Back to Journals » Clinical Ophthalmology » Volume 16
Psychosocial Impact of Demodex Blepharitis
Authors O’Dell L, Dierker DS , Devries DK , Garlich J , Whitley WO, Holdbrook M , Baba SN , Yeu E
Received 13 June 2022
Accepted for publication 23 August 2022
Published 2 September 2022 Volume 2022:16 Pages 2979—2987
DOI https://doi.org/10.2147/OPTH.S374530
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Leslie O’Dell,1 Damon S Dierker,2 Douglas K Devries,3 Jaclyn Garlich,4 Walter O Whitley,5 Mark Holdbrook,6 Stephanie N Baba,6 Elizabeth Yeu5
1Medical Optometry America, Shrewsbury, PA, USA; 2Eye Surgeons of Indiana, Indianapolis, IN, USA; 3Eye Care Associates of Nevada, Sparks, NV, USA; 4Envision Optometry, Boston, MA, USA; 5Virginia Eye Consultants, Norfolk, VA, USA; 6Tarsus Pharmaceuticals, Inc, Irvine, CA, USA
Correspondence: Elizabeth Yeu, Virginia Eye Consultants, 241 Corporate Boulevard, Suite 210, Norfolk, VA, 23502, USA, Tel +1 757 793 4942, Fax +1 757 319 2493, Email [email protected]
Purpose: To evaluate the impact of Demodex blepharitis on patients’ daily activities and quality of life.
Patients and Methods: In this multicenter, observational, prospective, IRB-approved study, 311 Demodex blepharitis patients aged ≥ 18 years were included. Demodex blepharitis was diagnosed based on the presence of ≥ 1.0 mite per lash (upper and lower eyelids combined), > 10 collarettes on the upper lashes, and at least mild lid margin erythema of the upper eyelid in at least one eye. All patients were asked to complete a questionnaire about their symptoms, daily activities, quality of life, and management approaches, and descriptive statistics were used to analyze the responses.
Results: More than half the patients had been experiencing symptoms of blepharitis for ≥ 4 years. The three most frequent and bothersome symptoms experienced by patients were dry eyes, itchiness, and irritation. Nearly half the patients (47%) responded that they were conscious of their eyes all day, and 23% said that they were constantly worrying about their eyes. Other activities that were negatively affected included difficulty driving at night (47%), additional time needed for daily hygiene routine (30%), and difficulty in wearing eye make-up (in 34% of females). While all subjects had objective signs of Demodex blepharitis confirmed by an eye care provider, 58% said they had never previously been diagnosed with blepharitis. The most commonly used management approaches for Demodex blepharitis were artificial tears (47%), warm compresses (32%), and lid wipes (14%).
Conclusion: Demodex blepharitis has a significant negative impact on daily activities and the mental and physical well-being of afflicted patients.
Keywords: Demodex blepharitis, dry eye disease, collarettes, cylindrical dandruff, Demodex mites, lid margin disease
Introduction
Demodex blepharitis is a condition that is commonly encountered in eye care practices.1 A high prevalence of Demodex blepharitis, ranging from 41% to 70%, has been reported worldwide.2–7 Two recent US studies have reported Demodex infestation rates of 55% and 58% based on the detection of mites following lash epilation or presence of collarettes (cylindrical dandruff), respectively, among patients presenting for eye examinations for varying reasons.8,9 Since approximately 45 million US patients visit eye care professionals annually; it is estimated that 25 million Americans may have Demodex blepharitis.10,11
Despite the high prevalence of Demodex blepharitis, patients with the condition may go undiagnosed or misdiagnosed for years. This may be due to the substantial overlap of symptoms with dry eye disease (DED) and other ocular surface or lid margin disorders, as well as a general lack of awareness among eye care professionals to actively look for collarettes (waxy, translucent, solidified excretions that form a cylindrical collar around the base of the eyelash follicle), the pathognomonic sign of Demodex blepharitis.9,12–14 These can be readily identified by asking patients to look down during a standard slit-lamp examination.12,15 Even when Demodex blepharitis is diagnosed, inconsistent and typically suboptimal efficacy with over-the-counter and other management options and the absence of an FDA-approved prescription therapeutic disincentivizes treatment. When the underlying cause goes untreated, the immune-mediated inflammatory processes associated with chronic Demodex blepharitis are detrimental to the eyelid and ocular surface health, presenting as itchy, irritated, and dry eyes, fluctuating and blurred vision, lid and lash abnormalities, ocular surface inflammation, noticeable eye and eyelid erythema, and contact lens intolerance and reduced wear time.15–22
We hypothesized that the persistent burden of blepharitis symptoms may also worsen and negatively affect patients’ quality of life and may have an impact on health care system resource utilization. To our knowledge, the burden of Demodex blepharitis on afflicted patients has not been well characterized. In the present study, a large dataset of patients with confirmed Demodex blepharitis was analyzed to better understand the impact of the disease on daily activities and quality of life.
Materials and Methods
In this multicenter, observational, prospective study, adult Demodex blepharitis patients from eight US ophthalmic and optometric centers (Appendix A) were examined clinically and asked questions about their symptoms, daily activities, quality of life and management approaches. The study was conducted in compliance with the study protocol and followed the tenets of the Declaration of Helsinki and its amendments. Institutional review board (IRB) approval was secured for all sites from Alpha Independent Review Board (San Clemente, CA) and all patients provided written informed consent using the IRB-approved informed consent forms.
Demodex blepharitis was diagnosed based on the presence of all of the following signs of Demodex blepharitis in at least one eye: (1) ≥1.0 mite per lash (upper and lower eyelids combined); (2) >10 collarettes on the upper lashes and (3) at least mild lid margin erythema of the upper eyelid. Mite density was assessed by selecting and removing two or more lashes from each of the upper and lower eyelids, one lash from each medial and lateral half of each lid, using fine forceps. If present, lashes with collarettes were targeted for epilation. Targeted lashes were gently rotated using the Mastrota technique and then extracted.23,24 The lashes from each lid were separately placed in artificial tear drops on four respective separate glass slides with cover slips and examined under microscopy. The number of Demodex mites observed and the number of lashes epilated were recorded and mite density was calculated as the number of mites per lash. Collarettes were graded for each eyelid using a previously described grading scale.23 Lid margin erythema was graded on a scale from 0 to 3 as previously described.25 All investigators were trained to perform epilation and grading consistently (See Appendix B).
Patients using artificial eyelashes within the previous week, those with lid structural abnormalities (eg, ectropion, entropion, etc.), acute ocular infection of active ocular inflammation other than blepharitis, severe dry eye, uncontrolled systemic disease, visual acuity worse than 0.7 logMAR in either eye; those who were pregnant, lactating, or planning pregnancy; those currently involved in an investigational drug or device study; and those with any other condition the investigator felt would confound results, put the patient at risk, or interfere with participation were excluded from the study.
Three hundred and eleven patients met the eligibility criteria and were recruited into the study. All 311 patients with confirmed Demodex blepharitis were asked to complete a blepharitis questionnaire based in part on the validated BLISS questionnaire.26
Continuous data were described using descriptive statistics (mean, standard deviation, and range, as applicable). For categorical data, the results have been represented as counts and percentages. Key results were presented graphically.
Results
The mean (±SD) age of the patients in the study was 68 (±13) years (median: 71 years; range: 23 to 92 years) with females accounting for a higher proportion (62.4%) of participants (N = 311) than males (37.6%). Demographic characteristics are shown in Table 1.
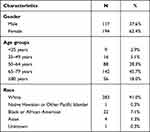 |
Table 1 Demographic Characteristics of Patients Included in the Study (N=311) |
The analysis of questionnaire responses revealed that three-fourths of patients (N = 306) had been experiencing symptoms of blepharitis for ≥2 years and 51% for ≥4 years (Figure 1). “Dry eyes”, “eyes that itch”, and “irritated eyes” were ranked by patients as the three most bothersome symptoms over the previous month (Figure 2). When analyzed by frequency, the same three symptoms were experienced “frequently” or “all of the time” by 64%, 50%, and 44% of patients (N = 301), respectively (Figure 3).
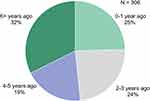 |
Figure 1 Time in years since the first diagnosis of Demodex Blepharitis. |
 |
Figure 2 Most bothersome symptoms over the last month as ranked by patients. |
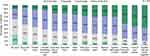 |
Figure 3 The frequency of symptoms over the last month as reported by patients. |
Patients were also asked how blepharitis affected their daily life (Figure 4). Overall, Demodex blepharitis negatively affected 80% of patients (N = 296) on psychosocial metrics. Forty-seven percent of patients (N = 296) responded that they were conscious of their eyes all day and 23% said that they were constantly worrying about their eyes. Six percent of patients (N = 296) felt that the blepharitis symptoms affected their mental state. Nearly half (47%) of patients (N = 296) reported difficulty driving at night and 30% needed additional time for their daily hygiene routine. Demodex blepharitis also affected respondents’ appearance, with 23% of patients (N = 296) saying it gave their eyes or eyelids a negative appearance to others. Among women (N = 185), 34% had difficulty in wearing eye make-up and 5% reported experiencing discomfort with artificial lashes or reducing artificial lash wear.
 |
Figure 4 Impact of blepharitis on the quality of life. |
One-third (33%) of patients (N = 68) said they had visited a doctor for blepharitis ≥2 times, including 18% who went to the doctor ≥4 times (Figure 5). When asked about the specialty of the health care provider patients initially saw for their blepharitis signs or symptoms, of the total 301 patients, 61% responded had consulted an ophthalmologist, 28% an optometrist and 11% a primary care physician. While all subjects (N = 303) had objective signs of Demodex blepharitis confirmed by an eye care provider during the study, 58% said they had never previously been diagnosed with blepharitis. When asked if they had been previously diagnosed with other lid margin or ocular surface conditions, 81% of patients (N = 239) said they had been diagnosed with DED, 3% with rosacea, and 16% with both DED and rosacea.
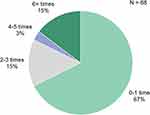 |
Figure 5 Number of visits ever made to a doctor for Demodex blepharitis. |
Eighty-one percent of patients (N = 300) said they had attempted various management approaches for their Demodex blepharitis, currently or in the past. The most common approaches currently in use were artificial tears, warm compresses, and lid wipes (Figure 6). Among those who attempted some form of management approach and discontinued (N = 145), 43% had discontinued due to side effects, tolerability, or lack of effectiveness. Patients were also asked if they had undergone any in-office device procedure for their condition; only a small minority (3%) of patients (N = 297) had done so.
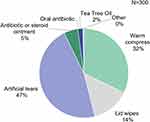 |
Figure 6 Management approaches currently being used for Demodex blepharitis as reported by patients. |
Discussion
Demodex blepharitis is a highly prevalent lid margin disease; still, it is often overlooked or misdiagnosed and, as a result, patients may struggle with the condition for years. Until now, the symptom burden and psychosocial impact of Demodex blepharitis has not been well characterized. The present study is to the authors’ knowledge the first multicenter observational study to evaluate the burden of clinical manifestations of Demodex blepharitis along with the psychosocial impact of the condition in adult patients. Patients with a confirmed diagnosis of Demodex blepharitis were asked questions about ocular symptoms, prior diagnoses, success with over-the-counter and other management options, comorbidities, and daily activities. The analysis of the questionnaire responses shows that Demodex blepharitis is associated with considerable symptomatic and psychosocial burden, negatively affecting daily life in the vast majority of patients with the disease.
The symptoms of Demodex blepharitis seem to impair daily activities and to be long-lasting. As with other lid margin and ocular surface diseases, dryness was the most common symptom reported and one of the most bothersome, as well. Itch has been identified by other authors as a symptom characteristic of Demodex blepharitis.27–30 In our study, 50% of patients reported that their eyes itched frequently or all of the time and 55% identified itching as one of the top three most bothersome symptoms, indicating that even those who had occasional itching found it quite bothersome. Ocular irritation, awareness of the eyes and foreign body sensation were also common.
Frequent and bothersome symptoms may affect visual concentration, disrupting productivity and affecting visually demanding tasks such as night driving. Nearly half the patients in the present study reported difficulty driving at night. Degradation of optical quality related to DED has previously been associated with visual impairments during driving;31 as such, blurred vision (reported by 27% of patients in the present study) may also have contributed to difficulties in night driving.
Untreated chronic disease may have substantial financial implications for affected patients and for the health care system, particularly because many patients experience blepharitis symptoms over long periods of time.32 More than half the patients in the present study (51%) responded that they had been experiencing symptoms of Demodex blepharitis for ≥4 years and 32% for ≥6 years. Many patients had visited a doctor multiple times in hopes of addressing their blepharitis symptoms, including some who had scheduled as many as 6 visits related to blepharitis. Multiple visits increase cost to individuals and health care systems and may increase patient frustration with their health care or health care provider if their chief complaint is not addressed accurately and effectively. Although 81% of patients had previously received or were currently using some kind of Demodex blepharitis management for their symptoms, the vast majority of these options were only supportive such as artificial tears, lid wipes and warm compresses. No FDA-approved prescription treatments are yet available. In some cases (5%), antibiotic or anti-inflammatory agents were prescribed. A small percentage of patients (2%) received OTC remedies containing tea tree oil, an ingredient that has been shown to cause ocular irritation.33–35 Among those who attempted and discontinued some form of Demodex management approach, 43% of patients discontinued the recommended management approach due to tolerability, lack of efficacy, or other issues.
The present study also explored the psychosocial impact and appearance-related concerns of patients with Demodex blepharitis. Overall, Demodex blepharitis negatively impacted 80% of patients on psychosocial metrics, including contributing to a negative appearance to others, causing worry and even an altered mental state. Pro-inflammatory cytokines reportedly cross the blood-brain barrier and can induce psychosocial and behavioral changes.36,37 A previous study reported that patients with blepharitis have a 67% higher risk of anxiety and 52% higher risk of depression compared to those without blepharitis.17 Anxiety related to ocular symptoms or appearance may also burden the healthcare system, affect work performance and social activities. Contact lens use has reportedly been associated with higher self-esteem and enhanced personality of the wearer making them socially more interactive.38–40 Therefore, reduced contact lens wear due to discomfort, reported by 8% of patients in the present study, may also contribute to low psychological well-being in Demodex blepharitis patients.
There are several publications describing the impact of DED on socioeconomic costs and quality of life. The available literature suggests that DED carries high socioeconomic costs as a result of both direct medical costs (health care visits and prescribed/over-the-counter drugs) and indirect costs (from impaired productivity or work absenteeism).32,41 In the US, the annual burden of DED on the health care system has been estimated to be $3.84 billion. Lost work days and reduced productivity add another $55.4 billion in indirect costs.42 Since Demodex blepharitis is as common as DED and there is substantial overlap of symptoms and clinical presentation with DED,9 Demodex blepharitis is also expected to have a similar socioeconomic impact.15 Although the economic burden of Demodex blepharitis was not evaluated, the findings related to multiple visits to eye care professionals and myriad treatments used, even if ineffective, suggest considerable direct costs. Future studies are needed to better understand the economic burden due to direct and indirect costs associated with Demodex blepharitis.
Despite half the patients in the study having experienced symptoms for more than 4 years and all having objective signs of Demodex blepharitis, the majority (58%) had not previously been diagnosed with blepharitis. Collarettes, the pathognomonic sign of Demodex blepharitis, can be easily identified by examining the upper lid margin and lash base when a patient looks down during a slit lamp examination. Widespread education is needed to ensure eye care providers check for collarettes at every eye examination as a simple and fast way of diagnosing Demodex blepharitis without adding chair time.
A limitation of this study is the overlapping nature of symptoms of Demodex blepharitis and DED. Future studies are needed to determine the psychosocial impact of each condition and better elucidate their separate effects on symptoms.
Conclusion
This study is limited by its observational nature and the fact that it relies on patient recollection of symptoms, attempted therapies, doctor visits, and prior diagnoses. However, it confirms that patients with Demodex blepharitis frequently experience and are bothered by ocular symptoms. These patients allocate time and resources to health care appointments and approaches that often do not resolve their symptoms, contributing to individual and health care system costs. Additionally, patients with Demodex blepharitis perceive significant negative effects on their daily activities, mental and physical well-being. Treatments that safely and effectively treat Demodex blepharitis and are simple to use are needed to relieve the symptom burden and reduce psychosocial effects of Demodex blepharitis.
Acknowledgment
Jan Beiting (Wordsmith Consulting, Cary, North Carolina) and Raman Bedi, MD (IrisARC - Analytics, Research & Consulting, Chandigarh, India) provided editorial assistance in the preparation of this manuscript. Portions of this paper were presented at the Association for Research in Vision and Ophthalmology (ARVO) 2021 Annual Meeting as poster presentations with interim findings. The poster abstracts were published in Investigative Ophthalmology and Visual Science, June 2021, Vol 62.
Funding
This study was funded by Tarsus Pharmaceuticals, Inc., Irvine, CA, USA.
Disclosure
JG, EY and DKD have received consulting fees from Tarsus Pharmaceuticals. SNB and MH are employees of Tarsus Pharmaceuticals. DSD has received consulting and research fees from Tarsus Pharmaceuticals and honoraria from Azura. WOW reports personal fees from Tarsus Pharmaceuticals, during the conduct of the study; personal fees from Alcon, Bruder, Baush and Lomb, Azura Pharmaceuticals, Kala Pharmaceuticals, Oyster Point, Regenereyes, Santen, Sight Sciences, Sun Pharmaceuticals and Thea Pharmaceuticals, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Lindstrom R, Donnenfeld E, Foulks G. Blepharitis update on research and management 2010. The New York Eye and Ear infirmary, MedEcus, Ophthalmolology Timesa Continuing Medical Education monograph; 2010.
2. Kasetsuwan N, Kositphipat K, Busayarat M, et al. Prevalence of ocular demodicosis among patients at Tertiary Care Center, Bangkok, Thailand. Int J Ophthalmol. 2017;10(1):122–127. doi:10.18240/ijo.2017.01.20
3. Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between demodex and ocular discomfort. Invest Ophthalmol Vis Sci. 2010;51(6):2906–2911. doi:10.1167/iovs.09-4850
4. Murphy O, O’Dwyer V, Lloyd-McKernan A. Ocular Demodex folliculorum: prevalence and associated symptoms in an Irish population. Int Ophthalmol. 2019;39(2):405–417. doi:10.1007/s10792-018-0826-1
5. Sedzikowska A, Oseka M, Grytner-Ziecina B. Ocular symptoms reported by patients infested with Demodex mites. Acta Parasitol. 2016;61(4):808–814. doi:10.1515/ap-2016-0112
6. Sedzikowska A, Oseka M, Skopinski P. The impact of age, sex, blepharitis, rosacea and rheumatoid arthritis on Demodex mite infection. Arch Med Sci. 2018;14(2):353–356. doi:10.5114/aoms.2016.60663
7. Wesolowska M, Knysz B, Reich A, et al. Prevalence of Demodex spp. in eyelash follicles in different populations. Arch Med Sci. 2014;10(2):319–324. doi:10.5114/aoms.2014.42585
8. Teo A, Rosenberg E, Jacobson A. Prevalence of Demodex colonization in patients presenting to an outpatient clinic. Invest Ophthalmol Vis Sci. 2021;62(8):1236.
9. Trattler W, Karpecki P, Rapoport Y, et al. The prevalence of Demodex Blepharitis in US eye care clinic patients as determined by collarettes: a pathognomonic sign. Clin Ophthalmol. 2022;16:1153–1164. doi:10.2147/OPTH.S354692
10. Farid M. Demodex Blepharitis: simple diagnosis, challenging treatment. Digital supplement. Cataract & Refractive Surgery Today. Available from:: https://crstoday.com/articles/demodex-blepharitis-simple-diagnosis-challenging-treatment/demodex-blepharitis-simple-diagnosis-challenging-treatment/.
11. Wilson FA, Stimpson JP, Wang Y. Inconsistencies exist in national estimates of eye care services utilization in the United States. J Ophthalmol. 2015;2015:1–4. doi:10.1155/2015/435606
12. Cheng AM, Sheha H, Tseng SC. Recent advances on ocular Demodex infestation. Curr Opin Ophthalmol. 2015;26(4):295–300. doi:10.1097/ICU.0000000000000168
13. Gao YY, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089–3094. doi:10.1167/iovs.05-0275
14. Hom MM, Mastrota KM, Schachter SE. Demodex. Optom Vis Sci. 2013;90(7):e198–205. doi:10.1097/OPX.0b013e3182968c77
15. Fromstein SR, Harthan JS, Patel J, Opitz DL. Demodex blepharitis: clinical perspectives. Clin Optom. 2018;10:57–63. doi:10.2147/OPTO.S142708
16. Biernat MM, Rusiecka-Ziolkowska J, Piatkowska E, Helemejko I, Biernat P, Gosciniak G. Occurrence of Demodex species in patients with blepharitis and in healthy individuals: a 10-year observational study. Jpn J Ophthalmol. 2018;62(6):628–633. doi:10.1007/s10384-018-0624-3
17. Chiang CC, Lin CL, Tsai YY, Peng CL, Liao YT, Sung FC. Patients with blepharitis are at elevated risk of anxiety and depression. PLoS One. 2013;8(12):e83335. doi:10.1371/journal.pone.0083335
18. Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505–510. doi:10.1097/ACI.0b013e32833df9f4
19. Luo X, Li J, Chen C, Tseng S, Liang L. Ocular demodicosis as a potential cause of ocular surface inflammation. Cornea. 2017;36(Suppl 1):S9–S14. doi:10.1097/ICO.0000000000001361
20. Pflugfelder SC, Solomon A, Stern ME. The diagnosis and management of dry eye: a twenty-five-year review. Cornea. 2000;19(5):644–649. doi:10.1097/00003226-200009000-00009
21. Putnam CM. Diagnosis and management of blepharitis: an optometrist’s perspective. Clin Optom. 2016;8:71–78. doi:10.2147/OPTO.S84795
22. Tarkowski W, Moneta-Wielgos J, Mlocicki D. Demodex sp. as a potential cause of the abandonment of soft contact lenses by their existing users. Biomed Res Int. 2015;2015:259109. doi:10.1155/2015/259109
23. Zakem M, Fodi C, Bitton E. Comparison of eyelash epilation techniques for the purpose of Demodex Folliculorum Mite Counts. In:
24. Mastrota KM. Method to identify Demodex in the eyelash follicle without epilation. Optom Vis Sci. 2013;90(6):e172–e174. doi:10.1097/OPX.0b013e318294c2c0
25. Yeu E, Baba S, Holdbrook M, Wirta D. Safety and efficacy of topical lotilaner 0.25% for the treatment of Demodex blepharitis: results of the Saturn-1 Phase 2b/3 FDA pivotal trial. Presented at ASCRS. 2021;24:2021.
26. Hosseini K, Bourque LB, Hays RD. Development and evaluation of a measure of patient-reported symptoms of Blepharitis. Health Qual Life Outcomes. 2018;16(1):11. doi:10.1186/s12955-018-0839-5
27. Schachter S, Yeu E, Holdbrook MJ, Baba SN, Gomes PJ. Clinical manifestations of Demodex Blepharitis. Invest Ophthalmol Vis Sci. 2021;62(8):1268.
28. Kabatas N, Dogan AS, Kabatas EU, Acar M, Bicer T, Gurdal C. The effect of Demodex infestation on blepharitis and the ocular symptoms. Eye Contact Lens. 2017;43(1):64–67. doi:10.1097/ICL.0000000000000234
29. Aumond S, Bitton E. Palpebral and facial skin infestation by Demodex folliculorum. Cont Lens Anterior Eye. 2020;43(2):115–122. doi:10.1016/j.clae.2019.09.001
30. Luo KS, Xie A, Yang JJ, Shen EP. Critical value of Demodex count per lash for symptomatic and clinical improvement of Demodex blepharitis. Eye. 2022;36(3):663–665. doi:10.1038/s41433-021-01442-z
31. Deschamps N, Ricaud X, Rabut G, Labbe A, Baudouin C, Denoyer A. The impact of dry eye disease on visual performance while driving. Am J Ophthalmol. 2013;156(1):184–189 e183. doi:10.1016/j.ajo.2013.02.019
32. McDonald M, Patel DA, Keith MS, Snedecor SJ. Economic and humanistic burden of dry eye disease in Europe, North America, and Asia: a systematic literature review. Ocul Surf. 2016;14(2):144–167. doi:10.1016/j.jtos.2015.11.002
33. Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular surface discomfort and Demodex: effect of tea tree oil eyelid scrub in Demodex blepharitis. J Korean Med Sci. 2012;27(12):1574–1579. doi:10.3346/jkms.2012.27.12.1574
34. Messaoud R, El Fekih L, Mahmoud A, et al. Improvement in ocular symptoms and signs in patients with Demodex anterior blepharitis using a novel terpinen-4-ol (2.5%) and hyaluronic acid (0.2%) cleansing wipe. Clin Ophthalmol. 2019;13:1043–1054. doi:10.2147/OPTH.S198585
35. Savla K, Le JT, Pucker AD. Tea tree oil for Demodex blepharitis. Cochrane Database Syst Rev. 2020;6:CD013333. doi:10.1002/14651858.CD013333.pub2
36. Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46–56. doi:10.1038/nrn2297
37. Miller AH. Norman Cousins Lecture. Mechanisms of cytokine-induced behavioral changes: psychoneuroimmunology at the translational interface. Brain Behav Immun. 2009;23(2):149–158. doi:10.1016/j.bbi.2008.08.006
38. Banerjee P, Chaudhry M, Puri A, Jothi K. Mental health status of the keratoconus patients visually corrected with contact lens compared to spectacles. J Psychol Clin Psychiatry. 2016;6(7):00404.
39. Dias L, Manny RE, Weissberg E, Fern KD. Myopia, contact lens use and self‐esteem. Ophthalmic Physiol Opt. 2013;33(5):573–580. doi:10.1111/opo.12080
40. Walline JJ, Jones LA, Sinnott L, et al. Randomized trial of the effect of contact lens wear on self-perception in children. Optom Vis Sci. 2009;86(3):222–232. doi:10.1097/OPX.0b013e3181971985
41. Chan C, Ziai S, Myageri V, Burns JG, Prokopich CL. Economic burden and loss of quality of life from dry eye disease in Canada. BMJ Open Ophthalmol. 2021;6(1):e000709. doi:10.1136/bmjophth-2021-000709
42. Yu J, Asche CV, Fairchild CJ. The economic burden of dry eye disease in the United States: a decision tree analysis. Cornea. 2011;30(4):379–387. doi:10.1097/ICO.0b013e3181f7f363
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
