Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Psychological Burden of Patients with Head and Neck Cancer Undergoing Radiotherapy and Their Family Caregivers: A Cross-Sectional Survey
Authors Tang Y, Hua Y, Huang X, Cao Y, Sun X
Received 17 November 2022
Accepted for publication 22 February 2023
Published 5 April 2023 Volume 2023:16 Pages 927—935
DOI https://doi.org/10.2147/JMDH.S398064
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Yuanyuan Tang,1,* Yuchen Hua,1,* Xiaoping Huang,2 Yuandong Cao,1 Xinchen Sun1
1Department of Radiation Oncology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, People’s Republic of China; 2Department of Nursing, The First Affiliated Hospital of Nanjing Medical University, Nanjing, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xinchen Sun, Department of Radiation Oncology, The First Affiliated Hospital of Nanjing Medical University, No. 300 Guangzhou Road, Nanjing, Jiangsu, 210029, People’s Republic of China, Tel +86 25 68305696, Email [email protected]
Background: The consequences of Head and neck cancer (HNC) affect both the person who receives the diagnosis and their family caregivers (FCs).
Objective: To investigate the psychological status of patients and their FCs, and the burden of the FCs during radiotherapy.
Methods: This cross-sectional study was conducted with a questionnaire survey by convenience sampling method. Patients with HNC and their caregivers (both N = 85) from the radiotherapy department of our hospital were recruited between March 2021 and March 2022. The Hospital Anxiety and Depression Scale (HADS), the Chinese version of the Connor and Davidson Resilience Scale (CD-RISC), and the Zarit Burden Interview (ZBI) were used to assess the symptoms of anxiety and depression, psychological resilience, and the impact of care work, emotions and social lives of participants. Pearson’s correlation analysis and a Mann–Whitney test were used to analyse the association between the HADS and the CD-RISC scores of the patients.
Results: About half of the patients (56.47%) and the caregivers (62.35%) have had anxiety. The average HADS-Anxiety scores, HADS-Depression scores, and CD-RISC scores of the patients with HNC were 7.4± 1.9, 6.4± 2.2, and 56.8± 12.6. The “Strength” and “Resilience” scores of the patients were inversely related to their HADS anxiety scores (p < 0.05). The “Resilience” and “optimism” scores of them were inversely related to HADS depression scores (p < 0.05). The average ZBI score of the caregivers was 23.8± 10.1; HADS anxiety scores and HADS depression scores of the caregivers were positively associated with total ZBI scores and individual burden scores (p < 0.05).
Conclusion: More than half of patients with HNC undergoing radiotherapy have anxiety, and about a third have depression. The anxiety and depression status of the FCs of patients with HNC undergoing radiotherapy is related to caregiver burden, deserving the attention of clinical medical staff.
Keywords: head and neck cancer, radiotherapy, family caregiver, psychological status
Introduction
Head and neck cancer (HNC) is a cancer with high mortality and morbidity. According to the latest report of the International Agency for Research on Cancer, the number of patients newly diagnosed with HNC in China in 2020 was estimated to exceed 142,000, and the number of deaths due to HNC was nearly 75,000, representing a steady growth trend that seriously threatens the lives and health of patients.1
Treatment options of HNC usually include surgery, radiotherapy, systemic therapy or combined therapy. More than 90% of malignant tumours of the head and neck are squamous cell carcinoma, and surgery and radiotherapy are the most common treatments.2 In addition to the effects of the cancer itself, the consequences of treatment often interfere with important functions such as breathing, swallowing, and speaking. For example, the side effects of radiotherapy mainly include radiation oral mucositis, radiation dermatitis and difficulty in opening the mouth. Among these, radiation oral mucositis usually manifests as oral mucosal hyperaemia, erythema, erosion, ulcers and fibrosis. Patients experience pain and feeding difficulties, which directly affect their eating status and physical health.3
HNC is also a psychologically painful cancer type that negatively impacts health-related quality of life (QOL).4,5 This psychological distress includes both normal feelings such as vulnerability, sadness, and fear, as well as problems that may significantly affect patients’ lives, such as depression, anxiety, panic, social isolation, and personal crisis.6 According to multisystem theory, patients are not independent individuals but are part of a system of interaction with their informal caregivers.7 FCs are companions, children or close friends who have a significant personal relationship with the patient, all of whom provide a broad range of assistance for the person with a chronic or disabling condition, such as HNC.8 Caregivers, as well as patients, may be adversely affected by cancer, and patients with cancer rely on the emotional, physical and financial support of their caregivers. The caregivers of patients with cancer have unique challenges compared with those of other types of patients, such as dementia, diabetes or normal ageing, because cancer caregivers typically spend more time performing care duties per day and generate more out-of-pocket costs than other caregivers, and they have to respond to rapidly changing conditions.9 The greater the somatic disease of patients with cancer, the greater the caregiver burden, which, in turn, affects their mental health.10
FCs are often the primary source of social and emotional support for patients, and they play major roles in how well patients manage the consequences of their illness and treatment.11–13 Historically, family care has been particularly important in China due to the country’s strong family structure, traditional culture (such as filial piety) and underdeveloped welfare system.14 However, little is known about the perceived social support during radiotherapy for HNC caregivers in the current study, including how it relates to caregiver burden and quality of life.
Current evidence on psychosocial functioning of HNC caregivers is sparse and limited to a few studies that prospectively assessed and used nonspecific measures of cancer care. In addition, most studies focus on caregivers after treatment of patients, not during radiotherapy.6 In this study, we used the HADS to evaluate the psychological status of patients with HNC and their FCs to investigate the psychological status of patients and the burden of their caregivers during radiotherapy.
Methods
Participants
Our cross-sectional survey was conducted in the radiotherapy department of a grade-III hospital in China between March 2021 and March 2022. Eligible patients (N = 85) and their FCs (N = 85) completed the corresponding questionnaires while waiting for radiotherapy. FCs were administered in separate 20–30 minutes interviews during this period.
The calculated sample size was set at 85 to detect a clinically meaningful difference in the Caregiver Strain Index scores before and after intervention (superiority design with α = 0.05, power = 80% and anticipated drop-out rate = 10%).15
Each patient and their caregiver completed the questionnaire and were interviewed once. All participants participated voluntarily and provided written informed consent in accordance with the Declaration of Helsinki. Respondents were assured of confidentiality and anonymity.
Participants who met the following criteria were included: (1) aged 18–70 years, (2) with a diagnosis of HNC without distant metastasis, (3) with a Karnofsky Performance Status Scale score of >60 points, (4) voluntarily participated in the study and (5) with no history of head or neck radiotherapy.
Participants with one or more of the following criteria were excluded: (1) life expectancy of <3 months, (2) a diagnosis of other serious diseases, such as heart, brain or lung disease, (3) mental illness, a severe cognitive impairment or a speech deficit according to medical history records, (4) a haematological tumour, (5) pregnant or breastfeeding and (6) within the active period of an infectious disease.
Instruments
All patients and caregivers were required to complete the following questionnaires and undergo interviews to provide sufficient information.
Basic Demographic Information
Basic demographic information was obtained using a self-designed questionnaire and included age, gender, year of birth, relationship to the patient, education level, profession, working status, income level, type of medical insurance, marital status (unmarried, married or divorced/widowed) and monthly household income.
The Chinese Version of the Hospital Anxiety and Depression Scale
The Chinese version of the Hospital Anxiety and Depression Scale (HADS) is a self-reported questionnaire that has been widely used in clinical practice.16 It contains 14 items and consists of two 7-item subscales, one measuring anxiety and the other measuring depression in populations with medical conditions.17 A Likert type 4-point scale was used to rate each item, ranging from 0 (no problems) to 3 (high-level problems). Participants answer each question with respect to their feelings and/or behaviour during the previous week. The score of each subscale is obtained by simple addition of each entry, which ranges from 0 to 21 points. A total score of <7 for each subscale indicates no depression/anxiety, 8–10 indicates the possibility of depression/anxiety, and 11+ indicates the presence of depression/anxiety.18
The Chinese Version of the Connor and Davidson Resilience Scale
The CD-RISC was compiled by Connor and Davidson, and includes 25 items, fixes the dimensions into 3 domains of strength (8 items), resilience (13 items), and optimism (4 items), and assigns a score from 0 to 4 based on the “never do so” option under each items, and the total score ranges from 0–100 points. The scale is suitable for the assessment of people who feel the psychological state such as stress and frustration, the patients of this study fit the characteristics of this type of population, suitable for the scale. The higher the score, the higher the level of psychological resilience.19
The Chinese version of the CD-RISC was translated and revised from the original CD-RISC by Yu and Zhang19 in 2007, resulting in a three-factor structure of psychological resilience based on Chinese culture (tenacity, strength and optimism). The Chinese version of the CD-RISC was tested in the Chinese general population, with a Cronbach’s alpha score of 0.91.
The Zarit Burden Interview
The Zarit Burden Interview (ZBI) was developed by Zarit et al20 in 1980. The Chinese version of the ZBI has adequate reliability and validity, with a Cronbach’s alpha score of 0.87.21 The scale includes a total of 22 items in two dimensions (including personal burden and responsibility burden) and evaluates the impact of care work on the health status, emotions and social lives of caregivers. Personal burden refers to the health status and mental status of caregivers, and responsibility burden dimension refers to the social and economic burden of caregivers. The ZBI uses a five-point scale from 0 (never) to 4 (almost always), and the total score ranges from 0–88 points with a higher score indicating a higher burden.
The ZBI were conducted by a researcher experienced in qualitative research and working with oncology patients and their families. Semistructured interviews assessed participants’ understanding of ZBI and its relevance to their own experiences as caregivers. Interviews were conducted until data saturation (no valuable information was obtained from the interviews).21 Interviews were audio taped and transcribed verbatim.
Statistical Analyses
The statistical analyses used Microsoft Excel and IBM® SPSS™ Statistics version 23.0 software. Categorical data were presented as numbers (percentages), with continuous data presented as mean ± standard deviation (SD). Pearson’s correlation analysis and a Mann–Whitney test were used to analyse the correlation between the HADS of the patients with HNC and those of their FCs. The significance levels were set at p < 0.05.
Results
Characteristics
A total of 180 questionnaires were distributed to the patients and their FCs, and 170 were recovered (85 for patients with HNC and 85 for their caregivers, all valid), with an efficiency of 94.44%. The clinical and descriptive data of the patients and FCs are shown in Table 1.
 |
Table 1 Descriptive and Clinical Data of the Patients |
Among the 85 patients, the average age was 62.8 years (SD = 10.6), and most (72.3%) were older than 51 years. Among all patients with HNC, those with nasopharyngeal cancer accounted for the largest proportion (53.4%), and the tumor stages were mostly stage 3–4 (82.4%). Most of the patients were male (68.2%) and married (94.1%). The majority of the patients (96.5%) had a senior high school education or below. In most cases (90.6%), the FCs did not discuss the topic of death with their patients.
The average age of the FCs was 52.6 years (SD = 12.5), ranging from 25 to 74 years. Most of the FCs were female (65.9%) and married (97.6%), and most (87.1%) had received a senior high school education or below. The majority (54.1%) had a family income of more than 2000 RMB per month. Spouses made up 35.3% of the caregivers. The vast majority of the FCs (94.1%) had no knowledge of palliative care. A vast majority of caregivers intended to choose palliative care for patients (94.1%). The epidemic of COVID-19 affected the medical problems of a larger number of patients (60.0%) and the care of patients by caregivers (44.7%).
The Hospital Anxiety and Depression Scale Scores of Patients with Head and Neck Cancer and Their Caregivers
As shown in Table 2, the average HADS anxiety score for the patients was 7.4 (SD = 1.9), and the average HADS depression score for the patients was 6.4 (SD = 2.2). About half (56.47%) of the patients may have had anxiety. Meanwhile, the average HADS anxiety score for the caregivers was 8.2 (SD = 2.7), and the average HADS depression score for the CAREGIVERS was 8.4 (SD = 2.2). More than half of the caregivers (62.35%) may have had anxiety. Additionally, about one-third of the caregivers (38.83%) may have had depression.
 |
Table 2 The Hospital Anxiety and Depression Scale Among Head and Neck Cancer Patients and Family Caregivers |
Relationship Between the Chinese Version of the Connor and Davidson Resilience Scale and the Hospital Anxiety and Depression Scale
As shown in Table 2, the average CD-RISC score for the patients was 56.8 (SD = 12.6). The average score for the “Strength” dimension was 28.9 (SD = 7.02). The “Strength” and “Resilience” scores of the patients with HNC were inversely related to their HADS anxiety scores (r = −0.89, p < 0.05; r = −0.65, p < 0.05). The “Resilience” and “Optimism” scores of the patients with HNC were inversely related to their HADS depression scores (r = −0.61, p < 0.05; r = −0.81, p < 0.05) (Table 3).
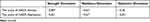 |
Table 3 Correlation Between the Chinese Version of the Connor and Davidson Resilience Scale and HADs (r) of Patients |
Correlation Between the Zarit Burden Interview of the Family Caregivers and the Hospital Anxiety and Depression Scale of the Patients with Head and Neck Cancer
In this study, the average ZBI score of the FCs was 23.8 (SD = 10.1). The results of Pearson’s correlation analysis are shown in Table 4. The HADS anxiety score of the FCs was positively associated with their total ZBI score and individual burden scores (r = 0.73, p < 0.05; r = 0.65, p < 0.05). The HADS depression score of the FCs was positively associated with their ZBI individual burden scores (r = 0.43, p < 0.05) (Table 4).
 |
Table 4 Correlation of Zarit Burden Interview of FCs and HADS (r) of Head and Patients with Head and Neck Cancer |
Discussion
Radiotherapy-related adverse reactions can lead to pain of HNC patients, which can resulting in dysphagia and its associated with caregiver distress and poorer quality of life for caregivers. Previous results showed that in the first year after the end of treatment, 60% of patients had dysphagia, 87% of patients complained of a dry mouth, and 58% experienced neck fibrosis. In studies comparing the caregiver burden of head and neck cancer and other types of malignancies, caregiver burden was higher for patients with HNC than for those with breast or ovarian cancer.22 Singer et al23 found that in patients with HNC, the depression/anxiety symptoms were 1.5 and 2.7 times more likely to occur at and after admission, respectively, compared with patients with other cancers. They also found the psychological distress of patients with head and neck cancer was almost 3 times that of patients with other tumors half a year after initial admission. However, tumor location alone does not appear to be a determinant. Patients with less social support were 3-fold more likely to experience emotional distress, and after controlling for this effect, the association between tumor location and distress was less pronounced.24 These studies all highlighted the significant contribution of the supportive role of FCs to reducing treatment distress and improving treatment outcomes for patients with HNC.
Resilience refers to the good adaptation process of individuals in the face of adversity, trauma, tragedy, threat, or other major pressures. This concept was first proposed by Anthony25 in the 1970s. It was borrowed from the concept of elasticity in physics to explain the phenomenon that some people can recover to the original state after external pressure, while some people cannot recover to the normal state in the short term. The data from this study indicate that patients with better psychological resilience tend to deal actively with the crisis and face possible treatment dilemmas. Good psychological elasticity is a protective factor and indicates internal strength for patients to deal with their disease, which can effectively improve their understanding of the condition and relieve their psychological pressure.26 Paek found that a good mental health function among the FCs of patients with HNC was associated with fewer difficulties regarding social contact (the primary stressor) and a lower caregiving burden (appraisal).27 Therefore, clinical healthcare staff must ensure they evaluate the anxiety and depression status of patients with HNC undergoing radiotherapy, as effective evaluation is the basis for providing the correct interventions. When a patient has anxiety and depression, we must provide timely counselling to improve their emotional state and help them face their disease.
Caregiver burden is defined as negative objective and subjective outcomes from physical, psychological, social and economic problems. Gosak et al,28 analyzing data from 180 pairs of patients and their family caregivers, found that FC was associated with greater financial and psychological stress in caring for others and also had higher scores on the “cancer worry”. Patients with HNC often have numerous medical appointments and are often accompanied by caregivers. These factors contribute to an increase in the negative impact on caregivers’ health during treatment and an increase in the cumulative stress associated with care.23 After treatment, the patient and caregiver may undergo a long recovery process, while the caregiver may continue to experience daily disruptions at this time. Additionally, we found that caregiver burden was positively correlated with the HADS scores of HNC patients. Fletcher et al29 showed that stressors, assessments, cognitive–behavioural responses, and contextual and cancer trajectory factors may be associated with physiological and psychological outcomes among the FCs of patients with cancer. In addition, the high FC burden may be related to the Confucian culture. The Confucian culture of upholding the family may be an influencing factor on the high burden of Chinese FCs.17 Therefore, strengthening effective communication, psychological counselling and nursing with FCs and enhancing attention to care needs will reduce the burden on the FCs to a certain extent.
Limitations and Perspective
This study has several limitations. First, the present study is that it was a single-centre trial study, and the number of included participants was relatively small. Second, this study did not collect the follow-up data of patients and their caregivers and could not reflect the possible psychological changes in patients and caregivers with an extension in chemotherapy time. Although this research respectively explored the psychological status of patients with HNC receiving radiotherapy and their FCs and investigated the correlation between them, it did not provide an in-depth discussion on the specific factors affecting the psychological status of caregivers. Nonetheless, despite these limitations, the analysis of patient/family responses to questions about experiencing cancer has profound value. In the future, we will further explore our understanding of the impact of age, gender, sociodemographic, complications and clinical factors on patients’ psychological status during treatment.
Conclusion
More than half of patients with HNC undergoing radiotherapy may have anxiety, and about a third may have depression. The anxiety and depression status of the FCs of patients with HNC undergoing radiotherapy is related to caregiver burden, deserving the attention of clinical medical staff.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
All participants participated voluntarily and provided written informed consent in accordance with the Declaration of Helsinki. Respondents were assured of confidentiality and anonymity.
Acknowledgments
We would like to thank the executives and participating staff of the hospital for their support and assistance.
Funding
There is no funding to report.
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest separately for this work.
References
1. Pan F. Immunotherapy opens a new era in the treatment of recurrent and metastatic head and neck tumors——2021《CSCO guidelines for the diagnosis and treatment of head and neck tumors》release. China Medical Herald. 2021;18(15):1–3.
2. Zhao C. Expert consensus on nutrition support therapy for head and neck cancer patients receiving radiotherapy. Chin J Radiat Oncol. 2018;27(01):1–6.
3. Lu Q, Zhang T, Zhang LC, et al. The change of skeletal muscle mass and its influencing factors in Head and Neck Cancer patients treated with radiotherapy. Chin Nurs Manag. 2020;20(3):338–343.
4. Branch of Radiation Oncology of Chinese Medical Association. Expert consensus on standardized management of radiotherapy nutrition. Chin J Radiat Oncol. 2020;29(5):324–331.
5. Ye W, Zuo HB, Cui WT, et al. Changes of NEUT and sTNF-RI in patients with head and neck tumors during radiotherapy and influencing factors for infection. Chin J Nosocomiol. 2020;30(24):3750–3753.
6. McDowell L, Rischin D, Gough K, Henson C. Health-related quality of life, psychosocial distress and unmet needs in older patients with head and neck cancer. Front Oncol. 2022;12:834068. doi:10.3389/fonc.2022.834068
7. Van Hof KS, Hoesseini A, Dorr MC, et al. Caregiver burden, psychological distress and quality of life among informal caregivers of patients with head and neck cancer: a longitudinal study. Int J Environ Res Public Health. 2022;19(23):16304. doi:10.3390/ijerph192316304
8. Blum K, Sherman DW. Understanding the experience of caregivers: a focus on transitions. Semin Oncol Nurs. 2010;26(4):243–258. doi:10.1016/j.soncn.2010.08.005
9. Streck BP, Wardell DW, LoBiondo-Wood G, Beauchamp JES. Interdependence of physical and psychological morbidity among patients with cancer and family caregivers: review of the literature. Psychooncology. 2020;29(6):974–989. doi:10.1002/pon.5382
10. Otto AK, Gonzalez BD, Heyman RE, Vadaparampil ST, Ellington L, Reblin M. Dyadic effects of distress on sleep duration in advanced cancer patients and spouse caregivers. Psychooncology. 2019;28(12):2358–2364. doi:10.1002/pon.5229
11. Bultz BD, Speca M, Brasher PM, et al. A randomized controlled trial of a brief psychoeducational support group for partners of early stage breast cancer patients. Psychooncology. 2000;9(4):303–313. doi:10.1002/1099-1611(200007/08)9:4<303::AID-PON462>3.0.CO;2-M
12. McGillivray HMK, Piccolo EEL, Wassersug RJ. “Partner”, “Caregiver”, or “Co-Survivor”-might the label we give the partners of cancer patients affect the health outcome of the patients and their partners? Curr Oncol. 2021;29(1):122–129. doi:10.3390/curroncol29010010
13. Levine DR, Van Noy K, Talleur AC, Snyder A, Kaye EC, Baker JN. Thoughts from the threshold: patient and family hopes, fears, values, and goals at the onset of pediatric hematopoietic cell transplantation. Bone Marrow Transplant. 2020;55(6):1103–1113. doi:10.1038/s41409-020-0794-8
14. Li J. Predictors of family caregiver burden in Shanghai. J Appl Gerontol. 2021;40(7):703–712. doi:10.1177/0733464820951029
15. Özcan Yüce U, Taşcı S. Effect of Reiki on the stress level of caregivers of patients with cancer: qualitative and single-blind randomized controlled trial. Complement Ther Med. 2021;58:102708. doi:10.1016/j.ctim.2021.102708
16. Li Q, Lin Y, Hu C, et al. The Chinese version of hospital anxiety and depression scale: psychometric properties in Chinese cancer patients and their family caregivers. Eur J Oncol Nurs. 2016;25:16–23. doi:10.1016/j.ejon.2016.09.004
17. Karlsson T, Johansson M, Finizia C. Well-being of caregivers of patients with laryngeal cancer treated by radiotherapy. Int Arch Otorhinolaryngol. 2020;24(2):e170–e174. doi:10.1055/s-0039-3399542
18. He Y, Bin J, Yang XH, et al. Correlation between the psychological resilience and the positive and negative emotions in patients with lung cancer during chemotherapy. Nurs J Chin People’s Lib Army. 2018;35(11):29–31. Chinese.
19. Yu XN, Zhang JX. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Soc Behav Person Int J. 2020;35(1):19–30. doi:10.2224/sbp.2007.35.1.19
20. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649–655. doi:10.1093/geront/20.6.649
21. Wang L, Yang XT, Hou Z, et al. Application and evaluation of Chinese version of zarit caregiver burden interview. Chin J Public Health. 2006;22(8):970–972.
22. Astrup GL, Hofsø K, Bjordal K, Rustøen T. Cancer patients’ diagnosis and symptoms and their family caregivers’ self-efficacy and social support are associated with different caregiver reactions. Eur J Cancer Care. 2020;29:e13311. doi:10.1111/ecc.13311
23. Singer S, Krauss O, Keszte J, et al. Predictors of emotional distress in patients with head and neck cancer. Head Neck. 2012;34(2):180–187. doi:10.1002/hed.21702
24. Eades M, Chasen M, Bhargava R. Rehabilitation: long-term physical and functional changes following treatment. Semin Oncol Nurs. 2009;25:222–230. doi:10.1016/j.soncn.2009.05.006
25. Troy AS, Willroth EC, Shallcross AJ, Giuliani NR, Gross JJ, Mauss IB. Psychological resilience: an affect-regulation framework. Annu Rev Psychol. 2023;74:547–576. doi:10.1146/annurev-psych-020122-041854
26. Qing Y, Bakker A, van der Meer CAI, Te Brake H, Olff M. Assessing psychological resilience: translation and validation of the Chinese version of the resilience evaluation scale (RES). Eur J Psychotraumatol. 2022;13(2):2133358. doi:10.1080/20008066.2022.2133358
27. Paek MS, Nightingale CL, Tooze JA, et al. Contextual and stress process factors associated with head and neck cancer caregivers’ physical and psychological well-being. Eur J Cancer Care. 2018;27(2):e12833. doi:10.1111/ecc.12833
28. Gosak M, Gradišar K, Rotovnik Kozjek N, et al. Psychological distress and nutritional status in head and neck cancer patients: a pilot study. Eur Arch Otorhinolaryngol. 2020;277(4):1211–1217. doi:10.1007/s00405-020-05798-y
29. Fletcher BS, Miaskowski C, Given B, et al. The cancer family caregiving experience: an updated and expanded conceptual model. Eur J Oncol Nurs. 2012;16(4):387–398. doi:10.1016/j.ejon.2011.09.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
