Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
Prognosis of Patients with Hepatocellular Carcinoma Treated with Transarterial Chemoembolization(MC-hccAI 001): Development and Validation of the ALFP Score
Authors Gong B , Wang X, Guo W , Yang H , Shi Y, Chen Y , Gao S , Chen J , Liu L , Lu L , Chen X
Received 12 April 2023
Accepted for publication 27 July 2023
Published 11 August 2023 Volume 2023:10 Pages 1341—1351
DOI https://doi.org/10.2147/JHC.S415770
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Prof. Dr. Imam Waked
Baocuo Gong,1,2,* Xuewen Wang,1,3,* Wanting Guo,1 Hongyi Yang,1 Yanhong Shi,1 Yaying Chen,1 Simiao Gao,1 Jialin Chen,1 Lifang Liu,2 Linbin Lu,1 Xiong Chen1 On behalf of Fujian HCC-biomarker Study Group
1Department of Oncology, Mengchao Hepatobiliary Hospital of Fujian Medical University, Fuzhou, Fujian, 350025, People’s Republic of China; 2Department of Oncology, Oriental Hospital Affiliated to Xiamen University, Fuzhou, Fujian, 350025, People’s Republic of China; 3Department of Histology and Embryology, School of Basic Medical Sciences, Fujian Medical University, Fuzhou, Fujian, 350122, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Linbin Lu; Xiong Chen, Department of Oncology, Mengchao Hepatobiliary Hospital of Fujian Medical University, 321 Xihong Road, Fuzhou, Fujian, 350025, People’s Republic of China, Email [email protected]; [email protected]
Background: Transarterial chemoembolization (TACE) is the recommended first-line treatment for intermediate-stage Hepatocellular carcinoma (HCC) patients. However, predicting the survival of HCC patients receiving TACE remains challenging.
Methods: In this retrospective study, we analyzed a total of 1805 HCC patients who received TACE. The patients were randomly divided into a training set (n = 1264) and a validation set (n = 541). We examined various prognostic factors within the training set and developed a simple ALFP (ALBI grade, AFP, and Prothrombin time) score, which was subsequently validated using the independent validation set.
Results: Our multivariate analysis revealed that baseline ALBI grade 2 or 3, AFP ≥ 100 ng/mL, and PT > 13.1 s were independent unfavorable prognostic factors for HCC patients receiving TACE (p < 0.05). Based on these findings, we constructed the ALFP score, which assigns 1 point each for ALBI grade 2 or 3, AFP ≥ 100 ng/mL, and PT > 13.1 s. The score has a range of 0 to 3, and higher scores are associated with poorer outcomes. The median overall survival (OS) varied significantly among different ALFP score groups, both in the training set and the validation set (p < 0.001). We further examined the ALFP score in subgroups based on tumor diameter and the number of intrahepatic lesions. In each subgroup, higher ALFP scores were consistently associated with lower OS (p < 0.05).
Conclusion: Our study confirms the prognostic value of the ALFP score in predicting the survival of HCC patients undergoing TACE. The score incorporates easily obtainable baseline parameters and provides a simple and practical tool for risk stratification and treatment decision-making in HCC patients.
Keywords: albumin-bilirubin grade, α-fetoprotein, prothrombin time, transarterial chemoembolization, hepatocellular carcinoma
Introduction
Hepatocellular carcinoma (HCC) is the predominant form of liver cancer and poses a significant global health burden. It ranks as the seventh most common cancer and the second leading cause of cancer-related deaths worldwide.1,2 While surgical resection and liver transplantation offer potential curative options.3 HCC is often diagnosed at advanced stages, such as BCLC stage B or advanced BCLC stage.4,5 According to the Barcelona Clinic Liver Cancer (BCLC) staging system, transarterial chemoembolization (TACE) serves as the primary treatment for patients with intermediate-stage HCC, characterized by asymptomatic, large, or multifocal tumors without macrovascular invasion or extrahepatic metastasis.6 However, the heterogeneity within the intermediate stage, including variations in liver function and tumor characteristics, introduces challenges in predicting patient outcomes and response to TACE,7,8 Consequently, the median survival time for patients treated with TACE has been reported to range from 3.4 to 54.2 months.8–10 It is important to note that not all patients with intermediate-stage HCC experience similar benefits from TACE. Therefore, predicting the survival of HCC patients undergoing TACE is crucial for making informed clinical decisions but remains a formidable challenge at present.
The liver plays a crucial role in synthesizing most coagulation factors, including factors VII, X, V, and II.11 Prothrombin Time (PT) is a commonly used test that assesses the tissue factor (TF) and coagulation pathways involving factors VII, X, V, II, and fibrinogen.12 Abnormalities in coagulation factors are observed in patients with HCC, such as Prothrombin induced by vitamin K absence or antagonist-II (PIVKA-II).13 PIVKA-II leads to prolonged Prothrombin Time and an increased risk of bleeding. Its diagnostic value in HCC patients undergoing surgery and curative ablation has been confirmed,13,14 although its clinical utilization remains limited. On the other hand, PT is a common and easily accessible test, however, its role in assessing the prognosis of HCC patients has not been thoroughly investigated. Some studies indicate that PT may serve as a reliable predictor of patient prognosis in the context of surgical treatment.15–17 Furthermore, PT has been utilized to develop new scoring systems for evaluating liver function and patient survival.18,19 In conclusion, PT shows promise as a prognostic factor for HCC. Since most HCC patients are diagnosed at advanced stages and often undergo TACE or systemic therapy according to guidelines,6 this patient population requires an effective and straightforward clinical scoring system. Based on the findings of our study, we have developed a novel scoring system called the albumin-bilirubin grade, α-fetoprotein, and prothrombin time (ALFP) score. By combining PT with other established prognostic markers such as α-fetoprotein (AFP) and the albumin-bilirubin grade (ALBI), we aim to enhance the accuracy and reliability of prognostic assessment in HCC patients. This comprehensive approach takes into account the liver function, tumor markers, and coagulation status, providing a more comprehensive evaluation of patient prognosis.
Methods and Patients
Patient Selection
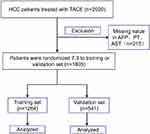
In this retrospective study, we reviewed a cohort of 2020 consecutive HCC patients diagnosed at Sun Yat-sen University Cancer Center (SYSUCC) between January 2007 and May 2012.20–23 In this study, no formal sample capacity calculation was performed. All data available from patients were considered for this study. 2020 patients with histologically or radiologically diagnosed HCC who received transarterial chemoembolization (TACE) were brought into this study. Among these 2020 patients, we excluded 215 patients whose baseline AFP, PT, and Aspartate transaminase (AST) data were missing. As a result, the remaining 1805 patients were included in this study, and we randomly divided patients 7:3 into a training set (n = 1264) and a validation set (n = 541) (Figure 1).
We collected the baseline characteristics of the patients, including gender, age, diameter of the main tumor, biochemical parameters, coagulation profile, and liver function. The liver function was defined using the albumin–bilirubin (ALBI) grade.24 These two cohorts represent patient populations treated with a similar therapeutic strategy, making them comparable in terms of patient and tumor characteristics.
Statement of Ethics
The study protocol (2017-FXY-129) was approved by the Department of Clinical Research at Sun Yat-sen University Cancer Center. Additionally, the Hospital Ethics Committee at the four medical centers granted approval for this study, which exempted the requirement for written informed consent due to its retrospective nature.
Statistical Analysis Methods
In this retrospective study, our cohort was randomly divided into two groups to ensure the accuracy and practicality of the score. We used the chi-squared or Fisher’s exact test to compare categorical data and the Mann–Whitney U-test to compare continuous variables. The prognostic factors were investigated using the Cox proportional hazards regression model. Variables with a p-value < 0.05 in the univariable analysis were considered for multivariable analysis. Variables with a p-value < 0.05 in the multivariable analysis were identified as prognostic factors. Based on the results of the multivariate analysis in the training set, we established a new and simple score. To validate the score and avoid overoptimistic results, we applied it to the validation set. Overall survival (OS) was calculated from the start of TACE until the date of death from any cause, while patients who were still alive were censored at the date of last contact. Survival curves were generated using the Kaplan-Meier method and compared using the Log rank test.
P values of <0.05 were considered statistically significant. All analyses were performed using Empower (R) (www.empowerstats.com, X&Y Solutions, Boston, Massachusetts, USA).
Results
Patient Characteristics (Training and Validation Sets)
A total of 1805 patients were included in this study. The patient characteristics of the training and validation sets are presented in Table 1. In the training set, the median age was 52.6 years, and 69.8% of the patients were male. Among them, 836 patients (66.1%) had a tumor diameter greater than 5 cm, and 777 patients (61.5%) had intrahepatic lesions larger than 3. Serum AFP levels ≥ 100 ng/mL were observed in 737 patients (58.3%), while 256 patients (20.3%) had a Prothrombin time > 13.1 s. According to the ALBI score, grades 1, 2, and 3 were represented by 309 patients (24.4%), 856 patients (67.7%), and 99 patients (7.8%), respectively. The patient characteristics in the validation set were similar to those in the training set, with no significant differences observed (p > 0.05, Table 1).
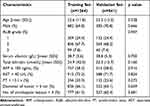 |
Table 1 Baseline Characteristics of Patients in the Training and Validation Sets (N=1805) |
The Development of the ALFP Score in the Training Set
The multivariate analysis revealed that baseline ALBI grade 2 or 3 and AFP ≥ 100 ng/mL and PT 13.1 s were associated OS (ALBI grade 2 or 3, hazard ratio [HR] 1.301, 95% CI 1.073–1.577, p = 0.007: AFP ≥ 100 ng/mL, HR 1.328, 95% CI 1.133–1.557, p < 0.001: PT> 13.1 s HR 1.262, 95% CI 1.047–1.521, p=0.015: Table 2). These factors, ALBI grade, AFP, and PT, emerged as independent prognostic factors, and their hazard ratios were similar in the multivariate analysis. Based on this result, we built an easy score named the albumin–bilirubin grade and α-fetoprotein and prothrombin time score (ALFP score). We assigned 1 point for ALBI grade 2 or 3 and 1 point for baseline AFP ≥ 100 ng/mL, and 1 point for baseline PT> 13.1 s. The grading of the score is as follows: ALFP score 0 points (ALBI grade 1 and AFP < 100 ng/mL and PT <13.1s), 1 point (either ALBI grade 2 or 3, and AFP ≥ 100 ng/mL, and PT>13.1s), and 2 points (both ALBI grade 2 or 3, and AFP ≥ 100 ng/mL, or PT>13.1s and AFP ≥ 100 ng/mL, or ALBI grade 2 or 3 and PT>13.1s), and 3 points (ALBI grade 2 or 3, and AFP ≥ 100 ng/mL, and PT>13.1s).
 |
Table 2 Results of Univariate and Multivariate Analysis in the Training Set |
According to these ALFP scores, the overall Survival (OS) is significantly connected with the score level. The median OS in patients with ALFP scores of 0, 1, 2, and 3 points was 50.1 months (95% CI not applicable [NA]), 33.6 months (95% CI 27.4–39.8), and 20.4 months (95% CI 18.0–22.8); and 12.7 months (95% CI 10.2–15.2), respectively; the difference was statistically significant (p < 0.001: Figure 2A). The 2022 BCLC version stratifies the Intermediate stage HCC into 3 groups,6 the first subgroup could be candidates for a liver transplant if they meet the extended Liver Transplant criteria’ according to the criteria of the Institution,25 aim for improving treatment strategy. Based on Milan criteria26 (1 lesion ≤5 cm or 2–3 lesions ≤ 3), we divided patients into two groups by the diameter of tumor (≤5 cm or >5cm) and the No. Of intrahepatic lesions (≤3 or >3), and calculating ALFP score in two sets, we found the OS is strongly connected with the level of score in each group, the median OS in the diameter of tumor ≤5 cm group with ALFP scores of 1, 2 and 3 points were: 54.9 months (95% CI not applicable), 50.0 months (95% CI 38.5–61.5), 23.9 months (95% CI 12.3–35.5), respectively; The difference was statistically significant (p = 0.0077: Figure 3A). The diameter of tumor >5 cm group with ALFP scores of 0, 1, 2 and 3 points were: 31.8 months (95% CI 11.7–51.9), 20.3 months (95% CI 17.4–23.2), 15.6 months (95% CI 13.1–18.1), 10.8 months (95% CI 8.2–13.4) respectively; The difference was statistically significant (p < 0.0001: Figure 3A). The median OS in No. Of intrahepatic lesions ≤ 3 groups with ALFP scores of 1, 2, and 3 points were: 42.7 months (95% CI 27.4–58.0), 34.4 months (95% CI 21.4–47.4), 16.8 months (95% CI 6.8–26.8), respectively; The difference was statistically significant (p = 0.002: Figure 4A). The No. of intrahepatic lesions >3 group with ALFP scores of 0, 1, 2 and 3 points were: 39.5 months (95% CI 23.6–55.4), 22.4 months (95% CI 14.5–30.3), 18.2 months (95% CI 16.0–20.4), 10.8 months (95% CI 7.8–13.8); The difference was statistically significant (p < 0.001: Figure 4A).
The Validation of the ALFP Score in the Validation Set
We validated our research result in the validation set (Figure 1), Baseline patients’ characteristics are described in Table 1, and there is no significant difference between the two cohorts (p>0.05: Table 1), which is considered comparable. The median OS in patients with ALFP scores of 0, 1, 2, and 3 points were 42.5 months (95% CI 16.1–68.9),32.6 months (95% CI 25.1–40.1), 20.4 months (95% CI 16.4–24.4), 13.0 months (95% CI 0.0–27.3), respectively; the difference was statistically significant (p < 0.0019: Figure 2B). The median OS in the diameter of tumor ≤5 cm group with ALFP scores of 0, 1, 2 and 3 points were: 59.0 months (95% CI 38.8–79.2), 47.7 months (95% CI not applicable), 29.6 months (95% CI 19.1–40.1), 27.0 months (95% CI 0.0–54.1), respectively; The difference was statistically significant (p = 0.015: Figure 3B). The diameter of tumor >5 cm group with ALFP scores of 0, 1, 2 and 3 points were: 21.6 months (95% CI 14.5–28.7), 25.1 months (95% CI 16.5–33.7), 16.3 months (95% CI 11.8–20.8), 9.8 months (95% CI 2.8–16.8); respectively. The difference was insignificant (p =0.092: Figure 3B). The median OS in intrahepatic lesions number ≤ 3 groups with ALFP scores of 0, 1, 2, and 3 points were: 59.0 months (95% CI 28.2–89.8), 39.3 months (95% CI 24.3–54.3), 35.6 months (95% CI 15.3–55.9), 28.3 months (95% CI 3.0–53.6), respectively; The difference was no statistically significant (p = 0.35: Figure 4B). In intrahepatic lesions number >3 groups with ALFP scores of 0, 1, 2 and 3 points were: 42.5 months (95% CI 7.9–77.1), 28.0 months (95% CI 11.2–44.8), 19.2 months (95% CI 15.1–23.3), 12.5 months (95% CI 8.3–16.7), respectively; The difference was statistically significant (p < 0.034: Figure 4B). The performance of ALFP score in validation is similar to the training set, indicate the accuracy and predictive ability of the score.
Discussion
In the current study, we identified baseline PT > 13.1 s, AFP > 100 ng/mL, and ALBI grade 2b/3 as independent unfavorable prognostic factors in HCC patients undergoing TACE. Building upon these findings, we developed a straightforward and practical scoring system called the ALFP score. The ALFP score exhibited good performance in terms of overall survival (OS) curves, both in the training set and in the validation set, providing further confirmation of its predictive ability.
TACE is the recommended therapy for unresectable HCC and has shown improved survival outcomes for patients.5,27 The prognosis of HCC patients is connected with liver function and tumor burden, and the prediction system should include both factors. Child-Pugh system (CPS) predicts prognosis in patients with chronic liver disease (CLD). It has been extended inclusion in many HCC staging systems, including the Cancer of the Liver Italian Program (CLIP)28 score, the Japan Integrated Staging Score (JIS score),29 and the widely used Barcelona Clinic Liver Cancer (BCLC)30 score. However, CPS is not the most suitable score for assessing liver dysfunction.31 To address this limitation, the albumin-bilirubin (ALBI) grade24 was proposed, which calculates a score based on serum albumin and bilirubin levels. The ALBI grade has demonstrated utility and accuracy in multiple external validations,32–35 and exhibited the highest homogeneity for survival prediction among various liver functional reserve models.36 In the 2022 version of BCLC staging system,6 the ALBI grade is recommended as a score for assessing compensated liver function. Previous studies have consistently indicated that the ALBI grade provides more precise and accurate prognostic information than the CPS, particularly in patients with well-preserved liver function. In the present cohort, the multivariate analysis in the training set confirmed that a baseline ALBI grade of 2 or 3 was associated with a poor prognosis (p = 0.007, Table 2). Based on these previous findings, we incorporated the ALBI grade as a favorable prognostic factor in our current study.
Alpha-fetoprotein (AFP) is a glycoprotein that is produced in the fetal yolk sac and liver during the gestational period.37 AFP has been widely used as a biomarker to monitor HCC treatment and guide therapeutic decision-making, as well as for predictive analysis.38 Researchers have observed that AFP-high tumors exhibit enrichment in the VEGF pathway, which promotes tumor progression and metastasis.39 Additionally, in cases where TACE is ineffective, there is an increase in VEGF (vascular endothelial growth factor) and b-FGF (basic fibroblast growth factor) during subsequent treatments, which may explain the association between elevated AFP levels and poor prognosis in HCC patients undergoing TACE.40 In this study, AFP levels ≥100 ng/mL were strongly associated with overall survival (OS) in 58% of the patients (p < 0.001, Table 1). Although the precise role of AFP in tumor growth is still not fully understood, it serves as a reliable indicator in HCC patients and is associated with the VEGF pathway. Therefore, AFP levels may guide the development of new treatment strategies in the future. In conclusion, we have incorporated AFP as an unfavorable indicator for HCC patients undergoing TACE.
In 1984, Liebman discovered that Prothrombin induced by vitamin K absence or antagonist-II (PIVKA-II) was significantly elevated in the serum of HCC patients.41 Numerous studies have since confirmed that PIVKA-II can be used for HCC diagnosis in combination with AFP and is strongly associated with the prognosis of HCC patients who receive curative treatment.14,42 In the absence of vitamin K, hepatocytes are unable to synthesize normal vitamin K-dependent coagulation factors (VII, X, V, II), resulting in impaired coagulation function and prolonged prothrombin time. In this study, we found that PT > 13.1 s was observed in 20% of both cohorts and was statistically significant in multivariate analysis with regard to overall survival (p < 0.025, Table 1). This finding is consistent with previous studies, which further validates the performance of PT as a prognostic factor. The prognostic factors of liver cancer are complex. AFP has been firmly established as a predictive factor for post-liver transplantation recurrence in large-scale external validation studies.43 ALBI demonstrates superior sensitivity to early liver damage compared to JIS score and CPS.44 Researchers achieved promising experimental results when using AFP combined with ALBI score to predict the prognosis of liver cancer patients receiving Atezolizumab plus bevacizumab (AtezoBev) treatment.45 To achieve the best predictive efficacy in the treatment of liver cancer, consideration must be given to both tumor-related factors and liver-related factors. Building upon the previous study, we developed a scoring system to enhance prediction accuracy. By incorporating these comprehensive scoring criteria based on common serum laboratory indexes, we are able to categorize HCC patients with TACE into four risk categories. This scoring system provides a more detailed and standardized approach to the treatment of liver cancer.
The multivariate analysis identified AFP > 100 ng/mL, ALBI grade 2b/3, and PT > 13.1 s as independent prognostic factors, with similar hazard ratios (HRs). Based on the ALFP score system, each score was found to be statistically significant in relation to overall survival (OS), with higher scores indicating a poorer outcome. This result was confirmed in the validation set and is consistent with previous studies. In the subgroup analysis, higher scores were associated with lower OS, and these associations were statistically significant. The importance of tumor burden and liver function reserve in HCC prognosis cannot be understated. Patients were grouped based on tumor diameter and the number of intrahepatic lesions, and under the same tumor burden, those with lower scores had better OS. This finding was confirmed in both sets and was particularly statistically significant in the higher tumor burden group (p < 0.0001, Figure 3; p < 0.00047, Figure 4). It indicates that the prognosis of these patients is strongly influenced by liver function, and those in the higher score group did not derive significant benefits from TACE compared to the low score group. However, in the validation set, the group with a tumor diameter >5 cm and the group with ≤3 intrahepatic lesions did not show statistically significant differences (p > 0.05, Figures 3 and 4). This could be attributed to the smaller sample size of the validation set compared to the training set.
Due to the retrospective nature of this study, it is important to acknowledge certain limitations. Firstly, the true survival time of many patients remains unknown due to loss to follow-up, thus necessitating the treatment of the last contact time as a censoring event. Secondly, the enrolled patients do not cover a comprehensive range of hepatitis types. Additionally, there is missing clinical information for some patients. To mitigate these limitations, future prospective studies are planned to complement our findings.
In conclusion, the ALFP score can predict the prognosis of HCC patients receiving TACE and guide the subdivision and precise treatment of intermediate hepatocellular carcinoma.
Ethics Committee Approval and Patient Consent
The study protocol (2017-FXY-129) was approved by the Department of Clinical Research at Sun Yat-sen University Cancer Center. Additionally, the Hospital Ethics Committee at the four medical centers granted approval for this study, which exempted the requirement for written informed consent due to its retrospective nature.
Acknowledgments
Xiong Chen received financial support from the Research Initiation Foundation of Mengchao Hepatobiliary Hospital of Fujian Medical University (Nos QDZJ-2022-001), Natural Science Foundation of Fujian Province (Nos.2021J0128 and 2020J011147) and the Science and Technology Innovation Joint Foundation of Fujian Province (Nos.2017Y9125).
Disclosure
The authors declare no competing interest exists in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. McGlynn KA, Petrick JL, El-Serag HB. Epidemiology of hepatocellular carcinoma. Hepatology. 2021;73(Suppl 1):4–13. doi:10.1002/hep.31288
3. Kim DW, Talati C, Kim R. Hepatocellular carcinoma (HCC): beyond sorafenib-chemotherapy. J Gastrointest Oncol. 2017;8(2):256–265. doi:10.21037/jgo.2016.09.07
4. Hucke F, Sieghart W, Schöniger-Hekele M, Peck-Radosavljevic M, Müller C. Clinical characteristics of patients with hepatocellular carcinoma in Austria - is there a need for a structured screening program? Wien Klin Wochenschr. 2011;123(17–18):542–551. doi:10.1007/s00508-011-0033-9
5. Llovet JM, Real MI, Montaña X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359(9319):1734–1739. doi:10.1016/S0140-6736(02)08649-X
6. Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol. 2022;76(3):681–693. doi:10.1016/j.jhep.2021.11.018
7. Bolondi L, Burroughs A, Dufour JF, et al. Heterogeneity of patients with intermediate (BCLC B) Hepatocellular Carcinoma: proposal for a subclassification to facilitate treatment decisions. Semin Liver Dis. 2012;32(4):348–359. doi:10.1055/s-0032-1329906
8. Raoul JL, Sangro B, Forner A, et al. Evolving strategies for the management of intermediate-stage hepatocellular carcinoma: available evidence and expert opinion on the use of transarterial chemoembolization. Cancer Treat Rev. 2011;37(3):212–220. doi:10.1016/j.ctrv.2010.07.006
9. Burrel M, Reig M, Forner A, et al. Survival of patients with hepatocellular carcinoma treated by transarterial chemoembolisation (TACE) using drug eluting beads. Implications for clinical practice and trial design. J Hepatol. 2012;56(6):212–220. doi:10.1016/j.jhep.2012.01.008
10. Malagari K, Pomoni M, Moschouris H, et al. Chemoembolization with doxorubicin-eluting beads for unresectable hepatocellular carcinoma: five-year survival analysis. Cardiovasc Intervent Radiol. 2012;35(5):1119–1128. doi:10.1007/s00270-012-0394-0
11. Woreta TA, Alqahtani SA. Evaluation of abnormal liver tests. Med Clin North Am. 2014;98(1):1–16. doi:10.1016/j.mcna.2013.09.005
12. Dorgalaleh A, Favaloro EJ, Bahraini M, Rad F. Standardization of Prothrombin Time/International Normalized Ratio (PT/INR). Int J Lab Hematol. 2021;43(1):21–28. doi:10.1111/ijlh.13349
13. Zhang D, Liu Z, Yin X, et al. Prognostic value of PIVKA-II in hepatocellular carcinoma patients receiving curative ablation: a systematic review and meta-analysis. Int J Biol Markers. 2018;33(3):266–274. doi:10.1177/1724600818760234
14. Feng H, Li B, Li Z, Wei Q, Ren L. PIVKA-II serves as a potential biomarker that complements AFP for the diagnosis of hepatocellular carcinoma. BMC Cancer. 2021;21(1):401. doi:10.1186/s12885-021-08138-3
15. Wang HS, Ge XX, Li QP, Nie JJ, Miao L. Clinical significance of prothrombin time in cholangiocarcinoma patients with surgeries. Can J Gastroenterol Hepatol. 2019;2019:3413969.
16. Yokoyama Y, Ebata T, Igami T, Sugawara G, Ando M, Nagino M. Predictive power of prothrombin time and serum total bilirubin for postoperative mortality after major hepatectomy with extrahepatic bile duct resection. Surgery. 2014;155(3):504–511. doi:10.1016/j.surg.2013.08.022
17. Furuyama T, Kudo A, Matsumura S, et al. Preoperative direct bilirubin to prothrombin time ratio index to prevent liver failure after minor hepatectomy. J Hepatobiliary Pancreat Sci. 2016;23(12):763–770. doi:10.1002/jhbp.400
18. Mao M, Wang X, Song Y, et al. Novel prognostic scores based on plasma prothrombin time and fibrinogen levels in patients with AFP-negative Hepatocellular Carcinoma. Cancer Control. 2020;27(1):1073274820915520. doi:10.1177/1073274820915520
19. Haruki K, Shiba H, Saito N, et al. Risk stratification using a novel liver functional reserve score of combination prothrombin time-international normalized ratio to albumin ratio and albumin in patients with hepatocellular carcinoma. Surgery. 2018;164(3):404–410. doi:10.1016/j.surg.2018.02.022
20. Shen L, Zeng Q, Guo P, et al. Dynamically prognosticating patients with hepatocellular carcinoma through survival paths mapping based on time-series data. Nat Commun. 2018;9(1):2230. doi:10.1038/s41467-018-04633-7
21. Chen MS, Li JQ, Zhang YQ, et al. High-dose iodized oil transcatheter arterial chemoembolization for patients with large hepatocellular carcinoma. World J Gastroenterol. 2002;8(1):74–78. doi:10.3748/wjg.v8.i1.74
22. Chen ZH, Hong YF, Lin J, et al. Validation and ranking of seven staging systems of hepatocellular carcinoma. Oncol Lett. 2017;14(1):705–714. doi:10.3892/ol.2017.6222
23. He C, Zhang Y, Lin X. Increased overall survival and decreased cancer-specific mortality in patients with hepatocellular carcinoma treated by transarterial chemoembolization and human adenovirus type-5 combination therapy: a competing risk analysis. J Gastrointest Surg. 2018;22(6):989–997. doi:10.1007/s11605-018-3703-3
24. Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33(6):550–558. doi:10.1200/JCO.2014.57.9151
25. Mehta N, Bhangui P, Yao FY, et al. Liver transplantation for hepatocellular carcinoma. Working Group report from the ILTS transplant oncology consensus conference. Transplantation. 2020;104(6):1136–1142. doi:10.1097/TP.0000000000003174
26. Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334(11):693–699. doi:10.1056/NEJM199603143341104
27. Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35(5):1164–1171. doi:10.1053/jhep.2002.33156
28. The Cancer of the Liver Italian Program (CLIP) Investigators. Prospective validation of the CLIP score: a new prognostic system for patients with cirrhosis and hepatocellular carcinoma. Hepatology. 2000;31(4):840–845. doi:10.1053/he.2000.5628
29. Kudo M, Chung H, Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging Score (JIS score). J Gastroenterol. 2003;38(3):207–215. doi:10.1007/s005350300038
30. Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19(3):329–338. doi:10.1055/s-2007-1007122
31. Durand F, Valla D. Assessment of prognosis of cirrhosis. Semin Liver Dis. 2008;28(1):110–122. doi:10.1055/s-2008-1040325
32. Hickey R, Mouli S, Kulik L, et al. Independent analysis of albumin-bilirubin grade in a 765-patient cohort treated with transarterial locoregional therapy for Hepatocellular Carcinoma. J Vasc Interv Radiol. 2016;27(6):795–802. doi:10.1016/j.jvir.2016.03.005
33. Li MX, Zhao H, Bi XY, et al. Prognostic value of the albumin-bilirubin grade in patients with hepatocellular carcinoma: validation in a Chinese cohort. Hepatol Res. 2017;47(8):731–741. doi:10.1111/hepr.12796
34. Ma XL, Zhou JY, Gao XH, et al. Application of the albumin-bilirubin grade for predicting prognosis after curative resection of patients with early-stage hepatocellular carcinoma. Clin Chim Acta. 2016;462:15–22. doi:10.1016/j.cca.2016.08.005
35. Pinato DJ, Sharma R, Allara E, et al. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma. J Hepatol. 2017;66(2):338–346. doi:10.1016/j.jhep.2016.09.008
36. Ho SY, Liu PH, Hsu CY, et al. Comparison of twelve liver functional reserve models for outcome prediction in patients with hepatocellular carcinoma undergoing surgical resection. Sci Rep. 2018;8(1):4773. doi:10.1038/s41598-018-22923-4
37. Mizejewski GJ. Biological role of alpha-fetoprotein in cancer: prospects for anticancer therapy. Expert Rev Anticancer Ther. 2002;2(6):709–735. doi:10.1586/14737140.2.6.709
38. Sauzay C, Petit A, Bourgeois AM, et al. Alpha-foetoprotein (AFP): a multi-purpose marker in hepatocellular carcinoma. Clin Chim Acta. 2016;463:39–44. doi:10.1016/j.cca.2016.10.006
39. Kamei S, Kono K, Amemiya H, et al. Evaluation of VEGF and VEGF-C expression in gastric cancer cells producing alpha-fetoprotein. J Gastroenterol. 2003;38(6):540–547. doi:10.1007/s00535-002-1099-y
40. Sergio A, Cristofori C, Cardin R, et al. Transcatheter arterial chemoembolization (TACE) in hepatocellular carcinoma (HCC): the role of angiogenesis and invasiveness. Am J Gastroenterol. 2008;103(4):914–921. doi:10.1111/j.1572-0241.2007.01712.x
41. Liebman HA, Furie BC, Tong MJ, et al. Des-gamma-carboxy (abnormal) prothrombin as a serum marker of primary hepatocellular carcinoma. N Engl J Med. 1984;310(22):1427–1431. doi:10.1056/NEJM198405313102204
42. Nakao A, Virji A, Iwaki Y, Carr B, Iwatsuki S, Starzl E. Abnormal prothrombin (DES-gamma-carboxy prothrombin) in hepatocellular carcinoma. Hepatogastroenterology. 1991;38(5):450–453.
43. Notarpaolo A, Layese R, Magistri P, et al. Validation of the AFP model as a predictor of HCC recurrence in patients with viral hepatitis-related cirrhosis who had received a liver transplant for HCC. J Hepatol. 2017;66(3):552–559. doi:10.1016/j.jhep.2016.10.038
44. Hiraoka A, Kumada T, Kudo M, et al. Albumin-Bilirubin (ALBI) grade as part of the evidence-based clinical practice guideline for HCC of the Japan Society of Hepatology: a comparison with the liver damage and child-Pugh classifications. Liver Cancer. 2017;6(3):204–215. doi:10.1159/000452846
45. Campani C, Bamba-Funck J, Campion B, et al. Baseline ALBI score and early variation of serum AFP predicts outcomes in patients with HCC treated by atezolizumab-bevacizumab. Liver Int. 2023;43(3):708–717. doi:10.1111/liv.15487
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.