Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Prognostic Value of Neutrophil to Lymphocyte Ratio for Predicting 90-Day Poor Outcomes in Hospitalized Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease
Authors Feng X , Xiao H, Duan Y , Li Q, Ou X
Received 14 December 2022
Accepted for publication 30 May 2023
Published 14 June 2023 Volume 2023:18 Pages 1219—1230
DOI https://doi.org/10.2147/COPD.S399671
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Xiaoyi Feng,1,* Huaye Xiao,2,* Yishan Duan,1 Qinxue Li,1 Xuemei Ou1
1Department of Respiratory and Critical Care Medicine, West China Hospital of Sichuan University, Chengdu, 610041, People’s Republic of China; 2Department of Respiratory and Critical Care Medicine, Fushun People’s Hospital, Zigong, Sichuan, 643200, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xuemei Ou, Department of Respiratory and Critical Care Medicine, West China Hospital of Sichuan University, Chengdu, 610041, People’s Republic of China, Email [email protected]
Objective: This study aimed to evaluate the predictive value of neutrophil to lymphocyte ratio (NLR) for poor outcomes within 90-day in hospitalized patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD).
Methods: A retrospective study including 503 AECOPD patients was performed, and the subjects’ clinical characteristics were collected. Binary logistic regression analysis was used to identify risk factors for 90-day poor outcomes in patients with AECOPD. Receiver-operating characteristic curves (ROC) and areas under the curves (AUC) were used to assess the ability of different biomarkers to predict the risk of 90-day mortality, readmission and re-exacerbation in patients with AECOPD.
Results: During the follow-up, 188 patients (38.4%) redeveloped exacerbations, 112 patients (22.9%) were readmitted, and 20 patients (4.1%) died directly resulted from COPD or COPD-related causes. Multivariate analysis demonstrated that age> 72 years (OR: 14.817, 95% CI: 1.561– 140.647), NLR> 14.17 (OR: 9.611, 95% CI: 2.303– 40.113), EOS< 0.15% (OR: 8.621, 95% CI: 3.465– 34.913) and BNP> 2840ng/L (OR: 5.291, 95% CI: 1.367– 20.474) at discharge were independent risk factors for 90-day mortality in AECOPD patients. NLR was the optimal biomarker for predicting 90-day mortality with an AUC of 0.802 (95% CI: 0.631– 0.973). Using 14.17 as the critical value of NLR, the sensitivity was 76.7%, and the specificity was 88.9%. Compared with mortality, NLR had no significant advantage in predicting risk of short-term re-exacerbation (AUC=0.580, 95% CI:0.529– 0.632, p=0.001) and readmission (AUC=0.555, 95% CI:0.497– 0.614, p=0.045), with AUCs less than 0.6. In contrast, the predictive value of EOS (AUC=0.561, 95% CI:0.502– 0.621, p=0.038) was slightly better than NLR in terms of readmission within 90 days. CRP did not serve as a well predictive biomarker for the risk of readmission and re-deterioration (p> 0.05).
Conclusion: NLR is of great value in predicting the risk of poor outcomes, especially COPD associated mortality, in hospitalized patients with AECOPD within 90 days after discharge.
Keywords: acute exacerbation of chronic obstructive pulmonary disease, neutrophil to lymphocyte ratio, mortality, readmission, eosinophil count, C-reactive protein, biomarker
Introduction
Chronic obstructive pulmonary disease (COPD) is one of the leading causes of morbidity and mortality worldwide, imposing substantial burden on medical and health resources.1,2 Acute exacerbation of COPD (AECOPD) is a critical condition where patients experience deterioration during the course of disease, easily inducing adverse events such as respiratory failure, respiratory distress syndrome, even hospitalization and mortality.3–5 Following an exacerbation episode, patients typically require a recovery period of 8–12 weeks to reach a state of clinical stability. This window is also associated with an increased risk of recurrent exacerbation, with studies indicating a 90-day readmission rate of approximately 30%.6,7 Furthermore, mortality rates remain high even after hospital discharge.6 Given these challenges, critical and prompt assessment of patients’ risk of adverse prognosis is crucial for providing informed medical decisions such as treatment intensification, therapy modification, and follow-up duration post-discharge.
The chronic inflammation plays a crucial role in the pathogenesis of COPD, and is closely linked to the acute onset, severity and prognosis.7 Extensive efforts have been made to identify reliable biomarkers that reflect disease severity and response to treatment. C-reactive protein (CRP) has been demonstrated to be related with disease severity, prognosis, diagnosis of acute exacerbations and complications.8–10 However, conflicting results have been reported regarding the usefulness of CRP in predicting short-term prognosis, which has hampered its clinical applications.11–13 Meanwhile, researches have suggested that increased eosinophil count(EOS) in stable COPD patients is correlated with a more favorable therapeutic response to glucocorticoids and an increased risk of future exacerbations.1,14–16 Nevertheless, the susceptibility of EOS to other factors and its fluctuation make it challenging to use as a definitive predictor of poor prognosis.14–16
In recent years, the neutrophil to lymphocyte ratio (NLR), reflecting changes in the immune system and inflammation, has gained attention as a systemic inflammatory biomarker due to its rapid, widely available and inexpensive assessment, particularly in chronic diseases.17–20 Gunay et al firstly utilized the NLR as a valuable biomarker for severity of inflammation in patients with COPD,21 while subsequent studies highlighted its significance as an independent predictor for the severity of COPD exacerbation and mortality.22,23 Notably, a systematic review and meta analysis have reported significant correlations between NLR and clinical symptoms, pulmonary function parameters, increased risk of bacterial infections, in-hospital, early (first 90 days) and late (within 24 months) mortality in AECOPD patients.24 Another meta-analysis of 5140 patients included in 9 studies by Ye et al similarly showed that higher NLR was associated with higher risk of exacerbation (OR:3.81, 95% confidence interval(CI):1.20–12.13) and mortality (OR:2.60, 95% CI:1.48–4.57), including short-term or long-term mortality.25 Nonetheless, there is a scarcity of correlational studies elucidating whether NLR holds a substantial advantage over other biomarkers for predicting poor prognosis after discharge, specifically regarding short-term mortality, re-exacerbation and readmission.
The aim of this study was to evaluate and contrast the predictive efficacy of NLR alongside other biomarkers such as EOS and CRP in gauging the possibility of mortality, readmission, and re-exacerbation within 90 days in patients with AECOPD to further explore the value of NLR in the clinical application of AECOPD.
Materials and Methods
Patients
A total of 503 patients admitted to west China hospital of Sichuan University from March 2015 to February 2021 and primarily diagnosed with “AECOPD” were included according to the criteria developed by the Global Initiative on Chronic Obstructive Pulmonary Disease (GOLD) in 2021.1 Patients with lung cancer, pure asthma, severe cardiovascular and cerebrovascular diseases, autoimmune disease, hematologic tumor and other diseases that may affect the relevant clinical indicators on the basis of the judgment of physicians, and patients with incomplete clinical data were excluded. This study was retrospective and approved by the Biomedical Ethics Review Committee of west China hospital of Sichuan University (No.2021–1374). This study complied with the Declaration of Helsinki.
Diagnostic criteria of COPD: a. the presence of respiratory symptoms such as chronic cough and expectoration and imaging tests suggesting manifestations of chronic bronchitis and emphysema, b. pulmonary function test (PFT) showing persistent airflow limitation after inhalation of bronchodilators, c. exclusion of other known diseases with airflow limitation. Spirometry was performed using Vmax 22 (SensorMedics, Yorba Linda, California, USA) and PFDX (MedGraphics, St. Paulo, Minnesota, USA) according to American Thoracic Society guidelines. Lung volumes were measured 15 minutes after administration of 400 μg salbutamol. The ratio of forced expiratory volume in the first second to forced vital capacity < 70% (FEV1/FVC<70%) was used to indicate persistent airflow limitation.
Diagnostic criteria of AECOPD: a. an acute sustained deterioration of dyspnea, cough and/or sputum beyond normal day-to-day variations in a patient with underlying COPD, requiring a change in conventional medication or even hospitalization, b. exclusion of other known causes of deterioration of respiratory function such as acute coronary syndrome, pneumothorax and pleural effusion and so on.1
The diagnosis of COPD was based on the PFT performed by the patients in the past, while most of the patients in this study were unable to complete the PFT during their hospitalization due to the severe conditions, so the pulmonary function parameters were not involved.
Predictors
Enrolled patients’ baseline information, first and last laboratory tests, and treatment measures, complications, and outcomes during hospitalization were collected through an electronic medical record system. Firstly, baseline information included age, gender, body mass index (BMI), smoking history, and history of previous frequent exacerbations. Secondly, laboratory tests included inflammatory indicators such as NLR, blood eosinophil count, C-reactive protein (CRP), interleukin-6 (IL-6), procalcitonin (PCT) as an infection index, coagulation indicators such as D-dimer and fibrinogen, brain natriuretic peptide (BNP) used to assess heart failure, arterial blood gas analysis and other biochemical parameters. Clinical information during hospitalization included oxygen therapy, glucocorticoids administration, the incidence of complications such as respiratory failure, heart failure, pneumonia, fungal infections and multi-drug resistant bacterial infections and mortality during hospitalization.
In this study, the history of previous frequent exacerbations was defined as occurring ≥2 moderate-to-severe exacerbations per year. Oxygenation index was calculated as the ratio of the partial pressure of arterial oxygen to the fraction of inspired oxygen (PaO2/FiO2). The laboratory indicators at admission (before treatment) referred to the values initially measured within 24 hours after admission, and the values at discharge (after treatment) were measured within 72 hours before discharge or death. There was no variation between the measurement times of each assay for different biomarkers.
Outcomes
In this study, every patient was surveyed for major events, including acute exacerbation, new diseases, accidents, readmission or death within 3 months after discharge, on an outpatient visit or by telephone. The mainly poor outcomes were re-exacerbation, readmission and COPD associated mortality within 90 days. If a cause other than COPD was dominant, as assessed by the attending physician, the deterioration was not regarded as an exacerbation. COPD associated mortality was calculated from the deaths that directly resulted from COPD or COPD-related causes.
All the diagnoses were eventually made by two senior respiratory physicians based on a combination of history, clinical symptoms, and imaging findings.
Statistical Analysis
The analysis was performed with SPSS 24.0 (SPSS Inc., Chicago, IL, USA). Qualitative variables were expressed as counts and frequencies, use Fisher’s exact test or χ2 test depending on data. Quantitative variables that conform to normal distribution were expressed as mean and standard deviation(SD), otherwise median and interquartile range (IQR) were applied, compared by t-test or Mann–Whitney U-test. The Youden index was utilized to calculate the cut-off value of each variable, and receiver operating characteristic (ROC) curve analysis was used to evaluate the sensitivity and specificity of different potential predictors of adverse prognosis. The area under the curve (AUC) was used to assess prognostic accuracy, which ranges from 0.5 to 1.0 – with higher values indicating higher discriminatory ability. Univariate logistic regression analysis was performed to identify risk factors for 90-day mortality in patients with AECOPD. All p values were two-sided and risk factors with p values <0.10 in univariate analysis were included in a multivariate analysis. A stepwise approach was used to identify the combination of variables that most accurately predicted the risk of death within 90 days after discharge, resulting in a prediction model in patients with AECOPD. In this study, p< 0.05 was considered as statistically significant.
Results
Patient Characteristics
Among the 503 patients, 371 (73.8%) were male, the median age was 74 years old, from 40 to 95 years old, and 148 (29.4%) had a history of frequent exacerbation. The average length of hospitalization was 15 days, from 3 to 83 days. In addition, 14 patients (2.8%) died during hospitalization. During the follow-up, 188 patients (38.4%) redeveloped exacerbations, 112 patients (22.9%) were readmitted, and 20 patients (4.1%) died directly resulted from COPD or COPD-related causes.
Prognostic Factors of 90-Day Mortality in AECOPD Patients
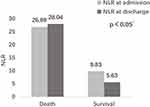
In order to explore risk factors associated with short-term mortality of AECOPD, patients were divided into death group and survival group. The results showed that patients in the death group were older (78.25±6.18 vs 71.60±9.76, p=0.015) and no statistical difference in terms of gender, BMI, smoking index and history of frequent exacerbation was observed between two groups. Significant increase of the levels of NLR (28.04±10.24 vs 5.63 ± 2.76, p=0.001), CRP (48.67mg/L vs 14.83mg/L, p=0.025), BNP (4779.85±539.94ng/L vs 1591.83±368.95ng/L, p=0.001) and D-dimer (4.16±2.51mg/L FEU vs 1.98±1.18mg/L FEU, p=0.002) were observed in death group. In addition, in death group the level of EOS (0.38±0.05 vs 2.20±1.21, p=0.000) was lower than those of survival group. Our data did not show obvious correlations between IL-6 and PCT and mortality in AECOPD patients (Table 1).
 |
Table 1 Comparison of Clinical Characteristics Between Death Group and Survival Group Within 90 Days After Discharge |
In the death group, patients had a higher proportion of combined cor pulmonale (25.0% vs 9.2%, p=0.037) and a greater probability of mechanical ventilation (80.0% vs 29.6%, p=0.000) and systemic glucocorticoids use (65.0% vs 42.0%, p=0.042) during hospitalization, accompanied by a longer mean time required for mechanical support (8.84±3.01d vs 4.49±3.99d, p=0.020). On the other hand, a greater likelihood of concurrent pneumonia was observed (85.0% vs 57.8%, p=0.015), with an elevated proportion of co-infections with fungi compared to the survival group, although there were no statistically significant difference (p<0.10). No statistical difference was observed in terms of duration of hospitalization, respiratory failure, heart failure and multi-drug resistant bacterial infections (p>0.05) (Table 1).
Binary logistic regression was performed with these associated factors using a stepwise method. Among these, multivariate analysis demonstrated that age>72 years (OR: 14.817, 95% CI: 1.561–140.647), NLR>14.17 (OR: 9.611, 95% CI: 2.303–40.113), EOS<0.15% (OR: 8.621, 95% CI: 3.465–34.913) and BNP>2840ng/L (OR: 5.291, 95% CI: 1.367–20.474) were independent risk factors for 90-day mortality in AECOPD patients (Table 2). In addition to age, NLR was the strongest predictive biomarker of short-term COPD-related mortality. Compared to patients with NLR≤14.17, patients with NLR>14.17 at discharge had a 9.611-fold increased risk of death within 3 months. Blood eosinophil count was inversely associated with short-term adverse outcomes prognosis. The predictive accuracy of the final model included these four variables was shown with a sensitivity of 89.0% and a specificity of 85.4%. The AUC of this model was 0.929 (95% CI: 0.862–0.995), which was significantly better than the prediction accuracy of a single NLR indicator (Figure 1).
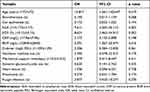 |
Table 2 Multivariate Regression Analysis of Risk Factors for Mortality Within 90 Days in Patients with AECOPD |
Predictive Value of NLR for 90-Day Mortality, Re-Exacerbation and Readmission
NLR was the optimal biomarker for predicting 90-day mortality with an AUC of 0.802 (95% CI:0.631–0.973), followed by BNP (AUC=0.766,95% CI: 0.616–0.916) and EOS (AUC=0.741, 95% CI:0.610–0.873). Using 14.17 as the critical value of NLR, the sensitivity was 76.7%, and the specificity was 88.9% (Figure 1). The accuracy of EOS for predicting the risk of mortality appeared to be slightly better than CRP. CRP for predicting 90-day mortality was poor (AUC=0.652, 95% CI:0.503–0.801).
The same way for analysis was also used to explore the predictive value of NLR, EOS and CRP for recurrent exacerbation and readmission within 90 days. The results showed that compared with mortality, NLR had no significant advantage in predicting risk of short-term recurrent exacerbation (AUC=0.580, 95% CI:0.529–0.632, p=0.001) and readmission (AUC=0.555, 95% CI:0.497–0.614, p=0.045) in patients with AECOPD, with AUCs less than 0.6. In contrast, the predictive value of EOS (AUC=0.561, 95% CI:0.502–0.621, p=0.038) was slightly better than NLR in terms of readmission within 90 days (Figure 2). Nevertheless, CRP did not serve as a well predictive biomarker for the risk of readmission and re-deterioration (p>0.05).
 |
Figure 2 The ROC curves of the different biomarkers for predicting the risk of (A) re-exacerbation and (B) readmission within 90 days in patients with AECOPD. |
Correlation of NLR with Severity of Disease and Short-Term Poor Prognosis
To further investigate the relationship between NLR and severity of disease, as well as its mechanism for predicting short-term adverse prognosis, all enrolled patients were classified into the high NLR group (NLR>14.17) and low NLR group (NLR≤14.17) according to their NLR levels upon admission to control for potential confounding factors such as comorbid infections and medication use during hospitalization. In the high NLR group, elderly (75.00±8.11 vs 71.32±9.95, p=0.017) and comorbid patients with coronary heart disease and cor pulmonale were more common (p<0.05). They exhibited higher levels of inflammation markers CRP and IL-6, bacterial infection-related indicators PCT, D-dimer and fibrinogen at admission than those in the low NLR group, while EOS was significantly lower in the high NLR group (p<0.05).
Additionally, patients in the high NLR group required longer hospital stay (16.4±6.9d vs 14.5±7.7d, p=0.001), more need for mechanical ventilation assistance (58.6% vs 27.0%, p=0.000) and longer time with the machine (7.6±5.2d vs 3.9±3.4d, p=0.048), as well as a greater proportion of systemic glucocorticoids use (53.5% vs 40.8%, p=0.022). Patients with high NLR level were significantly more prone to develop multiple serious complications during hospitalization, including respiratory failure, heart failure, pneumonia, fungal and multi-drug resistant organisms infections (p<0.05)(Table 3).
 |
Table 3 Comparison of Clinical Characteristics Between High NLR Group and Low NLR Group at Admission |
More importantly, the risk of death during hospitalization was significantly higher in the high NLR group compared to the low NLR group (10.1% vs 1.0%, p=0.000). Similarly, the risk of re-exacerbation (47.5% vs 34.9%, p=0.020) and mortality (14.1% vs 1.5%, p=0.000) within 90 days after discharge was obviously higher in the high NLR group, with no statistical difference in the risk of readmission (28.3% vs 20.8%, p>0.05) (Table 3).
Comparison of Changes in NLR Before and After Hospitalization Between Death and Survival Group
Comparing the NLR values of the death and survival groups tested at the same time of admission and discharge, respectively, it was found that NLR of the survival group decreased significantly at discharge, while NLR of the death group remained extremely high even at discharge, surpassing the admission level. The NLR of the death group remained significantly elevated compared to that of the survival group, both at admission (pre-treatment) (26.89±10.24 vs 9.83±5.76, p=0.001) and at discharge (post-treatment) (28.04±17.05 vs 5.63±3.23, p=0.000) (Figure 3).
Discussion
This study aimed to explore the potential correlation between the levels of biomarkers at discharge in hospitalized patients with AECOPD and their prognosis within 90 days. Through multivariate analysis, we identified several independent risk factors for 90-day mortality in AECOPD patients, including age>72 years, NLR>14.17, EOS<0.15%, and BNP> 2840ng/L at discharge. NLR was found to be the most reliable predictive biomarker for short-term mortality. Furthermore, in comparison to CRP, NLR was found to be more useful in predicting poor outcomes within 90 days after discharge in patients with AECOPD. However, NLR had no discernible benefit in predicting risk of short-term re-exacerbation and readmission compared to mortality.
Chronic inflammation with increased numbers of specific inflammatory cell types is an important pathogenesis of COPD. In general, an increased number of activated neutrophils are found in patients with COPD, which is related to the severity of the disease.7 Meanwhile, more and more studies have shown that critically ill patients always have low lymphocyte counts which is associated with poor outcomes, regardless of weather patients suffer from acute medical conditions or with chronic inflammatory diseases.13,26 However, little is known about the mechanism of lymphopenia in patients with chronic inflammatory diseases such as COPD. Some researchers hypothesized that apoptosis and redistribution of lymphocytes may occur in the development of AECOPD,26 and patients with COPD are mostly older and have poor nutrition,20 which may also be associated with low lymphocyte levels.20 NLR is the blood neutrophil to lymphocyte ratio. Recent researches have shown that NLR can be used as an inflammatory marker to evaluate the severity of AECOPD and to predict the prognosis.15–18,27,28 Allan Klitgaard Sørensen et al prospectively followed 386 patients with moderate to very severe COPD for 10 years and they found that NLR and low lymphocyte count were independent predictors of increased 5-year all-cause mortality in patients with moderate to very severe COPD.20
In the current study, NLR at discharge was significantly linked to short-term adverse outcomes, with mortality risk rising in accordance with NLR levels. Compared to those with NLR≤14.17, patients with NLR>14.17 at discharge exhibited a 9.611-fold heightened risk of death within 3 months. In addition, this study focused on the correlation between changes at admission and at discharge and the risk of mortality. Results demonstrated that the death group exhibited higher NLR levels at discharge than at admission. This finding may indicate that patients with higher NLR may experience worse outcomes during hospitalization, potentially correlated with the severity of the condition and poor response to anti-inflammatory treatment. The GOLD guideline recommends EOS as a critical biomarker for evaluating the benefits of ICS treatment in COPD patients.1 Conversely, AECOPD patients with lower level of EOS exhibit a poorer response to glucocorticoids, even increasing vulnerability to side effects of hormones, like secondary fungal infections.29–31 Our study identified that the high NLR group showed lower EOS levels upon admission, and patients who passed away after discharge continued to exhibit higher NLR and lower EOS levels than the survival group. These findings supported a rationale for ineffective glucocorticoid therapy and worse prognosis within those patients.
C-reactive protein (CRP) represents low-grade systemic inflammation and has been widely used in expressing disease severity in COPD.10 In recent years, some researchers have found that inflammatory biomarkers such as CRP have been associated with poor prognosis and can predict mortality and hospitalization in COPD.6–8,32 In a prospective and multicenter study by Bartolome R Celli et al, the authors concluded that CRP is associated with increased risk of death in patients with COPD.10 Moy et al suggested that combining CRP with step count is a good predictor of acute exacerbations (C-statistic=0.59) and hospital admission (C-statistic=0.69) in their observational cohort study of 167 persons with COPD.33 However, the value of CRP in predicting COPD prognosis has been inconsistent and clinical use has been hampered. Recent data suggest that CRP is elevated during an acute exacerbation of COPD but CRP alone is neither sensitive nor specific in predicting clinical severity or outcome. In a retrospective research, using clinical data from 218 stable patients with COPD, Juan P. de Torres et al have found that in patients with moderate to very severe COPD, CRP levels are not associated with survival status.11 In another study, Mia Moberg and his college found that CRP mostly expressed disease severity but did not add further information about prognosis in patients with severe COPD.13 In the meanwhile, more and more scientific evidence points to that the presence of eosinophils in patients with COPD predicts a more favourable therapeutic response to corticosteroids and is associated with prognosis, mortality, and structural change in COPD.32 Yeon-Mok Oh’s study, including 629 patients reported that in COPD, the severity of emphysema was independently linked with low blood eosinophil count and the longer survival period was associated with increased blood eosinophil count.16 In a study by Dildar Duman et al, where COPD patients were grouped into eosinophilic and non-eosinophilic patients, non-eosinophilic patients who experience COPD exacerbations have poorer outcomes than eosinophilic patients.34 Interestingly, in the Copenhagen study enrolled 7225 patients with stable COPD, it was found that patients with moderate-to-severe COPD who were not taking ICS and EOS≥2% experienced higher exacerbation frequency than patients with lower level of EOS.35
In this research the predictive values of NLR, CRP and EOS for AECOPD were examined. In terms of 90-day mortality, readmission, and re-exacerbation, it was discovered that NLR exhibited a stronger predictive value than CRP. The predictive accuracy of EOS for mortality was somewhat better than CRP. CRP has no significant value in predicting the risk of readmission and reworsening. The results regarding NLR and CRP were in line with Luo’s study. They discovered that NLR demonstrated a considerable advantage over CRP in predicting 28-day mortality in patients with AECOPD, with an AUC of 0.801 compared to 0.740 for CRP.18 Although EOS demonstrated marginally higher predictive accuracy for readmission, it is not recommended to rely solely on a single metric to predict both readmission and re-exacerbation.
Through univariate and multivariate regression analysis, it was of great value to use age, NLR, EOS and BNP at discharge to predict the risk of death within 3 months after discharge. The model exhibited high sensitivity and specificity, surpassing the predictive accuracy of individual NLR indicators. These findings suggested an increased risk of mortality associated with old age, elevated levels of inflammation at discharge and concomitant heart failure. Therefore, it was recommended a comprehensive assessment of patient condition and prognosis using multiple indicators, aiding clinicians in stratifying patients with AECOPD, with a particular emphasis on those with high levels of NLR both at admission and discharge. More importantly, early and aggressive intervention, as well as prompt follow-up, were emphasized to improve patient outcomes.
Furthermore, the present study showed that no superiority of NLR was observed for the predictive value of short-term acute exacerbation and readmission risk. Acute exacerbation of COPD is defined as worsening of the patient’s baseline dyspnoea, cough and/or sputum[4]. Until now, the specificity of the definition is poor, because many other respiratory or non-respiratory diseases will have similar manifestations and the diagnosis often depends on understanding the medical history and all current symptoms (including fatigue, fatigue, depression, etc.), as well as evaluating oxygen saturation, complete blood count and other necessary inspections. The sensitivity is also poor. This is because patients have very different perceptions of symptoms. There may be errors in the way we used telephone and outpatient follow-up. Recently, Using the modified Delphi method, Celli and other experts developed a new definition and classification system for acute exacerbations (the Rome proposal), published in Blue Journal.36 Compared with the definition commonly used today, the most significant feature of the Rome proposal is standardization and quantification, but its clinical practical value needs to be confirmed by research.28 Further prospective studies need to be designed to investigate the predictive value of NLR for post-discharge acute exacerbation and readmission in patients with AECOPD through more rigorous follow-up.
This study also has a few limitations. This study was a retrospective and confined to a single center. One of the weakness of this study was that most patients in our study lacked pulmonary function test due to severe illness, so there was no classification of airflow limitation severity in all COPD cases. More prospective studies are needed in the future to explore the value of NLR in the clinical application of AECOPD.
Conclusion
NLR is of great value in predicting the risk of poor outcomes, especially COPD associated mortality, in hospitalized patients with AECOPD within 90 days. It was suggested combining the age, NLR, EOS and BNP at discharge to improve the accuracy of prediction for 90-day mortality.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Science Foundation of China (Grants No.31671189) and the Sichuan Science and Technology Agency (Grants No.2018SZ0109).
Disclosure
Xiaoyi Feng and Huaye Xiao are co-first authors for this study. The authors report no conflicts of interest in this work.
References
1. Halpin DMG, Criner GJ, Papi A, et al. Global Initiative for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease. The 2020 GOLD Science Committee Report on COVID-19 and Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2021;203(1):24–36. doi:10.1164/rccm.202009-3533SO
2. Koch M, Butt T, Guo W, et al. Characteristics and health burden of the undiagnosed population at risk of chronic obstructive pulmonary disease in China. BMC Public Health. 2019;19(1):1727. doi:10.1186/s12889-019-8071-8
3. Hurst JR, Siddiqui MK, Singh B, et al. Review of the Humanistic Burden of COPD. COPD. 2021;16:1303–1314. doi:10.2147/COPD.S296696
4. Mathioudakis AG, Janssens W, Sivapalan P, et al. Acute exacerbations of chronic obstructive pulmonary disease: in search of diagnostic biomarkers and treatable traits. Thorax. 2020;75(6):520–527. doi:10.1136/thoraxjnl-2019-214484
5. Ko FW, Chan KP, Hui DS, et al. Acute exacerbation of COPD: hot topics on acute exacerbation of COPD. Respirology. 2016;21(7):1152–1165. doi:10.1111/resp.12780
6. Mantero M, Rogliani P, Di Pasquale M, et al. Acute exacerbations of COPD: risk factors for failure and relapse. COPD. 2017;12:2687–2693. doi:10.2147/COPD.S145253
7. Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27. doi:10.1016/j.jaci.2016.05.011
8. Paone G, Leone V, Conti V, et al. Blood and sputum biomarkers in COPD and asthma: a review. Eur Rev Med Pharmacol Sci. 2016;20(4):698–708
9. Fermont JM, Masconi KL, Jensen MT, et al. Biomarkers and clinical outcomes in COPD: a systematic review and meta-analysis. Thorax. 2019;74(5):439–446. doi:10.1136/thoraxjnl-2018-211855
10. Celli BR, Anderson JA, Brook R, et al. Serum biomarkers and outcomes in patients with moderate COPD: a substudy of the randomised SUMMIT trial. BMJ Open Respiratory Research. 2019;6(1):e000431. doi:10.1136/bmjresp-2019-000431
11. de Torres JP, Pinto-Plata V, Casanova C, et al. C-Reactive Protein Levels and Survival in Patients With Moderate to Very Severe COPD. Chest. 2008;133(6):1336–1343. doi:10.1378/chest.07-2433
12. Antonescu-Turcu AL, Tomic R. C-reactive protein and copeptin: prognostic predictors in chronic obstructive pulmonary disease exacerbations. Curr Opin Pulm Med. 2009;15(2):120–125. doi:10.1097/MCP.0b013e3283218603
13. Moberg M, Vestbo J, Martinez G, Lange P, Ringbaek T. Prognostic Value of C-Reactive Protein, Leukocytes, and Vitamin D in Severe Chronic Obstructive Pulmonary Disease. Scientific World J. 2014;2014:1–7. doi:10.1155/2014/140736
14. Lv MY, Qiang LX, Li ZH, Jin SD. The lower the eosinophils, the stronger the inflammatory response? The relationship of different levels of eosinophils with the degree of inflammation in acute exacerbation chronic obstructive pulmonary disease (AECOPD). J Thorac Dis. 2021;13(1):232–243. doi:10.21037/jtd-20-2178
15. Acartürk Tunçay E, Karakurt Z, Aksoy E, et al. Eosinophilic and non-eosinophilic COPD patients with chronic respiratory failure: neutrophil-to-lymphocyte ratio as an exacerbation marker. COPD. 2017;12:3361–3370. doi:10.2147/COPD.S147261
16. Oh YM, Lee KS, Hong Y, et al. Blood eosinophil count as a prognostic biomarker in COPD. COPD. 2018;13:3589–3596. doi:10.2147/COPD.S179734
17. El-Gazzar AG, Kamel MH, Elbahnasy OKM, El-Naggar MES. Prognostic value of platelet and neutrophil to lymphocyte ratio in COPD patients. Expert Rev Respir Med. 2020;14(1):111–116. doi:10.1080/17476348.2019.1675517
18. Luo Z, Zhang W, Chen L, Xu N. Prognostic Value of Neutrophil:lymphocyte and Platelet:lymphocyte Ratios for 28-Day Mortality of Patients with AECOPD. IJGM. 2021;14:2839–2848. doi:10.2147/IJGM.S312045
19. Paliogiannis P, Fois AG, Sotgia S, et al. The neutrophil-to-lymphocyte ratio as a marker of chronic obstructive pulmonary disease and its exacerbations: a systematic review and meta-analysis. Eur J Clin Invest. 2018;48(8):e12984. doi:10.1111/eci.12984
20. Sørensen AK, Holmgaard DB, Mygind LH, Johansen J, Pedersen C. Neutrophil-to-lymphocyte ratio, calprotectin and YKL-40 in patients with chronic obstructive pulmonary disease: correlations and 5-year mortality – a cohort study. J Inflamm. 2015;12(1):20. doi:10.1186/s12950-015-0064-5
21. Günay E, Sarınç Ulaşlı S, Akar O, et al. Neutrophil-to-Lymphocyte Ratio in Chronic Obstructive Pulmonary Disease: a Retrospective Study. Inflammation. 2014;37(2):374–380. doi:10.1007/s10753-013-9749-1
22. Teng F, Ye H, Xue T. Predictive value of neutrophil to lymphocyte ratio in patients with acute exacerbation of chronic obstructive pulmonary disease. PLoS One. 2018;13(9):e0204377. doi:10.1371/journal.pone.0204377
23. Wang H, Lv C, Wang S, Ying H, Weng Y, Yu W. NLRP3 Inflammasome Involves in the Acute Exacerbation of Patients with Chronic Obstructive Pulmonary Disease. Inflammation. 2018;41(4):1321–1333. doi:10.1007/s10753-018-0780-0
24. Pascual-González Y, López-Sánchez M, Dorca J, Santos S. Defining the role of neutrophil-to-lymphocyte ratio in COPD: a systematic literature review. COPD. 2018;13:3651–3662. doi:10.2147/COPD.S178068
25. Ye Z, Ai X, Liao Z, You C, Cheng Y. The prognostic values of neutrophil to lymphocyte ratio for outcomes in chronic obstructive pulmonary disease. Medicine. 2019;98(28):e16371. doi:10.1097/MD.0000000000016371
26. Ayala A, Herdon C, Lehman D, Ayala C, Chaudry I. Differential induction of apoptosis in lymphoid tissues during sepsis: variation in onset, frequency, and the nature of the mediators. Blood. 1996;87(10):4261–4275. doi:10.1182/blood.V87.10.4261.bloodjournal87104261
27. Lee HUm SJ, Kim YS, et al. Association of the Neutrophil-to-Lymphocyte Ratio with Lung Function and Exacerbations in Patients with Chronic Obstructive Pulmonary Disease. PLoS One. 2016;116: e0156511. doi:10.1371/journal.pone.0156511.
28. Rahimirad S, Reza M. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute exacerbation of chronic obstructive pulmonary disease. Am J Cardiol. 2008;102(6):653
29. Pascoe S, Barnes N, Brusselle G, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med. 2019;7(9):745–756. doi:10.1016/S2213-2600(19)30190-0
30. Pavord ID, Lettis S, Anzueto A, Barnes N. Blood eosinophil count and pneumonia risk in patients with chronic obstructive pulmonary disease: a patient-level meta-analysis. Lancet Respir Med. 2016;4(9):731–741. doi:10.1016/S2213-2600(16)30148-5
31. Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med. 2015;3(6):435–442. doi:10.1016/S2213-2600(15)00106-X
32. Mendy A, Forno E, Niyonsenga T, Gasana J. Blood biomarkers as predictors of long-term mortality in COPD. Clin Respir J. 2018;12(5):1891–1899. doi:10.1111/crj.12752
33. Moy ML, Teylan M, Danilack VA, Gagnon DR, Garshick E. An Index of Daily Step Count and Systemic Inflammation Predicts Clinical Outcomes in Chronic Obstructive Pulmonary Disease. Annals ATS. 2014;11(2):149–157. doi:10.1513/AnnalsATS.201307-243OC
34. Duman D, Aksoy E, Coban Agca M, et al. The utility of inflammatory markers to predict readmissions and mortality in COPD cases with or without eosinophilia. COPD. 2015:2469. doi:10.2147/COPD.S90330
35. Vedel-Krogh S, Nielsen SF, Lange P, Vestbo J, Nordestgaard BG. Blood Eosinophils and Exacerbations in Chronic Obstructive Pulmonary Disease. The Copenhagen General Population Study. Am J Respir Crit Care Med. 2016;193(9):965–974. doi:10.1164/rccm.201509-1869OC
36. Celli BR, Fabbri LM, Aaron SD, et al. An Updated Definition and Severity Classification of Chronic Obstructive Pulmonary Disease Exacerbations: the Rome Proposal. Am J Respir Crit Care Med. 2021;204(11):1251–1258. doi:10.1164/rccm.202108-1819PP
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.