Back to Journals » Journal of Inflammation Research » Volume 17
Progressive Facial Ulcer: A Case Report of Pyoderma gangrenosum
Authors Zhang XQ, Tang ZW , Jing J
Received 6 November 2023
Accepted for publication 16 January 2024
Published 3 February 2024 Volume 2024:17 Pages 687—691
DOI https://doi.org/10.2147/JIR.S441751
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Tara Strutt
Xian-Qi Zhang,* Zhen-Wei Tang,* Jing Jing
Department of Dermatology, Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, 310009, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jing Jing, Department of Dermatology, Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, 310009, People’s Republic of China, Tel +86 571 87784558, Fax +86 571 87783504, Email [email protected]
Abstract: Pyoderma gangrenosum (PG) is a rare neutrophilic dermatosis characterized by rapidly developing and painful skin ulcers with distinctive features. As far as we are concerned, there is no previous case report on facial PG in East-Asia. In this case, we describe a case of a 79-year-old man with a 3-month history of progressive painful ulcers on his cheek and upper lip. Initial suspicion of atypical mycobacterium infection led to an ineffective treatment regimen. Comprehensive infectious testing yielded negative results, and a positive pathergy test indicated a potential diagnosis of PG. A skin biopsy confirmed the diagnosis, and the patient showed significant improvement with intravenous methylprednisolone and oral cyclosporine treatment. After three months, complete resolution of the lesions was achieved without recurrence. The case highlights the diagnostic challenges associated with PG, which is often misdiagnosed due to its resemblance to other conditions. Thorough evaluation is crucial to exclude alternative diagnoses, particularly cutaneous infections. Clinical morphology, tissue biopsy, and culture are essential for accurate diagnosis. The presence of pathergy, the development of new lesions following minor trauma, can also be a diagnostic clue.
Keywords: Pyoderma gangrenosum, neutrophilic dermatosis, ulcer
Introduction
Pyoderma gangrenosum (PG) is a rare neutrophilic dermatosis that presents with rapidly developing, painful skin ulcers characterized by cutaneous infiltration of neutrophils, which is hallmarked by undermined borders and peripheral erythema.1 As a diagnostically challenging variant of neutrophilic dermatosis, diagnosis of PG is made by exclusion of infection, neoplasia, thrombophilia, and other inflammatory conditions, with a misdiagnosis rate of 10%.2
Case Presentation
A 79-year-old man presented with a 3-month history of rapidly progressive painful ulcers involving his cheek and upper lip. He reported that it had occurred after shaving the face with a razor and enlarged rapidly after surgical debridement. Physical examination revealed deep ulcers with irregular, violaceous and undermined borders on his bilateral cheek and upper lip (Figure 1a and b). The nursing assessment and doctor’s evaluation during hospital admission did not support the presence of psychological issues in the patient. Atypical mycobacterium infection was initially suspected on the basis of his fever, elevated inflammatory markers and leukocytosis. After a triple drug regimen treatment, including rifampicin, amikacin and clindamycin for 4 days, his temperature was 40.2°C and the facial lesion rapidly progressed. Multiple irregular, violaceous lesions with central ulcer and undermined elevated borders had developed on his bilateral cheek and upper lip (Figure 1c).
 |
Figure 1 (a–c) Rapidly progressive painful ulcer (d) Positive pathergy test. |
Serological and cultured test for infectious causes, including virus, bacteria, atypical mycobacteria and deep fungi were negative. A metagenomic next-generation sequencing (mNGS) of lesional tissue was also performed and turned out negative detection. PPD test and T-SPOT were negative. During hospital, cutaneous papulopustule developed on his opisthenar at an intravenous cannula site, suggesting positive pathergy test (Figure 1d). A skin biopsy of the facial ulcer revealed an intense neutrophilic infiltrate, neutrophilic pustules and abscess formation (Figure 2). According to the diagnostic Criteria proposed by a delphi consensus of international experts, this case meets 1 major criterion and more than 4 minor criterion are met, so we made a diagnosis of pyoderma gangrenosum.3
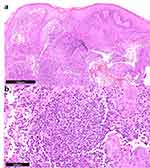 |
Figure 2 Histological HE staining photographs. (a) magnified 5 times, and (b) magnified 20 times. |
The patient’s ulcer improved dramatically with intravenous methylprednisolone (2mg/kg/day) and oral cyclosporine treatment (3mg/kg/day) for 2 weeks. The dosage of methylprednisolone and cyclosporine was progressively tapered. After a 7-month follow-up, the patient’s skin lesions have healed well and there are no signs of recurrence (Figure 3).
 |
Figure 3 Clinical photos of 7 months after treatment. |
Discussion
As stated in most reviews on PG, the ulcerative lesion is commonly seen in lower extremities.4 However, there are case reports of head and neck involvement in children, while involvement of the genital and perianal area has been reported in infants.4,5 Kratzsch et al and Abela et al reported two cases of facial ulceration in a 90-year-old male and 34-year-old female, which were diagnosed with PG finally.6,7 However, as far as we are concerned, there is no previous case report on facial PG in East-Asia.
Considering the high misdiagnosis rate, a thorough evaluation is required in all patients suspected of PG in order to rule out alternative diagnoses, especially cutaneous infection. Clinical morphologic test as well as tissue biopsy and culture are critical to making a diagnosis of PG.1 Of note, with the widespread of next generation sequencing technology, mNGS was applied into the differential diagnosis of cutaneous infection.8 Zhang et al managed to distinguished a pyoderma gangrenosum-like ulcer caused by Helicobacter cinaedi using mNGS.9 In this case, the combination of negative results of serological, cultured test and mNGS assist us to exclude a skin infection and further make a diagnosis of PG. Pathergy, the development of new lesions induced by minor trauma, may be a diagnostic clue in patients with neutrophilic dermatosis, including PG.10
The pathogenesis of PG remains poorly understood, which is likely a multifactorial combination of neutrophil dysfunction, inflammatory mediators and genetic predisposition.2 Minor trauma and surgery are suggested as initiating factors in lesion development, which is known to induce the release of cytokines and danger signals that can support innate immune responses.11 Therefore, the treatment for PG requires on tropic and systematic immunosuppressive agent, such as cyclosporine or corticosteroid.12 Biologics such as interleukin inhibitors or tumor necrosis factor inhibitors also appear to be effective for PG.13 Besides, negative pressure wound therapy can also be used in conjunction with immunosuppressive agents as an adjuvant therapy to enhance the efficiency of ulcer healing in PG.14
Conclusion
In conclusion, the case highlights the diagnostic challenges associated with PG, which is often misdiagnosed due to its resemblance to other conditions. Thorough evaluation is crucial to exclude alternative diagnoses, particularly cutaneous infections. Clinical morphology, tissue biopsy, and culture are essential for accurate diagnosis. The presence of pathergy, the development of new lesions following minor trauma, can also be a diagnostic clue.
Ethical Approval
Written informed consent was obtained from the patient and the patient’s parents for the publication of all the images and data included in this article. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical review and approval were not required to publish the case details in accordance with the institutional requirements.
Consent to Publish
The patient provided informed consent to publish their case details and any accompanying images.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (No. 81972955).
Funding
This study was supported by the National Natural Science Foundation of China (No. 81972955).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Maverakis E, Marzano AV, Le ST, et al. Pyoderma gangrenosum. Nat Rev Dis Primers. 2020;6(1):81. doi:10.1038/s41572-020-0213-x
2. Braswell SF, Kostopoulos TC, Ortega-Loayza AG. Pathophysiology of pyoderma gangrenosum (PG): an updated review. J Am Acad Dermatol. 2015;73(4):691–698. doi:10.1016/j.jaad.2015.06.021
3. Maverakis E, Ma C, Shinkai K, et al. Diagnostic criteria of ulcerative pyoderma gangrenosum: a delphi consensus of international experts. JAMA Dermatol. 2018;154(4):461–466. doi:10.1001/jamadermatol.2017.5980
4. Alavi A, French LE, Davis MD, Brassard A, Kirsner RS. Pyoderma gangrenosum: an update on pathophysiology, diagnosis and treatment. Am J Clin Dermatol. 2017;18(3):355–372. doi:10.1007/s40257-017-0251-7
5. Sandhu K, Handa S, Kanwar AJ. Idiopathic pyoderma gangrenosum in a child. Pediatr Dermatol. 2004;21(3):276–277. doi:10.1111/j.0736-8046.2004.21322.x
6. Abela CB, Soldin M, Gateley D. Pyoderma gangrenosum--case report. Br J Oral Maxillofac Surg. 2007;45(4):328–330. doi:10.1016/j.bjoms.2005.11.004
7. Kratzsch D, Ziemer M, Milkova L, Wagner JA, Simon JC, Kendler M. Facial pyoderma gangrenosum in senescence. Case Rep Dermatol. 2013;5(3):295–300. doi:10.1159/000356100
8. Kong M, Li W, Kong Q, Dong H, Han A, Jiang L. Application of metagenomic next-generation sequencing in cutaneous tuberculosis. Front Cell Infect Microbiol. 2022;12:942073. doi:10.3389/fcimb.2022.942073
9. Zhang L, Zhou M, Lv W, Li T, Xu Y, Liu Z. Metagenomics assists in the diagnosis of a refractory, culture-negative pyoderma gangrenosum-like ulcer caused by Helicobacter cinaedi in a patient with primary agammaglobulinemia. J Microbiol Immunol Infect. 2023;56(6):1284–1287. doi:10.1016/j.jmii.2023.07.001
10. Moon JH, Huynh J. Pathergy in neutrophilic dermatosis. N Engl J Med. 2021;384(3):271. doi:10.1056/NEJMicm1901738
11. Lindberg-Larsen R, Fogh K. Traumatic pyoderma gangrenosum of the face: pathergy development after bike accident. Dermatology. 2009;218(3):272–274. doi:10.1159/000182266
12. Facheris P, De Santis M, Gargiulo L, et al. Concomitant Pyoderma gangrenosum-like and amicrobial pustulosis of the folds: a case report. J Clin Immunol. 2020;40(7):1038–1040. doi:10.1007/s10875-020-00819-1
13. Ben Abdallah H, Fogh K, Vestergaard C, Bech R. Pyoderma gangrenosum and interleukin inhibitors: a semi-systematic review. Dermatology. 2022;238(4):785–792. doi:10.1159/000519320
14. Almeida IR, Coltro PS, Gonçalves HOC, et al. The role of negative pressure wound therapy (NPWT) on the treatment of pyoderma gangrenosum: a systematic review and personal experience. Wound Repair Regen. 2021;29(3):486–494. doi:10.1111/wrr.12910
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
