, the small number of sexually active woman, the considerable number of patients who dropped out of our study, and the short-term follow-up were limitations of this study. Therefore, the study is not representative. Further studies with a larger number of sexually active women and long-term follow-up of more than a year should be conducted. By excluding women who were dissatisfied with pessary treatment, improvement after pessary therapy will be overestimated. However, the present study was not a randomized trial but rather observational prospective study; thus, intention-to-treat analysis could not be applied. Satisfaction and achievement of pre-treatment goals should be explored and evaluated as relevant patient-reported outcome measures.
In conclusion, at 1 and 6 month(s) after treatment, women with symptomatic POP reported substantial improvement in prolapse symptoms, functional outcomes, and overall QOL parameters when treated with pessary or surgical correction.
Acknowledgment
We thank Analisa Avila, MPH, ELS, of Edanz (www.edanz.com/ac) for editing a draft of this manuscript.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Barber MD, Maher CF. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogyn J. 2013;24:1783–1790. doi:10.1007/s00192-013-2169-9
2. Chuenchompoonut V, Bunyavejchevin S, Wisawasukmongchol W, Taechakraichana N. Prevalence of genital prolapse in Thai menopausal women (using new standardization classification). J Med Assoc Thai. 2005;88:1–4.
3. Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogyn J. 2016;27:165–194. doi:10.1007/s00192-015-2932-1
4. Zhu Q, Shu H, Dai Z. Effect of pelvic floor dysfunction on sexual function and quality of life in Chinese women of different ages: an observational study. Geriatr Gerontol Int. 2019;19:299–304. doi:10.1111/ggi.13618
5. Brandt C, Janse van Vuuren EC. Dysfunction, activity limitations, participation restriction and contextual factors in South African women with pelvic organ prolapse. S Afr J Physiother. 2019;75:933–940. doi:10.4102/sajp.v75i1.933
6. Anantawat T, Manonai J, Wattanayingcharoenchai R, Sarit-apirak S. Impact of a vaginal pessary on the quality of life in women with pelvic organ prolapse. Asian Biomed. 2016;10:249–252.
7. Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for managing pelvic organ prolapse in women. Cochrane Database Syst Rev. 2020;11:CD004010. doi:10.1002/14651858.CD004010.pub4
8. The American College of Obstetricians and Gynecologists and the American Urogynecologic Society. INTERIM UPDATE: this practice bulletin is updated as highlighted to reflect the US Food and Drug Administration order to stop the sale of transvaginal synthetic mesh products for the repair of pelvic organ prolapse. Pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2019;25:397–408. doi:10.1097/SPV.0000000000000794
9. Lone F, Thakar R, Sultan AH. One-year prospective comparison of vaginal pessaries and surgery for pelvic organ prolapse using the validated ICIQ-VS and ICIQ-UI (SF) questionnaire. Int Urogyn J. 2015;26:1305–1312. doi:10.1007/s00192-015-2686-9
10. Abdool Z, Thakar R, Sultan AH, Oliver RS. Prospective evaluation of outcome of vaginal pessaries versus surgery in women with symptomatic pelvic organ prolapse. Int Urogyn J. 2011;22:273–278. doi:10.1007/s00192-010-1340-9
11. Coolen AWM, Troost S, Mol BWJ, Roovers JWR, Bongers MY. Primary treatment of pelvic organ prolapse: pessary use versus prolapse surgery. Int Urogyn J. 2018;29:99–107. doi:10.1007/s00192-017-3372-x
12. Miceli A, Dueñas-Diez JL. Effectiveness of ring pessaries versus vaginal hysterectomy for advanced pelvic organ prolapse. A cohort study. Int Urogynecol J. 2019;30:2161–2169. doi:10.1007/s00192-019-03919-8
13. Sung VW, Wohlrab KJ, Madsen A, Raker C. Patient-reported goal attainment and comprehensive functioning outcomes after surgery compared with pessary for pelvic organ prolapse. Am J Obstet Gynecol. 2016;215:
14. Mamik MM, Rogers RG, Qualls CR, Komesu YM. Goal attainment after treatment in patients with symptomatic pelvic organ prolapse. Am J Obstet Gynecol. 2013;209:
15. Barber MD, Walters MD, Cundiff GW; PESSRI Trial Group. Responsiveness of the Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ) in women undergoing vaginal surgery and pessary treatment for pelvic organ prolapse. Am J Obstet Gynecol. 2006;194:1492–1498. doi:10.1016/j.ajog.2006.01.076
16. De Boer TA, Gietelink DA, Vierhout ME. Discrepancies between physician interview and a patient self-assessment questionnaire after surgery for pelvic organ prolapse. Int Urogyn J. 2008;19:1349–1352. doi:10.1007/s00192-008-0656-1
17. Price N, Jackson SR, Avery K, Brookes ST, Abrams P. Development and psychometric evaluation of the ICIQ vaginal symptoms questionnaire: the ICIQ-VS. BJOG. 2006;113:700–712. doi:10.1111/j.1471-0528.2006.00938.x
18. Digesu GA, Khullar V, Cardozo L, Robinson D, Salvatore S. P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J. 2005;16:176–181. doi:10.1007/s00192-004-1225-x
19. Madhu C, Swift S, Moloney GS, Drake MJ. How to use the Pelvic Organ Prolapse Quantification (POP-Q) system. Neurourol Urodyn. 2018;37:39–43. doi:10.1002/nau.23740
20. Sriwat W, Manonai J, Sillaphakit C, Sarit-apirak S, Chittacharoen A. Validation of the Thai version of ICIQ-VS (international consultation on incontinence questionnaire -vaginal symptoms) in Thai women. Rama Med J. 2016;39:1–3.
21. Manchana T, Bunyavejchevin S. Validation of the Prolapse Quality of Life (P-QOL) questionnaire in Thai version. Int Urogyn J. 2010;21:985–993. doi:10.1007/s00192-010-1107-3
22. Bodner-Adler B, Bodner K, Stinglmeier A, et al. Prolapse surgery versus vaginal pessary in women with symptomatic pelvic organ prolapse: which factors influence the choice of treatment? Arch Gynecol Obstet. 2019;299:773–777. doi:10.1007/s00404-019-05046-7
23. Sung VW, Rogers RG, Barber MD, Clark MA. Conceptual framework for patient-important outcomes for pelvic organ prolapse. Neurourol Urodyn. 2014;33:414–419. doi:10.1002/nau.22397
24. Lee H, Vlaev I, King D, Mayer E, Darzi A, Dolan P. Subjective well-being and the measurement of quality in healthcare. Soc Sci Med. 2013;99:27–34. doi:10.1016/j.socscimed.2013.09.027
25. Cichowski S, Grzybowska ME, Halder GE, et al. International urogynecology consultation: patient reported outcome measures (PROs) use in the evaluation of patients with pelvic organ prolapse. Int Urogynecol J. 2022;33(10):2603–2631. doi:10.1007/s00192-022-05315-1
26. Albuquerque Coelho SC, Castro EB, Juliato CR. Female pelvic organ prolapse using pessaries: systematic review. Int Urogynecol J. 2016;27:1797–1803. doi:10.1007/s00192-016-2991-y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


