Back to Journals » Infection and Drug Resistance » Volume 16
Prognostic Value of Wagner Grade and Platelet Level in Diabetics with Infected Foot Ulcers After Antibiotic Therapy
Authors Yang X, Yan T, Shen D , Sheng M, Huang W, Li L, Chai D
Received 19 September 2023
Accepted for publication 30 November 2023
Published 5 December 2023 Volume 2023:16 Pages 7435—7445
DOI https://doi.org/10.2147/IDR.S436869
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Xi Yang,1,* Ting Yan,2,* Danfeng Shen,3,* Mengyao Sheng,1 Wenya Huang,1 Li Li,1 Dayang Chai4
1Department of Endocrinology, The First People’s Hospital of Taicang, The Affiliated Taicang Hospital of Soochow University, Taicang, People’s Republic of China; 2Department of Dermatology, The First People’s Hospital of Taicang, The Affiliated Taicang Hospital of Soochow University, Taicang, People’s Republic of China; 3Department of General Surgery, The First People’s Hospital of Taicang, The Affiliated Taicang Hospital of Soochow University, Taicang, People’s Republic of China; 4Department of Cardiology, The First People’s Hospital of Taicang, The Affiliated Taicang Hospital of Soochow University, Taicang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Dayang Chai, Department of Cardiology, The First People’s Hospital of Taicang, The Affiliated Taicang Hospital of Suzhou University, No. 58 Changsheng Road, Taicang, 215400, People’s Republic of China, Email [email protected] Li Li, Department of Endocrinology, The First People’s Hospital of Taicang, The Affiliated Taicang Hospital of Soochow University, No. 58 Changsheng Road, Taicang, 215400, People’s Republic of China, Email [email protected]
Purpose: The aim of the current study was to investigate factors potentially associated with the healing of infected foot ulcers in patients with diabetes after antimicrobial therapy with drugs selected based on antimicrobial susceptibility testing.
Patients and Methods: A retrospective study was conducted to analyze clinical data from 99 type 2 diabetes mellitus patients with foot infection admitted to our center from January 2016 to December 2020. Pathogenic characteristics, results of wound discharge testing, and relevant wound surface factors were analyzed. Etiological characteristics and the results of susceptibility testing, wound healing rates, and factors potentially associated with wound healing rates were also analyzed.
Results: Baseline data were analyzed via the t-test for independent samples, the Mann–Whitney U-test, and the chi-square test to identify variables significantly associated with prognosis. Least absolute shrinkage and selection operator regression analysis then determined that Wagner grade, essential hypertension, platelets, Gram negative bacteria, and neutrophil-to-lymphocyte ratio were of predictive value. A nomogram plot was built based on these five variables, and it yielded a standard C-index of 0.964, and an internally corrected C-index of 0.931. In multivariate logistic regression analysis Wagner grade (odds ratio [OR] 12.30, 95% confidence interval [CI] 2.471– 61.194, p = 0.002) and platelet level (OR 0.978, 95% CI 0.960– 0.996, p = 0.018) were significantly associated with wound healing outcomes. Restricted cubic spline analysis indicated that there was a linear relationship between wound healing and platelet levels, and that this relationship was strongest in patients classified as Wagner grade 2 with a platelet count ≤ 200 (p for nonlinearity = 0.442).
Conclusion: Wagner grade, essential hypertension, platelet count, Gram negative bacteria, and neutrophil-to-lymphocyte ratio could predict the course of healing of infected foot ulcers in type 2 diabetes mellitus patients. When the Wagner grade was 2 and the platelet level was ≤ 200, platelet level was linearly associated with healing outcome, whereby a lower platelet level predicted a worse wound healing outcome.
Keywords: diabetic foot ulcer, DFU, platelet, RCS, ulcer healing, Wagner grade
Introduction
Currently the global prevalence of diabetes is 9.3%, and it is one of the top ten causes of death in the world. It is estimated that by 2030, it will exceed 500 million.1 Diabetes-related foot disease (DFD) is one of the most serious complications of diabetes. It is one of the main causes of hospitalization of diabetes patients, and it greatly increases the cost of treatment.2 The main risk factors for foot ulcer in diabetes include a history of foot ulcers, a prolonged course of diabetes, peripheral vascular disease, coronary artery disease, advanced peripheral neuropathy, and end-stage renal disease.1,3,4 Patients with diabetic foot ulcer (DFU) infection are at a higher risk of amputation, and their costs of treatment are increased, so they must be evaluated and treated in a timely manner.5–7
DFUs are difficult to treat successfully, and they are the main reason for hospitalization and lower limb amputation. In one study they occurred in 15% of all diabetes patients and were present in 84% of all diabetes-related lower limb amputees.8 Due to a lack of consensus on treatment, many chronic wounds persist for longer than necessary.9 As the life expectancy of aging populations increases, the prevalence of chronic wounds is likely to increase, resulting in higher social costs.10 Therefore, improved wound healing rates and new developments in this field should be encouraged.11
Multidisciplinary nursing and structured medical care have proven to be the most effective ways to reduce the amputation index of DFD,12 and the incorporation of optimized infection control management could significantly improve the prognosis of patients with DFU.13,14 Rapid initiation of appropriate empirical antibiotic treatment, as well as early identification of pathogens and corresponding adjustment of the antibiotic regimen with respect to drug sensitivity are reportedly essential for effective treatment of ulcers and prevention of amputation.15,16 In previous studies, factors such as low socio-economic status, smoking,17,18 gender, kidney injury,19 ischemia, diabetes neuropathy,20 and high levels of glucose and triglycerides21 have been significantly associated with the risk of foot amputation. It remains unclear which factors are most conducive to foot wound healing in diabetics however, particularly in those treated for infections after antimicrobial drug sensitivity testing.
The current study assessed the effects of clinical, biochemical, and epidemiological factors, and patient behavior-related predictors on wound prognosis in DFD patients. Understanding these factors and their effects is crucial for enabling multidisciplinary teams to develop management and treatment plans for diabetes patients aimed at preventing amputation.
Materials and Methods
Study Setting and Data Collection
This retrospective study was conducted at the Endocrinology Department of a tertiary hospital in eastern China. All patients in the unit were managed in accordance with the established treatment plan for diabetes foot infection. In accordance with the nursing standards of the department, if feasible, wound secretion samples were collected at the bedside or debridement room immediately after admission. That testing included blood plate culture for 18–24 hours to obtain pure colonies, and the preparation of bacterial suspensions. Bacteria were identified with a VITEK2 Compact automatic bacterial identification instrument. Concurrently, MH plates were coated with bacterial suspensions and manual drug sensitivity testing was performed. In cases of suspected systemic infection, blood culture was also conducted. Patients’ clinical characteristics and health status were retrospectively obtained from the hospital information system. A group of experts evaluated comorbidities in accordance with expert consensus and guidelines.
Laboratory examinations performed on samples acquired at admission included blood glucose, glycosylated hemoglobin, creatinine, routine blood examinations, inflammatory index, liver function, thyroid function, blood lipid level, and blood coagulation function. The Wagner grading method was used to assess DFD. Infection severity was assessed using the American Society of Infectious Diseases classifications, which are based on signs of local infection and evidence of systemic infection.22 Complications including peripheral neuropathy and diabetic fundus disease were identified via physical and laboratory examinations recorded by physicians. The study only included cultures collected within the first 2 weeks of hospitalization, not during subsequent coinfections, in an effort to identify primary pathogens. The study was approved by the Helsinki local committee of the hospital (IRB 2023-KY-116). The ethics Committee of The Affiliated Taicang Hospital of Soochow University has confirmed that no need consent in this study, as a retrospective study and data analysis was performed anonymously.
Inclusion Criteria
All patients diagnosed with foot infection due to type 2 diabetes mellitus (T2DM) at the center from January 2016 to December 2020 were included if they were an inpatient and had DFU, foot disease was assessed in accordance with the Wagner classification method, and wound secretion culture and drug sensitivity testing were conducted after admission.
Exclusion Criteria
Patients were excluded if they had taken antibiotics before wound secretion culture and drug sensitivity testing, or had severe liver and kidney dysfunction and could not tolerate normal doses of antibiotics, or if there was a history of anti-infection treatment within 3 months before admission.
Follow-Up and Outcomes
Patients whose wounds healed before discharged from hospital were assigned to a healed group. Patients with an ulcer site that did not heal prior to discharge, and patients who underwent amputation were assigned to a non-healed group. All patients were followed up for 6 months to determine outcomes.
Statistical Analysis
Quantitative continuous variables are expressed as means ± the standard deviation (SD). Categorical variables are expressed as frequencies and percentages. The chi-square test and the t-test were used to compare categorical variables and continuous variables between groups, and the Mann–Whitney U-test was used to compare non-normally distributed variables. Least absolute shrinkage and selection operator (LASSO) regression analysis was used to identify factors related to diabetes prognosis, establish a clinical model and nomogram, generate a model calibration curve, calculate the C-index, and test the reliability of the model via internal verification procedures. Multivariate logistic regression was used to evaluate correlations between covariates, and statistically significant variables were analyzed. Linear relationships between variables and prognosis were then analyzed using a restricted cubic spline chart. These tests were conducted at a significance level of 5%. Statistical analyses were performed using SPSS (version 23.0; Chicago, Illinois, USA) and R (v.4.1.2; https://www.r-project.org) software.
Results
Group Assignment and Baseline Characteristics
A total of 99 patients diagnosed with diabetic foot infection were included in the study, of which 11 (11.1%) experienced adverse events such as non-healing or amputation after treatment and follow-up. Thus, 11 patients were assigned to the non-healed group and 88 were assigned to the healed group. Baseline characteristics are shown in Table 1. There were significant differences in Gram negative bacteria (GNB), Wagner grade, neutrophils, lymphocytes, eosinophils, blood urine nitrogen, lymphocyte-to-C-reactive protein ratio, monocyte-to-lymphocyte ratio, and neutrophil-to-lymphocyte ratio (NLR) between the non-healed group and the healed group (all p < 0.05).
 |
Table 1 Baseline Characteristics |
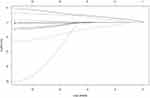
LASSO Regression Analysis and Nomogram Generation
Associated factors that may affect healing after anti-infection treatment in patients with diabetic foot infection were included in the LASSO regression model (p < 0.1 at baseline). At the minimum value of lg (lambda), five factors—Wagner grade, essential hypertension, platelets, GNB, and NLR—emerged as factors that may be related to the prognosis of anti-infection treatment of diabetic foot infection (Figures 1 and 2). Based on the results of LASSO regression, these five factors were used to establish a predictive nomogram. The lower the sum of the specified points in the nomogram, the higher the foot wound healing rate in DFD patients. The C-index was 0.964, calculated as the discrimination value of the nomogram, indicating good predictive power with a bias-corrected C-index of 0.931. Nonsignificant Hosmer-Lemeshow test results using the calibration curve (p = 0.935) indicated that the prediction matched well with observed healing rates (Figure 3).
Validation of Clinical Application of the Nomogram
Decision curve analysis was performed to investigate the net benefit of the predictive model (Figure 4). The results suggested that the nomogram could provide greater net benefit than other models when the threshold probability ranged from 30% to 60%.
 |
Figure 4 Decision curve analysis. Abbreviations: EH, Essential hypertension; G, Gram negative bacteria; NLR, Neutrophil to lymphocyte ratio; PLT, Platelet count. |
Restricted Cubic Spline and Multivariate Logistic Regression Analysis
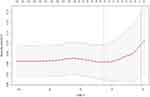
Multivariate logistic regression analysis was used to compare the variables included in the LASSO regression analysis (Table 2). Healing rate was significantly associated with Wagner grade (odds ratio [OR] 12.30, 95% confidence interval [CI] 2.471–61.194, p = 0.002) and platelet count (OR 0.978, 95% CI 0.960–0.996, p = 0.018). Restricted cubic spline modelling indicated a linear association between platelet count and non-healing rate (p for non-linearity = 0.442, Figure 5).
 |
Table 2 Multivariate Logistic Regression Analysis for Predictors of Healed Wound for Diabetes Foot Patients |
Discussion
In the current study Wagner grade, essential hypertension, NLR, GNB, platelet count, and other factors influenced the foot infection healing rate in patients with T2DM. These factors were used to establish a clinical predictive model, and internal validation confirmed the reliability of the model. In multivariate logistic analysis Wagner grade and platelet count were the main factors that affected the prognosis of T2DM patients with foot infection. When the peripheral serum platelet count was <200, it was linearly associated with foot wound prognosis with respect to healing. The lower the platelet count, the worse the prognosis.
In a previous study Gram positive bacteria (GPB) played a leading role in diabetes foot infection in more developed countries, but the prevalence of GNB isolates in low-income people was significantly higher.23 In general, the most common GPB identified via pathogen examination were Staphylococcus aureus, Streptococcus, and Enterococcus, and the most common GNB were Pseudomonas, Escherichia coli, Klebsiella, and Proteus. Differences in these pathogen types may be affected by environmental hygiene, personal hygiene, the use of different footwear, and other factors.23,24 In the present study GPB was dominant in the samples collected, but patients with GPB had poorer prognoses. GNB were more commonly associated with severe sepsis and septic shock than other microorganisms,25 and GNB were more likely to develop drug resistance.26 Although the most effective antibiotic treatment was selected based on drug sensitivity testing of the pathogen in the current study, the development of resistance during the treatment process cannot be ruled out.
In previous studies the NLR has been associated with various infections and bacteremia.27–30 The NLR has been used to predict the prognosis of sepsis patients with inconsistent results. A recent study indicated that NLR may be a useful prognostic biomarker in sepsis patients, and higher NLR values may indicate unfavorable prognoses in these patients.31 In the current study NLR was related to the prognosis of foot infection in diabetes patients, and in the predictive model higher NLR predicted a poorer prognosis. Although the positive association with a poorer prognosis was not strong, there was a trend in that direction.
The prognosis of foot infection in diabetes was clearly predicted by Wagner grade. In a previous study Wagner grade was significantly associated with amputation risk.32 Different Wagner grades have different predictive value for the prognosis of foot infection in diabetes patients. For example, the amputation rates in patients with Wagner grades 4 and 5 were significantly higher than those in patients with lower grades.33–35 Wagner grades ≤ 2 have been associated with significantly lower amputation rates,36–38 thus it can be concluded that increased wagner grade predicts poor outcomes. In the present study Wagner grade was an independent predictor of prognosis in diabetes patients with foot infection, and the higher the Wagner grade the worse the prognosis.
The healing of infected foot wounds in diabetic patients is determined by many factors, and involves keratinocytes, fibroblasts, endothelial cells, macrophages, and platelets.39 The wound healing process is regulated by a complex mixture of growth factors and cytokines released from platelet-α particles. As well as preventing blood loss, platelets can promote tissue regeneration, enhance collagen synthesis, and trigger angiogenesis and immune responses by releasing growth factors and cytokines.40 They can also promote the migration of keratinocytes within a wound, resulting in morphometric and mitotic effects, ensuring formation of a skin barrier.41 Platelets and their derivatives also have specific effects on the treatment of chronic wounds, such as diabetic foot infections and leg ulcers.42 These considerations may explain the linear relationship between wound healing of foot infections and peripheral plasma platelet count in diabetics, which is stronger when the platelet count is <200.
Infection plays an important role in the development of DFU. Combined infection accelerates plantar injury, leading to chronic ulcers, and even systemic infection and osteomyelitis. In the worst cases there is a risk of amputation. Early judgment of the degree of infection is of great significance with respect to predicting future developments and formulating a treatment plan. Long-term use of antibiotics to select resistant microorganisms can reportedly make treatment more difficult and increase the risk of amputation. In the current study the risk of amputation was greater in patients with poor drug treatment compliance. Adherence to prescribed treatment significantly improves the health and quality of life of diabetes patients.43,44 Drug compliance and effectiveness are crucial for the effective treatment of foot infection in diabetics. Therefore, in the present study, in order to reduce drug resistance all antibiotics were selected in strict accordance with the results of pathogen drug sensitivity tests. Relevant research is currently lacking, therefore in conjunction with reducing drug resistance, other factors that affect prognosis should be investigated. The primary aims are to improve prognoses, reduce amputation risks, improve survival rates and quality of life, and reduce patients’ medical expenses. The current study provides a foundation for future research.
The current study had some limitations. It was a single center retrospective study, which may have affected some results by way of insufficient data volume. Secondly, there were differences in the use of antibiotics by select patients before drug sensitivity test results were available, and this may have affected the final results.
Conclusion
The clinical model described herein can predict healing of infected foot ulcers in T2DM patients. The model incorporates Wagner grade, essential hypertension, platelet count, GNB, and NLR. There was a linear relationship between healing outcome and plasma platelet level, and when the Wagner grade was 2 and the platelet level was ≤ 200, a lower platelet level indicated a worse wound healing prognosis.
Abbreviations
BUN, blood urine nitrogen; CAD, coronary artery disease; CI, confidence interval; DFU, Diabetic Foot Ulcer; EH, essential hypertension; GNB, Gram negative bacteria; GPB, Gram positive bacteria; HIS, Hospital Information System; LASSO, Least absolute shrinkage and selection operator; MLR, monocyte to lymphocyte ratio; NLR, neutrophily to lymphocyte ratio; PVD, peripheral vascular disease; PLT, platelet; RCS, restricted cubic spline; T2DM, type 2 diabetic mellitus.
EthicaI Approval
The study was carried out in accordance with the Declaration of Helsinki and was approved by the Institutional Ethics Committee of the Affiliated Taicang Hospital of Soochow University (IRB: 2023-KY-116). As a retrospective study and data analysis was performed anonymously, this study was exempt from the informed consent from patients.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. International Diabetes Federation. IDF diabetes atlas. 9th edition. Brussels, Bel Gium Atlas. Brussels, Belgium: IDF Diabetes; 2019. Available from: https://www.diabetesatlas.org.
2. Brechow A, Slesaczeck T, Münch D, et al. Improving major amputation rates in the multicomplex diabetic foot patient: focus on the severity of peripheral arterial disease. Ther Adv Endocrinol Metab. 2013;4(3):83–94. doi:10.1177/2042018813489719
3. Crawford F, Cezard G, Chappell FM; PODUS Group. The development and validation of a multivariable prognostic model to predict foot ulceration in diabetes using a systematic review and individual patient data meta-analyses. Diabet Med. 2018;35(11):1480–1493. doi:10.1111/dme.13797
4. Kaminski MR, Raspovic A, McMahon LP, et al. Risk factors for foot ulceration and lower extremity amputation in adults with end-stage renal disease on dialysis: a systematic review and meta-analysis. Nephrol Dial Transplant. 2015;30(10):1747–1766. doi:10.1093/ndt/gfv114
5. Gordois A, Scuffham P, Shearer A, Oglesby A, Tobian JA. The health care costs of diabetic peripheral neuropathy in the US. Diabetes Care. 2003;26(6):1790–1795. doi:10.2337/diacare.26.6.1790
6. Gazzaruso C, Gallotti P, Pujia A, Montalcini T, Giustina A, Coppola A. Predictors of healing, ulcer recurrence and persistence, amputation and mortality in type 2 diabetic patients with diabetic foot: a 10-year retrospective cohort study. Endocrine. 2021;71(1):59–68. doi:10.1007/s12020-020-02431-0
7. Ugwu E, Adeleye O, Gezawa I, Okpe I, Enamino M, Ezeani I. Predictors of lower extremity amputation in patients with diabetic foot ulcer: findings from MEDFUN, a multi-center observational study. J Foot Ankle Res. 2019;12:34. doi:10.1186/s13047-019-0345-y
8. Reiber GE, Vileikyte L, Boyko EJ, et al. Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Diabetes Care. 1999;22(1):157–162. doi:10.2337/diacare.22.1.157
9. Lazarus GS, Cooper DM, Knighton DR, Percoraro RE, Rodeheaver G, Robson MC. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen. 1994;2(3):165–170. doi:10.1046/j.1524-475X.1994.20305.x
10. Natarajan S, Williamson D, Stiltz AJ, Harding K. Advances in wound care and healing technology. Am J Clin Dermatol. 2000;1(5):269–275. doi:10.2165/00128071-200001050-00002
11. Velnar T, Bailey T, Smrkolj V. The wound healing process: an overview of the cellular and molecular mechanisms. J Int Med Res. 2009;37(5):1528–1542. doi:10.1177/147323000903700531
12. Weck M, Slesaczeck T, Paetzold H, et al. Structured health care for subjects with diabetic foot ulcers results in a reduction of major amputation rates. Cardiovasc Diabetol. 2013;12(1):45. doi:10.1186/1475-2840-12-45
13. Cahn A, Elishuv O, Olshtain-Pops K. Establishing a multidisciplinary diabetic foot team in a large tertiary hospital: a workshop. Diabetes Metab Res Rev. 2014;30(5):350–353. doi:10.1002/dmrr.2527
14. Sanders LJ, Robbins JM, Edmonds ME. History of the team approach to amputation prevention: pioneers and milestones. J Vasc Surg. 2010;52(3 Suppl):3S–16S. doi:10.1016/j.jvs.2010.06.002
15. Lipsky BA, Senneville É, Abbas ZG, et al. Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3280. doi:10.1002/dmrr.3280
16. Ndosi M, Wright-Hughes A, Brown S, et al. Prognosis of the infected diabetic foot ulcer: a 12-month prospective observational study. Diabet Med. 2018;35(1):78–88. doi:10.1111/dme.13537
17. Van Olmen J, Marie KG, Christian D, et al. Content, participants and outcomes of three diabetes care programmes in three low and middle income countries. Prim Care Diabetes. 2015;9(3):196–202. doi:10.1016/j.pcd.2014.09.001
18. Quddus MA, Uddin MJ. Evaluation of foot ulcers in diabetic patients. Mymensingh Med J. 2013;22(3):527–532.
19. Markowitz JS, Gutterman EM, Magee G, Margolis DJ. Risk of amputation in patients with diabetic foot ulcers: a claims-based study [published correction appears in Wound Repair Regen. 2007 Jan-Feb; 15(1):163]. Wound Repair Regen. 2006;14(1):11–17. doi:10.1111/j.1743-6109.2005.00083.x
20. Carlson T, Reed JF. A case-control study of the risk factors for toe amputation in a diabetic population. Int J Low Extrem Wounds. 2003;2(1):19–21. doi:10.1177/1534734603002001004
21. Chaturvedi N, Stevens LK, Fuller JH, Lee ET, Lu M. Risk factors, ethnic differences and mortality associated with lower-extremity gangrene and amputation in diabetes. The WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44(Suppl 2):S65–S71. doi:10.1007/pl00002941
22. Monteiro-Soares M, Russell D, Boyko EJ, et al. Guidelines on the classification of diabetic foot ulcers (IWGDF 2019). Diabetes Metab Res Rev. 2020;36(Suppl 1):e3273. doi:10.1002/dmrr.3273
23. Ramakant P, Verma AK, Misra R, et al. Changing microbiological profile of pathogenic bacteria in diabetic foot infections: time for a rethink on which empirical therapy to choose? Diabetologia. 2011;54(1):58–64. doi:10.1007/s00125-010-1893-7
24. Mishra SC, Chhatbar KC, Kashikar A, Mehndiratta A. Diabetic foot. BMJ. 2017;359:j5064. doi:10.1136/bmj.j5064
25. Abe R, Oda S, Sadahiro T, et al. Gram-negative bacteremia induces greater magnitude of inflammatory response than Gram-positive bacteremia. Crit Care. 2010;14(2):R27. doi:10.1186/cc8898
26. Giske CG, Monnet DL, Cars O, Carmeli Y; ReAct-Action on on Antibiotic Resistance. Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob Agents Chemother. 2008;52(3):813–821. doi:10.1128/AAC.01169-07
27. Loonen AJ, de Jager CP, Tosserams J, et al. Biomarkers and molecular analysis to improve bloodstream infection diagnostics in an emergency care unit. PLoS One. 2014;9(1):e87315. doi:10.1371/journal.pone.0087315
28. de Jager CP, van Wijk PT, Mathoera RB, de Jongh-Leuvenink J, van der Poll T, Wever PC. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care. 2010;14(5):R192. doi:10.1186/cc9309
29. Ljungström L, Pernestig AK, Jacobsson G, Andersson R, Usener B, Tilevik D. Diagnostic accuracy of procalcitonin, neutrophil-lymphocyte count ratio, C-reactive protein, and lactate in patients with suspected bacterial sepsis. PLoS One. 2017;12(7):e0181704. doi:10.1371/journal.pone.0181704
30. Asik Z. The Role of the NLR and PLR in Urinary Tract Infection. Clin Lab. 2021;67(10). doi:10.7754/Clin.Lab.2021.210133
31. Huang Z, Fu Z, Huang W, Huang K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: a meta-analysis. Am J Emerg Med. 2020;38(3):641–647. doi:10.1016/j.ajem.2019.10.023
32. Dos Santos VP, da Silveira DR, Caffaro RA. Risk factors for primary major amputation in diabetic patients. Sao Paulo Med J. 2006;124(2):66–70. doi:10.1590/s1516-31802006000200004
33. Shin JY, Roh SG, Sharaf B, Lee NH. Risk of major limb amputation in diabetic foot ulcer and accompanying disease: a meta-analysis. J Plast Reconstr Aesthet Surg. 2017;70(12):1681–1688. doi:10.1016/j.bjps.2017.07.015
34. International Diabetes Federation. IDF Diabetes Atlas, Eighth Edition 2017; 2018. Available from http://www.diabetesatlas.org.
35. Uçkay I, Gariani K, Pataky Z, Lipsky BA. Diabetic foot infections: state-of-The-art. Diabetes Obes Metab. 2014;16(4):305–316. doi:10.1111/dom.12190
36. Armstrong DG, Boulton AJM, Bus SA, Ingelfinger JR. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–2375. doi:10.1056/NEJMra1615439
37. Selva Olid A, Solà I, Barajas-Nava LA, Gianneo OD, Bonfill Cosp X, Lipsky BA. Systemic antibiotics for treating diabetic foot infections. Cochrane Database Syst Rev. 2015;2015(9):CD009061. doi:10.1002/14651858.CD009061.pub2
38. Prompers L, Huijberts M, Apelqvist J, et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia. 2007;50(1):18–25. doi:10.1007/s00125-006-0491-1
39. Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16(5):585–601. doi:10.1111/j.1524-475X.2008.00410.x
40. Nurden AT, Nurden P, Sanchez M, Andia I, Anitua E. Platelets and wound healing. Front Biosci. 2008;13:3532–3548. doi:10.2741/2947
41. Seeger MA, Paller AS. The roles of growth factors in keratinocyte migration. Adv Wound Care. 2015;4(4):213–224. doi:10.1089/wound.2014.0540
42. Akingboye AA, Giddins S, Gamston P, Tucker A, Navsaria H, Kyriakides C. Application of autologous derived-platelet rich plasma gel in the treatment of chronic wound ulcer: diabetic foot ulcer. J Extra Corpor Technol. 2010;42(1):20–29. doi:10.1051/ject/201042020
43. Pscherer S, Dippel FW, Lauterbach S, Kostev K. Amputation rate and risk factors in type 2 patients with diabetic foot syndrome under real-life conditions in Germany. Prim Care Diabetes. 2012;6(3):241–246. doi:10.1016/j.pcd.2012.02.004
44. Venermo M, Manderbacka K, Ikonen T, Keskimäki I, Winell K, Sund R. Amputations and socioeconomic position among persons with diabetes mellitus, a population-based register study. BMJ Open. 2013;3(4):e002395. doi:10.1136/bmjopen-2012-002395
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.