Back to Journals » Infection and Drug Resistance » Volume 16
Pulmonary Infections and Outcomes in AIDS Patients with Respiratory Failure: A 10-Year Retrospective Review
Authors Hao J, Liu J, Pu L, Li C, Yin N , Li A
Received 31 October 2022
Accepted for publication 8 February 2023
Published 20 February 2023 Volume 2023:16 Pages 1049—1059
DOI https://doi.org/10.2147/IDR.S395658
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Jingjing Hao, Jingyuan Liu, Lin Pu, Chuansheng Li, Ningning Yin, Ang Li
Department of Critical Care Medicine, Beijing Ditan Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Ang Li, Email [email protected]
Background: Respiratory failure in acquired immunodeficiency syndrome (AIDS) patients was the leading cause of intensive care unit (ICU) admission in our center. We aimed to describe the pulmonary infections and outcomes for respiratory failure in AIDS patients.
Methods: A retrospective study was conducted on AIDS adult patients with respiratory failure who were admitted to the ICU in Beijing Ditan hospital, China, from January 2012 to December 2021. We investigated pulmonary infections complicated by respiratory failure in AIDS patients. The primary outcome was ICU mortality, and a comparison between survivors and nonsurvivors was performed. Multiple logistic regression analysis was used to identify predictors of ICU mortality. The Kaplan-Meier curve and Log rank test were used for survival analysis.
Results: A total of 231 AIDS patients were admitted to ICU with respiratory failure over a 10-year period with a male predominance (95.7%). Pneumocystis jirovecii pneumonia was the main etiology of pulmonary infections (80.1%). The ICU mortality was 32.9%. In multivariate analysis, ICU mortality was independently associated with invasive mechanical ventilation (IMV) [odds ratio (OR), 27.910; 95% confidence interval (CI, 8.392– 92.818; p = 0.000) and the time before ICU admission (OR, 0.959; 95% CI, 0.920– 0.999; p = 0.046). In the survival analysis, patients with IMV and later admission to ICU had a higher probability of mortality.
Conclusion: Pneumocystis jirovecii pneumonia was the primary etiology for respiratory failure in AIDS patients admitted to the ICU. Respiratory failure remains a severe illness with high mortality, and ICU mortality was negatively associated with IMV and later admission to ICU.
Keywords: acquired immunodeficiency syndrome, AIDS, respiratory failure, pulmonary infections, ICU mortality
Background
Human immunodeficiency virus (HIV) infected patients, especially at the stage of acquired immunodeficiency syndrome (AIDS), are at high risk for critical illness due to severe opportunistic infections.1 HIV-infected patients are usually admitted to intensive care unit (ICU) for hypoxemic respiratory failure.2–11 Before the introduction of combination antiretroviral therapies (cART), pneumocystis jirovecii pneumonia (PJP), which was previously called PCP, with respiratory failure were the most common causes seen in HIV-infected patients admitted to ICU.4,5 With the use of cART, the proportion of opportunistic infections has significantly decreased.6,7 However, ICU admission rates remained stable and respiratory failure still the leading reason for ICU admission in HIV-infected patients.3,6,8 What’s more, infectious causes remained predominant, with PCP and bacterial pneumonia accounting for most cases.7–10 And other infectious causes causing respiratory failure were pulmonary tuberculosis and severe pneumonia due to non-tuberculosis mycobacteria, Cytomegalovirus (CMV), and other pathogens.1,2 A retrospective cohort study in our center has shown that respiratory failure was the most common condition in HIV-infected patients admitted to ICU.11 When all etiologies causing respiratory failure in patients with HIV admitted to ICU were considered, the proportion of non-infectious etiologies was 21.1%-34.7%.2,12,13 We only focused on patients with pulmonary infections, as the pathophysiological features of respiratory failure caused by pulmonary infections and non-infectious causes were quite different.
We want to know the distribution of etiology of pulmonary infections causing respiratory failure in AIDS patients admitted to ICU. The study described the characteristics of AIDS patients with respiratory failure caused by pulmonary infections and identified the predictors of ICU mortality.
Methods
We retrospectively reviewed the medical records of all AIDS patients in the ICU of Ditan Hospital (a university-affiliated tertiary referral hospital in Beijing, China) from January 2012 to December 2021. The hospital’s research ethics committee approved the study (No.2018–005-01). All clinical and laboratory data were used anonymously, and written informed consent was not required.
Study Population
All patients over 18 years old with AIDS and respiratory failure admitted to the ICU, either from the emergency department or transferred from medical wards, were included sequentially. HIV infection was either previously known or newly diagnosed. AIDS patients with CD4 count < 200 cells/µL or with clinical AIDS-defining conditions. Those diagnosed within two months before admission to ICU and had not received cART were defined as newly diagnosed HIV infection. Respiratory failure was defined as the partial pressure of arterial oxygen (PaO2) ≤ 60 mmHg on room air or the ratio between PaO2 and inspired oxygen fraction (PaO2/FiO2) ≤ 300 mmHg. Patients who did not have pulmonary infections, accepted invasive mechanical ventilation (IMV) before ICU admission, and had an ICU stay of fewer than 24 hours were excluded. We included patients with respiratory failure caused by pulmonary infections. Pulmonary infections were based on clinical symptoms and abnormalities on computed tomography scan, along with the morphological identification of the organism in induced sputum, low tracheal aspiration or bronchoalveolar lavage fluid if accessible. The samples were cultured for bacteria and fungi. Pneumocystis jirovecii organisms were identified with staining (eg, Giemsa or Gomori-Grocott) or immunofluorescence on specimens.14 CMV DNA was tested using quantitative real-time polymerase chain reaction. What’s more, we did laboratory tests to evaluate for atypical bacterial pathogens like mycoplasma or legionella.
Only the first episode was evaluated in patients with multiple episodes admitted to the ICU for respiratory failure during their hospitalization.
Data Collection
Baseline information was collected at ICU admission, including age, sex, body weight, comorbidity, smoking history, and HIV-related data (last count of CD4 and viral load within three months before ICU admission). The severity of illness at ICU admission was evaluated by Acute Physiological and Chronic Health Status Score (APACHE) II15 and the sequential organ failure assessment (SOFA).16 Clinical and laboratory profiles were collected 24 hours after ICU admission, and the worst values were recorded. Complications newly developed during treatment, including sepsis,17 nosocomial lower respiratory tract infection (NLRTI) and air leaks were also collected.
All intensivists determined the primary etiology of acute respiratory failure. The management of oxygen support included conventional oxygen, high-flow nasal cannula oxygen therapy (HFNC), non-invasive ventilation (NIV) and IMV. The primary outcome was ICU mortality, and the secondary outcomes were hospital mortality, 90-day mortality after ICU admission, and length of ICU and hospitalization.
Statistical Analysis
Patients were divided into two groups, survivors and nonsurvivors, and clinical and laboratory data were compared. The numerical variables were expressed as mean (± standard deviation, SD) or median (interquartile, IQR), according to the Shapiro–Wilk test, and compared using Student’s t-test or Mann–Whitney U-test. Categorical data were expressed as numbers (percentage) and evaluated using the chi-square or Fisher exact test. A two-sided p < 0.05 was considered significant. Key prognostic variables in determining ICU mortality were assessed using multivariate analysis by binary logistic regression model using a stepwise forward method. Variables were measured by the estimated odds ratio (OR) and 95% confidence interval (CI). The Kaplan-Meier curve and Log rank test were used for survival analysis. Data analyses were performed using IBM SPSS Statistics version 22 (SPSS Inc., Chicago, IL, USA).
Results
Patient Characteristics
During the 10-year study period, 283 AIDS adult patients with respiratory failure were admitted to the ICU, of which 52 patients (18.4%) were excluded: 29 patients (55.8%) with respiratory failure not caused by pulmonary infections, 2 patients (3.8%) accepted IMV before ICU admission and 21 patients (40.4%) stayed in ICU less than 24 hours. The final sample consisted of 231 patients (81.6%). Table 1 presents the characteristics of all patients, survivors and nonsurvivors according to the ICU outcome. The mean age of AIDS patients was 41.0 ± 12.1 years and most (95.7%) were male. Comorbidities were detected in 41 patients (17.7%) as follows: hypertension in 19 (46.3%), diabetes in 15 (36.6%), chronic hepatopathy in 10 (24.4%), chronic kidney disease in 3 (7.3%) and cardiac disease in 6 (14.6%). No one had chronic pulmonary disease. Eighty-seven patients (37.7%) were admitted to ICU from the emergency department directly, and the other patients were transferred from medical wards. One hundred and sixty-nine patients (73.2%) were newly diagnosed with HIV infection at ICU admission. Forty-five (19.5%) patients received cART with a median length of 30 days (IQR, 13 days-3 years), and 17 patients (7.4%) did not take cART even though they knew their HIV status. One hundred forty-one patients (61.0%) received tracheal intubation and IMV, 77.3% within 24 hours after ICU admission. IMV subsequently had a median length of 222 (IQR, 114–412) hours.
 |
Table 1 Characteristics of AIDS Patients with Pulmonary Infections Causing Respiratory Failure |
Pulmonary Infections
Pulmonary infections identified are shown in Table 2, including the diagnoses and microbiological profiles of pulmonary infections. There was a total of 277 pulmonary infections identified in 231 patients, the most common being PCP, which was identified in 185 (80.1%) patients. PCP was identified in 143 patients (84.6%) with newly diagnosed HIV infection, in 165 patients (82.1%) with CD4 count ≤ 50 cells/µL, and in 35 patients (77.8%) with cART. Bacterial pneumonia was interpreted by the bacterial isolates collected before ICU admission or within 48 hours after ICU entry and was identified in 26 patients. Two or more etiologies of pulmonary infections were identified in 41 (17.7%) patients. Thirty patients (73.2%) had PCP and other opportunistic pneumonia, 8 patients (19.5%) had PCP and bacterial pneumonia, and 3 patients (7.3%) had PCP, other opportunistic pneumonia and bacterial pneumonia. The distribution of different pulmonary infections in terms of CD4 counts, cART, and diagnosis time of HIV infection is shown in (Figure 1a–c).
 |
Table 2 Causative Diagnoses and Pathogens of Pulmonary Infections in the 231 AIDS Patients |
Patient Outcomes
ICU mortality, hospital mortality and 90-day mortality after ICU admission were 32.9% (76/231), 39.8% (92/231) and 53.2% (123/231), respectively. Figure 2 indicates a downward trend in mortality rates over the 10-year period. A comparison of the characteristics between ICU survivors and nonsurvivors is shown in Table 1. Nonsurvivors had a lower rate of newly diagnosed HIV infection and PCP than survivors (p = 0.037 and p = 0.016). In terms of severity of illness, nonsurvivors were worse in clinical and laboratory data [respiratory rate, heart rate, mean arterial pressure (MAP), PaO2/FiO2 ratio, hemoglobin and albumin], had higher APACHE II and SOFA scores and higher rates of newly developed sepsis and NLRTI. Nonsurvivors had a higher rate of IMV (p = 0.000), a longer time before ICU admission (p = 0.004) than survivors. There were no significant differences in the length of ICU stay between survivors and nonsurvivors. Nonsurvivors had a shorter length of hospitalization (p = 0.020) than survivors.
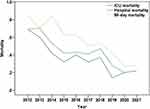 |
Figure 2 Trend of mortality rates in AIDS patients with respiratory failure over the 10-year period. Abbreviation: AIDS, acquired immunodeficiency syndrome. |
ICU mortality, hospital mortality and 90-day mortality after ICU admission of AIDS patients with PCP were 29.2% (54/185), 36.2% (67/185) and 47.6% (88/185), respectively. One hundred and two (55.1%) AIDS patients with PCP required IMV, and the ICU mortality of PCP patients with IMV was 52.9%.
We used multivariate logistic regression analyses to clarify the clinical risk factors for ICU mortality among the 231 AIDS patients with respiratory failure due to pulmonary infections (see Table 3). IMV (OR, 27.910; 95% CI, 8.392–92.818; p = 0.000) and the time before ICU admission (OR, 0.959; 95% CI, 0.920–0.999; p = 0.046) were independently associated with ICU mortality. The Hosmer-Lemeshow test in our multivariate logistic regression analysis model showed it was a good fit (p = 0.401). In the survival analysis, we also found that patients with IMV (Log rank test = 55.130, p = 0.000) and later admission to ICU (Log rank test = 20.825, p = 0.000) had a higher probability of mortality (see Figure 3a and b).
 |
Table 3 Multivariate Analysis of Risk Factors for ICU Mortality in AIDS Patients with Respiratory Failure |
Discussion
This retrospective study focused on the etiology of pulmonary infections causing respiratory failure in AIDS patients admitted to ICU in a tertiary hospital in China over a 10-year period. It provides important insights into critically ill AIDS patients, through the identification of variables influencing prognosis. To our knowledge, this is the first study to analyze the etiology of pulmonary infections causing respiratory failure and their outcome in AIDS patients admitted to ICU in China.
There was a retrospective study focused on etiology and outcomes for patients infected with HIV in this center from January 2009 to October 2013.11 Over the five-year study period, 122 HIV-infected patients admitted to ICU and respiratory failure accounting for 53.4%. In this 10-year retrospective study at the same center from January 2012 to December 2021, we admitted 231 AIDS patients with respiratory failure, which indicates the advances in the treatment of respiratory failure, and positive attitude towards AIDS patients.
In the pre-cART era, opportunistic infections, mainly PCP, have been the leading cause of morbidity and mortality in HIV-infected patients.18,19 The incidence of PCP has declined with advances in the diagnosis, prevention and treatment among patients with HIV infection.20,21 While the incidence decreased, mortality remains high, especially among those who required IMV.8 Retrospective cohort studies have reported mortality rates ranging between 10% and 20% for patients with HIV.22–25 The data in our hospital from August 2009 to January 2018 showed the overall hospital mortality of HIV-infected patients with PCP was 17.3%, and patients in the high-risk group with mortality of 38.78%-81.63%.25 In this cohort, PCP was the leading cause of respiratory failure, followed by other opportunistic pneumonia, with a high rate of newly diagnosed HIV infection and a low rate of cART. As the high mortality rate of PCP with respiratory failure, the use of PCP prophylaxis should be positive, especially in patients with CD4 count < 200 cells/µL.
During the cART era, non-AIDS-associated admission diagnoses were significant. Some studies showed bacterial pneumonia and bacterial sepsis had become the leading reasons for ICU admission and can happen at every stage of HIV infection.2,26 In this study, there was a considerable number of cases of bacterial pneumonia, accounting for 11.3% of all pulmonary infections, which was much less than two other studies (35.3% and 64.9% of infectious etiologies, respectively).2,18 In Orsini’s study, 54.8% of the patients were receiving cART on ICU admission and the median CD4 count were 123 cells/µL.2 In Barbier’s study, the median CD4 count were 192 cells/µL and the rate of newly diagnosed HIV infection was 29.2%.18 Streptococcus pneumoniae was the leading pathogen of bacterial pneumonia, accounting for 20% to 40%.2,27,28 The ratio of streptococcus pneumoniae was less in this study, as bacterial pneumonia was identified by bacterial isolates.
The hospital mortality in HIV-infected patients was 19.7% to 65.9%, related to different etiologies, management and socio-economic conditions.2,18,19 The hospital mortality rate of this cohort was 39.8%, consistent with the result. However, the 90-day mortality rate was much higher than hospital mortality, as some patients were discharged or transferred without consentment while still in critical condition. In the former study, taking all etiologies into account, ICU mortality was 65.9%.11 The ICU mortality in this study was 32.9% and higher than in two other similar studies (10.9% and 31.0%, respectively).2,18 The relatively high mortality in our study may relate to the following reasons. First, patients were unaware of their HIV infection until their first manifestation with dyspnea caused by an opportunistic infection, and the newly diagnosed HIV infection rate was 73.2%. Second, patients did not receive cART even though they knew they had HIV infection, and the rate of cART was 7.4% of previously known HIV infection. What’s more, treatment failure of cART happened due to poor adherence or other causes. We found a downtrend in ICU, hospital, and 90-day mortality rates, which indicated the advance of treatment in AIDS patients with respiratory failure.
In this study, 61% of patients required IMV, and accepted IMV was independently associated with ICU mortality. In a single-center, prospective observational study, 85.1% of all HIV-infected patients with respiratory failure admitted to the ICU required IMV, and increased mortality was observed in that patients.18 In a 10-year retrospective study from January 1999 to June 2009, the mechanical ventilation rate was 60.4% of all HIV-infected patients, and the need for IMV is associated with ICU survival.8 In a retrospective study, in which bacterial pneumonia was the leading cause of respiratory failure in the first decade of cART, IMV was independently associated with ICU mortality.2
Admission to ICU was independently associated with hospital mortality in HIV-infected patients.29,30 We believe that the patients admitted to ICU were mainly for severe illness and needed critical care, which can describe the relationship between ICU admission and mortality. HIV-infected patients should be offered ICU admission if it is likely to benefit them.8 The overall mortality decreased with improved critical care, even without the effects of cART, in severely ill patients admitted to the ICU.21 Intensive care and advanced therapies like IMV and ECMO were only available in ICU. The time before ICU admission was independently associated with mortality in a retrospective study,2 with a higher cART rate of 29.3% and a higher CD4 count lever than our study. In a prospective, observational study, patients from another ward to the ICU had a higher mortality rate than those from the emergency department.31 Patients with HIV infection, even at late stages, should be considered for referral to ICU as early as possible if they need critical care.
IMV and the time before ICU admission were independent predictors of ICU mortality. If AIDS patients with respiratory failure were admitted to ICU earlier and provided advanced respiratory support like HFNC or NIV to avoid IMV, the prognosis may change.
Several limitations should be considered when interpreting the results. First, the retrospective observational data of the study has inherent biases, and the single-center nature of the study limits its generalizability. Second, the data was collected over a long period, and fluctuations in diagnosis and treatment existed. Third, as bacterial isolates identified bacterial pneumonia, blood cultures and urinary antigen tests were not carried out, we may underestimate its incidence and power on mortality.
Conclusion
PCP was the primary etiology for respiratory failure in AIDS patients admitted to the ICU. Respiratory failure remains a severe illness with high mortality, and ICU mortality was negatively associated with IMV and later admission to ICU.
Data Sharing Statement
The dataset consisting of de-identified participants’ data is available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This retrospective study was approved by the Ethics Committee of Beijing Ditan Hospital, Capital Medical University, No. 2018-005-01, on March 1, 2018, and complies with the principles of the Declaration of Helsinki. The Ethics Committee of Beijing Ditan Hospital waived the need for specific informed consent for this retrospective study.
Acknowledgments
We acknowledge the work of HIV health care providers for their diagnosis, nursing and treatment of patients with HIV/ AIDS in Beijing Ditan Hospital.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Capital Development Special Program of Beijing Hospital Authority, China (NO. 2018-1-2171). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Barbier F, Mer M, Szychowiak P, et al. Management of HIV-infected patients in the intensive care unit. Intensive Care Med. 2020;46(2):329–342. doi:10.1007/s00134-020-05945-3
2. Barbier F, Coquet I, Legriel S, et al. Etiologies and outcome of acute respiratory failure in HIV-infected patients. Intensive Care Med. 2009;35(10):1678–1686. doi:10.1007/s00134-009-1559-4
3. Chiang HH, Hung CC, Lee CM, et al. Admissions to intensive care unit of HIV-infected patients in the era of highly active antiretroviral therapy: etiology and prognostic factors. Crit Care. 2011;15(4):R202. doi:10.1186/cc10419
4. Nickas G, Wachter RM. Outcomes of intensive care for patients with human immunodeficiency virus infection. Arch Intern Med. 2000;160(4):541–547. doi:10.1001/archinte.160.4.541
5. Barbier F, Roux A, Canet E, et al. Temporal trends in critical events complicating HIV infection: 1999–2010 multicentre cohort study in France. Intensive Care Med. 2014;40(12):1906–1915. doi:10.1007/s00134-014-3481-7
6. Powell K, Davis JL, Morris AM, Chi A, Bensley MR, Huang L. Survival for patients With HIV admitted to the ICU continues to improve in the current era of combination antiretroviral therapy. Chest. 2009;135(1):11–17. doi:10.1378/chest.08-0980
7. Benito N, Moreno A, Miro JM, Torres A. Pulmonary infections in HIV-infected patients: an update in the 21st century. Eur Respir J. 2012;39(3):730–745. doi:10.1183/09031936.00200210
8. Adlakha A, Pavlou M, Walker DA, et al. Survival of HIV-infected patients admitted to the intensive care unit in the era of highly active antiretroviral therapy. Int J STD AIDS. 2011;22(9):498–504. doi:10.1258/ijsa.2011.010496
9. Casalino E, Wolff M, Ravaud P, Choquet C, Bruneel F, Regnier B. Impact of HAART advent on admission patterns and survival in HIV-infected patients admitted to an intensive care unit. AIDS. 2004;18(10):1429–1433. doi:10.1097/01.aids.0000131301.55204.a7
10. Narasimhan M, Posner AJ, DePalo VA, Mayo PH, Rosen MJ. Intensive care in patients with HIV infection in the era of highly active antiretroviral therapy. Chest. 2004;125(5):1800–1804. doi:10.1378/chest.125.5.1800
11. Xiao J, Zhang W, Huang Y, et al. Etiology and outcomes for patients infected with HIV in intensive care units in a tertiary care hospital in China. J Med Virol. 2015;87(3):366–374. doi:10.1002/jmv.24063
12. Nirappil FJ, Maheshwari A, Andrews J, Martin GS, Esper AM, Cribbs SK. Characteristics and outcomes of HIV-1-infected patients with acute respiratory distress syndrome. J Crit Care. 2015;30(1):60–64. doi:10.1016/j.jcrc.2014.10.020
13. Elabbadi A, Pichon J, Visseaux B, et al. Respiratory virus-associated infections in HIV-infected adults admitted to the intensive care unit for acute respiratory failure: a 6-year bicenter retrospective study (HIV-VIR study). Ann Intensive Care. 2020;10:123. doi:10.1186/s13613-020-00738-9
14. Thomas CF, Limper AH. Pneumocystis pneumonia. N Engl J Med. 2004;350(24):2487–2498. doi:10.1056/NEJMra032588
15. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. doi:10.1097/00003246-198510000-00009
16. Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–710. doi:10.1007/BF01709751
17. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
18. Orsini J, Ahmad N, Butala A, et al. Etiology and outcome of patients with HIV infection and respiratory failure admitted to the intensive care unit. Interdiscip Perspect Infect Dis. 2013;2013:732421. doi:10.1155/2013/732421
19. Xiao J, Du S, Tian Y, Su W, Yang D, Zhao H. Causes of death among patients infected with HIV at a tertiary care hospital in china: an observational cohort study. AIDS Res Hum Retroviruses. 2016;32(8):782–790. doi:10.1089/aid.2015.0271
20. Morris A, Wachter RM, Luce J, Turner J, Huang L. Improved survival with highly active antiretroviral therapy in HIV-infected patients with severe Pneumocystis carinii pneumonia. AIDS. 2003;17(1):73–80. doi:10.1097/00002030-200301030-00010
21. Miller RF, Allen E, Copas A, Singer M, Edwards SG. Improved survival for HIV infected patients with severe Pneumocystis jirovecii pneumonia is independent of highly active antiretroviral therapy. Thorax. 2006;61(8):716–721. doi:10.1136/thx.2005.055905
22. Mansharamani NG, Garland R, Delaney D, Koziel H. Management and outcome patterns for adult Pneumocystis carinii pneumonia, 1985 to 1995: comparison of HIV-associated cases to other immunocompromised states. Chest. 2000;118(3):704–711. doi:10.1378/chest.118.3.704
23. Kelley CF, Checkley W, Mannino DM, Franco-Paredes C, Del Rio C, Holguin F. Trends in hospitalizations for AIDSassociated Pneumocystis jirovecii pneumonia in the United States (1986 to 2005). Chest. 2009;136(1):190–197. doi:10.1378/chest.08-2859
24. Walzer PD, Evans HE, Copas AJ, Edwards SG, Grant AD, Miller RF. Early predictors of mortality from Pneumocystis jirovecii pneumonia in HIV-infected patients: 1985–2006. Clin Infect Dis. 2008;46(4):625–633. doi:10.1086/526778
25. Wu L, Zhang Z, Wang Y, et al. A model to predict in-hospital mortality in HIV/AIDS patients with pneumocystis pneumonia in China: the clinical practice in real world. Biomed Res Int. 2019;2019:6057028. doi:10.1155/2019/6057028
26. Azoulay É, de Castro N, Barbier F. Critically ill patients with HIV: 40 years later. Chest. 2020;157(2):293–309. doi:10.1016/j.chest.2019.08.002
27. Cilloniz C, Torres A, Polverino E, et al. Community-acquired lung respiratory infections in HIV-infected patients: microbial aetiology and outcome. Eur Respir J. 2014;43(6):1698–1708. doi:10.1183/09031936.00155813
28. Segal LN, Methe BA, Nolan A, et al. HIV-1 and bacterial pneumonia in the era of antiretroviral therapy. Proc Am Thorac Soc. 2011;8(3):282–287. doi:10.1513/pats.201006-044WR
29. Silva DR, Menegotto DM, Schulz LF, Gazzana MB, Dalcin PT. Mortality among patients with tuberculosis requiring intensive care: a retrospective cohort study. BMC Infect Dis. 2010;10:54. doi:10.1186/1471-2334-10-54
30. Perelló R, Escoda O, Camón S, et al. Changes in the etiology, incidence and prognosis of acute lower respiratory track infections in human immunodeficiency virus patients. Enferm Infecc Microbiol Clin. 2015;33(4):243–247. doi:10.1016/j.eimc.2014.06.002
31. Afessa B, Green B. Clinical course, prognostic factors, and outcome prediction for HIV patients in the ICU. The PIP (Pulmonary complications, ICU support, and prognostic factors in hospitalized patients with HIV) study. Chest. 2000;118(1):138–145. doi:10.1378/chest.118.1.138
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


