Back to Journals » Risk Management and Healthcare Policy » Volume 17
Psychometric Characteristics of the Chinese Version of the Tuberculosis Related-Stigma Scale in a Population of Medical Students and Its Correlation with Selected Demographic Characteristics
Authors Yi Y, Sun M, Lu J , Dou X, Yu Y, Zhou L
Received 1 November 2023
Accepted for publication 8 February 2024
Published 5 April 2024 Volume 2024:17 Pages 815—826
DOI https://doi.org/10.2147/RMHP.S446068
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Haiyan Qu
Yaohui Yi, Meng Sun, Jiachen Lu, Xiaofeng Dou, Yingying Yu, Ling Zhou
School of Public Health, Dalian Medical University, Dalian City, Liaoning Province, People’s Republic of China
Correspondence: Ling Zhou, School of Public Health, Dalian Medical University, Dalian City, Liaoning Province, People’s Republic of China, Tel +86-411-8611-0368, Email [email protected]
Background: As future health workers, medical students’ attitudes towards tuberculosis (TB) patients can impact TB control. However, in China, there is a lack of well-quantified assessment regarding the stigma among medical students towards TB patients. Therefore, this study aimed to validate the Chinese version of the Tuberculosis related-Stigma Scale (TSS) in medical students and to apply the scale to measure stigma and its determinants.
Methods: A total of 1035 eligible medical students participated in the cross-sectional questionnaire. Exploratory factor analyses (EFA) and confirmatory factor analyses (CFA) were first conducted to test Chinese version of the TSS construct validity, and then internal consistency was assessed using Cronbach’s α. Finally, multiple linear regression analyses were conducted to identify predictors of stigma.
Results: EFA extracted two factors (“Social distance” and “Exclusionary sentiments”). The CFA further confirmed the two-factor construct. The internal consistency, convergent and divergent validity of the adapted Chinese version of the TSS was acceptable. Furthermore, Whether one has received TB health education and whether know a person with TB are associated with all dimensions of TB stigma, while differences in sex and place of residence play different roles in influencing the different dimensions of stigma.
Conclusion: The adapted Chinese version of the TSS can be used to assess the level of stigma among medical students in China towards tuberculosis patients. When implementing future interventions to reduce stigma associated with TB, special attention should be given to medical students from urban areas, of male gender, who have not received TB health education, and no know a person with TB. However, these two dimensions (“Social distance” and “Exclusionary sentiments”) are impacted by different determinants and should therefore be addressed separately when designing, implementing, and evaluating measures to reduce stigma.
Keywords: tuberculosis related-stigma scale, medical student, psychometrics, determinants
Introduction
Tuberculosis(TB) is an infectious disease with a significantly high global mortality rate. In 2022, an estimated 10.6 million individuals fell ill and 1.6 million died due to TB worldwide.1 The majority of TB cases occur in less developed and developing countries, particularly in China. Although China has made progress in TB control in recent years, it still bears one of the highest burdens of TB and multidrug-resistant TB globally, with nearly 900,000 new cases of TB reported each year.2–4 Additionally, China accounts for approximately 12,000 new cases of Multidrug-resistant tuberculosis (MDR-TB) annually, representing 24% of the global MDR-TB cases.5 According to the latest national TB epidemiological survey in China, among 280 isolates of Mycobacterium TB, 162 strains were found to be sensitive to all 11 tested anti-tuberculosis drugs, while 118 strains were drug-resistant, resulting in a drug resistance rate of 42.1%. Specifically, the drug resistance rate among newly diagnosed TB patients was 42.7%, while it was 38.5% among previously treated patients with relapse.6 Therefore, there is still a need to focus on TB prevention and control.
Timely TB detection and prompt initiation of treatment are two crucial components for successful TB control.7 Currently, various technologies are available for rapid diagnosis of TB, including conventional sputum smear microscopy, rapid molecular diagnostics, and culture-based methods as the reference standard. Diagnostic methods such as rapid tests and cultures can also be employed, along with sequencing techniques, for the detection of TB by conducting microbiological testing on patient’s sputum samples, such as acid-fast staining and Mycobacterium TB nucleic acid amplification tests. Additionally, auxiliary diagnostic methods such as Purified Protein Derivative Tuberculin (PPD) and TB antibody testing are widely utilized. These methods are simple, convenient, rapid, and easy to perform, making them of significant importance for routine TB testing.8 Among these, Molecular-based Drug-Susceptibility Testing (DST) has revolutionized TB diagnosis, with the level of detecting rifampicin resistance increasing from 7% in 2012 to 61% in 2019.9 However, there remains a substantial gap between the estimated and reported number of identified and treated TB cases. For instance, in 2020, less than 60% of the estimated TB cases were reported.10 Stigmatization has been reported as a significant factor contributing to this phenomenon.11,12 The stigma associated with TB often portrays individuals with the disease as deviants, attributing negative personality traits to them and holding them responsible for their illness.13 The main reasons for stigmatization are myths about disease transmission, lack of knowledge, and association with HIV/AIDS.14,15 Studies have also shown that TB stigma leads to decreased treatment adherence and negative impacts on TB treatment outcomes.16,17 In addition, when healthcare providers have negative attitudes towards people with TB, this can also lead to stigmatization of the disease in society as a whole, which has wider socio-economic implications.18,19 Therefore, destigmatization is a critical measure in preventing and controlling the spread of TB.
Medical colleges, as training institutions, are in a prime position to mitigate the stigma associated with TB among future healthcare workers and society. As future health workers, medical students will likely interact with TB patients, and their attitudes toward these patients can impact treatment outcomes. Therefore, measuring medical students’ stigmatization of TB patients in the context of TB control is therefore critical to understanding its determinants, as well as to assessing the effectiveness of stigmatization reduction interventions.
However, most studies have used different, invalidated instruments or only qualitative measures of stigma. Only a few scales have been validated and shown good reliability. For example, in 2008, Van Rie and other researchers conducted in-depth interviews with TB patients and their families, healthcare professionals, and community members in southern Thailand and focused on the aggregation of stigma, after which they created the TB-Related Stigma Scale (TSS), which has been widely used.20,21 Somma et al developed a scale for measuring stigma among TB patients and also included Indian and Bangladeshi versions with good reliability and validity.22 In 2021, Lisa et al developed a stigma scale specifically for drug-resistant tuberculosis (DR-TB) patients. This scale consisted of 14 items and was designed to measure the sense of shame experienced by individuals with DR-TB. The scale demonstrated good reliability and validity.23 In China, there are fewer studies related to the TB Stigma Scale. In 2011, Zhao et al translated and validated the TSS developed by Van Rie in Chinese. The results indicated that the Chinese version of the TSS demonstrated good reliability and validity among TB patients.24 In 2016, Yang developed a scale for measuring disease stigma in TB patients. However, the scale has not yet been widely used, and its scientific validity and usefulness need to be validated in different regions.25
In this study, we used the Chinese version of the TSS translated by Zhao et al.24 This version was specifically translated and adapted within the cultural context of China, making it more suitable for our research.21,26 It is noteworthy that China, being the most populous developing country globally, adopting the Chinese version of the TSS scale can also serve as a reference for other countries in Asia.27 As far as we know, the Chinese version of the TSS has not yet been validated in the population of Chinese medical students, nor has it been subjected to CFA.24 Ahmad et al suggest that when applying a scale to other populations, it is necessary to validate and improve the scale to ensure its accuracy, reliability, and robustness.28 Consequently, this study aimed to validate the Chinese version of the TSS among Chinese medical students and to apply it to measure the level of stigma and respective determinants.
Materials and Methods
Study Site and Participants
Between March 7, 2023, and May 30, 2023, medical students from Dalian Medical University in Dalian, Liaoning Province, Northeast China, participated in this cross-sectional study. The inclusion criteria for participants were as follows: (a) completion of the questionnaire no later than May 30, 2023; (b) full-time undergraduate medical students; (c) signing the informed consent form. Exclusion criteria are as follows: (a) undergraduate medical students not enrolled during the survey period; (b) undergraduate medical students who have already graduated.
The sample size calculation was determined using the formula N=Z2*P(1-P)/d2.29 The determination of sample size in this study was conducted using a two-sided approach, with Z = 1.96 corresponding to a significance level (α) of 0.05. Moreover, to ensure the rigor of the research, a pilot survey method was employed to determine the P-value, yielding a result of P = 51.11%. Based on these parameters, the required sample size was calculated to be 784. To minimize sampling errors, the sample size was increased by 35%.
As a result, 1058 paper questionnaires were eventually distributed to undergraduate students. The final number of valid questionnaires returned was 1035, representing a participation rate of 97.83%.
Data Collection
In designing this Chinese version of the paper-based structured questionnaire, a large number of references were consulted, and experts in the field were consulted to ensure the validity of the questionnaire content. To ensure participants’ accurate understanding of each item, a pre-survey was conducted at the study site. The questionnaire was modified accordingly based on the results of the pre-survey. The questionnaire was divided into two sections: sociodemographic characteristics and Chinese version of the TSS. Sociodemographic characteristics included sex, age, place of residence, whether they had received health education about TB, and whether they knew a person with TB. Figure 1 shows the design flow of this study.
 |
Figure 1 Research Design Flowchart. |
Procedures
Participants are informed about the purpose and procedures of the study, and are required to sign an informed consent form before being asked to complete the paper questionnaire. All questionnaire responses will be kept anonymous and confidential. This study follows the principles of the Helsinki Declaration and has received approval from the Ethics Committee of the School of Public Health, Dalian Medical University.
Measure
TB-Related Stigma Scale (TSS)
TSS was originally developed by Van Rie et al and has been translated into several versions. The scale is divided into two dimensions (community stigma against TB patients and the stigma perceived by TB patients) with a total of 23 items.20,30 In this study, we chose the Chinese version of the TSS (public perspective), which consisted of 12 items with scores between 0 (strongly disagree) and 3 (strongly agree). The higher the scores, the higher the stigmatization level.24,31 Previous research has highlighted that the original item stem “Some people” may lead to inflated scores and impact validity. Therefore, we modified the scale entry by replacing “Some people” with “You”. For example, ‘Some people may not want to eat or drink with friends who have TB’ changed to ‘You may not want to eat or drink with friends who have TB’.31,32
Statistical Analysis
Raw data were input into the database of the EpiData (EpiData Association, Odense, Denmark) software in a two-person entry and evaluated for consistency. Data analysis was conducted using Stata 16.0, SPSS 26.0, and Amos 22.0. Considering that the Chinese version of the TSS has not been validated among medical students and there is uncertainty about how many factors exist, EFA is considered necessary.33 Bartlett’s test of sphericity (p<0.05) and Kaiser-Meyer-Olkin (KMO) >0.50 will be considered suitable for EFA. An item was removed if its loadings were less than 0.4 or the variance of the common factor was less than 0.5.34–37
Following the EFA, we evaluated the construct validity of the scale using CFA. Studies have shown that if the sample size is too large, the chi-square statistic will have a hard time meeting the criteria.38 Since the sample size of this study was greater than 1000, the chi-square test criterion was not utilized in the fitting degree test. The following metrics were used to assess model fit, including root of mean square residual (RMR), root-mean-square error of approximation (RMSEA), the goodness of fit index (GFI), normed fit index (NFI), Tucker-Lewis index (TLI) and comparative fit index (CFI).38–41 The critical values for acceptable model fit used in the present study were SRMR<0.08, RMSEA≤1.0, GFI≥0.80, NFI≥0.80, TLI≥0.80, CFI≥0.85.42–44 Composite Reliability (CR), Average Variance Extracted (AVE) and Heterotrait-Monotrait ratio (HTMT) values of scale were calculated to test convergent and divergent validity.
The internal consistency reliability of the scale was assessed using Cronbach’s α. A Cronbach α level of >0.7 indicates good reliability.45
To ensure the responsiveness of the scale, we examined the presence of floor and ceiling effects. If floor and ceiling effects were observed (15% of the responses focused on the lowest or highest total score), it would have a negative impact on the scale’s responsiveness.46
The sociodemographic characteristics of the participants were analyzed with descriptive statistics, expressed as mean and standard deviation (SD), and categorical variables expressed as frequency and percentage. The normality of TSS scores was determined using the Shapiro–Wilk W-test, the data were tested to be not normally distributed (p-value < 0.05). Consequently, the TSS scores of the participants were expressed as medians and quartiles, and Kruskal–Wallis H was used to examine differences between TSS scores. Variables with p-values < 0.05 were included in the multiple linear regression model to identify variables that were statistically significant. All variables with p-values < 0.05 were considered statistically significant.
Results
Characteristics of Medical Students
In this study, more than half of the participants were female (57.87%), and a significant proportion held a medical degree (67.83%). More than two-thirds of the participants came from families residing in urban areas (69.47%). Over half of the participants were between the ages of 17 and 20 (64.14%). More than one-half of the participants had received TB health education (63.29%), and the majority of the participants did not know a person with TB (85.80%) (Table 1).
 |
Table 1 Demographic Characteristics of Medical Students |
Exploratory Factor Analysis (EFA)
Since the KMO value=0.890 > 0.50 and Bartlett’s test of sphericity was highly significant, the TSS met the requirements for EFA (χ2 = 4865.045 and p-value < 0.001). The results of the EFA showed, that only items 3, 4, and 12 had a common factor variance of less than 0.5; therefore, these three items were deleted to improve the total explained variance of the scale35 (Table 2). In addition, the emergence of two factors with eigenvalues higher than 1. The total explained variance was 63.67%. Since the original Chinese version of the TSS (public perspective) was split into two factors (Table 3). Thus, we named the two subscales “Social Distance” and “Exclusionary sentiments” based on the dimensions recommended by the TB Stigma Measurement Guidelines21 (Table 3).
 |
Table 2 Common Factor Variance and Loading for Each Item in the Tuberculosis-Related Stigma Scale |
 |
Table 3 Results from Exploratory Factor Analysis After Varimax Rotation and Internal Consistency of the TSS |
Confirmatory Factor Analysis (CFA)
The CFA results for the two-factor model indicated the model was a good fit: SRMR=0.038<0.05, RMSEA=0.12<1.0, GFI=0.912>0.800, NFI=0.883>0.800, TLI=0.845>0.800, CFI=0.888>0.850.42–44 Furthermore, although there is a positive correlation between these two dimensions, they represent distinct facets of stigma and may be considered independent. This finding provides further evidence for the necessity of analyzing these two dimensions separately (Figure 2).
 |
Figure 2 CFA: standardized estimates (n=1035). (SRMR=0.038, RMSEA=0.12, GFI=0.912, NFI=0.883, TLI=0.845, CFI=0.888). |
Reliability: Internal Consistency
The Cronbach’s α of the adapted TSS and its two subscales was greater than 0.6, indicating good internal consistency (Table 4).
 |
Table 4 Reliability of the TSS |
Validity: Convergent and Divergent Validity
The convergent and divergent validity of the adapted TSS and its two subscales were met47–49 (Table 5).
 |
Table 5 Convergent and Divergent Validity of the TSS |
The Level of Different Dimensions of Adapted TSS
Table 6 showed the median and quartiles of the adapted TSS and its dimensions. With regard to the lower and upper limit effects, the absence of these effects in the dimensions was observed, which favors the responsiveness of the scale.30
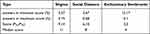 |
Table 6 Analysis of Floor and Ceiling Effects of Answers, Score (P25,P75) and Median Score, in TSS Dimensions |
Factors Associated with Three Dimensions of Stigma
The results of the analyses indicated that the variables of whether they had received TB health education and whether they knew a person with TB may significantly influence the stigma and its dimensions of students’ stigmatization of people with TB. However, differences in sex and place of residence affected the stigmatization dimensions differently (All p-values<0.05) (Table 7).
 |
Table 7 Multiple Linear Regression Analysis of Factors Associated with Different Dimensions of TSS |
Discussion
As future health worker, the medical students’ stigmatization of TB patients can have an impact on the general public as well. Therefore, there is a need for a scale to measure the stigma of medical students towards TB patients. To the best of our knowledge, this is the first study to validate the Chinese version of the TSS among Chinese medical students and the first study to use CFA in the Chinese version of the TSS.
Based on the results of the EFA, the factor loadings of the adapted TSS after deletion of the three ineligible items ranged from 0.599 to 0.859. The factor loadings of the original scale by Van Rie et al ranged from 0.49 to 0.82. Additionally, other versions of the TSS factor loadings were 0.52–0.80.28,50,51 However, there is currently no available report on the factor loadings of the original Chinese version of the scale. Therefore, the high correlation coefficients between the adapted TSS and its factors also indicate the high internal consistency of the scale. This study also found that the adapted TSS was categorized into two dimensions after conducting EFA, and the EFA of the Indonesian version of the TSS supported a two-factor model, but with a slightly different division of items, which may be due to the different cultural backgrounds in different regions.28,52
Regarding model fit, Van Rie et al reported the following fit indices for the original scale; TLI = 0.94, CFI = 0.88, and RMSEA = 0.11.20 According to the report, the fit indices for the Turkish version of TSS were: CFI=0.94, RMSEA=0.077, GFI=0.95, SRMR=0.079.50 The fit indices for the Colombian version were: TLI=0.72, CFI=0.77, RMSEA=0.16, SRMR=0.08.51 The fit indices for the Indonesian version of TSS were: TLI=0.798, CFI=0.849, RMSEA=0.088, SRMR=0.062.28 However, the original Chinese version did not undergo confirmatory factor analysis (CFA), so fit indices are not available. Whereas after CFA in the present study, the fit of the two-factor model was also acceptable (TLI = 0.845, CFI = 0.888, RMSEA = 0.12, GFI = 0.912, SRMR = 0.038). When testing convergent and divergent validity, CR values > 0.70 and AVE values > 0.50 indicate good convergent validity. HTMT values < 0.85 indicate good divergent validity.47–49 Therefore, based on the results of this study, it was determined that all of the above metrics satisfy the conditions.
The Cronbach’s α reliability coefficient is used to assess internal consistency. Measurement instruments are considered relatively reliable when their Cronbach’s α is between 0.60 and 0.79, and highly reliable when their Cronbach’s α is between 0.80 and 1. In this study, the adapted TSS scale demonstrated a Cronbach’s α of 0.86. The original scale developed by Van Rie et al had a Cronbach’s α of 0.85. The Cronbach’s α of the original Chinese version of the TSS scale translated by Zhao et al was 0.94.24,31 Other versions of the TSS Cronbach’s alpha were 0.81–0.89.28,50,51 The reason for the differences may be due to the differences in the target populations and sample sizes. Regarding the ceiling and floor effects of the scale, this study did not find any of these effects in any dimension of the scale, indicating that the scale has good responsiveness. According to the results of this study, the adapted TSS is a valid and reliable instrument.
The secondary aim of this study was to determine the possible predictors of stigmatization of TB patients among Chinese medical students. The present study found that both the receipt of TB health education and know a person with TB were associated with TB stigma and its dimensions, while differences in sex and place of residence played different roles in influencing the different dimensions of stigma.
More than one-third of the medical students in this study still had not received TB health education. This study showed that TB health education plays a vital role in decreasing the stigma of TB. Similarly, the findings of N.A. Idris and Peng have again proved the importance of TB health education in decreasing the stigma of TB patients among students.53,54 In addition, the same conclusion has been reached in AIDS related studies.55 This may be because students who had received TB health education were able to have a basic understanding of TB information, such as the causes of the disease and its transmission routes, which reduced their misconceptions about the disease and thus improved their behavioral attitudes towards TB patients. Therefore, it is recommended that TB health education be included in the medical students’ curriculum, which is essential to reduce TB stigma.
Previous studies have shown that whether know a person with TB is strongly associated with the level of stigmatization of people with TB.56 COVID-19 stigma-related studies support this view, which is consistent with our findings.57 Some studies have shown that intergroup contact experiences are conducive to reducing stigmatization, as they help to provide an understanding of the living conditions of the stigmatized group, as well as an understanding of the feelings and worldview of the stigmatized group, which improves stereotypes and creates empathy for the group and mitigates the stigmatization of the group.58,59 This may suggest that adding an interactive component with successfully treated TB patients to future TB stigmatization interventions would be beneficial in reducing the stigmatization of this population.
Consistent with previous studies on the stigma associated with COVID-19, HIV, and TB, women were less likely to stigmatize TB patients than men.60–62 This may be because women tend to take their health more seriously, are more likely to obtain relevant information about TB from various sources, and can hold a correct view of TB. In addition, studies have shown that women have higher levels of empathy than men, which is the ability to understand the feelings and experiences of others.63,64 This may also explain why women’s rejection of TB patients is also lower for women compared to men. However, there was no significant difference between males and females in terms of social distance towards TB patients, which may be due to the infectious nature of TB patients. More resources could be allocated to men when implementing stigma-related interventions in the future.
Our study showed that medical students from rural areas had a lower level of stigmatization of TB patients compared to those from urban areas. Oladele et al showed that a higher percentage of rural residents had positive attitudes towards TB patients compared to those from urban areas, which is consistent with our study.65 Similarly, the same conclusions have been reached in studies on AIDS.66 In addition, rural medical students were less socially distant from TB patients than urban medical students. It has been reported that the incidence of TB in rural China is higher than that in urban areas.67 This results in rural residents being more likely to encounter TB patients than urban residents, which may result in rural residents having some basic understanding of TB and being less likely to hold higher levels of stigma and social distance from TB patients. Perceptions of stigmatization as a sociological concept also vary culturally by geographic region. Therefore, this discrepancy requires further exploration in the future.
This study has some limitations. Firstly, it was a cross-sectional survey, and therefore, causal inferences cannot be made. Secondly, although a large number of medical students were recruited for this study, the sample was not representative of the entire population in China, which may limit the generalizability of the results. Future studies should include more diverse samples, to address this limitation and generalize the results to a broader context. Finally, compared to the original version, the modified Chinese version of the TB-related stigma scale has undergone changes and reductions in the number of items, resulting in variations in questionnaire scores.
Conclusion
As far as we know, the first to use the validity of the EFA and CFA in measuring the Chinese version of the TSS in a sample of medical students. The study results indicate that the adapted Chinese version of TSS demonstrates good reliability among medical students in China and can be used to assess the level of stigma towards TB patients. When implementing future interventions to reduce stigma associated with TB, special attention should be given to medical students from urban areas, of male gender, who have not received TB health education, and no know a person with TB. Additionally, the study found that gender and place of residence have different impacts on different dimensions of stigma. Therefore, when designing, implementing, and evaluating stigma reduction programs, these two dimensions should be considered separately.
Abbreviations
TB, Tuberculosis; TSS, Tuberculosis-related Stigmatization Scale; EFA, Exploratory factor analyses; CFA, Confirmatory factor analyses; HIV, Human immunodeficiency virus; AIDS, Acquired immune deficiency syndrome; WHO, World Health Organization; MDR-TB, Multidrug-resistant tuberculosis; DST, Drug-Susceptibility Testing; PPD, Purified Protein Derivative Tuberculin; DR-TB, drug-resistant tuberculosis; KMO, Kaiser-Meyer-Olkin; RMR, Root of mean square residual; RMSEA, Root-mean-square error of approximation; GFI, Goodness of fit index; NFI, Normed fit index; TLI, Tucker-Lewis index; CFI, Comparative fit index; CI, Confidence interval; SD, Standard deviation; HTMT, Heterotrait-monotrait ratio.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The Ethics Committee of the School of Public Health, Dalian Medical University approved this study. Before the investigation, the students were informed of the purpose of the study and the presentation of the results, and they were assured that their personal information would not be disclosed. All students signed informed consent forms in our study. The research adhered to the tenets of the Declaration of Helsinki.
Acknowledgments
We thank the student of Dalian Medical University for their cooperation in carrying out this research. We thank data collectors and supervisors for their commitment. We would be remiss if we did not thank the students who participated in this study.
Author Contributions
LZ and YHY provided the research design and carried out the whole study. YHY analysed the data and drafted the manuscript. YHY and MS reviewed the article.YHY, MS, JCL, XFD and YYY participated in the collection and entry of the data. All authors read, revised and approved the final manuscript. All authors have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study had no funding support.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Adam T, Baddeley A, Bastard M, et al. WHO’s Global Tuberculosis Report 2023. World Health Organization; 2023.
2. Chunrong L, Hongxia F, Puxuan L, Lecai J. The global tuberculosis report 2021: key data analysis for China and the global world. Emerg Infect Dis. 2021;6(4):368.
3. World Health Organization. Global tuberculosis report 2021: supplementary material.2022.
4. Zhang H, Liu X, Xu C, et al. Guiding tuberculosis control through the healthy China initiative 2019− 2030. China CDC Weekly. 2020;2(49):948. doi:10.46234/ccdcw2020.236
5. World Health Organization. Multidrug and Extensively Drug-Resistant TB. World Health Organization; 2010.
6. ChenYH C. Meta-analysis of the status of drug resistance of tuberculosis in China. Guide Chin Med. 2011;9(17):26–28.
7. Chimbatata NBW, Zhou C-M, Chimbatata CM, Xu B. Post-2015, why delay to seek healthcare? Perceptions and field experiences from TB healthcare providers in northern Malawi: a qualitative study. Infect Dis Poverty. 2017;6(1). doi:10.1186/s40249-017-0279-1
8. Lifa X, Changhao H, Xiaohuan L. Advances in immunologic assays for tuberculosis. J Med Pest Control. 2021;37(02):152–156.
9. World Health Organization. Catalogue of mutations in mycobacterium tuberculosis complex and their association with drug resistance; 2021.
10. Bagcchi S. WHO’s global tuberculosis report 2022. Lancet Microbe. 2023;4(1):e20. doi:10.1016/S2666-5247(22)00359-7
11. Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125(4_suppl):34–42. doi:10.1177/00333549101250s407
12. Fatiregun A, Ejeckam C. Determinants of patient delay in seeking treatment among pulmonary tuberculosis cases in a government specialist hospital in Ibadan, Nigeria. Tanzan J Health Res. 2010;12(2):113–120. doi:10.4314/thrb.v12i2.56398
13. Katz I. Some thoughts about the stigma notion. Pers Soc Psychol Bull. 1979;5(4):447–460. doi:10.1177/014616727900500406
14. Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: a qualitative study. BMC Public Health. 2007;7(1):1–10. doi:10.1186/1471-2458-7-211
15. Rau A, Wouters E, Engelbrecht M, et al. Towards a health-enabling working environment-developing and testing interventions to decrease HIV and TB stigma among healthcare workers in the Free State, South Africa: study protocol for a randomised controlled trial. Trials. 2018;19(1):1–15. doi:10.1186/s13063-018-2713-5
16. Chang S-H, Cataldo J. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. Int J Tuberc Lung Dis. 2014;18(2):168–173. doi:10.5588/ijtld.13.0181
17. Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 2007;4(7):e238. doi:10.1371/journal.pmed.0040238
18. Dodor E. Health professionals expose TB patients to stigmatization in society: insights from communities in an urban district in Ghana. Ghana Med J. 2008;42(4):144.
19. Pardeshi GS, Kadam D, Chandanwale A, Bollinger R, Deluca A. Resident doctors’ attitudes toward tuberculosis patients. Indian J Tuberc. 2017;64(2):89–92. doi:10.1016/j.ijtb.2016.11.001
20. Van Rie A, Sengupta S, Pungrassami P, et al. Measuring stigma associated with tuberculosis and HIV/AIDS in southern Thailand: exploratory and confirmatory factor analyses of two new scales. Int J Trop Med. 2008;13(1):21–30. doi:10.1111/j.1365-3156.2007.01971.x
21. Craig G, Meershoek A, Zwerling A et al. TB stigma–measurement guidance. ; 2018.
22. Somma D, Thomas BE, Karim F, et al. Gender and socio-cultural determinants of TB-related stigma in Bangladesh, India, Malawi and Colombia. Int J Tuberc Lung Dis. 2008;12(7):856–866.
23. Redwood L, Mitchell EMH, Thu Anh N, Viney K, Viet Nhung N, Fox GJ. Psychometric evaluation of a new drug-resistant tuberculosis stigma scale. J Clin Epidemiol. 2021;133:101–110. doi:10.1016/j.jclinepi.2021.01.007
24. Aiqing Z, Peixia W. Sinicization of the tuberculosis stigma perception scale and evaluation of its reliability and validity. Nurs J Chin People’s Liberat Army. 2011;28(06):12–14+75.
25. Yang T, Yanhong G, Xiaoxu Y. Development and evaluation of the tuberculosis-related stigma scale. J Prev Med Public Health. 2016;27(06):46–48.
26. Bergman A, McNabb K, Farley JE. A systematic review and psychometric appraisal of instruments measuring tuberculosis stigma in Sub-Saharan Africa. Stigma Health. 2021;9(1):81–93. doi:10.1037/sah0000328
27. Zhilong C. Geography, agglomeration economies and the long-term evolution of the spatial distribution of population. Popul Dev. 2024;30(01):41–51+119.
28. Fuady A, Arifin B, Yunita F, et al. Stigma towards people with tuberculosis: a cross-cultural adaptation and validation of a scale in Indonesia. BMC Psychol. 2023;11(1):112. doi:10.1186/s40359-023-01161-y
29. Wald A. Sequential Analysis. Oxford, England: John Wiley; 1947.
30. Crispim J, Caetano da Silva LM, Yamamura M, et al. Validity and reliability of the tuberculosis-related stigma scale version for Brazilian Portuguese. BMC Infect Dis. 2017;17. doi:10.1186/s12879-017-2615-2
31. Kipp AM, Pungrassami P, Nilmanat K, et al. Socio-demographic and AIDS-related factors associated with tuberculosis stigma in southern Thailand: a quantitative, cross-sectional study of stigma among patients with TB and healthy community members. Bmc Public Health. 2011;11(1). doi:10.1186/1471-2458-11-675
32. Audet CM, McGowan CC, Wallston KA, Kipp AM. Relationship between HIV stigma and self-isolation among people living with HIV in Tennessee. PLoS One. 2013;8(8):e69564. doi:10.1371/journal.pone.0069564
33. Kipp AM, Audet CM, Earnshaw VA, Owens J, McGowan CC, Wallston KA. Re-validation of the Van Rie HIV/AIDS-related stigma scale for use with people living with HIV in the United States. PLoS One. 2015;10(3):e0118836. doi:10.1371/journal.pone.0118836
34. Bujang MA, Omar ED, Baharum NA. A review on sample size determination for cronbach’s alpha test: a simple guide for researchers. Malaysian J Med Sci. 2018;25(6):85. doi:10.21315/mjms2018.25.6.9
35. Chanchan H, Jianbo H, Jianbo L. Reliability and validity analysis of the short version of the DSM-5 personality inventory (Chinese version) and its preliminary use in a Chinese population. Zhejiang Med. 2020;42(19):2037–2041.
36. Pallant J SPSS survival manual: a step by step guide to data analysis using IBM SPSS: mcGraw-hill education (UK); 2020.
37. Song C, Hashim SB, Xu X, Ling H. Career adapt-ability scale-short form: validation among early career stage of Chinese university graduates. Frontiers in Psychology. 2023;14:1110287. doi:10.3389/fpsyg.2023.1110287
38. Dullie L, Meland E, Hetlevik Ø, Mildestvedt T, Gjesdal S. Development and validation of a malawian version of the primary care assessment tool. BMC Fam Pract. 2018;19(1):1–11. doi:10.1186/s12875-018-0763-0
39. Ruan F, Fu G, Zhou M, et al. Application of the Chinese version of Zelaya’s HIV-related stigma scale to undergraduates in mainland China. Bmc Public Health. 2019;19(1). doi:10.1186/s12889-019-8054-9
40. Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. psychology press; 2004.
41. Feng L-S, Dong Z-J, Yan R-Y, et al. Development and validation of the cancer symptoms discrimination scale: a cross-sectional survey of students in Yunnan, China. BMC Palliat Care. 2020;19(1). doi:10.1186/s12904-020-00662-6
42. Bahar Z, Cal A, Beser A, et al. A study on the adaptation of the HIV/AIDS-related Stigma Scale into Turkish. Perspect Psychiatr Care. 2022;58(2):509–517. doi:10.1111/ppc.12984
43. Yue Z, Ma C, Lim K-S, et al. Validation of the Chinese version of public attitudes toward epilepsy scale in Mainland China. Epilepsy Behav. 2017;72:150–155. doi:10.1016/j.yebeh.2017.04.028
44. Asiandi A, Erlina M, Lin Y-H, Huang M-C. Psychometric evaluation of the nurses professional values scale-3: Indonesian version. Int J Environ Res Public Health. 2021;18(16):8810. doi:10.3390/ijerph18168810
45. Yilmaz M, Dişsiz G, Demir F, Irız S, Alacacioglu A. Reliability and validity study of a tool to measure cancer stigma: patient version. Asia PacJ Oncol Nurs. 2017;4(2):155–161. doi:10.4103/apjon.apjon_10_17
46. McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. 1995;4(4):293–307. doi:10.1007/BF01593882
47. Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39–50. doi:10.1177/002224378101800104
48. Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Marketing Sci. 2015;43(1):115–135. doi:10.1007/s11747-014-0403-8
49. Cheung GW, Cooper-Thomas HD, Lau RS, Wang LC. Reporting reliability, convergent and discriminant validity with structural equation modeling: a review and best-practice recommendations. Asia Pac J Manag. 2023;1–39.
50. Beser A, Bahar Z, Kissal A, et al. Psychometric properties of the Turkish version of the tuberculosis-related stigma scale. Acta Paulista De Enfermagem. 2018;31(4):374–381. doi:10.1590/1982-0194201800053
51. Pamela Castaneda-Daniels N, Campo-Arias A, Carlos Pedrozo-Pupo J. Assessment of validity and reliability of the tuberculosis related stigma scale in Colombian patients. Curr Med Res Opin. 2022. doi:10.1080/03007995.2022.2065144
52. Soemarko DS, Halim FA, Kekalih A, et al. Developing a tool to measure tuberculosis-related stigma in workplaces in Indonesia: an internal validation study. SSM-Popul Health. 2023;21:101337. doi:10.1016/j.ssmph.2023.101337
53. Idris NA, Zakaria R, Muhamad R, Husain NRN, Ishak A, Mohammad WMZW. The effectiveness of tuberculosis education programme in Kelantan, Malaysia on knowledge, attitude, practice and stigma towards tuberculosis among adolescents. Malaysian J Med Sci. 2020;27(6):102. doi:10.21315/mjms2020.27.6.10
54. Peng Fei. Analysis of the results of an intervention finding on discrimination against tuberculosis patients among party school participants. Chin J Social Med. 2013;30(06):403–405.
55. Chuang Z, Xiameng Z, Wentong Z. The current situation of AIDS discrimination among Chinese medicine students in a medical school in Sichuan Province and its influencing factors. Occup Health. 2020;36(06):829–832. doi:10.13329/j.cnki.zyyjk.2020.0220
56. Jaramillo E. Tuberculosis and stigma: predictors of prejudice against people with tuberculosis. J Health Psychol. 1999;4(1):71–79. doi:10.1177/135910539900400101
57. Liu R, Nicholas S, Leng A, Qian D, Maitland E, Wang J. The influencing factors of discrimination against recovered coronavirus disease 2019 (COVID-19) patients in China: a national study. Hum Vaccines Immunother. 2022;18(1). doi:10.1080/21645515.2021.1913966
58. Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. J Pers Soc Psychol. 2006;90(5):751. doi:10.1037/0022-3514.90.5.751
59. Pettigrew TF, Tropp LR, Wagner U, Christ O. Recent advances in intergroup contact theory. Int J Intercultural Relations. 2011;35(3):271–280. doi:10.1016/j.ijintrel.2011.03.001
60. Zhang T-M, Zhang X-F, Meng X-D, et al. Comparison of stigmatizing views towards COVID-19 and mental disorders among adolescent and young adult students in China. Frontiers in Psychiatry. 2023;14. doi:10.3389/fpsyt.2023.1170540
61. Zhengbin Z, Yun Y, Li L. Analysis of the current situation of university students’ knowledge, beliefs and behaviors related to tuberculosis prevention and control in Wuhan and factors related to prevention and control behaviors. Chin J Sch Health. 2023;44(03):361–365. doi:10.16835/j.cnki.1000-9817.2023.03.010
62. Jahić R, Porobić-Jahić H, Žepić D, Piljić D, Petrović J, Čustović A. Knowledge, attitude and stigma towards HIV patients: a survey among medical students in Tuzla, Bosnia and Herzegovina. J Infect Developing Countries. 2020;14(09):1019–1026. doi:10.3855/jidc.12526
63. Eagly AH, Wood W, Diekman AB. Social role theory of sex differences and similarities: a current appraisal. Dev Soc Psychol Gender. 2000;12(174):9781410605245.
64. Dictionary O. Oxford Advanced Learner’s Dictionary. Oxford Learner Dictionaries; 2000.
65. Oladele DA, Balogun MR, Odeyemi K, Salako BL. A comparative study of knowledge, attitude, and determinants of tuberculosis-associated stigma in rural and urban communities of Lagos State, Nigeria. Tuberc Res Treat. 2020;2020:1964759. doi:10.1155/2020/1964759
66. Xuya, Jiaming L, Xiaohua Y. Analysis of the attitudes and influencing factors of workers in public places towards people living with HIV and patients. Mod Preventive Med. 2013;40(01):76–78+85.
67. Zhu B, Liu J, Fu Y, Zhang B, Mao Y. Spatio-temporal epidemiology of viral hepatitis in China (2003–2015): implications for prevention and control policies. Int J Environ Res Public Health. 2018;15(4):661. doi:10.3390/ijerph15040661
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
