Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Prognostic Role of Serum Soluble Tim-3 in Severe Traumatic Brain Injury: A Prospective Observational Study
Authors Zhang H, Lv QW, Zheng ZQ, Shen LJ, Zhou J, Guo M
Received 9 November 2022
Accepted for publication 7 January 2023
Published 18 January 2023 Volume 2023:19 Pages 153—169
DOI https://doi.org/10.2147/NDT.S396771
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Han Zhang, Qing-Wei Lv, Zi-Qiang Zheng, Liang-Jun Shen, Jing Zhou, Mi Guo
Department of Neurosurgery, Shengzhou People’s Hospital (the First Affiliated Hospital of Zhejiang University Shengzhou Branch), Shengzhou, People’s Republic of China
Correspondence: Mi Guo, Department of Neurosurgery, Shengzhou People’s Hospital (the First Affiliated Hospital of Zhejiang University Shengzhou branch), Shengzhou, People’s Republic of China, Tel +86 575 3032041, Email [email protected]
Objective: T cell immunoglobulin and mucin domain-3 (Tim-3) may be implicated in neuroinflammation. Herein, we attempted to discern the role of serum soluble (s) Tim-3 as an inflammatory prognostic biomarker of severe traumatic brain injury (sTBI).
Methods: In this prospective observational study of 112 sTBI patients and 112 controls, serum sTim-3 levels were determined, Rotterdam computed tomography (CT) classification and Glasgow coma scale (GCS) were selected as the two severity indicators, serum C-reactive protein (CRP) was regarded as an inflammatory biomarker, and poor prognosis was referred to as extended Glasgow outcome scale (GOSE) scores 1– 4 at 180 days after trauma.
Results: Serum sTim-3 levels were markedly higher in patients than in controls (median, 4.2 ng/mL versus 0.7 ng/mL; P< 0.001). Serum sTim-3 levels of patients were independently related to Rotterdam CT scores (β=1.126), GCS scores (β=− 0.589), serum CRP levels (β=0.155) and GOSE scores (β=− 0.211). Serum sTim-3 appeared as an independent predictor of post-traumatic 180-day mortality (odds ratio=1.289), overall survival (hazard ratio=1.208) and poor prognosis (odds ratio=1.293). Serum sTim-3 levels discriminated patients at risk of post-injury 180-day mortality and poor prognosis with areas under curve (AUCs) at 0.753 and 0.782, respectively. Serum sTim-3 levels combined with GCS scores and Rotterdam CT scores (AUC=0.869) exhibited significantly higher AUC than Rotterdam CT scores (P=0.026), but not than GCS scores (P=0.181) for death prediction and their combination (AUC=0.895) had significantly higher AUC than GCS scores (P=0.036) or Rotterdam CT scores (P=0.005) for outcome prediction.
Conclusion: Elevated serum sTim-3 levels, in close correlation with traumatic severity and inflammation, are substantially associated with long-term death and poor outcome, indicating that serum sTim-3, as an inflammatory biomarker, may be of clinical significance in severity assessment and prediction of prognosis following sTBI.
Keywords: traumatic brain injury, biomarkers, T cell immunoglobulin and mucin domain-3, severity, prognosis, death, inflammation
Introduction
Severe traumatic brain injury (sTBI) is a fatal form of trauma characterized by high mortality and poor outcome.1 sTBI-related pathophysiological mechanisms are rather complex, where neuroinflammation with involvement of some specific inflammatory cells and mediators plays a crucial role.2 Prognostic prediction emerges as a foremost issue to be followed during sTBI management.3 Generally, the Glasgow coma scale (GCS) and Rotterdam computed tomography (CT) scale are in very frequent use for evaluating sTBI severity and predicting clinical outcome.4 Extended Glasgow outcome scale (GOSE) is very often selected to estimate neurological function of sTBI patients.5 In past decades, various mediators and proteins, such as periostin, glial fibrillary acidic protein, ubiquitin C-terminal hydrolase L1, and microtubule-associated protein-2, have been identified as predictors of recovery after brain injuries and been extensively studied to aid in making prognostic predictions of sTBI.6–9
T-cell immunoglobulin and mucin domain protein −3 (Tim-3) is initially revealed to be expressed in activated Th1 cells and harbors an immuno-regulation potential.10 Compelling data have shown that Tim-3 is implicated in adaptive and innate immune responses, thereby participating in several inflammatory diseases, including systemic lupus erythematosus, viral hepatitis infection and acute pancreatitis.11–13 Gradually, Tim-3 is found to be chiefly expressed by microglia and neurons in central nervous system.14,15 In experimental models with acute brain injury, such as subarachnoid hemorrhage and intracerebral hemorrhage, Tim-3 could aggravate neuroinflammation and subsequently increase neuronal apoptosis, wherein neurologic function was impaired.16–18 Intriguingly, there was a significant elevation of Tim-3 expression on CD4(+) T cells and monocytes in humans with ischemic stroke, which were intimately and positively related to systemic interleukin-17 and tumor necrosis factor-alpha levels.19 Using flow cytometry, Tim-3 expression on peripheral cells were highly correlated with systemic inflammation response, illness severity and clinical outcome of human intracerebral hemorrhage.20,21 Hypothetically, soluble (s) Tim-3 may have the potential to serve as a proinflammatory biomarker of prognosis after acute brain injury. However, there is a paucity of data available with respect to circulating levels of sTim-3 in the peripheral blood of patients with acute brain injury. Herein, a cohort of sTBI patients were enrolled to verify the prognostic significance of serum sTim-3.
Materials and Methods
Study Design and Ethical Considerations
We undertook a prospective cohort study at the Shengzhou People’s Hospital and consecutively enrolled healthy controls and patients with head trauma. This study was done in compliance with the ethical guidelines of the Declaration of Helsinki and the protocol of the current study was approved by the Institutional Review Committee at the Shengzhou People’s Hospital (SZ2017021). The informed consent to participate in this study was signed by patients’ relatives or controls themselves.
Patient and Control Selection
From May 2017 to July 2020 at our hospital, we consecutively enrolled blunt head trauma adults (age of 18 years or greater) with admission GCS scores of 8 or less and injury severity score less than 9 in non-cranial aspects. Afterwards, we excluded those patients with admission time exceeding 12 hours following injury, history of neurological diseases (eg, ischemic or hemorrhagic stroke, intracranial tumors, myasthenia gravis and multiple sclerosis) or other specific conditions or diseases (eg, infections within recent a month, autoimmune diseases, use of immunosuppressants, pregnancies, severe hepatic, renal, pulmonary or cardiac diseases and malignancies).
Controls were consecutively recruited from physical examinees from July 2019 to July 2020 at our hospital. We required that all controls should be free of previous diseases, for instance hypertension, diabetes mellitus and atrial fibrillation; and be normal in some routine blood tests, for example blood glucose levels, blood leucocyte count, blood platelet count and blood albumin levels.
Demographic, Clinical and Radiological Data
Upon entry to the emergency room, some relevant information was inquired, including time from trauma to arrival at hospital, demographic data (age, gender and body mass index), comorbidities (hypertension, diabetes mellitus, hyperlipidemia and coronary heart diseases), some specific adverse life habits (cigarette smoking and alcohol drinking) and traumatic causes (automobile/motorcycle, fall/jump or others). Admission GCS score was registered as an indicator for assessing sTBI clinical severity. Initial vital signs were recorded, including arterial blood pressure, body temperature, respiratory rate, pulse rate and blood oxygen saturation. Head CT scan was performed by radiological personnel who was unavailable to clinical data. Via the first available CT images, we collected some radiologic parameters, such as abnormal cisterns, midline shift, epidural hematoma, subdural hematoma, subarachnoid hemorrhage, intraventricular hemorrhage, intracerebral hematoma, brain contusion and pneumocephalus. Also, Rotterdam CT scores were estimated to indicate sTBI radiologic severity.22
Outcome Assessment
All sTBI patients were followed up until death or the completion of 180 days after head trauma. 8-grade Extended Glasgow Outcome Scale (GOSE) was utilized to assess neurologic function of patients. Patients with GOSE scores of 1–4 were considered to have poor prognosis and those with scores 5–8 were regarded as good prognosis.23 The prognosis parameters included death and poor prognosis at 180 days after sTBI.
Immune Analysis
Blood samples of patients were acquired at entrance into emergency center and those of controls were obtained at entry into study. After blood was centrifugated, serum samples were promptly stored at −80°C until further quantification. Using a commercially available Enzyme-Linked Immunosorbent Assay kit (Thermo Fisher Scientific Waltham, MA, USA), Serum sTim-3 levels were gauged by the same technician, who was inaccessible to clinical information. Every 3 months, a batch of samples were determined. Each sample was in duplicate measured and the mean value of two measurements were registered for final analysis.
Statistical Analysis
The SPSS 20.0 statistical package (SPSS Inc., Chicago, Illinois, USA) and MedCalc statistical software version 17.4 (MedCalc Software, Mariakerke, Belgium) were the two statistical softwares, which were used for statistical analysis in this study. Qualitative variables, which were reported as counts (percentages), were compared between patients and controls, between survivors and non-survivors, as well as between poor prognosis patients and those with good prognosis using the Pearson’s Chi-square test or Fisher’s exact test as appropriate. Normally distributed quantitative variables, which were summarized as means (standard deviations, SDs), were compared between two groups using the independent t-test. Non-normally distributed quantitative variables, which were shown as medians (percentages 25th-75th), were compared between two groups using the Mann–Whitney test. Using the Kruskal–Wallis H-test, comparison of serum sTim-3 levels among multiple groups was done in accordance with GCS scores, Rotterdam CT scores and GOSE scores. Bivariate correlations between serum sTim-3 levels and other variables, as well as between GOSE scores and other variables, were investigated using the Spearman test. Serum sTim-3 levels were dichotomized in accordance with its median value and subsequently comparison of 180-day overall survival time was done between two groups using the Log rank test. Using the precedingly described univariate analysis, we determined the variables, which were substantially correlated with serum sTim-3 levels and GOSE scores, as well as were markedly associated with 180-day death, poor prognosis and overall survival. And afterwards, such significant variables were incorporated into the multivariate linear regression model, binary logistic regression model or multivariate Cox’s proportional hazard where appropriate. Correlations were shown as β (95% confidence interval, 95% CI) and associations were reported as odds ratio (OR) (95% CI) or Hazard ratio (HR) (95% CI) as appropriate. Under receiver operating characteristic (ROC) curve, predictive efficiency was presented as area under ROC curve (AUC) (95% CI). Using the Youden method, the optimal value of serum sTim-3 levels was selected, thereby yielding the corresponding sensitivity and specificity values. The combined logistic regression model was constructed, and thereafter its predictive ability was assessed using Z test under ROC curve. Differences with P-values < 0.05 were regarded as statistical significance.
Results
Participant Selection and Characteristics
At the start, a total of 153 adult patients with blunt, isolated sTBI were consecutively enrolled for an initial assessment in compliance with the preseted inclusion criteria; thereafter, 41 patients were excluded from the current study in agreement with the exclusion criteria, and ultimately 112 patients were under epidemiological investigation (Figure 1). Alternatively, a group of healthy individuals were chosen as controls.
Patients with sTBI comprised of 64 males and 48 females, there were 37 alcohol drinkers and 36 cigarette smokers, their age ranged from 18 to 81 years (mean, 43.1 years; SD, 18.5 years), and body mass index ranged from 18.2 to 33.5 kg/m2 (mean, 24.6 kg/m2; SD, 3.4 kg/m2). Controls were composed of 57 males and 55 females, there were 38 alcohol drinkers and 40 cigarette smokers, their age ranged from 18 to 77 years (mean, 44.3 years; SD, 13.7 years), and body mass index ranged from 18.4 to 34.8 kg/m2 (mean, 24.8 kg/m2; SD, 4.2 kg/m2). Gender, smoker and drinker percentages, as well as mean age and body mass index insignificantly differed between controls and patients (all P>0.05).
This group of sTBI patients, among whom there were 20 hypertensive cases, 15 individuals with diabetes mellitus, 19 subjects inflicted with hyperlipidemia and 16 patients coexisting with coronary heart diseases, were admitted from 0.3 to 11.8 hours following trauma (median, 4.5 hours; percentiles 25th – 75th, 2.0–7.0 hours) and had blood samples collected from 0.7 to 14.3 hours (median, 6.0 hours; percentiles 25th – 75th, 3.2–8.5 hours) after injury. A large portion of head traumas resulted from automobile/motorcycle (52 cases) and fall/jump (50 cases) and the other 9 cases were traumatized by other causes. As regards clinical and radiological severity, GCS score ranged from 3 to 8 (median, 5; percentiles 25th – 75th, 4–6) and Rotterdam CT score ranged from 3 to 6 (median, 4; percentiles 25th – 75th, 4–5). The mean systolic and diastolic arterial pressures ranged from 71 to 180 mmHg (mean, 127.6 mmHg; SD, 26.5 mmHg) and from 36 to 108 mmHg (mean, 76.9 mmHg; SD, 17.4 mmHg), respectively. The registered trauma-related positive radiological appearances in the current study included epidural hematoma (54 cases), subdural hematoma (62 cases), subarachnoid hemorrhage (73 cases), intraventricular hemorrhage (14 cases), intracerebral hematoma (60 cases), brain contusion (63 cases), pneumocephalus (45 cases), abnormal cisterns (80 cases) and midline shift > 5 mm (65 cases).
Serum sTim-3 Levels and Trauma Severity
Patients, in comparison to controls, had substantially raised serum sTim-3 levels (P<0.001; Figure 2). Among those patients, serum sTim-3 levels were strongly correlated with serum C-reactive protein (CRP) levels (P <0.001; Figure 3A), GCS scores (P <0.001; Figure 3B), Rotterdam CT scores (P <0.001; Figure 3C) and other variables listed in Table 1 (ie, current cigarette smoking, epidural hematoma, abnormal cisterns, midline shift above 5 mm, blood glucose levels and blood leucocyte count; all P <0.05). Using multivariate linear regression model, which contained the preceding significantly correlated variables, serum CRP levels, GCS scores and Rotterdam CT scores remained to be independently related to serum sTim-3 levels after sTBI (all P<0.05; Figure 4A). Furthermore, both GCS and Rotterdam CT classification were considered as the two qualitative variables. GCS scores 3, 4, 5, 6, 7 and 8 were displayed in 14, 25, 32, 17, 10 and 14 patients, respectively. Rotterdam CT scores 3, 4, 5 and 6 were exhibited in 13, 54, 26 and 19 patients, respectively. In Figure 4B, serum sTim-3 levels were markedly highest in patients with GCS score 3, followed by scores 4, 5, 6 and 7, and were substantially lowest in those with score 8 (P<0.001). Also, there were pronouncedly lowest serum sTim-3 levels in patients with Rotterdam CT score 3, followed by scores 4 and 5, and significantly highest levels in those with Rotterdam CT score 6 (P<0.001, Figure 4C).
 |
Table 1 Factors in Correlation with Serum Soluble T Cell Immunoglobulin and Mucin Domain-3 Levels After Severe Traumatic Brain Injury |
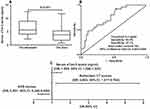
Serum sTim-3 Levels and Post-Traumatic 180-Day Death
Among this cohort of sTBI patients, twenty-five cases (25/112, 22.3%) were deceased within 180 days after trauma. In Figure 5A, there was a significant elevation of serum sTim-3 levels after sTBI in non-survivors, as compared to survivors (P<0.001). Under ROC curve, serum sTim-3 levels substantially discriminated 180-day death and a cutoff value of serum sTim-3 levels was identified using Youden method (Figure 5B). Additionally, its predictive ability was in range of GCS scores (AUC, 0.832; 95% CI, 0.760–0.905; P=0.090) and Rotterdam CT scores (AUC, 0.818; 95% CI, 0.728–0.909; P=0.243). However, serum sTim-3 levels numerically improved AUCs of GCS scores and Rotterdam CT scores to 0.842 (95% CI, 0.765–0.919; P=0.513) and 0.839 (95% CI, 0.757–0.921; P=0.245). Intriguingly, serum sTim-3 levels combined with GCS scores and Rotterdam CT scores (AUC, 0.869; 95% CI, 0.800–0.939) exhibited significantly higher AUC than Rotterdam CT scores (P=0.026), but not than GCS scores (P=0.181).
The dead were substantially older than the alive; GCS scores were significantly decreased and Rotterdam CT scores were markedly elevated in non-survivors, as compared to survivors; non-surviving patients, in comparison to other remainders, had pronouncedly higher percentages of abnormal cisterns and midline shift above 5 mm; as well as serum CRP levels, blood leucocyte count, serum sTim-3 levels and blood glucose levels were profoundly higher in non-surviving patients than in surviving ones (all P<0.05, Table 2). The above-mentioned variables were incorporated into the binary logistic regression model and subsequently GCS scores, Rotterdam CT scores and serum sTim-3 levels were still independently associated with 180-day death (all P<0.05, Figure 5C).
 |
Table 2 Factors in Association with 180-Day Mortality After Severe Traumatic Brain Injury |
The mean 180-day overall survival time was 147.8 days (95% CI, 136.0–159.6 days) in sTBI patients. Serum sTim-3 levels was dichotomized in view of the median value (namely, 4.2 ng/mL). In Figure 6A, 180-day overall survival time was significantly shorter in patients with serum sTim-3 levels > 4.2 ng/mL than in those with serum sTim-3 levels < 4.2 ng/mL (P<0.05). In addition, using univariate Cox’s proportional hazard analysis, hypertension, GCS scores, Rotterdam CT scores, abnormal cisterns, midline shift more than 5 mm, blood CRP levels, blood leucocyte count, blood glucose levels and serum sTim-3 levels were significantly associated with 180-day overall survival time (all P<0.05; Table 3). Afterwards, the preceding variables were entered in the multivariate model and thereafter, it was verified that GCS score, Rotterdam CT score and serum sTim-3 levels retained to be independently related to 180-day overall survival following trauma (all P<0.05, Figure 6B).
 |
Table 3 Factors Associated with 180-Day Overall Survival After Severe Traumatic Brain Injury |
Serum sTim-3 Levels and 180-Day Neurologic Functional Outcome Following Trauma
Among sTBI patients, 180-day GOSE scores 1, 2, 3, 4, 5, 6, 7 and 8 were found in 25, 10, 5, 11, 21, 19, 11 and 10 patients, respectively. In Figure 7A, serum sTim-3 levels were significantly highest in patients with GOSE score 1, followed by GOSE scores 2, 3, 4, 5, 6 and 7, and were markedly lowest in those with GOSE score 8 (P<0.001). Alternatively, GOSE scores ranged from 1 to 8, with a median value of 5 (lower-upper quartiles, 2–6). GOSE scores were highly correlated with serum sTim-3 levels (P<0.001; Figure 7B), hypertension, diabetes mellitus, GCS scores, Rotterdam CT scores, epidural hematoma, subdural hematoma, abnormal cisterns, midline shift more than 5 mm, serum CRP levels and blood glucose levels (all P<0.05; Table 4). Using multivariate analysis, the preceding variables were forced into the model and it was shown that GCS scores, Rotterdam CT scores and serum sTim-3 levels were independently correlated with 180-day GOSE scores after head trauma (all P<0.05; Figure 7C).
 |
Table 4 Factors in Relation to Extended Glasgow Outcome Scale Scores at 180 Days After Severe Traumatic Brain Injury |
In total, 51 patients (45.5%) experienced a poor outcome (GOSE scores 1–4) at 180 days after head trauma. In Figure 8A, serum sTim-3 levels were significantly higher in patients with a poor outcome than in those with a good outcome (P<0.001). Moreover, serum sTim-3 levels distinguished the risk of a poor outcome significantly (Figure 8B). Also, its prognostic predictive performance was equivalent to those of GCS scores (AUC, 0.844; 95% CI, 0.778–0.911; P=0.135) and Rotterdam CT scores (AUC, 0.838; 95% CI, 0.773–0.903; P=0.200). Prognostic predictive ability significantly differed between GCS scores and serum sTim-3 levels combined with GCS (AUC, 0.885; 95% CI, 0.826–0.945; P=0.049), as well as between Rotterdam CT scores and serum sTim-3 levels combined with Rotterdam CT scores (AUC, 0.886; 95% CI, 0.825–0.948; P=0.036). Serum sTim-3 levels combined with GCS scores and Rotterdam CT scores (AUC, 0.895; 95% CI, 0.838–0.952) had significantly higher AUC than GCS scores (P=0.036) or Rotterdam CT scores (P=0.005).
Just as listed in Table 5, patients with a poor outcome, in comparison to those with a good outcome, tended to have significantly rising percentages of hypertension, diabetes mellitus, epidural hematoma, subdural hematoma, subarachnoid hemorrhage, brain contusion, abnormal cisterns and midline shift above 5 mm, were prone to exhibit substantially declined GCS scores, and were likely to display substantially elevated Rotterdam CT scores, blood glucose levels, serum CRP levels and serum sTim-3 levels (all P<0.05). Furthermore, we configured the binary logistic regression model, where the preceding factors were contained, and thereafter found that GCS scores, Rotterdam CT scores and serum sTim-3 levels independently predicted a poor outcome at 180 days after head trauma (all P<0.05, Figure 8C).
 |
Table 5 Factors Related to 180-Day Poor Outcome After Severe Traumatic Brain Injury |
Discussion
To the best of our knowledge, this is the first clinical epidemiological investigation for measuring circulating sTim-3 levels of humans with acute brain injury and further exploring the relationship between serum sTim-3 levels and sTBI severity in addition to neurologic functional outcome following sTBI. Intriguingly, we revealed several noteworthy results as follows. (1) there was a significant elevation of serum sTim-3 levels in humans after sTBI, as compared to healthy controls; (2) serum sTim-3 levels were closely correlated with GCS scores and Rotterdam CT scores, both of which were whether identified as the categorical or continuous variable; (3) serum sTim-3 levels were independently correlated with serum CRP levels; (4) serum sTim-3 emerged as an independent biochemical predictor of 180-day death and overall survival; (5) serum sTim-3 levels were intimately related to GOSE scores, which was whether identified as the quantitative or qualitative variable; (6) serum sTim-3 appeared as a biomarker for independently predicting a poor outcome at 180 days after sTBI; and (7) Under ROC curve, serum sTim-3 levels were significantly in possession of high prognostic predictive efficiency. It is deduced that serum sTim-3 levels, which were substantially elevated after sTBI, may be highly in relation to trauma severity and be strongly associated with long-term death and functional outcome after sTBI, assuming that serum sTim-3 should be apt to serve as a potential biochemical marker for aiding in severity assessment and prognosis prediction of sTBI.
The TBI pathophysiological processes are rather complicated and multifactorial, which are conventionally divided into primary and secondary brain injuries.24 Primary brain injury is caused by mechanical disruption of brain tissues; and secondary brain injury involves excitotoxicity, hypoxia, ischemia, apoptosis, necrosis, oxidative reaction and inflammation.25 Neuroinflammation is a very important mechanism in the secondary brain injury following TBI, which can disrupt the blood–brain barrier, damage neuron, and aggravate brain edema, thereby inducing neurologic functional impairments.26 Thus, inflammation-related researches have attracted interests of experts in neuroscientific field.
Tim-3 has two forms, ie, the full-length form and a soluble form (sTim-3).27 Tim-3 mRNA could be spliced to produce two mRNA molecules, namely full-length Tim-3 and short-length Tim-3 (sTim-3), which should be a splice variant of the full-length form Tim-3 without the region encoding the mucin domain and transmembrane domain.27 In our study, an obvious enhancement was found of serum sTim-3 levels after sTBI, as compared to healthy controls. Nevertheless, studies with respect to sTim-3 in central nervous system remain scarce and it is unclear which cell type is responsible for the elevation of circulating sTim-3 levels. Full-length Tim-3 expression by CD4(+) T cells and monocytes was significantly elevated after human ischemic stroke,19 and full-length Tim-3 expression on CD14+ monocytes was substantially up-regulated in humans with intracerebral hemorrhage.20 Full-length Tim-3 is also expressed on microglia and nerve cells in the brain and is greatly up-regulated after acute brain injury.14–18 sTim-3 was initially found to be derived from activated-splenic lymphocytes.27 Gradually, sTim-3 was revealed to be generated by ectodomain shedding of A Disintegrin And Metalloprotease-10 and-17 from full-length membrane-anchored Tim-3 on immune cells.28,29 Taken together, sTim-3 in the peripheral blood may originate from peripheral blood cells, but another possibility is not excluded that it may be derived from injured brain tissue after sTBI. Hence, Thus, it is significant to investigate the expression levels of sTim-3 mRNA in different cell types to determine origin of sTim-3 in the peripheral blood of sTBI patients.
Tim-3 harbors the potential in regulating the inflammatory reaction.30 Experimental evidence has shown that it might be involved in neuroinflammatory response after intracerebral hemorrhage and subarachnoid hemorrhage.16–18 Previous clinical studies of intracerebral hemorrhage and ischemic stroke demonstrated that elevated expression of Tim-3 in peripheral blood cells were highly correlated with circulating levels of some inflammatory reactive biomarkers, such as tumor necrosis factor-alpha, interleukin-1beta and interleukin-17, indicating that Tim-3 may participate in systemic inflammatory reaction after acute brain injury.19,20 However, contrary to Tim-3, sTim-3 could confer immunoinhibitory function.27 Recombinant mouse sTim-3 depressed T cell responses to antigen-specific stimulation.27 Alternatively, the immunoinhibitory role of sTim-3 was confirmed to be involved in the development of sepsis.31 In the current study, we found an independent relation of serum sTim-3 levels to serum CRP levels after head trauma. Although it is unclear regarding the exact role of sTim-3 in acute brain injury, it can be assumed that serum sTim-3 may have the potential to be an inflammatory biomarker after acute brain injury.
Tim-3 expression on peripheral cells was inversely correlated with disease severity and outcome of patients with intracerebral hemorrhage.21 Until now, there has been a paucity of data available with respect to circulating levels of sTim-3 after acute brain injury. Our study found some independent relationships between serum sTim-3 levels and traumatic severity assessed by GCS scores and Rotterdam CT scores, as well as between serum sTim-3 levels and clinical outcomes indicated by 180-day GOSE scores, mortality, overall survival and poor prognosis (GOSE scores of 1–4) in this cohort of sTBI patients. Of note, when combined with GCS scores and Rotterdam CT scores, serum sTim-3 displayed significantly high prognostic predictive efficiency because their combination substantially improved AUC of GCS scores and Rotterdam CT scores, especially in prediction of poor prognosis at 180 days after sTBI. In summary, serum sTim-3 may have the potential to serve as a prognostic biochemical marker of sTBI.
There are several weaknesses in this study. First, this is a single-center study, characterized by a small sample size, and therefore, a larger multi-center cohort study is needed to validate the conclusions. Second, blood was collected in a single time-point in this study, and possibly, some relevant information would be lost. Hence, dynamic change of serum sTim-3 levels after head trauma should be explored in future. Last, some other rare complications, such as epileptic seizure, pneumonia, and acute heart injury, were not recorded in the current study. Such clinical information is collected for prognosis analysis and subsequently it may be of clinical significance for increasing study power.
Conclusions
To the best of our knowledge, this is a first clinical epidemiological investigation for finding the following interesting results: (1) serum sTim-3 levels are independently related to systemic inflammation indicated by serum CRP levels, traumatic severity assessed by GCS scores and Rotterdam CT scores, and long-term clinical outcomes reflected by 180-day GOSE scores, mortality, overall survival and poor prognosis (GOSE scores of 1–4); and (2) serum sTim-3 levels combined with GCS scores and Rotterdam CT scores has obviously higher prognostic ability. Overall, our pilot study offers clinical evidence, which are supportive of the hypothesis that serum sTim-3, as an inflammatory biomarker, may be in possession of clinically valuable prognostic role in sTBI.
Abbreviations
CT, computerized tomography; GCS, Glasgow coma scale; ROC, receiver operating characteristic; sTBI, severe traumatic brain injury; ROC, receiver operating characteristic; AUC, area under curve; OR, odds ratio; HR, hazard ratio; 95% CI, 95% confidence interval; Tim-3, T cell immunoglobulin and mucin domain-3; GOSE, extended Glasgow Outcome Scale.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Ethics Statement
This study was carried out in compliance with the tenets of the Declaration of Helsinki and the protocol conformed to the ethical standards of the Shengzhou People’s Hospital on human subjects. The study protocol was approved by the Human Investigations Committee at the Shengzhou People’s Hospital (SZ2017021). We acquired written informed consent to participate in the current study from legal representatives of patients or controls themselves.
Acknowledgments
The authors thank all participants for their willingness to participate in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Stocchetti N, Carbonara M, Citerio G, et al. Severe traumatic brain injury: targeted management in the intensive care unit. Lancet Neurol. 2017;16(6):452–464. doi:10.1016/S1474-4422(17)30118-7
2. Capizzi A, Woo J, Verduzco-Gutierrez M. Traumatic brain injury: an overview of epidemiology, pathophysiology, and medical management. Med Clin North Am. 2020;104(2):213–238. doi:10.1016/j.mcna.2019.11.001
3. Wang KK, Yang Z, Zhu T, et al. An update on diagnostic and prognostic biomarkers for traumatic brain injury. Expert Rev Mol Diagn. 2018;18(2):165–180. doi:10.1080/14737159.2018.1428089
4. Pavlovic D, Pekic S, Stojanovic M, Popovic V. Traumatic brain injury: neuropathological, neurocognitive and neurobehavioral sequelae. Pituitary. 2019;22(3):270–282. doi:10.1007/s11102-019-00957-9
5. Bergmans SF, Schober P, Schwarte LA, Loer SA, Bossers SM. Prehospital fluid administration in patients with severe traumatic brain injury: a systematic review and meta-analysis. Injury. 2020;51(11):2356–2367. doi:10.1016/j.injury.2020.08.030
6. Dong XQ, Yu WH, Du Q, et al. Serum periostin concentrations and outcomes after severe traumatic brain injury. Clin Chim Acta. 2017;471:298–303. doi:10.1016/j.cca.2017.06.020
7. Anderson TN, Hwang J, Munar M, et al. Blood-based biomarkers for prediction of intracranial hemorrhage and outcome in patients with moderate or severe traumatic brain injury. J Trauma Acute Care Surg. 2020;89(1):80–86. doi:10.1097/TA.0000000000002706
8. Lorente L, Martín MM, Pérez-Cejas A, et al. Traumatic brain injury patients mortality and serum total antioxidant capacity. Brain Sci. 2020;10(2):110. doi:10.3390/brainsci10020110
9. Driga MP, Catalin B, Olaru DG, et al. The need for new biomarkers to assist with stroke prevention and prediction of post-stroke therapy based on plasma-derived extracellular vesicles. Biomedicines. 2021;9(9):1226. doi:10.3390/biomedicines9091226
10. Zhao L, Cheng S, Fan L, Zhang B, Xu S. TIM-3 An update on immunotherapy. Int Immunopharmacol. 2021;99:107933. doi:10.1016/j.intimp.2021.107933
11. Jin L, Bai R, Zhou J, et al. Association of serum T cell immunoglobulin domain and Mucin-3 and interleukin-17 with systemic lupus erythematosus. Med Sci Monit Basic Res. 2018;24:168–176. doi:10.12659/MSMBR.910949
12. Osuch S, Laskus T, Berak H, et al. Decrease of T-cells exhaustion markers programmed cell death-1 and T-cell immunoglobulin and mucin domain-containing protein 3 and plasma IL-10 levels after successful treatment of chronic hepatitis C. Sci Rep. 2020;10(1):16060. doi:10.1038/s41598-020-73137-6
13. Lin M, Huang J, Huang J, Liu SL, Chen WC. Level of serum soluble Tim-3 expression in early-phase acute pancreatitis. Turk J Gastroenterol. 2019;30(2):188–191. doi:10.5152/tjg.2018.18137
14. Wang HW, Zhu XL, Qin LM, Qian HJ, Wang Y. Microglia activity modulated by T cell Ig and mucin domain protein 3 (Tim-3). Cell Immunol. 2015;293(1):49–58. doi:10.1016/j.cellimm.2014.12.005
15. Wu B, Huang B, Chen Y, et al. Upregulated expression of Tim-3 involved in the process of toxoplasmic encephalitis in mouse model. Parasitol Res. 2013;112(7):2511–2521. doi:10.1007/s00436-013-3416-1
16. Guo S, Li Y, Wei B, et al. Tim-3 deteriorates neuroinflammatory and neurocyte apoptosis after subarachnoid hemorrhage through the Nrf2/HMGB1 signaling pathway in rats. Aging. 2020;12(21):21161–21185. doi:10.18632/aging.103796
17. Xu C, Wang T, Cheng S, Liu Y. Increased expression of T cell immunoglobulin and mucin domain 3 aggravates brain inflammation via regulation of the function of microglia/macrophages after intracerebral hemorrhage in mice. J Neuroinflammation. 2013;10:141. doi:10.1186/1742-2094-10-141
18. Zhang T, Yang Z, Li M. Tim-3 enhances brain inflammation by promoting M1 macrophage polarization following intracerebral hemorrhage in mice. Int Immunopharmacol. 2017;53:143–148. doi:10.1016/j.intimp.2017.10.023
19. Zhao D, Hou N, Cui M, et al. Increased T cell immunoglobulin and mucin domain 3 positively correlate with systemic IL-17 and TNF-α level in the acute phase of ischemic stroke. J Clin Immunol. 2011;31(4):719–727. doi:10.1007/s10875-011-9534-6
20. Xu C, Ge H, Wang T, Qin J, Liu D, Liu Y. Increased expression of T cell immunoglobulin and Mucin Domain 3 on CD14+ monocytes is associated with systemic inflammatory reaction and brain injury in patients with spontaneous intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2018;27(5):1226–1236. doi:10.1016/j.jstrokecerebrovasdis.2017.11.041
21. Liu X, You J, Zhao D, et al. Dysregulated expression of T cell immunoglobulin and mucin domain 3 is associated with the disease severity and the outcome of patients with spontaneous intracerebral hemorrhage. Clin Biochem. 2013;46(15):1502–1508. doi:10.1016/j.clinbiochem.2013.04.030
22. Huang YH, Deng YH, Lee TC, Chen WF. Rotterdam computed tomography score as a prognosticator in head-injured patients undergoing decompressive craniectomy. Neurosurgery. 2012;71(1):80–85. doi:10.1227/NEU.0b013e3182517aa1
23. Bossers SM, van der Naalt J, Jacobs B, Schwarte LA, Verheul R, Schober P. Face-to-face versus telephonic extended Glasgow outcome score testing after Traumatic brain injury. J Head Trauma Rehabil. 2021;36(3):E134–E138. doi:10.1097/HTR.0000000000000622
24. Jha RM, Kochanek PM, Simard JM. Pathophysiology and treatment of cerebral edema in traumatic brain injury. Neuropharmacology. 2019;145:230–246. doi:10.1016/j.neuropharm.2018.08.004
25. Dixon KJ. Pathophysiology of traumatic brain injury. Phys Med Rehabil Clin N Am. 2017;28(2):215–225. doi:10.1016/j.pmr.2016.12.001
26. Karve IP, Taylor JM, Crack PJ. The contribution of astrocytes and microglia to traumatic brain injury. Br J Pharmacol. 2016;173(4):692–702. doi:10.1111/bph.13125
27. Geng H, Zhang GM, Li D, et al. Soluble form of T cell Ig mucin 3 is an inhibitory molecule in T cell-mediated immune response. J Immunol. 2006;176(3):1411–1420. doi:10.4049/jimmunol.176.3.1411
28. Möller-Hackbarth K, Dewitz C, Schweigert O, et al. A disintegrin and metalloprotease (ADAM) 10 and ADAM17 are major sheddases of T cell immunoglobulin and mucin domain 3 (Tim-3). J Biol Chem. 2013;288(48):34529–34544. doi:10.1074/jbc.M113.488478
29. Clayton KL, Douglas-Vail MB, Nur-ur Rahman AK, et al. Soluble T cell immunoglobulin mucin domain 3 is shed from CD8+ T cells by the sheddase ADAM10, is increased in plasma during untreated HIV infection, and correlates with HIV disease progression. J Virol. 2015;89(7):3723–3736. doi:10.1128/JVI.00006-15
30. Tang R, Rangachari M, Kuchroo VK. Tim-3: a co-receptor with diverse roles in T cell exhaustion and tolerance. Semin Immunol. 2019;42:101302. doi:10.1016/j.smim.2019.101302
31. Ren F, Li J, Jiang X, et al. Plasma soluble Tim-3 emerges as an inhibitor in sepsis: sepsis contrary to membrane Tim-3 on monocytes. Tissue Antigens. 2015;86(5):325–332. doi:10.1111/tan.12653
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.