Back to Journals » International Journal of General Medicine » Volume 16
Prospective Exploratory Study of the Effects of Postoperative Endocrine Medication on the Endometrium in Breast Cancer Patients
Authors He Y, Li YH, Geng YN, Liu A, Gao FY, Ji C, Liu Y, Wang M, Li XM, Wang Y, Wu YM
Received 20 April 2023
Accepted for publication 8 August 2023
Published 22 August 2023 Volume 2023:16 Pages 3677—3687
DOI https://doi.org/10.2147/IJGM.S417965
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Yue He,1 Yu-He Li,1 Yu-Ning Geng,1 Aihui Liu,2 Feng-Yun Gao,3 Chen Ji,1 Yang Liu,1 Ming Wang,1 Xing-Ming Li,4 Yan Wang,1 Yu-Mei Wu1
1Department of Gynecological Oncology, Beijing Obstetrics and Gynecology Hospital, Capital Medical University; Beijing Maternal and Child Health Care Hospital, Beijing, People’s Republic of China; 2Department of Breast, Beijing Obstetrics and Gynecology Hospital, Capital Medical University; Beijing Maternal and Child Health Care Hospital, Beijing, People’s Republic of China; 3Department of Ultrasonography, Beijing Obstetrics and Gynecology Hospital, Capital Medical University; Beijing Maternal and Child Health Care Hospital, Beijing, People’s Republic of China; 4School of Public Health Management, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Yu-Mei Wu, Department of Gynecological Oncology, Beijing Obstetrics and Gynecology Hospital, Capital Medical University; Beijing Maternal and Child Health Care Hospital, Dongcheng District, Qi-he-lou Street No. 17, Beijing, 100006, People’s Republic of China, Email [email protected]
Objective: This study aimed to investigate the pathological effects of long-term postoperative endocrine medication on the endometrium in breast cancer patients.
Methods: Data of 99 patients with primary breast cancer who underwent hysteroscopy and obtained endometrial biopsy from 1 June 2018 to 31 December 2021 at the Beijing Obstetrics and Gynecology Hospital, Capital Medical University. Beijing Maternal and Child Health Care Hospital were prospectively collected.
Results: Hysteroscopy was performed followed by endometrial histopathological examination in 99 breast cancer patients, including 44 taking tamoxifen (TAM), 26 taking other endocrine drugs, and 29 not taking endocrine drugs. The endometrial thickness in the TAM group was significantly higher than that in the other endocrine drug groups and the group not taking endocrine drugs (p=0.017). The receiver operating characteristic curves for the abnormal premenopausal endometrial thickening were plotted in this study; an endometrial thickness of 15.5 mm seen on ultrasound could be used as the most accurate ultrasound diagnostic threshold for the diagnosis of abnormal premenopausal endometrial hyperplasia, with an area under the curve of 0.888 (95% CI: 0.716, 1.000), a sensitivity of 100%, and a specificity of 75%, which was consistent with the results of our previous retrospective study. An endometrial thickness of ≥ 5 mm in postmenopausal women with breast cancer taking TAM was still used as the cut-off value for routine ultrasound diagnosis of abnormal postmenopausal endometrial hyperplasia.
Conclusion: An ultrasound endometrial thickness (proliferative phase) of > 15 mm in premenopausal patients can be used as the most accurate ultrasound diagnostic threshold for the diagnosis of abnormal endometrial hyperplasia. After menopause, an ultrasound endometrial thickness of ≥ 5 mm is still used as the criterion for diagnosing abnormal endometrial hyperplasia. Older patients should be monitored for signs of vaginal bleeding and fluid discharge, and hysteroscopy should be performed if necessary to ascertain the endometrial condition.
Keywords: endocrine medication, endometrium disease, breast cancer
Introduction
Breast cancer is the most common malignant tumour in women worldwide and is one of hormone-dependent tumours; about 80% of breast cancer patients exhibit oestrogen receptor (ER) positivity, while 65% of breast cancer patients exhibit progesterone receptor (PR) positivity; endocrine therapy is suitable for almost all patients with ER- and/or PR-positive breast cancer, which can effectively reduce the recurrence rate and improve the survival rate, and has been widely used in the clinical setting.1 Tamoxifen (TAM) is recommended for endocrine therapy in premenopausal women, but its long-term administration might lead to a series of abnormal endometrial manifestations. Transvaginal ultrasound is the most commonly used method to assess for endometrial lesions; it is used to monitor the endometrial thickness, abnormal endometrial echogenicity, abnormal blood flow signals, etc., and to determine whether diagnostic curettage based on the clinical manifestations of the patients.
In this study, we aimed to analyse the clinical data of breast cancer patients taking TAM and other endocrine medications postoperatively to determine their general clinical conditions, duration of medication use, and curettage pathological results; we also aimed to validate the accuracy of the ultrasound diagnostic threshold values defined in a previous retrospective study conducted by our project group to explore the pathological effects on the endometrium of breast cancer patients taking endocrine therapy and the standard cut-off value for requiring ultrasound-guided clinical diagnostic curettage.
Materials and Methods
Study Participants
Prospectively, data of 99 patients with primary diagnosis of breast cancer and who underwent hysteroscopy plus endometrial diagnostic curettage after surgery +/− radiotherapy +/- chemotherapy +/− endocrine therapy to determine the endometrial histopathological findings were collected from 1 June 2018 to 31 December 2021 at the Beijing Obstetrics and Gynecology Hospital, Capital Medical University. Beijing Maternal and Child Health Care Hospital. Their indications for hysteroscopy included vaginal bleeding and fluid flow, ultrasound suggestive of abnormal endometrial thickening, abnormal intrauterine echogenicity, and blood flow signal. A total of 44 study patients were taking TAM, 26 patients were taking other endocrine drugs, and 29 patients were not taking endocrine drugs. Ninety-nine patients were aged 31–73 years, with a mean age of 51.2±8.6 years; of the total study patients, 57 were menopausal women and 42 were premenopausal women. The endocrine drugs administered were as follows: TAM 20 mg/day for 6 months to 11 years and other classes of endocrine drugs for 3 months to 10 years (toremifene 60 mg/day, letrozole 2.5 mg/day, anastrozole 1 mg/day, and exemestane 25 mg/day). Patients whose endometrial pathological sample was obtained during hysteroscopic dilatation and curettage after receiving standard treatment for breast cancer and with complete case information and ultrasound report for the last 3 months were included in the study. Meanwhile, patients with other concomitant gynaecologic endocrine diseases or other concomitant non-gynaecologic malignancies were excluded.
Research Methodology
The patients were divided into groups according to their menopausal status (premenopausal and postmenopausal groups) and medication treatment duration (those treated for ≥5 years and <5 years, and those treated for ≥3 years and <3 years). The group with abnormal endometrial hyperplasia comprised those with endometrial cancer and atypical endometrial hyperplasia, while the group with benign endometrial lesions comprised those with endometrial hyperplasia without cellular atypia, endometrial polyps, and normal endometrium. Based on the results of a previous retrospective study,2 the criteria for diagnosing abnormal endometrial thickening by ultrasound were endometrial thickness of ≥5 mm for postmenopausal women and ≥15 mm (proliferative phase) for premenopausal women; the diagnostic criteria were validated.
Statistical Methods
SPSS 25.0 statistical software was used to analyse the data. F-test or chi-square test was used to compare the difference between the groups; the diagnosis was made based on the pathological diagnostic results as the gold standard. Vaginal ultrasound was used to measure the proliferative phase, which was suggestive of endometrial thickness, to predict the final diagnosis and validate the diagnostic threshold. The evaluation indexes of the diagnostic test included sensitivity, specificity, positive predictive value, and negative predictive value. A p-value of <0.05 was considered significant. The ROC curve of abnormal endometrial thickening on ultrasound was plotted; the Youden index (YI, also known as the correct diagnostic index: YI = sensitivity + specificity – 1) was also calculated to determine the optimal diagnostic point.
Results
Analysis of the Clinical Characteristics of Breast Cancer Patients
No significant differences were observed in age, number of pregnancies, number of births, menopausal status, concomitant chronic disease, clinical symptoms, family history of cancer, or body mass index (BMI) between patients taking TAM,taking other endocrine drugs,and not taking endocrine drugs for breast cancer (p>0.05). The mean duration of TAM treatment was 4.2±2.8 years, while that of treatment with other endocrine drugs was 3.3±2.9 years. No significant difference was observed in the proportion of patients with abnormal endometrial hyperplasia between the groups taking TAM, taking other endocrine drugs, and not taking endocrine drugs. Taking endocrine drugs did not significantly increase the proportion of patients with abnormal endometrial hyperplasia; one of the four patients with endometrial cancer had serous carcinoma of endometrium (patient taking TAM), while the other three had endometrioid carcinoma. Ultrasound suggested that the endometrial thickness was significantly higher in the TAM group than in the other endocrine drug and non-endocrine drug groups, with a significant difference (p=0.017), see Table 1.
 |
Table 1 Analysis of Clinical Characteristics of Breast Cancer Patients [Cases (%), Mean ± SD] |
Analysis of the Clinical Conditions in Breast Cancer Patients with Different Endometrial Pathological States
In the analysis of the clinical condition of patients with endometrial hyperplasia based on the histopathological findings obtained during hysteroscopy in breast cancer patients, patients with abnormal endometrial hyperplasia group (endometrial cancer + endometrial atypical hyperplasia) were older than those with benign endometrial hyperplasia group (endometrial polyps + endometrial hyperplasia without cellular atypia + normal endometrium), with significant differences (p=0.008). Among the 99 patients, 42.4% of patients with clinical symptoms underwent hysteroscopy; the proportion of patients with abnormal endometrial hyperplasia combined with vaginal bleeding and vaginal discharge [83.3% (10/12)] was significantly higher than that of patients with benign endometrial hyperplasia [36.8% (32/87)], with a significant difference (p=0.004). No significant difference (p>0.05) was observed between the two groups in terms of menopausal status, number of pregnancies, number of births, menopausal status, concomitant chronic diseases, family history of cancer, and BMI; used of TAM, and other endocrine therapeutic drugs did not increase the probability of developing abnormal endometrial hyperplasia. The endometrial thickness on ultrasound (14.5±11.6 mm) in the group with abnormal endometrial hyperplasia was slightly higher than that (10.8±6.0 mm) in the group with benign endometrial hyperplasia, but the difference was not significant (p>0.05), see Table 2.
 |
Table 2 Analysis of the Clinical Conditions in Breast Cancer Patients with Different Endometrial Pathological States [Cases (%), Mean ± SD] |
Clinical Analysis of Different Endometrial Pathology at Hysteroscopy in Breast Cancer Patients Taking TAM
In this study, 44 patients were taking TAM, of whom 22 had a menopausal status, while 22 had a premenopausal status. Endometrial lesions were detected in 27 patients, with the highest incidence of endometrial polyps reported in 43.2% (19/44) of the patients. Approximately 4.5% (2/44) of the patients had endometrial cancer, 1 patient had a postmenopausal status, and 1 patient had a premenopausal status. Moreover, 4.5% (2/44) of the patients had endometrial atypical hyperplasia, 1 patient had a postmenopausal status, and 1 patient had a premenopausal status. Approximately 9.1% (4/44) of the patients had endometrial hyperplasia without cellular atypia, while 37.8% (17/45) had normal endometrium.
Twenty patients used TAM for ≥5 years, of whom 5.0% (1/20) developed endometrial cancer + endometrial atypical hyperplasia. Meanwhile, 12.5% (3/24) of the patients treated with TAM for <5 years developed endometrial cancer + endometrial atypical hyperplasia; however, the difference between the two groups was not significant (p>0.05). A total of 29 patients used TAM for ≥3 years, of whom 6.9% (2/29) developed endometrial cancer + endometrial atypical hyperplasia. Meanwhile, 13.3% (2/15) who used TAM for <3 years developed endometrial cancer + endometrial atypical hyperplasia; however, all differences were not significant (p>0.05), see Table 3.
 |
Table 3 Clinical Analysis of Different Endometrial Pathology During Hysteroscopy in Breast Cancer Patients Taking TAM [Cases (%)] |
Validation of Standard Thresholds of Endometrial Thickness for Ultrasound Diagnosis in Patients with Breast Cancer Using TAM
This prospective study found the endometrial thickness had no significant difference between the abnormal endometrial hyperplasia group and the benign endometrial hyperplasia/normal endometrium group in breast cancer patients taking TAM, whether menopausal or not (p>0.05); by contrast, the endometrial thickness was significantly higher in the premenopausal abnormal endometrial hyperplasia group than in the benign endometrial hyperplasia/normal endometrium group,the expanded sample size may have potential clinical significance. The number of patients with clinical symptoms, such as vaginal bleeding or vaginal discharge, was significantly higher in the abnormal endometrial hyperplasia group (75.0%, 3/4) than in the benign endometrial hyperplasia/normal endometrium group (37.5%, 15/40), although the difference was not significant (p=0.295); however, it also suggested that more attention should be paid to monitoring these patients with complaints and symptoms, see Table 4.
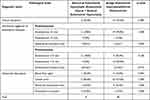 |
Table 4 Validation of the Ultrasound Diagnostic Criteria Values in Patients Taking TAM After Breast Cancer Surgery [Cases (%), Mean ± SD] |
Our previous study reported the ultrasound suggestive endometrial thickness cut-off values of ≥5 mm for postmenopausal patients and ≥15 mm for premenopausal patients (proliferative). Forty-four patients taking TAM after breast cancer surgery were included in the prospective study and triaged according to the above criteria, with pathological diagnosis as the final criterion. Postmenopausal women had a sensitivity of 100%, specificity of 5.0%, positive predictive value of 9.5%, and negative predictive value of 100% if the predictive threshold for ultrasonographic diagnosis of endometrial thickness was ≥5 mm. Premenopausal women with an ultrasound diagnostic endometrial thickness prediction cut-off of ≥15 mm (proliferative phase) had 100% sensitivity, 65.0% specificity, 22.2% positive predictive value, and 100% negative predictive value, see Table 4. According to the results of the prospective study of patients taking TAM after undergoing breast cancer surgery, the ROC curve of ultrasound abnormal endometrial hyperplasia in premenopausal patients (Figure 1) with an area under the curve (AUC) of 0.888 (95% CI: 0.716, 1.000) and a maximum Youden index of 0.75 (sensitivity = 1, specificity = 0.75), corresponding to an endometrial thickness of 15.5 mm (proliferative phase), could be used as a diagnostic and an accurate ultrasound diagnostic cut-off value for abnormal endometrial hyperplasia. In our previous retrospective study, we plotted the ROC curve of ultrasound abnormal endometrial thickening in premenopausal patients taking TAM after breast cancer surgery and found that the optimal endometrial thickness ultrasound diagnostic cut-off value for diagnosing abnormal endometrial hyperplasia was 15 mm (proliferative phase). The premenopausal endometrial thickness cut-off value for breast cancer patients taking TAM in the prospective study was the same as the corresponding endometrial thickness cut-off value in the retrospective study (15 mm).2 This finding indirectly validated the accuracy of the retrospective study data in the determination of the ultrasound diagnostic cut-off value.
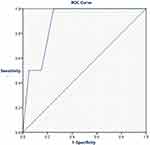 |
Figure 1 ROC curves of premenopausal ultrasound diagnosis of abnormal endometrial hyperplasia thickness in breast cancer patients taking TAM (prospective study). |
Discussion
Effects on the Endometrium in Breast Cancer Patients Taking TAM
Breast cancer is one of the most common malignant tumours in women; with the development of modern detection technology and with the improvement in women’s social status and self-awareness, the rate of breast cancer diagnosis is relatively increasing annually. Currently, breast cancer is the most prevalent malignant tumour affecting in women worldwide,3 with 2,088,800 new cases and 626,600 deaths per year, accounting for 24.2% of the global female malignancies. China4 has the highest number of new breast cancer cases and deaths; a total of 272,400 new cases and 70,700 new deaths are reported each year, which account for 6.9% of female malignancy-related deaths in China; breast cancer is more prevalent in urban population than in rural population and among young adults, which seriously threatens women’s life and health. Several endocrine treatment options are available based on the menopausal status of patients and at different stages of treatment, including preoperative neoadjuvant chemotherapy, postoperative adjuvant chemotherapy, and relief chemotherapy for recurrent patients. The most commonly used endocrine agents for breast cancer fall under the following four categories: TAM, aromatase inhibitor (AI), fulvestrant, and goserelin (GnRH-a), of which the most cost-effective endocrine agent is TAM. The three treatment options for premenopausal women were as follows:5 TAM treatment for 5 to 10 years, TAM+ovarian function suppression (OFS) for 5 years, and OFS+AI for 5 years. The treatment options for postmenopausal patients were as follows: 5 years of AI as a first-line treatment, 5 years of TAM followed by 5 years of AI, or an extension of TAM to 10 years. TAM plays an important role in the endocrine treatment of breast cancer.
TAM is a selective oestrogen receptor modulator for postoperative endocrine therapy in patients with premenopausal ER-positive breast cancer. Approximately 60–70% of breast cancer patients required continuous TAM treatment for up to 5 years after surgery. TAM has both anti-oestrogenic and weak estrogenic effects, which can competitively bind ER in target cells, thus reducing intracellular ER content, producing anti-oestrogenic effects, and inhibiting the growth and metabolism of tumour cells. It can reduce the growth and metabolism of tumour cells and effectively reduce the risk of recurrence and death among breast cancer patients. However, TAM targets different organs and has a dual effect. In postmenopausal women with low oestrogen levels, TAM exhibits weak oestrogen-like effects and can cause a series of lesions in the endometrium, as a target organ, and even cancer with long-term administration.6 TAM, as the adjuvant treatment after surgery, and radiation therapy for premenopausal breast cancer can significantly prevent breast cancer recurrence or alleviate the disease. Takahashi et al7 suggested that the effect of TAM on the endometrium was related to the level of oestrogen in the body; experiments conducted in mice showed that ovariectomised mice had a significant increase in uterine weight after treatment with TAM, whereas mice with ovaries had a slight decrease in uterine weight after treatment with TAM. It was thus hypothesised that the effect of TAM was dependent on the concentration of peripheral oestradiol, with TAM exhibiting an anti-oestrogenic effect when the oestradiol levels were high, but an oestrogen-like effect when the oestradiol levels were low. Thus, TAM could have an anti-oestrogenic effect in premenopausal women, leading to menopause and even endometrial atrophy in patients. Moreover, TAM could cause the endometrium of postmenopausal breast cancer patients to show diverse pathological histological changes such as polyps-proliferation-malignancy due to its weak estrogenic effect; long-term TAM administration can increase the risk of endometrioid carcinoma.8 Therefore, special attention should be paid to the evaluation of endometrial lesions in breast cancer patients taking TAM, especially in postmenopausal women. In this study, we showed that TAM administration in breast cancer patients resulted in a significant increase in endometrial thickness, with a significant difference (p=0.017) compared with that in the group taking other endocrine drugs and the group not taking the drugs; in addition, the TAM group showed the greatest endometrial thickness on imaging compared with those taking other endocrine drugs.
In earlier studies,9,10 TAM as treatment for breast cancer was associated with the occurrence of endometrioid carcinoma; most scholars believed that TAM was associated with endometrioid carcinoma and that long-term TAM use increased the incidence of endometrioid carcinoma, which was related to the duration of use. The relative risk of endometrioid carcinoma among patients using TAM for more than 5 years was 4.06. Another previous study also found11 that the risk of endometrioid carcinoma in patients treated with TAM was not correlated with the dose of TAM, but significantly increased if TAM was used for more than 5 years. Results of a domestic study12 found that TAM promoted the development of endometrial lesions in postmenopausal women; both severe atypical hyperplasia of the endometrium and endometrial cancer occurred in postmenopausal patients, and the incidence of endometrial lesions tended to increase with the duration of TAM use, leading to an increase in the malignancy grade of endometrial disease. The results of our study showed no significant difference (p=0.824) between breast cancer patients taking TAM and those taking other endocrine drugs and not taking endocrine drugs in endometrium pathological state; meanwhile, the incidence of abnormal endometrial hyperplasia slightly increased in the breast cancer patients not treated with endocrine drugs; therefore, breast cancer patients taking endocrine drugs were positive for oestrogen-progestin receptors. Those not further treated with endocrine drugs had triple negative breast cancer, while a large proportion of the latter had hereditary breast cancer (containing BRCA mutations) with poor prognosis. Therefore, the risk of concomitant endometrial and ovarian cancer was higher in this patient group than in those with ER- and PR-positive breast cancer. This study showed that patients taking TAM for breast cancer, based on their menopausal status and the duration of endocrine medication resulted in endometrial thickening; most of them had predominantly benign endometrial hyperplasia and endometrial polyps. The incidence of abnormal endometrial hyperplasia was not significantly higher (p>0.05), and it did not induce the development of endometrial disease. Meanwhile, longer TAM use increased the malignant grade, which was consistent with the findings of some other studies.13–15 The aforementioned differences in endometrial imaging outcomes in patients taking TAM for breast cancer might be related to the duration of follow-up and the number of cases. Hence, future studies with a large sample size, multi-centre design, and longer duration should be conducted to determine whether the duration of TAM administration was associated with endometrial lesions. For breast cancer patients, based on menopausal status, who were ER positive and required endocrine medication, TAM therapy might be an option to prolong patient’s survival and reduce recurrence; with close follow-up and ultrasound monitoring, the administration of endocrine medication should not be refused among this patient group due to fear of increasing the risk of endometrioid carcinoma, as it is safer for premenopausal women based on the current mechanism of TAM.
Endometrial Thickness Cut-off Values for Ultrasound Diagnosis in Breast Cancer Patients Taking TAM
The advantages of ultrasound examination of the endometrium are as follows: it is easy to perform, non-invasive, and can be repeated.16 Some studies have reported that endometrial thickness is maintained for several years after the end of TAM treatment, leading to an increased likelihood of endometrial cancer. Therefore, monitoring of the endometrium is crucial; although there are no clearly defined and generally accepted guidelines related to the follow-up examinations of TAM-treated patients, ultrasound monitoring of the endometrium is most commonly performed, and patients treated with TAM undergo strict annual or semi-annual vaginal ultrasound, with hysteroscopy and histopathology in cases of abnormalities.17 Ultrasound examination has a specificity of 63.6%, sensitivity of 81.8%, positive predictive value of 72.9%, and negative predictive value of 73.7%; meanwhile, the hysteroscopy had a specificity of 100.0%, sensitivity of 98.1%, positive predictive value of 100.0%, and negative predictive value of 97.8%. The accuracy of hysteroscopy was significantly higher than that of ultrasound (p=0.000).18 In conclusion, ultrasound had high sensitivity in detecting early lesions at risk of malignancy and endometrial cancer, while hysteroscopy had high specificity.
No uniform standards had been established for monitoring endometrial thickness in breast cancer patients taking TAM. For patients taking TAM after breast cancer surgery, uniform acceptable ultrasound endometrial cut-off values were used as indicators for hysteroscopy in China and abroad; a proliferative endometrial thickness of 12 mm by ultrasound in normal women before menopause and an endometrial thickness of 5 mm after menopause were used as the cut-off values for performing hysteroscopy. Repeated diagnostic curettage in such patients increased the risk of surgical complications, caused waste of medical resources, and increased patient’s burden. Burkart et al19 suggested that hysteroscopy + curettage should be performed to determine the nature of the lesion in postmenopausal patients with endometrial thickness of >8 mm, while some scholars suggested 10 mm as an acceptable threshold for endometrial pathology.20 In our previous retrospective study,2 data of 59 breast cancer patients taking TAM were collected, and their endometrium was evaluated using ultrasound; results showed that premenopausal endometrial thickness in breast cancer patients taking TAM was associated with abnormal endometrial hyperplasia (p=0.035). A ROC curve analysis was performed to determine whether an ultrasound suggestive endometrial thickness (proliferative phase) of 15 mm could be used as the best ultrasound diagnostic cut-off value with a sensitivity of 0.714 and a specificity of 0.818. We further validated this in a prospective study, in which the predictive cut-off value for ultrasound diagnosis of abnormal endometrial thickening in premenopausal women was set as ≥15 mm with a sensitivity of 100%, a specificity of 65.0%, a positive predictive value of 22.2%, and a negative predictive value of 100%. The prospective study verified that in postoperative breast cancer patients taking TAM, the premenopausal endometrial thickness cut-off value was 15.5 mm, which was similar to the corresponding endometrial thickness cut-off value of 15 mm in the retrospective study and indirectly proved the accuracy of the diagnostic cut-off value of the retrospective study data; for premenopausal women, >15 mm can be used as an ultrasound diagnostic cut-off value for the preliminary judgment of abnormal endometrial hyperplasia (proliferative phase) in breast cancer patients taking TAM in the future. A retrospective study found that endometrial thickness was not associated with abnormal endometrial proliferation in postmenopausal patients (p=0.631); for postmenopausal women, an acceptable ultrasound endometrial thickness of ≥5 mm was used as the diagnostic cut-off value. In addition, a prospective study was conducted to further validate this ultrasound diagnostic cut-off value with 100% sensitivity, 5.0% specificity, 9.5% positive predictive value, and 100% negative predictive value. Although the specificity and positive predictive value were low, considering the fact that postmenopausal women taking TAM for breast cancer were more likely to have endometrioid carcinoma, a single ultrasound diagnostic criteria and endometrial thickening are not specific; hence, the use of an endometrial thickness of ≥5 mm as a diagnostic criterion can reduce the underdiagnosis rate in clinical practice.
Our prospective study further revealed that patients in the group with abnormal endometrial hyperplasia were older and had higher endometrial thickness than those in the group with benign endometrial hyperplasia; moreover, patients had more vaginal bleeding and vaginal drainage symptoms than the latter. Therefore, in breast cancer patients taking TAM, further hysteroscopy is recommended in those with older age and postmenopausal women with concomitant vaginal bleeding and drainage, even if the endometrial thickness was <5 mm. In premenopausal women with older age, concomitant symptoms of vaginal bleeding and vaginal drainage, or endometrial thickness of >15 mm, they should be informed of the possibility of developing abnormal endometrial hyperplasia; if necessary, pelvic magnetic resonance imaging techniques and related tumour marker tests should be improved, and hysteroscopy should be performed at the same time to determine the condition of the endometrium. Markovitch et al21 studied 279 asymptomatic patients taking TAM for breast cancer and found that as the endometrial thickness cut-off value increased, the specificity of vaginal ultrasound increased, the sensitivity decreased, and the number of positive histopathological examinations increased. The most satisfactory prediction results were obtained when the cut-off value was 15 mm, with specificity rate, sensitivity rate, positive predictive value, and negative predictive value of 37.9%, 87.2%, 63.0%, and 70.2%, respectively. Unnecessary hysteroscopy was avoided in 78.5% of patients, but setting an extremely high cut-off value could lead to the occurrence of missed endometrial cancer diagnosis. Single vaginal ultrasound diagnostic criteria such as abnormal endometrial echo, intrauterine occupying lesions, and abnormal blood flow signal were not specific for the diagnosis of abnormal endometrial hyperplasia in this study. Therefore, prompt hysteroscopy and surgical excision are recommended for those presenting with abnormal echogenicity or occupying lesions in the uterus; however, considering the small sample size of this study, a large sample, prospective, multi-centre study is still warranted to further clarify the accuracy of this cut-off value. Determining a cut-off value with high specificity and sensitivity to effectively predict endometrial lesions is the current direction of future research. The results of this study provide a theoretical basis for the development of ultrasound diagnostic cut-off values for endometrial thickening after TAM treatment for breast cancer and establishment of guidelines for the early detection of endometrial abnormalities in breast cancer patients taking TAM. This study also highlights the need for providing a standardised clinical treatment, reducing unnecessary tests, and decreasing the medical costs.
Conclusion
The incidence of abnormal endometrial hyperplasia was not significantly increased by the administration of endocrine drugs after breast cancer surgery; TAM was safe for premenopausal women according to its mechanism of action and current guidelines related to breast cancer. In premenopausal breast cancer patients taking TAM, a proliferative endometrial thickness of >15 mm could be used as a diagnostic cut-off value for screening abnormal endometrial hyperplasia. Because the timing of endometrial lesions was uncertain, close monitoring must be performed regularly, especially in postmenopausal patients. Physicians should monitor patients with concomitant vaginal bleeding and increased vaginal discharge; furthermore, hysteroscopy should be performed if necessary to ascertain the nature of the pathology, determine the endometrial condition, and guide subsequent treatment.
Abbreviations
TAM, tamoxifen; AUC, area under the curve; ROC, receiver operating characteristic; ER, oestrogen receptor; PR, progesterone receptor; BMI, body mass index; OFS, ovarian function suppression; AI, aromatase inhibitor.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Ethical Approval and Consent to Participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Ethic Committee (EC) from the Beijing Obstetrics and Gynecology Hospital, Capital Medical University. Beijing Maternal and Child Health Care Hospital (2018-KY-020-01).
Informed consent was obtained from all subjects and/or their legal guardian(s) in this research.
Acknowledgments
We are grateful to all the reviewers and editors who provided comments that substantially improved the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
1. Funding was gratefully received from: Capital’s Funds for Health Improvement and Research (No. 2018-4-2113). 2. Beijing Obstetrics and Gynecology Hospital, Capital Medical University, Beijing Maternal and Child Health Care Hospital “Excellent Youth” Plan Special Funds (No.YQRC201806). 3. Beijing Municipal Science & Technology Commission (grand No.Z221100007422087). 4. Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support (No. ZYLX202120).
Disclosure
No potential conflict of interest relevant to this article was reported.
References
1. Potkul RK, Unger JM, Livingston RB, et al. Randomized trial of medroxyprogesterone acetate for the prevention of endometrial pathology from adjuvant tamoxifen for breast cancer. NPJ Breast Cancer. 2016;2:16024. doi:10.1038/npjbcancer.2016.24
2. Li YH, He Y, Yang SL, et al. Progress on relationship between endocrine therapy and endometrial disease in postoperative breast cancer patients and its monitoring. Chin J Pract Gynecol Obstet. 2019;35(8):900–904.
3. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi:10.3322/caac.21492
4. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi:10.3322/caac.21338
5. Gradishar WJ, Moran MS, Abraham J, et al. NCCN guidelines insights: breast cancer, version 4.2021. JNCCN. 2021;19(5):484–493. doi:10.6004/jnccn.2021.0023
6. Günaldi M, Erkisi M. Evaluation of endometrial thickness and bone mineral density based on CYP2D6 polymorphisms in Turkish breast cancer patients receiving tamoxifen treatment. Pharmacol. 2014;94(3–4):183–189. doi:10.1159/000363304
7. Takahashi M, Shimomoto T, Miyajima K, et al. Promotion, but not progression, effects of tamoxifen on uterine carcinogenesis in mic initiated with Nethyl-N’-nitro -N-nitrosoguanidine. Carcinogenesis. 2002;23(9):1549–1555. doi:10.1093/carcin/23.9.1549
8. van de Velde CJ, Verma S, van Nes JG, et al. Switching from tamoxifen to aromatse inhibitors for adjuvant endocrine therapy in postmenopausal patients with early breast cancer. Cancer Treat Rev. 2010;36(1):54–62. doi:10.1016/j.ctrv.2009.10.003
9. Uziely B, Lewin A, Brufman A, et al. The effect of tamoxifen on the endometrium[J]. Breast Cancer Res Treat. 1993;26:101–105. doi:10.1007/BF00682705
10. Cardosi RJ, Fiorica JV. Surveillance of the endometrium in Tamoxifen treated women. Curr Opin Obstet Gynecol. 2000;12(1):27–3l. doi:10.1097/00001703-200002000-00005
11. Swerdlow AJ, Jones ME. Tamoxifen treatment for breast cancer and risk of endometrial cancer: a case-control study. J Natl Cancer Inst. 2005;97(5):375–384. doi:10.1093/jnci/dji057
12. Yuan F, Wang FL, Ma DL, et al. Clinical and pathologic analysis of endometrial lesion in postoperative breast cancer patients taking Tamoxifen. Cancer Res Prevent Treat. 2012;39(8):970–972.
13. Lee S, Kim YH, Kim SC, et al. The effect of tamoxifen therapy on the endometrium and ovarian cyst formation in patients with breast cancer. Obstet Gynecol Sci. 2018;61(5):615–620. doi:10.5468/ogs.2018.61.5.615
14. Le Donne M, Lentini M, De Meo L, et al. Uterine pathologies in patients undergoing tamoxifen therapy for breast cancer: ultrasonographic, hysteroscopic and histological findings. Eur J Gynaecol Oncol. 2005;26:623–626.
15. Wang YL, Chen LZ, Li QG. Clinical and pathologic analysis of endometrial lesion in breast cancer patients taking tamoxifen. Chin J N Clin Med. 2014;7(8):719–721.
16. Wang JL. Scientific evaluation of methods for endometrial cancer screening. Chin J Pract Gynecol Obstet. 2016;32(5):402–405.
17. Guo X, Guan MM, Liu CH, et al. Application of hysteroscopy in the diagnosis and treatment of endometrial cancer. Chin J Pract Gynecol Obstet. 2017;33(1):13–15.
18. Gao WL, Zhang LP, Feng LM. Comparative study of transvaginal ultrasonographic and diagnostic hysteroscopic findings in postmenopausal breast cancer patients treated with tamoxifen. Chinese Med J. 2011;124(15):2335–2339.
19. Burkart C, Wight E, Pók J, et al. Ultrasound endometrium follow-up during tamoxifen treatment: really not reliable or useful after all? Ultraschall Der Medizin. 2001;22(3):136–142. doi:10.1055/s-2001-15243
20. Dalbert D, Mm R, Figueredo A, et al. Tamoxifen and endometrial disease in patients with breast cancer. Med. 2013;73(2):97–103.
21. Markovitch O, Tepper R, Aviram R, et al. The value of sono⁃hysterography in the prediction of endometrial pathologies in asymptomatic postmenopausal breast cancer tamoxifen-treated patients. Gynecol Oncol. 2004;94(3):754–759. doi:10.1016/j.ygyno.2004.06.033
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
