Back to Journals » Infection and Drug Resistance » Volume 16
Proteomic Study of Middle Ear Effusion and Its Clinical Application for Otitis Media with Effusion
Authors Wang X, Xu J, Feng G, Gao Z, Sun W
Received 25 June 2023
Accepted for publication 31 August 2023
Published 7 September 2023 Volume 2023:16 Pages 5923—5940
DOI https://doi.org/10.2147/IDR.S424475
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Xi Wang,1,* Jiyu Xu,2,* Guodong Feng,1 Zhiqiang Gao,1 Wei Sun2
1Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100730, People’s Republic of China; 2Institute of Basic Medical Sciences, School of Basic Medicine, Peking Union Medical College, Chinese Academy of Medical Sciences, Beijing, 100730, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhiqiang Gao; Wei Sun, Email [email protected]; [email protected]
Background: Proteins found in middle ear effusion play crucial roles in the physiological and pathological processes of otitis media with effusion (OME), influencing the etiology and clinical characteristics of this disease. The qualitative and quantitative composition of these proteins depending on the underlying pathogenesis of middle ear effusion. Understanding their physiological and pathological functions is of great importance.
Methods: We collected samples from 19 volunteers diagnosed with OME. After offline separation using high-pH reversed-phase liquid chromatography (RPLC), the pooled sample was subjected to LC-MS/MS analysis to obtain a comprehensive profile of the OME proteome. Functional analysis was performed using Gene Ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG), and Ingenuity Pathway Analysis (IPA) annotations. Data-independent acquisition (DIA) technology was utilized to analyze samples and fix whether the OME proteome could replicate the pathophysiological features associated with this disease. We conducted a differential proteomic analysis between patients with simple OME and patients who had received radiotherapy. The radiotherapy-reduced group was further divided into two subgroups: nasopharyngeal carcinoma (NPC) and other types of carcinoma. Parallel reaction monitoring (PRM) technology was used for validation of 36 differentially expressed proteins (DEPs).
Results: A number of 732 proteins were identified in the OME proteome database. Among them, 527 proteins were quantified using peak intensity-based semi-quantification (iBAQ), covering a wide dynamic range of approximately 8 orders of magnitude. Based on the functional analysis, we proposed a hypothetical mechanism of OME.
Conclusion: This study managed to put up an inclusive analysis of the OME proteome, establishing the first human OME proteome database. We focused on differential proteomic analysis among different groups to gain a more comprehensive concept of the OME proteome and search for meaningful biomarkers.
Keywords: otitis media with effusion, proteome, function annotation, radiotherapy-reduced OME, nasopharyngeal carcinoma
Introduction
Otitis media with effusion (OME), also known as secretory otitis media (SOM), is a prevalent cause of hearing loss worldwide, particularly among children.1 The disease affects approximately 0.6% of adults and 20% of 2-year-old children.1,2 Middle ear effusion commonly leads to conductive hearing loss. It can also have implications for language acquisition and learning, particularly in children.3 In this study, we focus on simple secretory otitis media and radiotherapy-reduced secretory otitis media, where the most common primary disease associated with the latter is nasopharyngeal carcinoma (NPC). However, the underlying pathophysiology of OME, especially at the gene and protein levels, remains incompletely understood.
OME was defined as an infection-free disease in the past.4 However, recent studies have challenged this definition by demonstrating bacterial colonization in the middle ear charge or mucosa of patients with OME. These findings have raised questions regarding the existing theories of the disease’s etiology. Over the past decade, several studies have investigated the pathophysiology of OME. For instance, Stabenau et al used RNA-Seq to identify differential gene expression in middle ear effusion, revealing implications for infectivity-related susceptibility and clinical management.5 Mahmood F. Bhutta’s study showed that upregulation of hypoxia signaling and the RANK-RANKL pathway were important in the pathophysiology of OME through genome-wide transcript analysis.6 However, there has been no proteomic study of middle ear effusion thus far. Previous studies have not provided analyses of the OME effusion proteome database or disease differential analyses.4–6 With advancements in proteomic techniques, a more inclusive analysis is needed to realize the function of middle ear effusion. Moreover, previous studies have indicated that the pathogenesis of OME is associated with immune response, coagulation activities, and inflammatory disorders.7 Further studies are obligatory to determine whether the function of disease differential proteins can reveal pathophysiological modifications in different groups.
Initially, we selected serum as the control group and performed GO and KEGG analyses to identify the specific characteristics of OME effusion. Subsequently, we conducted IPA analysis of proteins in the medium and low abundance groups of middle ear effusion to explore the differences in functional and canonical pathways between the two groups. Furthermore, we conducted a differential proteomic analysis between patients with simple OME and those who underwent radiotherapy, aiming to explain the distinct pathologies observed in these groups. Within the radiotherapy-reduced group, we further divided patients into two subgroups (NPC vs other carcinoma types). By analyzing the functions and pathways of the differential proteins, we hope to provide insights into the different pathologies observed. This study aims to enhance our understanding of the OME effusion proteome and expedite the application of otitis media research in clinic.
In the present study, we aimed to establish a comprehensive profile of OME effusion proteome and provide a detailed proteomic functional annotation. We also focus on differential proteomic analysis in order to have a better perspective of OME and its meaningful biomarker discovery. We believe our study could benefit the understanding of OME effusion proteome and accelerate the application of otitis media to clinical research.
Materials and Methods
Ethical Approval
Prior to enrolling participants in our study, a verbal clarification was provided to all volunteers, and each participant gave their informed consent by signing a consent form. The consent formula and experiment protocol were reviewed and officially approved by the Ethics Committee for Human and Animal Research at Peking Union Medical College (No. JS-3370). The study policies abide by the Declaration of Helsinki.
Clinical Materials
The OME effusion samples were collected from 19 patients during outpatient surgery. A total of 19 middle ear charge samples were obtained using a sterile procedure. It’s important to note that all patients had not received any form of treatment prior to sample collection. We allocated the samples into two groups: group one consisted of 12 samples from patients with simple OME, while group two consisted of 7 samples from patients with radiotherapy-reduced OME. Each sample was approximately 0.2–1.0 mL in volume and was aspirated from the middle ear of patients using a lumbar puncture needle (#7) under strict aseptic conditions. Following collection, the effusion samples were immediately transported and stored at −80°C for subsequent analysis.
Protein Extraction and Digestion
The OME samples were subjected to precipitation overnight at 4°C. The protein samples were subjected to digestion using the method published by Gravett et al. A total of 200 μg of protein samples was utilized for the digestion process. Initially, the samples were reduced and carbamidomethylated, 20mM DTT and 50mM IAM were used, respectively. Each protein sample was then supplemented with 4 μg of trypsin in 25 mM NH4HCO3 and incubated at 37°C for a whole night. These peptides were then subjected to desalting using a C18 SPE column (Waters Oasis) and subsequently lyophilized to prepare them for further experiments.
Offline HPLC
All the peptides obtained from the digestion were separated using a RPLC column. The eluting gradient involved using buffer B1, which contained 90% acetonitrile (ACN) with a pH of 10. The rate of flow was 1 mL per min.
LC/MS/MS
The MS analysis in both DDA-MS (Data-Dependent Acquisition MS) and DIA-MS (Data-Independent Acquisition MS) modes was performed using the Orbitrap Fusion Lumos tribrid mass spectrometer (Thermo Scientific, Bremen, Germany) together with the EASY-nLC 1000 system. 30 fractions obtained from RPLC separation were subjected to DDA mode analysis. We then set related parameters as follows: the cycle time was 3s; full scan was demanded the range of from m/z 400 to 1500 at 5,5000 resolution; we then put up auto gain control, also known as AGC, at the level of 1e6, meanwhile, the maximum level of injection time was 50 ms. For each individual sample, DIA mode analysis was conducted. A total of 38 isolation windows was developed in DIA method. The isolation windows ensured equal distribution of precursor ion numbers. The DIA scan setting: a resolution of 35,000 with 32% collision energy on HCD mode. All of the related MS data file and resources could be obtained at iProX (Integrated Proteome resources) with open access.
PRM Mass Spectrometry
The Parallel Reaction Monitoring analysis was conducted by the TripleTOF 5600 mass spectrometer. Separation was achieved using an RPC18 self-packing capillary LC column. The elution gradient employed was from 5% to 30% buffer B1 over a 60-minute period, with 0.35 mL/min flow rate.
Data Analysis
Spectronaut Pulsar and Skyline software were used to analyze the DIA data and PRM data with a default setting, which was applied in our previous study (Proteomic Study of Aqueous Humor and Its Application in the Treatment of Neovascular Glaucoma).8
Abundance Ranking
In our study, we use a specific algorithm to perform the abundance ranking of proteins we obtained from the former experiments. This algorithm is called intensity-based absolute quantification (iBAQ), following the procedure described by Schwanhausser et al. We then use Progenesis LC-MS software (V2.6, Non-linear Dynamics, United Kingdom) to process protein intensities which based on the method published by Hauck et al in 2010.
Each protein’s iBAQ value was provided by the division of the sum of peptide intensities. The sum value was calculated according to the theoretical protein peptides we managed to find out. In details, we referred to the approach published by Liu et al in 2017. They used silico protein digestion and considered tryptic peptides ranged from six to thirty aa as a whole. To obtain relative iBAQ values, we firstly divided absolute iBAQ values according to the sum of all the absolute iBAQ values we got, thereby normalizing these intensities. Estimated protein abundance was thereby computed by multiplying these relative iBAQ values according to molecular weight of corresponding protein.
Bioinformatics Analysis
In order to assign gene symbols to the differentially expressed proteins (DEPs), the investigators used the Panther database. The Panther database is a comprehensive resource that provides gene symbol annotations based on protein sequences. Gene Ontology (GO) was performed for the DEPs aiming to classify these proteins. This classification provides valuable information about the roles and functions of the proteins in various biological contexts. To analyze protein-protein interactions, the DEPs were uploaded to the STRING database, which is a widely used resource for studying protein interactions and functional associations. A minimum interaction score of 0.4 was set to ensure the reliability of the predicted interactions. The biomolecular interaction networks obtained from the STRING database were visualized and analyzed using the software Cytoscape and its plugins. Cytoscape is a popular tool for network visualization and analysis, and it provides various plugins that enhance its functionality.
For further analysis of the DEPs, the investigators utilized Ingenuity Pathway Analysis (IPA) software. The SwissProt accession proteins numbers were uploaded to IPA, which is a powerful tool for exploring biological pathways, diseases, and functional annotations. The results were ranked based on the P-value, indicating the significance of the associations between the DEPs and the identified pathways or functions.
Results
Clinical Results
Among the 19 enrolled patients, 8 were females and 11 were males, resulting in a gender distribution of approximately 42.1% females and 57.9% males. The average age of the patients was 47.10 years, with a range of 27 to 68 years. Regarding the affected side of the disease, 10 patients had OME on the left ear, while the remaining 9 patients had it on the right ear. The degree of hearing loss among the patients varied from mild to moderate and severe. Specifically, 6 patients suffered from mild hearing loss, 6 patients were of moderate-severe hearing loss and the remaining patients had moderate hearing loss (Table 1).
 |
Table 1 Clinical Information of 19 Patients with Otitis Media with Effusion |
OME Proteome Analysis Workflow
We aimed to establish a comprehensive description of OME proteome using 19 samples obtained from patients with otitis media with effusion. All OME samples were pooled into a single sample, which was then subjected to digestion and evaluated using 2D-RP-RP LC-MS/MS. To reduce interference from high-abundance proteins. Since there was no previous OME proteome analysis available, we used serum as a control group for comparative analysis. GO annotation and IPA analysis were performed for functional analysis, providing insights into the biological functions and pathways associated with OME (Figure 1).
To further investigate the etiology of OME, the 19 samples were allocated into two experimental groups: simple OME group (12 samples) and radiotherapy-reduced group (7 samples). Within the radiotherapy-reduced group, we further subdivided the samples based on the primary tumor pathological diagnosis, distinguishing between nasopharyngeal carcinoma (NPC) and other types of tumors. This subgrouping aimed to identify differential proteins among different tumor types associated with OME. DIA technique was used for protein quantification. PRM technology was used for validation thereafter. A subset of 17 samples was subjected to PRM analysis, allowing for targeted and accurate quantification of the selected proteins of interest. In order to ensure the stability and reliability of the experiment results, we also carried out quality control (QC) on the samples we collected (Figure 2).
Overall, our study provides insights into the OME proteome, its functional annotations, and the identification of differential proteins associated with different tumor types and radiotherapy response.
Database Establishment of the OME Proteome
After we analyzed gathered samples using 2D-LC/MS/MS, a total of 4337 peptides were eventually identified, corresponding to 732 proteins, among them 392 proteins were put up with the standard of unique peptides no less than 2. We provide quantitative proteomic analysis through iBAQ algorithm. The total range of relative abundance covered 8 magnitude orders (Figure 3). The comparison between serum and OME effusion revealed significant differences in molecular function and cellular component (Figure 4). In terms of molecular function, proteins involved in molecular function regulation and protease regulation activity were upregulated in OME effusion compared to serum. On the other hand, transporter activity was more prominent in the serum group. These findings suggest differences in the functional activities of proteins between OME effusion and serum.
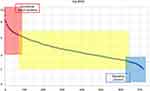 |
Figure 3 Protein abundance rank. Quantitative protein abundance range in OME samples with an iBAQ algorithm (left y-axis) and cumulative protein abundances of the OME proteome (right y-axis). |
 |
Figure 4 Venn diagram of protein identification in OME patients’ middle ear charge and serum from healthy volunteers. |
Regarding cellular component, chronic inflammatory response was higher in OME effusion compared to serum. However, no substantial differences were found between these two groups according to protein-containing complexes or synapse-related processes. This suggests that OME effusion is similar in composition to serum but exhibits distinct cellular components and molecular functions, particularly related to immune responses and inflammatory processes, highlighting the characteristics of disease occurrence and development.
We adopted PANTHER classification system to performed GO analysis aiming to revealed enrichment in cellular processes and immune responses in the cellular component category (Figure 5). The major molecular functions of OME proteins were related to binding as well as immunoglobulin receptor regulation. In terms of biological processes, OME proteins primarily participated in cell and extracellular region processes.
 |
Figure 5 GO analysis of the OME proteome compared with the serum proteome ((A) GO-biological process, (B) GO-cellular component and (C) GO-molecular function). Abbreviation: GO, Gene Ontology. |
The IPA pathway analysis identified several pathways associated with OME, including cell death and survival (necrosis and apoptosis), immunological diseases (hypersensitive reactions, allergies, psoriasis, and systemic autoimmune syndrome), and inflammatory responses (chronic inflammatory disorders, inflammation of organs, classical complement pathway, complement activation, and degranulation of cells). Proteins took part in immune cell adhesion, binding of blood cells, activation of cells, and binding of leukocytes, were also identified. These findings suggest the involvement of immune and inflammatory processes in the mechanism of OME (Figure 6).
In order to provide quantitative proteomic analysis, the iBAQ algorithm was employed, quantifying 527 proteins in the OME proteome. The total range of relative abundance covered 8 magnitude orders. The ranked analysis of these proteins based on abundance revealed different categories: high-abundance proteins (>95%), medium-abundance proteins (95–99%), and low-abundance proteins (<1%). The canonical pathway analysis of medium and high-abundance proteins revealed their involvement in inflammatory/immune-related pathways (eg, acute phase response signaling and complement system signaling), as well as coagulation-related pathways. In contrast, low-abundance proteins were associated with protein synthesis-related pathways (proteolysis, cleavage of protein in fragments, hydrolysis of protein, and metabolism of cellular protein), as well as inflammatory/immune-related pathways (allergy, hypersensitive reaction, chronic inflammatory disorder, inflammation of organs, classical complement pathway, complement activation, and degranulation of cells).
Table 2 of the study shows that the top 8 abundant proteins made up for about 76% of all the OME proteins. Half of them belonged to the immunoglobulin family. Notably, one of the most abundant proteins in OME was Albumin (ALB), with the accession number P02768.
 |
Table 2 The 8 Top Abundant Proteins in Normal AF Proteome |
ALB is known to be the most plentiful protein in human blood. ALB plays a crucial part in regulating blood serum colloid osmotic pressure. It also serves as a carrier for hormones, fatty acids, metabolites, and exogenous drugs. The abundance of albumin in the middle ear charge supports the theory that middle ear effusion is essentially an exudate originating from serum. This finding provides additional support for the use of serum as a control group in this study.
The Differential Proteomic Analysis of OME with Different Etiology
In this study, a total of 549 proteins were found proceeding by DIA method among OME samples, which were thereafter divided into two groups according to different etiologies: the simple OME group and the radiotherapy-reduced OME group. A clear distinction between these two groups was observed in the PLS-DA score plot, indicating significant differences (P = 1.69145e-07). Out of the 549 proteins, 120 proteins were defined as differentially expressed proteins (DEPs). Among these DEPs, 119 were upregulated and 1 was downregulated (Figure 7). According to GO annotation. The DEPs were mainly located in extracellular region and were basically involved in the cellular-related processes and maintenance processes. Their molecular functions were enriched in binding activities, coagulation processes, and cell-to-cell signaling. These findings suggest that the DEPs play important roles in intercellular communication and coagulation.
Furthermore, the IPA analysis identified 10 significantly involved pathways (Figure 8). It was observed that pathways including complement system, LXR/RXR activation and cell maturation were significantly suppressed in OME samples. These results provide insights into the molecular alterations and functional changes associated with different etiologies of OME. The downregulation of specific pathways related to complement activation, coagulation, and cell maturation suggests potential dysregulation in immune response, coagulation processes, and tissue maturation in OME.
The Differential Proteomic Analysis of Radiotherapy-Reduced OME with Different Kinds of Tumor
In the study, the radiotherapy-reduced OME group was further divided into two subgroups based on the primary tumor type: NPC (nasopharyngeal carcinoma) and other kinds of carcinoma (Table 3). An OPLS-DA score plot was used to visualize the differences between these subgroups, revealing significant distinctions (P = 1.59621e-07).
 |
Table 3 Clinical Information of 7 Patients in Radiotherapy-Reduced OME Group |
A number of 37 differentially expressed proteins (DEPs) were found in these subgroups, with a fold change no less than 2.0 as well as the p-value of 0.05. Among these DEPs, 14 were upregulated, while 23 were downregulated (Figure 9).
Our functional analysis of these DEPs indicated enrichment in pathways such as LXR/RXR activation, acute phase response signaling, coagulation system, and complement activation (Figure 10). These findings align with the canonical pathways observed in the DEPs of the other two groups. However, it was also noted that these DEPs were primarily associated with cancer, organismal injuries, and abnormalities, including serous adenocarcinoma, benign solid tumors, low-grade acinar-cell carcinoma, and glandular intraepithelial neoplasm. Furthermore, they were involved in cellular functions and maintenance, such as chemotaxis and invasion of tumor cell lines. This functional analysis of DEPs in the NPC and other carcinoma subgroups differed from that of the DEPs in the first two groups.
These findings provide a deeper understanding of the etiology of different types of OME. The distinct functional characteristics observed in the DEPs of the NPC and other carcinoma subgroups suggest potential differences in underlying mechanisms and pathogenic processes associated with these specific tumor types.
PRM Validation
The PRM (Parallel Reaction Monitoring) validation was conducted on 17 randomly selected samples from the original samples. PRM variation was assessed by computing the coefficient of variation (CV) of peptide abundance in three quality control (QC) replicates, resulting in a high correlation coefficient of R2=0.975. Through PRM analysis, a total of 36 peptides corresponding to 19 proteins were validated, and all of them were found to be upregulated. In the comparison between the first two groups (simple OME group vs radiotherapy-reduced OME group), 14 upregulated proteins were validated. In the comparison between the latter two groups (NPC group vs Other tumors group), 3 upregulated proteins and 1 downregulated protein were validated. These results were consistent with the findings from the experimental groups.
Among the validated proteins, several specific peptides were identified, including 3 peptides from the G4m marker, 3 peptides from the complement C1q B chain, 2 peptides from HIST1H2BJ, and 2 peptides from immunoglobulin lambda. Additionally, peptides from key proteins such as IGKC, defensin alpha 3, and vitamin D binding protein were also validated, showing a similar trend among peptides from the same protein (Figure 11). The functional and pathway analysis of the validated differentially expressed proteins (DEPs) indicated significant involvement in thrombosis, apoptosis, immune response of cells, and inflammation of the body cavity. These findings align with the main pathways identified in the analysis of the entire set of DEPs, further supporting their correlation with the pathological changes observed in secretory otitis media.
Discussion
We established a comprehensive profile of the human middle ear effusion proteome, with a number of 732 proteins was identified. Our data serves as a valuable baseline for understanding the proteomic composition of otitis media with effusion (OME). By conducting differential analysis of the OME proteome in different groups, we were able to validate two sets of differentially expressed proteins (DEPs). These DEPs may play crucial roles in the pathological process of OME. The identification and validation of these DEPs provide valuable insights into the molecular mechanisms and potential biomarkers associated with OME. We believe our findings could lead to a more comprehensive perspective of OME at proteomic level and enhances our knowledge of biomarker discovery in this condition. The findings of our research have the potential to impact the diagnosis and treatment of this disease by uncovering key proteins involved in the disease process.
The Clinical Etiology of Otitis Media with Effusion
The formation of middle ear charge and the source of proteins in OME have been subjects of discussion in the field.1,2 This specific disease is typically characterized by the presence of yellow clear liquid or jelly-like mucus in the middle ear. It is considered non-purulent, and bacterial culture results are usually negative.9 As a result, OME is often classified as a non-infectious condition according to consensus guidelines such as the International Consensus of the World Federation of Otorhinolaryngology (2017, Paris), which defines OME as middle ear effusion without signs of ear infection.
However, some researchers believe that bacterial infection and the associated inflammatory response have an impact on the onset of OME.10 Previous experiments have explored the connection between infection and radiotherapy-reduced OME as well.9,10 It is proposed that after radiotherapy, tumor cell necrosis and damage to normal mucosal tissue in the nasopharynx can lead to the formation of adherent necrotic scabs.11 These scabs can persist and promote bacterial growth and infection, particularly in individuals with compromised immunity. Patients may experience a foul smell in the nasal cavity, and examination may reveal necrotic pus and scabs in the nasopharynx.12 Reflex sinusitis following radiotherapy can also contribute to bacterial colonization in the nasopharynx, leading to obstruction and accumulation of middle ear effusion due to eustachian tube swelling and adhesion.13 Furthermore, some studies have highlighted the potential involvement of allergic processes in OME.14 Biochemical and immunological diagnostic methods, such as the detection of immune factors and immune cells in vivo, have been applied in the clinical diagnosis of OME. Tumor necrosis factor-alpha (TNF-a), various kinds of interleukin and other immune factors have been studied.15,16 Additionally, CD4+ T cells and CD8+ T cells have been investigated as immune cell markers in OME.17
These various lines of research contribute to our understanding of the multifactorial nature of OME, involving factors such as bacterial infection, inflammatory responses, radiotherapy-related changes, and allergic processes. Further exploration of biochemical and immunological markers may help in the diagnosis and management of OME.
Comparison of OME and Serum Proteome
Our study findings regarding the abundance of albumin and other proteins in OME and serum support the hypothesis that middle ear effusion is essentially derived from serum. The presence of albumin, which is known for its role in transporting various substances to cells, suggests that the proteins found in OME are similar to those present in serum. This also justifies the use of serum as a control group in our trial. Furthermore, the high abundance of immunoglobulin kappa constant, immunoglobulin heavy constant gamma 2, transferrin, serpin family A member 1, immunoglobulin heavy constant alpha 1, and haptoglobin in OME indicates their involvement in the middle ear effusion.
Pathway analysis in our study indicated that the common proteins in OME are basically associated with immune process and inflammatory-related procedures, such as hypersensitive reactions, allergies, psoriasis, systemic autoimmune syndrome, chronic inflammatory disorders, inflammation of organs, and the classical complement pathway. These pathways collectively account for 35% of the quantitative protein abundance. This suggests that immune and inflammatory processes play a significant role in OME.
In terms of gene ontology (GO) analysis, proteins in OME were found to be located in the extracellular region and supramolecular complexes. They were involved in immune response, blood coagulation, regulation of fibrinolysis, and chronic inflammation at the cellular component level. In molecular function, proteins in the middle ear charge were notably enriched in protease regulator activity compared to serum. This finding indicates that although middle ear effusion originates from ‘serum, it may have specific functions related to coagulation, immune response, and inflammation, which are crucial aspects of the development and progression of secretory otitis media.
Overall, these observations provide valuable insights into the proteomic characteristics of OME and shed light on the roles of various proteins and pathways in the pathogenesis of secretory otitis media.
DEPs Functional Analysis Between Simple OME and Radiotherapy-Reduced OME
Simple OME is the most common type of secretory otitis media, particularly among young population.18 It is characterized by middle ear effusion without a clear underlying cause, such as congenital eustachian tube malformation or previous surgery or radiotherapy involving the eustachian tube.19 Simple OME can lead to hearing loss, especially in the 10 years following radiotherapy for nasopharyngeal carcinoma, significantly impacting patients’ quality of life.20 Prolonged middle ear effusion can result in irreversible damage, including tympanic atrophy, tympanic sclerosis, and auditory bone necrosis.20,21 On the other hand, radiotherapy-reduced OME is a common complication in individuals who have undergone radiotherapy aiming to treat malignant lesions in head and neck area.9 Conventional two-dimensional radiotherapy (2DRT) can lead to various ear-related issues and malfunction of Eustachian tube is just one of them.22 Post-radiation OME is a prevalent otologic adverse effect observed among patients with NPC treated with radiotherapy.9,22
Although the basic etiology of both types of secretory otitis media involves neg-pressure in patient’s tympanic cavity resulting in the exudation of capillary blood serum and the formation of middle ear effusion, the course and characteristics of the diseases differ.2 Hence, our study aimed to explore the differences between the two types of secretory otitis media at the protein level. From the division of samples into the simple OME group (N=12) and the radiotherapy-reduced OME group (N=7), we managed to find significant differences between these two experimental groups according to OPLS-DA score plot (P = 1.69145e-07) and heatmap analysis. Through further analysis using a volcano plot, we identified 120 differentially expressed proteins (DEPs) with the defined fold change over 2.0 together with a p-value of 0.05, including 119 upregulated DEPs and 1 downregulated DEP.
The gene ontology (GO) annotation analysis revealed that the DEPs were mainly located in the extracellular region and participated in cellular processes and maintenance processes. Their functions were enriched in binding, coagulation processes, and cell-to-cell signaling. Additionally, Ingenuity Pathway Analysis (IPA) indicated significant involvement of 10 pathways. Notably, the complement system, coagulation system, LXR/RXR activation, and cell maturation pathways were significantly suppressed in radiotherapy-reduced OME compared to simple OME. These findings suggest that proteins in radiotherapy-reduced OME are more likely to be involved in inflammatory responses and protein synthesis, highlighting the potential influence of radiotherapy on the molecular processes of OME.
Previous studies have suggested a relationship between OME and infection, particularly bacterial infection.23 PCR technology has allowed detecting various microorganism in the middle ear charge, with the bacterial spectrum being consistent with that of the adenoid.24 Common detected pathogenic bacteria include Haemophilus influenzae, Streptococcus pneumoniae, and, in some cases, Staphylococcus aureus.25 The high prevalence of Staphylococcus aureus in adult middle ear effusion suggests that bacteria, including Staphylococcus aureus, may be a likely cause of OME, especially in cases of simple secretory otitis media.25 Regarding the protein synthesis-related pathways, the findings may be associated with the hypermetabolic nature of tumors.9 Malignant tumors exhibit biological characteristics that lead to metabolic disturbances, including increased protein synthesis.26 Our research also identified differential proteins related to cell metabolism, supporting the notion of altered protein metabolism in OME, particularly in radiotherapy-reduced OME.
Overall, our study provides valuable insights into the differences between simple OME and radiotherapy-reduced OME at the protein level, highlighting the potential role of inflammation, infection, and altered protein synthesis in the pathogenesis of these conditions.
DEPs Functional Analysis Between Different Tumors in Radiotherapy-Reduced OME
In our subgroup, our team further put the patients into two categories: NPC group (N=5) and other types of head and neck carcinoma group (N=2), both of which included cases of carcinoma of the gingiva. The analysis of differentially expressed proteins (DEPs) using the same approach revealed significant differences between these two groups based on the OPLS-DA score plot (P = 1.59621e-07). A total of 37 DEPs were identified. Among them, 14 proteins were upregulated while 23 of them were downregulated.
The functional analysis of these DEPs showed enrichment in the LXR/RXR pathway, coagulation system and complement-related bio-processes. What’s more, signal transfer in acute response phase was also discovered meaningful in our study. These results were actually in accordance with those canonical pathways found in previous analysis of the other two groups. However, it was noted that these DEPs were mainly associated with cancer, organismal injury (including serous adenocarcinoma, benign solid tumor, low-grade acinar-cell carcinoma, and glandular intraepithelial neoplasm), and cellular function and maintenance (chemotaxis and invasion of tumor cell lines). This functional profile differed from the DEPs observed in the first two groups, indicating unique molecular characteristics in the radiotherapy-reduced OME subgroup, particularly in the context of different primary tumor types.
Interestingly, LXR/RXR pathway was found enriched in the DEPs of both the radiotherapy-reduced OME group and the NPC subgroup suggests a potential relationship between OME and lipid metabolism. The LXR/RXR pathway, associated with lipid metabolism, has been implicated in intracellular lipid accumulation.27 Excessive intracellular lipid accumulation can lead to various pathological processes, including endoplasmic reticulum stress, apoptosis, inflammation and also the stress of endoplasmic reticulum, collectively referred to as “lipotoxicity”.28,29 This finding raises the possibility that the occurrence and progression of OME may be related to alterations in lipid metabolism, warranting further investigation in future studies. Our research has provided valuable insights into the molecular characteristics of radiotherapy-reduced OME, specifically in the context of different primary tumor types. The identification of unique DEPs and enrichment of specific pathways shed light on the potential involvement of lipid metabolism and its association with lipotoxicity in OME. These findings contribute to the understanding of the underlying mechanisms and may guide future investigations in this field.
Studies in recent years have indicated that inflammatory factors play an important role in middle ear’s response, leading to the release of mediators such as leukokines and prostaglandins by the mucosa.26,30 These mediators increase vascular permeability, resulting in tympanic mucosal edema, exudate formation, and the development of OME.30 Allergic reactions are believed to be involved in this process, and certain factors have been identified in OME middle ear effusion following radiotherapy for nasopharyngeal carcinoma, including endotoxin and cytokines including IL-1B, TNF-a and so on.26 Furthermore, the presence of eosinophils in those tympanic effusion suggests a potential link between the middle ear and allergic reactions.31 The middle ear mucosa shares a similar allergic reaction mechanism with other mucosal tissues, supporting the rationale for hormone therapy in managing OME. The concordance of our study’s findings with these existing theories further strengthens the credibility of our research. Understanding the involvement of allergic reactions in OME can have implications for the development of targeted therapies or interventions aimed at modulating the inflammatory response and alleviating symptoms associated with OME. Further exploration of the specific mechanisms underlying allergic reactions in middle ear would probably provide valuable insights for development of new treatment approaches in the future.
Treatment Options for Otitis Media with Effusion
The treatment options for secretory otitis media mainly include surgical treatment and conservative drug treatment. Surgical treatment generally refers to tympanic membrane puncture or tympanostomy tube incision,32 while conservative drug treatment generally uses antibiotics and adenoids. Although some guidelines have clearly pointed out that these two types of drugs should not be prescribed to patients with OME,33 some patients, especially children, who still receive antibiotics and corticosteroids for treatment.34 The results of our study suggest that some middle ear effusion proteins are related to inflammation, but the prominent portion is related to immunity, cell cycle, function and cell maintenance. Therefore, we hold the opinion that antibiotics should not be used for secretory otitis media treatment in the first place, which is consistent with the results of some previous study.33 On the other hand, previous studies have reported that injecting protease into the tympanic cavity cloud relieve symptoms.35 According to our study, the abundance and relative concentration of middle ear effusion proteins are relatively high and some proteins are richer than those in human serum. As a result, it is reasonable to increase the fluidity of effusion and drainage of the middle ear charge by injecting protease to enzymatically digest proteins. Regarding the conclusion that children received antibiotic treatment with obvious effect, we believe that the reason for this result may be that children usually have adenoid hypertrophy contributed to upper respiratory tract infection, which affects the function of eustachian tube and leads to OME. Therefore, it is reasonable that the use of antibiotics can effectively alleviate the primary disease and relieve symptoms secretory otitis media. However, the specific indications and standards of medication still need further discussion and research.
Conclusion
The OME proteome holds great potential as a base of biomarkers which could help us to identify the relevant pathophysiological variations. We believe our study could present a foundational reference for studies related to OME in the future by setting up a descriptive database of OME protein for the first time. We also focus on differential proteomic analysis in different groups in order to have a better promising perspective of proteomic analysis of otitis media with effusion and its meaningful biomarker discovery, which may provide data basis for diagnosis and clinical intervention of otitis media with effusion in the future.
Funding
This work was sponsored in part by Beijing Municipal Health Commission Capital Health Development Research Special Project (2020-2Z-40115).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhang J, He J, Luo Y, Liu Y, Fan X. miR-210 regulates the inflammation of otitis media with effusion by inhibiting the expression of hypoxia-inducible factor (HIF)-1a. Biochem Biophys Res Commun. 2021;534:401–407. doi:10.1016/j.bbrc.2020.11.068
2. Yukkaldıran A, Erdoğan O, Kaplama ME. Neutrophil-lymphocyte and platelet-lymphocyte ratios in otitis media with effusion in children: diagnostic role and audiologic correlations. Int J Clin Pract. 2021;75(3):e13805. doi:10.1111/ijcp.13805
3. Wu ZH, Tang Y, Niu X, Sun HY, Chen X. The relationship between otitis media with effusion and gastroesophageal reflux disease: a meta-analysis. Otol Neurotol. 2021;42(3):e245–e253. doi:10.1097/MAO.0000000000002945
4. Takahashi M, Oka A, Kariya S, et al. IgG4 expression in patients with eosinophilic otitis media. ORL J Otorhinolaryngol Relat Spec. 2021;83(3):167–171. doi:10.1159/000512726
5. Stabenau KA, Zimmermann MT, Mathison A, et al. RNA sequencing and pathways analyses of middle ear epithelia from patients with otitis media. Laryngoscope. 2021;131(11):2590–2597. doi:10.1002/lary.29551
6. Mahmood F, Khan A, Hussain R, et al. Patho-bacteriological investigation of an outbreak of Mycoplasma bovis infection in calves - emerging stealth assault. Microb Pathog. 2017;107:404–408. doi:10.1016/j.micpath.2017.04.003
7. Lechien JR, Hans S, Simon F, et al. Association between laryngopharyngeal reflux and media otitis: a systematic review. Otol Neurotol. 2021;42(7):e801–e814. doi:10.1097/MAO.0000000000003123
8. Yu M, Xie F, Liu X, et al. Proteomic study of aqueous humor and its application in the treatment of neovascular glaucoma. Front Mol Biosci. 2020;7:587677. doi:10.3389/fmolb.2020.587677
9. Na G, Kim KH, Byun HK, Bae SH. Assessment of radiation-induced otitis media in patients with parotid gland malignancy. Acta Otolaryngol. 2021;141(5):466–470. doi:10.1080/00016489.2021.1892184
10. Boers SA, de Zeeuw M, Jansen R, et al. Characterization of the nasopharyngeal and middle ear microbiota in gastroesophageal reflux-prone versus gastroesophageal reflux non-prone children. Eur J Clin Microbiol Infect Dis. 2018;37(5):851–857.
11. Li X, Ye M. The expression of VEGF and VEGFR in endotoxin induced otitis media with effusion in rats. Int J Pediatr Otorhinolaryngol. 2021;144:110669. doi:10.1016/j.ijporl.2021.110669
12. Chen T, Ashman PE, Bojrab DI 2nd, et al. Diagnosis and management of eosinophilic otitis media: a systematic review. Acta Otolaryngol. 2021;141(6):579–587. doi:10.1080/00016489.2021.1901985
13. Daval M, Picard H, Bequignon E, et al. Chronic otitis media with effusion in chronic sinusitis with polyps. Ear Nose Throat J. 2018;97(8):E13–E18. doi:10.1177/014556131809700803
14. Sharifian MR, Mahmoudi M, Pourmomenarabi B, Keramati MR. Correlation between allergic rhinitis and otitis media with effusion. Iran J Otorhinolaryngol. 2019;31(105):209–215.
15. Bodmer D, Kern P, Bächinger D, Monge Naldi A, Levano Huaman S, Monsanto RDC. STAT1 deficiency predisposes to spontaneous otitis media. PLoS One. 2020;15(9):e0239952. doi:10.1371/journal.pone.0239952
16. Elbistanli M, Koçak H, Acipayam H, Yiğider A, Keskin M, Kayhan F. The predictive value of neutrophil-lymphocyte and platelet-lymphocyte ratio for the effusion viscosity in otitis media with chronic effusion. J Craniofac Surg. 2017;28(3):e244–e247. doi:10.1097/SCS.0000000000003452
17. Ersoy B, Aktan B, Kilic K, Sakat M, Sipal S. The anti-inflammatory effects of erythromycin, clarithromycin, azithromycin and roxithromycin on histamine-induced otitis media with effusion in Guinea pigs. J Laryngol Otol. 2018;132(7):579–583. doi:10.1017/S0022215118000610
18. Buzatto GP, Tamashiro E, Proenca-Modena JL, et al. The pathogens profile in children with otitis media with effusion and adenoid hypertrophy. PLoS One. 2017;12(2):e0171049. doi:10.1371/journal.pone.0171049
19. Francis NA, Cannings-John R, Waldron C-A, et al. Oral steroids for resolution of otitis media with effusion in children (OSTRICH): a double-blinded, placebo-controlled randomised trial. Lancet. 2018;392(10147):557–568. doi:10.1016/S0140-6736(18)31490-9
20. Gan R, Daniel M, Ridley M, Barry J. Quality of questionnaires for the assessment of otitis media with effusion in children. Clin Otolaryngol. 2018;43(2):572–583. doi:10.1111/coa.13026
21. Hafrén L, Pajari M, Vento S, Saarinen R. Otitis media with effusion in aspirin-exacerbated respiratory disease patients-A series of 22 cases. Clin Otolaryngol. 2018;43(5):1387–1391. doi:10.1111/coa.13150
22. Akazawa K, Doi H, Ohta S, et al. Relationship between Eustachian tube dysfunction and otitis media with effusion in radiotherapy patients. J Laryngol Otol. 2018;132(2):111–116. doi:10.1017/S0022215118000014
23. Jung SY, Kim D, Park DC, et al. Immunoglobulins and transcription factors in otitis media. Int J Mol Sci. 2021;22:3201.
24. Yazıcı H. Nasal mucociliary clearance in adenoid hypertrophy and otitis media with effusion. Curr Allergy Asthma Rep. 2015;15(12):74. doi:10.1007/s11882-015-0576-3
25. Hoon K, Gu K, Seon S, Su K, Il K, Geun Y. Lower Beclin-1 mRNA levels in pediatric compared with adult patients with otitis media with effusion. J Int Adv Otol. 2018;14:48–52. doi:10.5152/iao.2018.4481
26. Yeghaneh Moghaddam A, Talaei R, Nikoueinejad H, Akbari H. Studying the serum as well as serous level of IL-17 and IL-23 in patients with serous otitis media. Iran J Allergy Asthma Immunol. 2017;16(6):520–524.
27. Jung S, Kim S, Kim Y, Kim H, Kim S, Yeo S. Expression of aquaporins mRNAs in patients with otitis media. Acta Otolaryngol. 2018;138(8):701–707. doi:10.1080/00016489.2018.1447685
28. Jung SY, Kwon KJ, Min HK, et al. Expression of endoplasmic reticulum stress mRNAs in otitis media. Acta Otolaryngol. 2021;141(5):459–465. doi:10.1080/00016489.2021.1883733
29. Kondyarpu A, Ray CS, Panda KC, Biswal NC, Ramchander PV. Association of ISL1 polymorphisms and eosinophilic levels among otitis media patients. J Clin Lab Anal. 2021;35(3):e23702. doi:10.1002/jcla.23702
30. Val S, Jeong S, Poley M, et al. Purification and characterization of microRNAs within middle ear fluid exosomes: implication in otitis media pathophysiology. Pediatr Res. 2017;81(6):911–918. doi:10.1038/pr.2017.25
31. Ueki S, Ohta N, Takeda M, Konno Y, Hirokawa M. Eosinophilic otitis media: the aftermath of eosinophil extracellular trap cell death. Curr Allergy Asthma Rep. 2017;17(5):33. doi:10.1007/s11882-017-0702-5
32. Rosenfeld RM, Shin JJ, Schwartz SR, et al. Clinical practice guideline: otitis media with effusion (update). Otolaryngol Head Neck Surg. 2016;154(1):S1–S41. doi:10.1177/0194599815623467
33. Simon F, Haggard M, Rosenfeld RM, et al. International consensus (ICON) on management of otitis media with effusion in children. Eur Ann Otorhinolaryngol Head Neck Dis. 2018;135(1S):S33–S39. doi:10.1016/j.anorl.2017.11.009
34. Spoială EL, Stârcea IM, Ioniuc IK, et al. Watchful waiting in pediatric acute otitis media: a real practice approach or an intangible desideratum? Medicina. 2023;59(3):520. doi:10.3390/medicina59030520
35. Guo X, Olszewski E, Fan Z, et al. Expression of surfactant protein-A during LPS-induced otitis media with effusion in mice. Otolaryngol Head Neck Surg. 2015;153(3):433–439. doi:10.1177/0194599815587699
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.








