Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Public Attitudes Towards Lung Cancer Screening in Saudi Arabia: A Cross-Sectional Study
Authors Dairi MS , Bahakeem B
Received 22 April 2023
Accepted for publication 1 August 2023
Published 14 August 2023 Volume 2023:16 Pages 2279—2289
DOI https://doi.org/10.2147/JMDH.S418296
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mohammad S Dairi, Basem Bahakeem
Department of Medicine, College of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia
Correspondence: Mohammad S Dairi, Department of Medicine, College of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia, Tel +966555501560, Email [email protected]
Objective: Lung cancer is one of the leading causes of death worldwide, and it is ranked as the first cause of death in more than 100 countries around the world. The aim of this study was to explore the knowledge and attitude of the general population in Saudi Arabia toward lung cancer screening.
Methods: A cross-sectional study employing an online survey was conducted between November 2021 and February 2022 in Saudi Arabia. This study utilized a previously developed questionnaire instrument. Logistic regression was used to identify predictors of positive attitude toward lung cancer screening.
Results: A total of 473 participants were involved in this study. The majority of the study participants (74.6%) reported that they are current smokers. Almost 31.5% of the study participants reported that if lung cancer is detected early, the person’s chance of surviving is poor to very poor. The majority of the study participants reported that they would be willing to do tests to diagnose lung cancer if you were invited by the Ministry of Health or their doctor. Males, participants aged (24– 34 years), and current smokers were more likely to have positive attitude towards lung cancer screening (p ≤ 0.05). On the other hand, patients aged 46 years and over and those with higher education had less positive attitude towards lung cancer screening (p ≤ 0.05).
Conclusion: This is the first study to look into the general public’s attitudes toward lung cancer screening in Saudi Arabia. According to our findings, the majority of people believe that early detection of lung cancer can lead to improved results and have a favourable attitude toward lung cancer screening if it is indicated. Thus, incorporating lung cancer screening into the local guidelines in at-risk population is highly recommended and considering the launch of nation-wide lung cancer screening program is advised.
Keywords: cancer, lung, screening, smokers
Introduction
Lung cancer is one of the most common types of cancer worldwide.1 It is regarded as a major public health concern and it also causes a heavy burden on the healthcare system and the economy.2 According to the WHO, in 2020, there were around 2.21 million cases of lung cancer worldwide.1 In Saudi Arabia lung cancer is the fifth most common type of cancer in male in Saudi Arabia, while it is the 17th most common type of cancer among females in Saudi Arabia.3 A previous epidemiological study that analyzed data from the Saudi cancer registry reported that the age standardized incidence rate of lung cancer in Saudi Arabia ranged from 1.2 to 12.3 per 100,000 cases in different regions of Saudi Arabia.4 However, this number is also expected to increase with the ongoing aging and growth of the Saudi population, making it a major public health concern. A previous study in Saudi Arabia found that the median duration of survival for patients with small cell lung carcinoma was 6.4 months.5
Lung cancer is one of the leading causes of death worldwide, and it is ranked as the first cause of death in more than 100 countries around the world.6 The five-year survival rate of lung cancer is only around 14%,7 however, when it is diagnosed at early age, the overall survival rate will increase in around 50% of the patients, nevertheless, only small percentage of patients are diagnosed at early stage.8,9 The majority of cases of lung cancer are tobacco related, and only around 10% of lung cancer are not related to tobacco.3
Despite that smoking is the major risk factor for lung cancer, there are other risk factors that can increase the risk of lung cancer including occupational exposures, respiratory disease, and a family history of lung cancer.10 Smoking cessation is also a major contributing factor that decreases lung cancer incidence.11 Therefore, major international and national guidelines offer strong recommendations regarding smoking cessations.12
For many years, there have been uncertainties about the advantages of lung cancer screening programs and whether they can reduce the mortality rate of lung cancer.13 In the last few years, there has been some interest worldwide in lung cancer screening programs using a low dose of computed tomography (LDCT). The National Lung Screening Trial (NLST) has demonstrated that screening for lung cancer among high-risk populations may decrease the risk of mortality by 20%.13–15 However, in Saudi Arabia, there are no current recommended screening programs for lung cancer, this includes the national guidelines by the Saudi Lung Cancer Association (SLCA) and Saudi National Cancer Centre.12 However, these guidelines provide guidance for health care professionals who are seeking further investigations among high-risk populations.
Previous study in Taiwan found that the utilization of LDCT screening in non-smoking population is increasing.16 Wu, F. Z., and Chang, Y. C. reported that in the future, lung cancer screening programs targeting non-smokers could have a significant prognostic impact on health promotion in Asian nations.17 In the future, it will be crucial to effectively encourage smokers to participate in lung cancer screening programs through financial incentives and pedagogical training.18 Previous studies investigating the attitude and perceptions of the public towards lung cancer screening focused mainly on the smoking population and the older age group,19–22 with limited studies on the general population who is also at risk of lung cancer and can benefit from future lung screening programs. In addition, no previous study investigated the attitudes and perceptions of the public toward lung cancer. Therefore, in this cross-sectional online survey, we aimed to explore the knowledge and attitude of the general population in Saudi Arabia toward lung cancer screening. There are a number of ways to emphasize the importance of international and national guidelines in regard to how the general public views lung cancer screening. These include the use of targeted awareness campaigns, sharing personal accounts of people whose lives have been improved by following the recommendations for lung cancer screening, ensuring that the recommendations are communicated in plain language, avoiding medical jargon to the greatest extent possible, and working with media outlets and social media influencers to share accurate and evidence-based information.
Method
Study Design
Between November 2021 and February 2022, a cross-sectional study employing an online survey was done in Saudi Arabia to examine the general population’s knowledge and attitude regarding lung cancer screening.
Study Population and Recruitment
Using convenience sampling technique, eligible subjects were invited to participate in the study. Social media platforms (Facebook and WhatsApp) were utilized to reach out to the general public and invite them to participate in this study. All subjects supplied their informed consent freely; consequently, written consent was not required. Detailed descriptions of the study’s aims and objectives were provided at the outset of the survey.
The inclusion criteria required participants to be at least 18 years old and to be currently residing in Saudi Arabia. Participants who were under 18 or who could not read or understand Arabic were not permitted to participate.
Study Tool
This study utilized a self-administered questionnaire instrument created by Quaife et al.23 There were two sections containing 19 questions in total. The demographics of the participants were covered in the first section, which consisted of nine questions regarding age, gender, education level, employment status, smoking status, whether they know someone with cancer from their family or friends, and their confidence in their ability to quit smoking. The second half of the questionnaire comprised ten 5-point Likert scale and yes/no questions that investigated the beliefs and concerns of participants regarding lung cancer.
Piloting Phase
Clinicians from the college of medicine at Umm Al-Qura University assessed and confirmed the questionnaire instrument. They were asked about the clarity, comprehensibility, and face validity of the questions, as well as whether any were difficult to understand. Additionally, they were asked about any questions they considered disrespectful or annoying. They commented that the questionnaire was straightforward to understand and complete. In addition, a pilot research was done with a small group of individuals who met the inclusion criteria in order to check comprehension prior to using the questionnaire on a larger scale; the results confirmed that it is simple and uncomplicated.
Translation Procedure
The original survey tool was translated into Arabic using the forward-backward technique. This technique involved the translation of three independent clinicians who are bilingual. The translation focused on preserving the context of the items of the survey rather than word-by-word translation.
Sample Size
Using a confidence interval (CI) of 95%, a standard deviation (SD) of 0.5, and an error margin of 5%, the minimum sample size required was 385 individuals.
Statistical Analysis
Using descriptive statistics, the demographic characteristics of the individuals were described. Percentages were reported for categorical data (frequencies). Logistic regression was used to calculate the odds ratios (ORs) and 95% CI for those who are more likely to have a positive attitude toward lung cancer screening. For logistic regression, the dummy variable was established as any participant who affirmed a desire to undergo lung cancer diagnostic tests if invited by the Ministry of Health or treating physician.
Results
Participants’ Demographic Characteristics
A total of 473 participants were involved in this study. Males comprised more than half (77.6%) of the study sample. Around one-third (27.7%) of the study participants were aged 30–34 years. More than half of them (59.6%) were married, hold bachelor degree (69.6%), and work outside the healthcare sector (65.5%). Almost half of the study sample (49.5%) reported that their monthly income is 7500 Saudi Riyal (SAR) and over. Around 46.0% of the study participants reported that they know someone from family or friends who has cancer. The majority of the study participants (74.6%) reported that they are current smokers. Almost half of the study participants (50.7%) showed high levels of confidence (answered extremely high, very high, or high) that they have the ability to stop smoking. For further details on the demographic characteristics of the study participants refer to Table 1.
 |
Table 1 Participants’ Demographic Characteristics |
Beliefs and Worry About Lung Cancer
Almost one-fifth of the study participants showed agreement that diagnosis of cancer is a death sentence and the percentage was even higher for lung cancer specifically (31.6%), Figure 1. Almost 31.5% of the study participants reported that if lung cancer is detected early, the person’s chance of surviving is poor to very poor. More than half of the study participants (55.6%) showed positive attitude (answered yes probably or yes definitely) towards doing recommended surgery if the screening test found that they had early-stage lung cancer. Almost one-fifth of the study participants (22.0%) reported that they worry (answered frequently or always) about their chance of getting lung cancer.
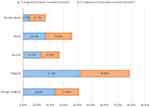 |
Figure 1 Perception of cancer and lung cancer. |
The majority of the study participants (77.2%) reported that clear computed tomography (CT) scan would reassure them. The majority of the study participants reported that they would be willing to do tests to diagnose lung cancer if they were invited by the Ministry of Health or their doctor with 78.0% and 81.2%, respectively, Figure 2. For further details on participants’ beliefs and worry about lung cancer refer to Table 2.
 |
Table 2 Participants’ Beliefs and Worry About Lung Cancer |
 |
Figure 2 Attitudes and beliefs towards lung cancer screening. |
Predictors of Positive Attitude Towards Lung Cancer Screening
Binary logistic regression analysis identified that males (p-value≤0.001), participants aged (30–34 years) (p-value=0.042), and current smokers (p-value=0.012) were more likely to have positive attitude towards lung cancer screening, Table 3. On the other hand, patients aged 46 years and over (p-value≤0.001) and those with higher education (p = 0.009) had less positive attitude towards lung cancer screening.
 |
Table 3 Predictors of Positive Attitude Towards Lung Cancer Screening |
Discussion
This cross-sectional online survey aimed to explore the attitude of the general population in Saudi Arabia toward lung cancer screening. The main finding of this study showed that the majority of the study participants reported that early detection of lung cancer can have better outcomes. In addition, most of the study participants reported a good attitude regarding lung screening programs for the detection of lung cancer, and that clear computed tomography (CT) scan would reassure them.
Cancer is the leading cause of death worldwide and every year, and there were more than 10 million deaths due to cancer in 2020 worldwide.1 A study in the United States (U.S) that analyzed data of 7674 adults between 2007 and 2008 of the nationally representative Health Information National Trends Survey, showed that 61.6% of respondents perceived cancer as death sentence.24 In this study, one-fifth of the study participants showed agreement that diagnosis of cancer is a death sentence, and the percentage was even higher for lung cancer specifically. These percentages were also consistent with a previous study in the UK that included around 1400 participants.23 These thoughts of death are alarming and may raise concern about the knowledge of the public about survival rates and the management of cancer as some people may be discouraged from seeking help if they believe that cancer is a death sentence. This was also reported in a previous study where the authors concluded that people who had negative beliefs about lung cancer are more likely to avoid lung screening.19 However, this study also showed that the majority of the study participants reported that early detection of lung cancer can have better outcomes. This was also in line with a previous study in the UK, where the majority reported that early detection of lung cancer has the potential to save lives.25 It is well known that early detection of cancer is associated with better outcomes.26 In addition, in Saudi Arabia several awareness programs are conducted yearly across the country to raise the awareness and knowledge about the risk of lung cancer and to promote smoking cessation.27,28
Our data showed that the majority of the study participants (86%) reported positive attitude regarding lung screening programs for the detection of lung cancer, and the majority of the study participants (83.7%) also think that lung cancer screening is a good idea. In addition, in this study, the majority of the study participants (77.2%) reported that clear computed tomography (CT) scan would reassure them. These results are similar to a previous study in the U.S and the UK where most of the study sample in both studies reported that they are willing to undergo lung cancer screening if it was recommended by their physician.20,25 According to a previous study conducted in the UK, there may be substantial obstacles to the successful implementation of a lung cancer screening program that targets tobacco smokers.22 In addition, current smokers were less likely than never smokers to assume that early detection would result in a favourable prognosis for survival. Smokers were 52.0% less inclined to consider lung cancer screening with computed tomography.22 Prior research has demonstrated that Asian non-smokers are eager to participate in lung cancer screenings. These difference could be justified due to the differences among difference study populations. Sources of differences could be having smoking stigma, different socioeconomic status, and other factors such as perceived invulnerability and dread and avoidance.16–18
The cost of medical care can serve as a potential barrier to the willingness to screen for lung cancer, this was highlighted in a previous study in the U.S.29 However, in Saudi Arabia, health care services are provided for the Saudi population free of charge and this might explain the positive attitude among our study sample toward lung cancer screening. Further research is warranted to examine the impact of free of charge healthcare on public attitude towards cancer screening program.
In previous study, they also found that higher educational level is associated with positive attitude toward lung cancer screening. This was reported in a previous systematic review that included more than 1000 articles and showed that women with the highest level of education were more likely to have screenings.30 This was different from our study findings, which found that individuals with higher education were less likely to have positive attitude towards lung cancer screening. There may be a number of reasons why people with higher levels of education may have a less positive attitude toward lung cancer screening, including critical thinking and risk perception, which may cause people to scrutinize and question the evidence and efficacy of certain screening programs and having a more accurate perception of their own personal risk factors for lung cancer (if they believe they have low levels of risk). Additionally, some individuals with higher levels of education may prioritize other cancer prevention and early detection techniques, such as quitting smoking or maintaining a healthy diet, above screening, which might result in a less favourable attitude toward screening programs.
There are advantages and disadvantages to lung cancer screening. According to the National Lung Screening Trial, one in 320 high-risk patients who undergo low-dose CT screening over a five-year period will not get lung cancer.31 But no other research has demonstrated an advantage from this screening. A substantial percentage of low-dose CT scans are false-positive. Of 1,000 high-risk individuals without cancer, 250 will have an abnormal low-dose CT result and need additional testing to rule it out; 2.5% of cancer-free patients will have invasive procedures (such as lung biopsies and bronchoscopies), which carry a minor risk of complications and mortality.31 At least 20% of the tumors detected by low-dose CT are over-diagnosed, meaning they would not have affected the patient if left untreated. Over-diagnosed lung cancer patients will be subjected to possibly harmful and life-threatening procedures with little benefit.31
It is worth mentioning that the implementation of a national lung cancer screening program faces a number of obstacles and difficulties, including the need to raise the necessary funds, the need for a strong healthcare infrastructure and resources, the need for developing precise and useful risk assessment criteria in order to identify individuals who would benefit from screening, and the need for high levels of patient compliance and follow-up.
This study is the first study to explore the attitude of the general population in Saudi Arabia toward lung cancer screening. Our study results highlight the positive attitude toward lung cancer screening, and this could serve as an initial step in a national-level plan in dealing with lung cancer. Awareness campaign should target females and those aged 46 years and over due to their less favourable attitude towards lung cancer screening. Future studies developing effective interventions to enhance public awareness and attitude towards lung cancer screening program are warranted. In addition, future cost-effectiveness studies may be needed to better understand the need to implement new policies regarding lung cancer screening. However, this study has several limitations, first, the findings may not be generalized to the entire population as we have conducted an online survey. In addition, the study’s findings were based on survey data, which means that, like any other cross-sectional study, the results cannot be used to infer causality. The use of convenience sampling technique is not free from criticism, as the generalisability of the study findings could be affected due to missing some of the targeted population (those who do not use social media website) due to potential sampling bias.
Conclusion
This study is the first study to explore the attitude of the general population in Saudi Arabia toward lung cancer screening. Our study found that the majority believe that early detection of lung cancer can have better outcomes and showed a positive attitude toward lung cancer screening if recommended. Thus, incorporating lung cancer screening into the local guidelines in at-risk population is highly recommended and considering the launch of nation-wide lung cancer screening program is advised. Given that females and people over 46 have a less favourable attitude towards lung cancer screening, these groups should be the focus of awareness campaigns.
Data and Materials Availability
All data for this study were analysed and presented in the manuscript.
Institutional Review Board Statement
This study was approved by the Research ethics Committee at Umm Al-Qura University, Makkah, Saudi Arabia (Ref: HAPO-02-K-012-2022-11-1361). Informed consent was obtained from all subjects involved in the study. All procedures comply with the principles of Helsinki Declaration.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received for this study.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. World Health Organization. Cancer; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/cancer.
2. Zhang J, Li J, Xiong S, et al. Global burden of lung cancer: implications from current evidence. Ann Cancer Epidemiol. 2021;5:56.
3. Health, S.M.o. Lung Cancer; 2022. Available from: https://www.moh.gov.sa/en/awarenessplateform/ChronicDisease/Pages/LungCancer.aspx.
4. Almatroudi A. A Retrospective Cohort Study of Lung Cancer Incidences and Epidemiological Analysis in Saudi Arabian Population from 2006-2016. Int J Environ Res Public Health. 2021;18(22):11827. doi:10.3390/ijerph182211827
5. Alhejaili F, Al-Hajeili M, Bakhsh SI, et al. Survival of Patients with Small Cell Lung Cancer in King Abdulaziz University Hospital, Jeddah. Saudi Arabia Cureus. 2020;12(1):1–5.
6. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
7. Jemal A, Murray T, Samuels A, et al. Cancer statistics, 2003. CA Cancer J Clin. 2003;53(1):5–26. doi:10.3322/canjclin.53.1.5
8. Walters S, Maringe C, Coleman MP, et al. Lung cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the UK: a population-based study, 2004-2007. Thorax. 2013;68(6):551–564. doi:10.1136/thoraxjnl-2012-202297
9. Quaife SL, Marlow LAV, McEwen A, et al. Attitudes towards lung cancer screening in socioeconomically deprived and heavy smoking communities: informing screening communication. Health Expectations. 2017;20(4):563–573. doi:10.1111/hex.12481
10. Malhotra J, Malvezzi M, Negri E, et al. Risk factors for lung cancer worldwide. Eur Respir J. 2016;48(3):889–902. doi:10.1183/13993003.00359-2016
11. Su Z, Jia XH, Zhao FH, et al. Effect of Time Since Smoking Cessation on Lung Cancer Incidence: an Occupational Cohort With 27 Follow-Up Years. Front Oncol. 2022;12:817045.
12. Jazieh AR, AlGhamdi M, AlGhanem S, et al. Saudi lung cancer prevention and screening guidelines. Ann Thorac Med. 2018;13(4):198–204. doi:10.4103/atm.ATM_147_18
13. Field JK, Vulkan D, Davies MPA, et al. Lung cancer mortality reduction by LDCT screening: UKLS randomised trial results and international meta-analysis. Lancet Reg Health Eur. 2021;10:100179. doi:10.1016/j.lanepe.2021.100179
14. de Koning HJ, van der Aalst CM, de Jong PA, et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N Engl J Med. 2020;382(6):503–513. doi:10.1056/NEJMoa1911793
15. Team A, R. D, Adams AM, et al.; National Lung Screening Trial Research. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409.
16. Wu FZ, Huang YL, Wu CC, et al. Assessment of Selection Criteria for Low-Dose Lung Screening CT Among Asian Ethnic Groups in Taiwan: from Mass Screening to Specific Risk-Based Screening for Non-Smoker Lung Cancer. Clin Lung Cancer. 2016;17(5):e45–e56. doi:10.1016/j.cllc.2016.03.004
17. Wu FZ, Chang YC. Toward More Effective Lung Cancer Risk Stratification to Empower Screening Programs for the Asian Nonsmoking Population. J Am Coll Radiol. 2023;20(2):156–161. doi:10.1016/j.jacr.2022.10.010
18. Wu FZ, Wu YJ, Chen CS, Yang SC. Impact of Smoking Status on Lung Cancer Characteristics and Mortality Rates between Screened and Non-Screened Lung Cancer Cohorts: real-World Knowledge Translation and Education. J Personalized Med. 2022;12(1):1–10. doi:10.3390/jpm12010026
19. Smits SE, McCutchan GM, Hanson JA, et al. Attitudes towards lung cancer screening in a population sample. Health Expect. 2018;21(6):1150–1158. doi:10.1111/hex.12819
20. Jonnalagadda S, Bergamo C, Lin JJ, et al. Beliefs and attitudes about lung cancer screening among smokers. Lung Cancer. 2012;77(3):526–531. doi:10.1016/j.lungcan.2012.05.095
21. Carter-Harris L, Ceppa DP, Hanna N, et al. Lung cancer screening: what do long-term smokers know and believe? Health Expectations. 2017;20(1):59–68. doi:10.1111/hex.12433
22. Silvestri GA, Nietert PJ, Zoller J, et al. Attitudes towards screening for lung cancer among smokers and their non-smoking counterparts. Thorax. 2007;62(2):126–130. doi:10.1136/thx.2005.056036
23. Quaife SL, Vrinten C, Ruparel M, et al. Smokers’ interest in a lung cancer screening programme: a national survey in England. BMC Cancer. 2018;18(1):497. doi:10.1186/s12885-018-4430-6
24. Moser RP, Arndt J, Han PK, et al. Perceptions of cancer as a death sentence: prevalence and consequences. J Health Psychol. 2014;19(12):1518–1524. doi:10.1177/1359105313494924
25. Monu J, Triplette M, Wood DE, et al. Evaluating Knowledge, Attitudes, and Beliefs About Lung Cancer Screening Using Crowdsourcing. Chest. 2020;158(1):386–392.
26. World Health Organization. Promoting Cancer Early Diagnosis; 2022. Available from: https://www.who.int/activities/promoting-cancer-early-diagnosis.
27. Ministry of Health. Health Days; 2022. Available from: https://www.moh.gov.sa/en/HealthAwareness/healthDay/2020/Pages/HealthDay-2020-11-01-30.aspx.
28. Ministry of Health. Anti Smoking Clinics; 2022. Available from: https://www.moh.gov.sa/en/Ministry/Projects/TCP/Pages/default.aspx.
29. Sheppard RS, Beale S, Joseph J, et al. Potential barriers to lung cancer screening in a minority population: assessing attitudes, beliefs, and values towards screening with low-dose computed tomography amongst a high-risk minority population. J Clin Oncol. 2021;39(28_suppl):17. doi:10.1200/JCO.2020.39.28_suppl.17
30. Damiani G, Basso D, Acampora A, et al. The impact of level of education on adherence to breast and cervical cancer screening: evidence from a systematic review and meta-analysis. Prev Med. 2015;81:281–289. doi:10.1016/j.ypmed.2015.09.011
31. Lazris A, Roth AR. Lung Cancer Screening: pros and Cons. Am Fam Physician. 2019;99(12):740–742.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
