Back to Journals » OncoTargets and Therapy » Volume 10
Prognostic and clinicopathological significance of ubiquitin-specific protease 22 overexpression in cancers: evidence from a meta-analysis
Received 12 April 2017
Accepted for publication 6 August 2017
Published 21 November 2017 Volume 2017:10 Pages 5533—5540
DOI https://doi.org/10.2147/OTT.S139458
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Geoffrey Pietersz
Ning Ao,1 Liang Wang,2 Yuqin Liu3
1Department of Pathology, Beijing Tiantan Hospital, Capital Medical University, 2Department of Pathology, Chinese PLA General Hospital, 3Department of Pathology, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences and Peking Union Medical College, Tsinghua University, Beijing, People’s Republic of China
Purpose: This meta-analysis study aimed to reveal the prognostic relevance of ubiquitin-specific protease 22 (USP22) expression in patients with cancers.
Methods: PubMed, Embase, and the Cochrane Library electronic databases were searched for relevant studies published up to April 2017. The prognostic value of USP22 expression was evaluated by hazard ratio with 95% confidence intervals (CIs). Relative risk (RR) with 95% CIs assessed the effects of USP22 expression on clinicopathological parameters. A total of 16 studies of 2,233 Chinese patients were included in the final meta-analysis.
Results: A significant association was found between USP22 overexpression and survival in patients with cancers. The pooled RR indicated that USP22 overexpression was related to histological grade, advanced tumor–node–metastasis stage, positive lymph node metastasis, and distant metastasis.
Conclusion: This meta-analysis demonstrated that USP22 could be a novel biomarker for predicting prognosis in patients with cancers in the Chinese population.
Keywords: ubiquitin-specific protease 22, cancer, survival, prognosis, meta-analysis
Introduction
Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. It has a high mortality rate,1 but the number of survivors has slightly increased because of improvements in treatment modalities and screening programs that identify the grade, stage, and size of the tumor in the last 10 years; however, these clinicopathological factors cannot fully predict individual outcomes.2,3 Therefore, to improve clinical care, it is imperative to explore effective biological prognostic markers.
Ubiquitin-specific protease 22 (USP22) is a subunit of the human SAGA transcriptional cofactor acetylation complex that functions to deubiquitinate histones H2B and H2A.4 USP22 was identified as one of the 11-gene “death-from-cancer” signatures that predict rapid disease recurrence, distant metastatic sites, and poor response to therapy across multiple solid tumors.5,6 Its expression correlates with a stem cell-like expression profile and appears to be driven by the BMI-1 oncogene. Previous studies showed that USP22 enhances cancer cell proliferation through interaction with Rb and p53.7–9 USP22 is recruited by the Myc oncoprotein or nuclear receptors and counteracts heterochromatin silencing, thereby transactivating specific target genes in cancer cells.10,11 USP22 activation markedly contributes to aberrant cell cycle control and anoikis resistance, and its aberrant expression is associated with cancer progression and poor prognosis.8,12,13
Many studies have evaluated the prognostic value of USP22 overexpression in patients with cancer; some other conflicting conclusions were arrived.14,15 Therefore, the impact of USP22 expression on cancer prognosis remains controversial. To better understand the relationship between cancer pathogenesis and USP22 overexpression, we performed a meta-analysis to evaluate the effects of USP22 on survival and clinicopathological parameters in patients with cancer.
Methods
Search strategy
A systematic literature search of the databases PubMed, Embase, and the Cochrane Library was performed to identify relevant English language studies published up to April 2017 using the following keywords: “USP22” AND “prognosis” OR “prognostic” OR “survival” OR “outcome” AND “cancer” OR “carcinoma” OR “neoplasm” OR “tumor” OR “malignant”. We also inspected the references listed in identified studies to find additional relevant studies. Eligible reports were identified independently by two investigators (NA and LW).
Inclusion criteria
Eligible studies had to meet the following inclusion criteria: 1) evaluating USP22 expression in human cancer tissues; 2) evaluating the association between USP22 expression and cancer prognosis; and 3) providing sufficient information to estimate hazard ratios (HRs) with 95% confidence intervals (CIs). The exclusion criteria were as follows: 1) reviews, case reports, letters, and conference abstracts and 2) overlapping data. A flow diagram of the study selection process is shown in Figure 1. Because immunohistochemistry (IHC) is the most common method used to detect USP22 expression in tumors, and as mRNA expression levels were analyzed by reverse transcription polymerase chain reaction in cancer tissues than in paired adjacent normal tissues,16–23 we did not include studies reporting relationship of USP22 mRNA expression and clinicopathological parameters of patients in our current meta-analysis.
  | Figure 1 PRISMA flow diagram of study selection. |
Data extraction
Data from eligible studies were extracted independently by two investigators (NA and LW). The following items were collected: first author’s name, year of publication, nationality, number of cases, cancer type, method of detection, cutoff value of USP22 positivity, HRs with corresponding 95% CIs for disease-free survival (DFS) and overall survival (OS) analyses, and clinicopathological parameters. Any disagreements were settled by a third investigator (NA).
Quality assessment
The quality of included studies was assessed by two independent investigators (NA and LW) on the basis of the Newcastle–Ottawa scale (NOS) 9-point scoring system.24 Studies with an NOS score of ≥6 were regarded as high quality.
Statistical analysis
HRs with their 95% CIs were used to evaluate the association between USP22 expression levels and survival. If available, we obtained the data directly from the article. Alternatively, we reviewed the data from Kaplan–Meier survival curves using the Engauge Digitizer version 4.1 software. All included HRs derived from univariable models. Then, we stratified the variables by clinicopathological parameters of patients shown to contribute to poor survival, including lymph invasion, M stage, tumor–node–metastasis (TNM) stage, and histodifferentiation. The impact of USP22 expression on clinicopathological parameters was assessed by relative risks (RRs) with their 95% CIs. Heterogeneity among the included studies was checked by the chi-squared Q test.25 If the studies were heterogeneous (P<0.10 or I2>50%), the random effects model was used; otherwise, the fixed effects model was used.26 A sensitivity analysis was carried out to evaluate whether any single study affected the pooled univariable HRs by sequentially discarding individual studies. Egger’s test and Begg’s funnel plots were applied to assess publication bias.27 All statistical analyses were performed using the R 3.2.0 meta-analysis software. P-values <0.05 were considered statistically significant.
Results
Study characteristics
A total of 86 studies were selected following an initial search, of which 16 eligible studies from 2011 to 2015 met the inclusion and exclusion criteria and were included in this meta-analysis. The articles from January 2016 to April 2017 do not meet the inclusion criteria that we mentioned. The main characteristics of the eligible studies are summarized in Table 1. All studies were performed exclusively in patients from China. Seven of the studies were of patients with digestive system cancers (colorectal cancer, hepatocellular cancer, esophageal cancer, gastric cancer, and pancreatic cancer),16,18,23,28–31 two of the studies were of patients with salivary carcinoma,20,22 and seven of the studies were of patients with other cancer types (oral squamous cell carcinoma, lung cancer, glioma cancer, breast cancer, epithelial ovarian cancer, and papillary thyroid carcinoma).17,19,21,32–35 IHC was the main method used to detect USP22 expression in these studies.
Meta-analysis results
USP22 expression and survival
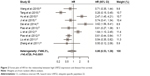
As shown in Figures 2 and 3, USP22 overexpression was significantly associated with poor DFS (HR =0.86, 95% CI: 0.53–1.38) and OS (HR =0.78, 95% CI: 0.37–1.64) in cancers. Owing to the heterogeneity detected in these studies, the random effects model was applied.
USP22 expression and clinicopathological parameters
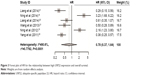
As shown in Figure 4 and Table 2, increased USP22 was significantly associated with histological grade (RR =0.72, 95% CI: 0.66–0.78, P=0.002), advanced TNM stage (RR =0.55, 95% CI: 0.49–0.61, P=0.000), positive lymph node metastasis (RR =0.69, 95% CI: 0.64–0.75, P=0.000), and positive distant metastasis (RR =0.66, 95% CI: 0.61–0.72, P=0.017) but not with gender (P=0.748). Owing to insufficient data, we did not detect a relationship between USP22 overexpression and other clinicopathological parameters.
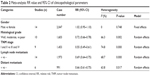  | Table 2 Meta-analysis: RR value and 95% CI of clinicopathological parameters |
Sensitivity analysis
Sensitivity analysis revealed no significant changes in HRs when any individual study was discarded (Figure 5). The investigation of the impact of USP22 overexpression on survival gave a Begg’s test score of P=0.533 and an Egger’s test score of P=0.368, reflecting no evidence of publication bias in the analysis.
  | Figure 5 Sensitivity analysis of survival. |
Discussion
The USP22 gene is located on human chromosome 17 and consists of 14 exons. Its 1,578 bp open reading frame encodes a 525 amino acid polypeptide with a molecular weight of ~66 kDa, containing a C-terminal peptidase domain of the C19 family and an N-terminal zinc finger motif that mediates the association between the enzyme and other proteins.8,12 USP22 was previously shown to be weakly expressed or absent in normal tissues but highly expressed in various cancers.36 Although the focus area of much USP22 research is digestive system cancers, the role of USP22 in other malignant tumors has received increasing attention in recent years. Several studies reported that USP22 could be considered as an important prognostic marker for malignant cancers.19,23,29,32,33,37,38 However, because only some reports correlated USP22 expression with prognosis, no pooled analysis has previously been performed. Our study conducted a pooled analysis of the prognostic value of USP22 expression relevant to 2,233 patients with cancers in China. Some independent prognostic factors are indicated via pooled analysis in general.
In the present meta-analysis, high USP22 expression was associated with worse survival in patients with cancer. Schrecengost et al39 previously showed that USP22 depletion dramatically downregulated androgen receptor protein levels and abolished androgen receptor activity in both androgen deprivation therapy and castration-resistant prostate adenocarcinoma cells. Xu et al7 speculated that the observed increase in USP22 activity in CRC might stabilize major vault protein by rescuing it from proteolysis and thus contributing to drug resistance. Therefore, the potential use of USP22 as a target for cancer therapy warrants further study.
We stratified the variables by clinicopathological parameters of patients shown to contribute to poor survival, including lymph invasion, M stage, TNM stage, and histodifferentiation. The random effects model was applied because of the significant heterogeneity observed for the association between evaluated USP22 expression and histological grade, TNM stage, and distant metastasis. Our meta-analysis has some limitations that should be acknowledged. First, most of the included studies focused on digestive system cancers and the small number of studies focusing on other cancer types might weaken our conclusions; thus, additional studies of different cancers could be included in a future meta-analysis. Second, all the included studies were of patients from China; hence, our conclusion might not be reliably extrapolated to non-Asian populations. Third, our extraction of data from Kaplan–Meier curves to derive HRs with 95% CIs might not have been reliable. Finally, although all studies detected USP22 expression by IHC, the use of different antibody concentrations and variable cutoff values might have influenced the results.
Conclusion
This meta-analysis indicated that USP22 overexpression was significantly associated with poor prognosis in cancer patients and that it could be used as a biomarker to predict clinical outcomes, especially in patients with cancers of the digestive system. Further clinical research is needed to support our conclusions and to confirm the precise prognostic value of USP22 in cancers.
Acknowledgment
The authors acknowledge the previous authors researched on USP22 and PubMed, Embase, and the Cochrane Library electronic databases.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Schneider G, Schmidt-Supprian M, Rad R, Saur D. Tissue-specific tumorigenesis: context matters. Nat Rev Cancer. 2017;17(4):239–253. | ||
Allard B, Longhi MS, Robson SC, Stagg J. The ectonucleotidases CD39 and CD73: novel checkpoint inhibitor targets. Immunol Rev. 2017;276(1):121–144. | ||
Andrews LP, Marciscano AE, Drake CG, Vignali DA. LAG3 (CD223) as a cancer immunotherapy target. Immunol Rev. 2017;276(1):80–96. | ||
Zhang XY, Pfeiffer HK, Thorne AW, McMahon SB. USP22, an hSAGA subunit and potential cancer stem cell marker, reverses the polycomb-catalyzed ubiquitylation of histone H2A. Cell Cycle. 2008;7(11): 1522–1524. | ||
Glinsky GV, Berezovska O, Glinskii AB. Microarray analysis identifies a death-from-cancer signature predicting therapy failure in patients with multiple types of cancer. J Clin Invest. 2005;115(6):1503–1521. | ||
Glinsky GV. Genomic models of metastatic cancer: functional analysis of death-from-cancer signature genes reveals aneuploid, anoikis- resistant, metastasis-enabling phenotype with altered cell cycle control and activated Polycomb Group (PcG) protein chromatin silencing pathway. Cell Cycle. 2006;5(11):1208–1216. | ||
Xu H, Liu YL, Yang YM, Dong XS. Knock-down of ubiquitin-specific protease 22 by micro-RNA interference inhibits colorectal cancer growth. Int J Colorectal Dis. 2012;27(1):21–30. | ||
Cao J, Yan Q. Histone ubiquitination and deubiquitination in transcription, DNA damage response, and cancer. Front Oncol. 2012;2:26. | ||
Ding F, Bao C, Tian Y, et al. USP22 promotes NSCLC tumorigenesis via MDMX up-regulation and subsequent p53 inhibition. Int J Mol Sci. 2014;16(1):307–320. | ||
Pijnappel WW, Timmers HT. Dubbing SAGA unveils new epigenetic crosstalk. Mol Cell. 2008;29(2):152–154. | ||
Zhao Y, Lang G, Ito S, et al. A TFTC/STAGA module mediates histone H2A and H2B deubiquitination, coactivates nuclear receptors, and counteracts heterochromatin silencing. Mol Cell. 2008;29(1):92–101. | ||
Cole AJ, Clifton-Bligh R, Marsh DJ. Histone H2B monoubiquitination: roles to play in human malignancy. Endocr Relat Cancer. 2015; 22(1):T19–T33. | ||
Zhang XY, Varthi M, Sykes SM, et al. The putative cancer stem cell marker USP22 is a subunit of the human SAGA complex required for activated transcription and cell-cycle progression. Mol Cell. 2008; 29(1):102–111. | ||
Ao N, Liu Y, Bian X, Feng H, Liu Y. Ubiquitin-specific peptidase 22 inhibits colon cancer cell invasion by suppressing the signal transducer and activator of transcription 3/matrix metalloproteinase 9 pathway. Mol Med Rep. 2015;12(2):2107–2113. | ||
Ao N, Liu Y, Feng H, et al. Ubiquitin-specific peptidase USP22 negatively regulates the STAT signaling pathway by deubiquitinating SIRT1. Cell Physiol Biochem. 2014;33(6):1863–1875. | ||
Tang B, Liang X, Tang F, et al. Expression of USP22 and Survivin is an indicator of malignant behavior in hepatocellular carcinoma. Int J Oncol. 2015;47(6):2208–2216. | ||
Ji M, Shi H, Xie Y, et al. Ubiquitin specific protease 22 promotes cell proliferation and tumor growth of epithelial ovarian cancer through synergy with transforming growth factor beta1. Oncol Rep. 2015; 33(1):133–140. | ||
Ning Z, Wang A, Liang J, et al. USP22 promotes the G1/S phase transition by upregulating FoxM1 expression via beta-catenin nuclear localization and is associated with poor prognosis in stage II pancreatic ductal adenocarcinoma. Int J Oncol. 2014;45(4):1594–1608. | ||
Ning J, Zhang J, Liu W, Lang Y, Xue Y, Xu S. Overexpression of ubiquitin-specific protease 22 predicts poor survival in patients with early- stage non-small cell lung cancer. Eur J Histochem. 2012;56(4):e46. | ||
Dai W, Yao Y, Zhou Q, Sun CF. Ubiquitin-specific peptidase 22, a histone deubiquitinating enzyme, is a novel poor prognostic factor for salivary adenoid cystic carcinoma. PLoS One. 2014;9(1):e87148. | ||
Wang H, Li YP, Chen JH, et al. Prognostic significance of USP22 as an oncogene in papillary thyroid carcinoma. Tumour Biol. 2013; 34(3):1635–1639. | ||
Piao S, Ma J, Wang W, et al. Increased expression of USP22 is associated with disease progression and patient prognosis of salivary duct carcinoma. Oral Oncol. 2013;49(8):796–801. | ||
Liu YL, Yang YM, Xu H, Dong XS. Aberrant expression of USP22 is associated with liver metastasis and poor prognosis of colorectal cancer. J Surg Oncol. 2011;103(3):283–289. | ||
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. | ||
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. | ||
Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127(9):820–826. | ||
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. | ||
Wang Z, Zhu L, Guo T, Wang Y, Yang J. Decreased H2B monoubiquitination and overexpression of ubiquitin-specific protease enzyme 22 in malignant colon carcinoma. Hum Pathol. 2015;46(7):1006–1014. | ||
Li J, Wang Z, Li Y. USP22 nuclear expression is significantly associated with progression and unfavorable clinical outcome in human esophageal squamous cell carcinoma. J Cancer Res Clin Oncol. 2012; 138(8):1291–1297. | ||
Yang DD, Cui BB, Sun LY, et al. The co-expression of USP22 and BMI-1 may promote cancer progression and predict therapy failure in gastric carcinoma. Cell Biochem Biophys. 2011;61(3):703–710. | ||
Liang JX, Ning Z, Gao W, et al. Ubiquitin specific protease 22 induced autophagy is correlated with poor prognosis of pancreatic cancer. Oncol Rep. 2014;32(6):2726–2734. | ||
Hu J, Yang D, Zhang H, et al. USP22 promotes tumor progression and induces epithelial-mesenchymal transition in lung adenocarcinoma. Lung Cancer. 2015;88(3):239–245. | ||
Liang J, Zhang X, Xie S, et al. Ubiquitin-specific protease 22: a novel molecular biomarker in glioma prognosis and therapeutics. Med Oncol. 2014;31(4):899. | ||
Zhang Y, Yao L, Zhang X, et al. Elevated expression of USP22 in correlation with poor prognosis in patients with invasive breast cancer. J Cancer Res Clin Oncol. 2011;137(8):1245–1253. | ||
Piao S, Liu Y, Hu J, et al. USP22 is useful as a novel molecular marker for predicting disease progression and patient prognosis of oral squamous cell carcinoma. PLoS One. 2012;7(8):e42540. | ||
Melo-Cardenas J, Zhang Y, Zhang DD, Fang D. Ubiquitin-specific peptidase 22 functions and its involvement in disease. Oncotarget. 2016;7(28): 44848–44856. | ||
Yang M, Liu YD, Wang YY, Liu TB, Ge TT, Lou G. Ubiquitin-specific protease 22: a novel molecular biomarker in cervical cancer prognosis and therapeutics. Tumour Biol. 2014;35(2):929–934. | ||
Hu J, Liu YL, Piao SL, Yang DD, Yang YM, Cai L. Expression patterns of USP22 and potential targets BMI-1, PTEN, p-AKT in non-small-cell lung cancer. Lung Cancer. 2012;77(3):593–599. | ||
Schrecengost RS, Dean JL, Goodwin JF, et al. USP22 regulates oncogenic signaling pathways to drive lethal cancer progression. Cancer Res. 2014;74(1):272–286. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.