Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
PRIMUS – Prompt Initiation of Maintenance Therapy in the US: A Real-World Analysis of Clinical and Economic Outcomes Among Patients Initiating Triple Therapy Following a COPD Exacerbation
Authors Tkacz J, Evans KA , Touchette DR , Portillo E, Strange C , Staresinic A, Feigler N, Patel S, Pollack M
Received 4 November 2021
Accepted for publication 24 January 2022
Published 10 February 2022 Volume 2022:17 Pages 329—342
DOI https://doi.org/10.2147/COPD.S347735
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Joseph Tkacz,1 Kristin A Evans,1 Daniel R Touchette,2 Edward Portillo,3 Charlie Strange,4 Anthony Staresinic,5 Norbert Feigler,5 Sushma Patel,5 Michael Pollack5
1Life Sciences, IBM Watson Health, Cambridge, MA, USA; 2Center for Pharmacoepidemiology and Pharmacoeconomic Research, University of Illinois College of Pharmacy, Chicago, IL, USA; 3Pharmacy Practice Division, University of Wisconsin-Madison School of Pharmacy, Madison, WI, USA; 4Division of Pulmonary, Critical Care, Allergy and Sleep Medicine, Medical University of South Carolina, Charleston, SC, USA; 5BioPharmaceuticals, US Medical Affairs, AstraZeneca, Wilmington, DE, USA
Correspondence: Michael Pollack, AstraZeneca, 1800 Concord Pike, Wilmington, DE, 19850, USA, Tel +1 302 377 4911, Email [email protected]
Purpose: Patients with chronic obstructive pulmonary disease (COPD) may experience moderate (requiring outpatient care) or severe (requiring hospitalization) disease exacerbations. Guidelines recommend escalation from dual to triple therapy (inhaled corticosteroid + long-acting beta agonist + long-acting muscarinic antagonist) after two moderate or one severe exacerbation in a year. This study examined whether prompt initiation of triple therapy lowers risk of future exacerbations and reduces healthcare costs, compared to delayed/very delayed triple therapy after an exacerbation.
Patients and Methods: This retrospective observational study of US healthcare claims included patients ≥ 40 years old with COPD who initiated triple therapy (1/1/2011– 3/31/2020) after ≥ 2 moderate or ≥ 1 severe exacerbation in the prior year. The earliest of the second moderate or first severe exacerbation was the index date. Patients were stratified by triple therapy timing: prompt (≤ 30 days post-index), delayed (31– 180 days), very delayed (181– 365 days). COPD exacerbations, all-cause and COPD-related healthcare utilization and costs were assessed during 12 months post-index (follow-up). Multivariable regression estimated the effect of each 30-day delay in triple therapy on the odds of exacerbations, number of exacerbations, and costs during follow-up, controlling for patient characteristics.
Results: A total of 24,770 patients were included: 7577 prompt, 9676 delayed, 7517 very delayed. Each 30-day delay of triple therapy was associated with 11% and 7% increases in the odds of any exacerbation and a severe exacerbation, respectively (odds ratio [95% CI]: 1.11 [1.10– 1.13] and 1.07 [1.05– 1.08]), a 4.3% (95% CI: 3.9– 4.6%) increase in the number of exacerbations, a 1.8% (95% CI: 1.3– 2.3%) increase in all-cause costs, and a 2.1% (95% CI: 1.6– 2.6%) increase in COPD-related costs during follow-up.
Conclusion: Promptly initiating triple therapy after two moderate or one severe exacerbation is associated with decreased morbidity and economic burden in COPD. Proactive disease management may be warranted to prevent future exacerbations and lower costs among patients with COPD.
Keywords: costs, discharge, hospitalization, utilization
Introduction
Chronic obstructive pulmonary disease (COPD) is a common progressive disease characterized by persistent airflow limitation,1 affecting an estimated 4.6–6.6% of American adults.2,3 Patients with COPD often have periods of acute worsening of symptoms, termed COPD exacerbations.4 Moderate exacerbations require use of antibiotics and/or systemic corticosteroids, whereas severe exacerbations are those that result in hospitalization. Severe events may account for as much as 70% of the estimated $40 billion annual COPD-related medical costs in the United States (US).5–8 Thus, reduction of exacerbation frequency and severity should be a primary goal for clinicians and payers to reduce the clinical and economic burden of COPD.
Currently, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) report recommends escalation of COPD treatment based on the presence of ongoing symptoms and recent history of exacerbations.9 Escalation to triple therapy (inhaled corticosteroid [ICS]/long-acting beta-agonist [LABA]/long-acting muscarinic antagonist [LAMA]) is recommended specifically for patients who have experienced recurrent moderate exacerbations or a severe exacerbation in the prior year, despite receiving dual therapy with an ICS/LABA or LAMA/LABA. Over the past decade, several real-world studies have assessed the relationship between COPD maintenance treatment initiation and health outcomes. Results indicate that prompt initiation of general maintenance therapy after an exacerbation is associated with reduced healthcare utilization and expenditures, in addition to lower risk for subsequent exacerbations.10–16 However, many of these findings are now outdated with certain studies utilizing administrative claims data as far back as 2003, and few have considered the role of moderate exacerbations.17–19 Furthermore, these prior studies have not examined the initiation of triple therapy specifically in the context of current treatment recommendations. Therefore, the objectives of this study were to assess the risk of subsequent exacerbations and added costs associated with delayed initiation of triple therapy after one severe or ≥2 moderate COPD exacerbations, and to describe patients with prompt vs delayed initiation of triple therapy.
Methods
Study Design and Data Source
This retrospective observational analysis used health insurance claims data from the IBM® MarketScan® Commercial, Medicare Supplemental, and Multi-State Medicaid Research Databases spanning January 1, 2009 through March 31, 2020. All patient records were de-identified and certified to be fully compliant with US patient confidentiality requirements set forth in the Health Insurance Portability and Accountability Act of 1996. Since this was a secondary analysis of an existing database of administrative claims, Institutional Review Board approval was not required.
Patient Selection and Cohort Assignment
Patients with COPD were identified in the databases by at least 1 non-diagnostic inpatient or outpatient medical claim with a diagnosis of COPD between January 1, 2010 and March 31, 2020. COPD was identified by International Classification of Diseases, Clinical Modification, 9th and 10th revision diagnosis codes (ICD-9: 491.xx-492.xx, 494.xx, 496.xx; ICD-10: J41.0, J41.1, J41.8, J42, J43.0-J43.2, J43.8-J44.1, J44.9, J47.0, J47.1, J47.9).20,21
Evidence of triple therapy was required between January 1, 2011 and March 31, 2019, defined as either one pharmacy claim for a closed triple therapy product containing ICS+LABA+LAMA, or separate pharmacy claims for each component of triple therapy with at least 14 consecutive and 30 total days of overlap between all components during a 90-day period.
Patients were then required to show evidence of at least two moderate or one severe exacerbation during the 12-month period preceding triple therapy initiation. Moderate exacerbations were defined as either a) an outpatient medical claim (office or emergency department [ED]) with a COPD diagnosis and a pharmacy claim for a short course (≤14 days) of a systemic corticosteroid or antibiotic within ± 7 days, or b) an outpatient medical claim with a COPD diagnosis code and a procedure code for a corticosteroid injection. Severe exacerbations were defined as inpatient admissions with a primary diagnosis of COPD. The earliest of the second moderate or first severe exacerbation in the 12 months before index treatment was the index exacerbation date.
Patients were required to be at least 40 years old on the index exacerbation date and to have at least 12 months of continuous enrollment in the database with medical and pharmacy benefits before (baseline) and after (follow-up) the index exacerbation date. A minimum age of 40 years was used to be consistent with common healthcare quality measures used by the Agency for Healthcare Research and Quality20 and the Centers for Medicare and Medicaid Services.21 Patients were excluded if they presented evidence of cancer other than basal or squamous cell skin cancer, interstitial fibrosis, sarcoidosis, or pulmonary embolism during the baseline or follow-up periods, evidence of triple therapy during baseline, or any days of overlap between the three triple therapy components (not meeting the minimum requirement for triple therapy described above) between the index exacerbation and triple therapy initiation, or if they were dually eligible for Medicare and Medicaid during the baseline or follow-up periods.
Patients were stratified into three groups according to the time between their index exacerbation and triple therapy initiation: 1) prompt: ≤30 days; 2) delayed: 31–180 days; 3) very delayed: 181–365 days.
Outcomes Assessment
Primary outcomes included COPD exacerbations, healthcare resource utilization, and healthcare costs during the 12-month follow-up. The number and type of exacerbations were assessed. To be counted as separate exacerbations, at least 14 days were required between consecutive events.
The frequency and number of all-cause and COPD-related inpatient admissions, ED visits, outpatient office visits, primary care provider (PCP) office visits, pulmonologist office visits, other outpatient visits (all other outpatient settings), and outpatient prescriptions were assessed during the 12 months after the index exacerbation, not including the index outpatient visit for moderate index exacerbations or the index hospitalization for severe index exacerbations. Ninety-day COPD readmissions were also assessed. COPD-related healthcare encounters were identified as inpatient admissions with a primary diagnosis of COPD, outpatient claims with a diagnosis of COPD in any position, and outpatient pharmacy claims for COPD treatments, including long-acting maintenance treatments (ICS, LABA, LAMA, LAMA/LABA, ICS/LABA) and short-acting maintenance treatments (short-acting beta agonists [SABA], short-acting muscarinic antagonists [SAMA], SABA/SAMA, oral corticosteroids [OCS]). Due to inherent differences in reimbursement practices between payer types, healthcare resource utilization and costs were examined separately among Commercial/Medicare and Medicaid patients.
Healthcare costs were derived from fully adjudicated claims as the total paid amounts (payer plus patient payments), adjusted for inflation using the medical care component of the Consumer Price Index, and standardized to 2020 US dollars.22 Cost analyses are reported for the 89% of study patients who had full paid amounts on their claims during the study period.
Baseline Variables
Demographic characteristics were assessed on the index exacerbation date; clinical characteristics were assessed during the 12-month baseline period, including the Elixhauser Comorbidity Index (ECI),23 presence of comorbidities, tobacco use, nebulizer use, and oxygen therapy. Baseline comorbidities were identified by the presence of one or more medical claim(s) with the diagnosis in any position. Tobacco use was identified by claims with a diagnosis or procedure code for tobacco use disorder, history of tobacco use, nicotine dependence, or tobacco abuse or cessation counseling. Nebulizer use and oxygen therapy were identified using relevant procedure codes for these services.
Statistical Analyses
Outcomes and patient characteristics are described for each triple therapy cohort (prompt, delayed, very delayed), and where appropriate, according to payer type. Descriptive statistics included means, standard deviations (SD), and medians for continuous variables, and frequencies and proportions for categorical variables. Continuous variables were compared between groups by analyses of variance and Mann–Whitney U-tests; categorical variables were compared by chi-square tests. An alpha level of 0.05 was used to identify significant differences between groups.
Multivariable logistic regression models estimated the effect of each 30-day delay in initiation of triple therapy on the odds of having any exacerbation (moderate or severe), a severe exacerbation, any inpatient admission, a 90-day COPD readmission, and an all-cause or COPD-related ED visit during the 12-month follow-up period. Negative binomial regression estimated the change in the number of COPD exacerbations during follow-up per 30-day delay in triple therapy initiation. Generalized linear models (GLM) with a log-link function and gamma distribution estimated the incremental change in all-cause and COPD-related costs associated with each 30-day delay of triple therapy. All models controlled for baseline patient characteristics, exacerbations, and healthcare utilization.
Results
Study Sample and Baseline Characteristics
A total of 24,770 patients met inclusion and exclusion criteria (Figure 1). Demographic characteristics are shown in Table 1. The mean time from index exacerbation to triple therapy initiation was 120 (±107) days. Nearly three quarters (73.3%) of patients had at least one long-acting COPD treatment during baseline, and 81.6% had a short-acting maintenance treatment. ICS/LABA and LAMA were the most common long-acting treatments during baseline among all groups, with 45.3% and 26.2% of all patients, respectively, having at least one baseline prescription; 74.8% of patients had a SABA and 24.2% had a SABA/SAMA during baseline.
 |
Table 1 Demographic Characteristics |
Nearly one third (30.6%) of patients had prompt (≤30 days), 39.1% delayed (31–180 days), and 30.3% very delayed (181–365 days) initiation of triple therapy. The average time to initiation was 7.5 days (±9.4) for prompt initiators, 98.5 days (±43.7) among delayed initiators, and 260 days (±48.9) among very delayed initiators. Delayed and very delayed patients presented a greater baseline comorbidity burden than prompt patients (Table 2). Baseline nebulizer use and oxygen therapy were significantly more common among delayed and very delayed vs prompt initiators (P<0.05).
 |
Table 2 Clinical Characteristics During the 12-Month Baseline Period |
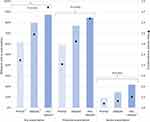
Patients with delayed or very delayed triple therapy were more likely than prompt initiators to fill a prescription for a long-acting or short-acting maintenance medication during baseline, though about one quarter of delayed or very delayed patients had no baseline long-acting maintenance treatment (Figure 2). Delayed and very delayed patients were significantly more likely than prompt patients to have any COPD-related pulmonologist visits before their index exacerbation, and they had up to twice as many pulmonologist visits, on average.
Follow-Up COPD Exacerbations
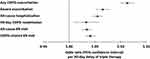
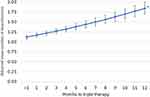
Unadjusted results for the occurrence and number of exacerbations during follow-up are depicted in Figure 3. After adjusting for patient characteristics and baseline exacerbation history, each 30-day delay in receiving triple therapy was associated with an 11% increase in the odds of another exacerbation during the 12 months after the index exacerbation (P<0.001; Figure 4), which equates to 44% greater odds of an exacerbation for a patient with the mean time to triple therapy of the full sample (4 months), compared to a patient who received triple therapy <30 days after their exacerbation. There was a significant 6.5% increase in the odds of a severe exacerbation per 30-day delay of triple therapy, which equates to 26% greater odds of a severe exacerbation for the average patient who initiates therapy 4 months after their index exacerbation. Furthermore, adjusted analysis shows that each additional 30-day delay of triple therapy was associated with a statistically significant 4% increase in the average number of exacerbations during the follow-up period. As depicted in Figure 5, patients who do not receive triple therapy until one year after their index exacerbation would, on average, experience 1.84 exacerbations during the 12-month post-index period (95% CI: 1.70–2.00), compared to 1.12 (95% CI: 1.07–1.16) exacerbations among patients who received triple therapy within 30 days.
Follow-Up Healthcare Utilization and Costs
Unadjusted results for healthcare utilization by payer type are shown in Table 3. After adjusting for patient characteristics, each additional 30-day delay of triple therapy was associated with a significant 5.5% and 3.3% increase in the odds of any hospitalization and a 90-day COPD readmission, respectively (Figure 4). The average study patient would have had 22% greater odds of an all-cause inpatient admission and 13% greater odds of a 90-day COPD readmission after a 4-month delay of triple therapy, compared to a patient who received triple therapy <30 days after their exacerbation. The adjusted increase in odds of an all-cause or COPD-related ED visit for each additional month to triple therapy were 3.4% and 4.1%, respectively.
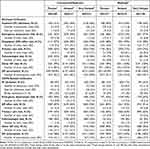 |
Table 3 All-Cause and COPD-Related Healthcare Utilization During 12-Month Follow-Up |
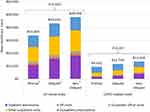
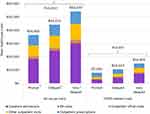
Prior to adjustment, total all-cause healthcare costs during the 12-month follow-up period were 28% and 42% higher among delayed and very delayed patients, respectively, compared to prompt patients within the Commercial/Medicare sample (P<0.001) (Figure 6). Notably, all-cause prescription costs among prompt patients were up to 13–14% lower than prescription costs among delayed and very delayed patients. While generally 28% of total-costs were attributed to COPD-related care, delayed and very delayed patients had 24% and 43% higher COPD-related costs, respectively, compared to prompt patients. Similar trends were observed for the Medicaid sample, where all-cause prescription costs were 4–17% lower among prompt vs delayed or very delayed patients and the proportion of total costs attributed to COPD increased from 22% for prompt patients to 27% for very delayed patients (Figure 7).
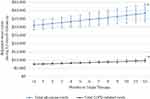
Multivariable adjustment demonstrated a modest yet significant 1.8% increase in total all-cause healthcare costs in the 12 months after the index exacerbation for each additional 30-day delay of triple therapy, equating to an average increase of $616 (95% CI: $593-$638) per patient per month of delay (Figure 8). Adjusted mean all-cause costs for patients with less than one month to triple therapy were estimated to be $31,027 ($28,418–$33,635), compared to $38,415 ($33,213–$44,114) for patients with a 12-month delay. Each 30-day delay of triple therapy was also associated with a significant increase in COPD-related costs of 2.1%, for an average monthly increase of $178 ($170-$186) per patient. Adjusted mean COPD-related costs for patients with less than one month to triple therapy were estimated to be $7535 ($7116–$7595), compared to $9671 ($8642–$10,802) for patients with a 12-month delay.
Discussion
To our knowledge, this study is the first to describe patient characteristics associated with both delayed and very delayed initiation of triple therapy after two moderate or one severe COPD exacerbation. Patients who did not receive triple therapy promptly after their index exacerbation had a greater comorbidity burden than patients with prompt initiation of triple therapy. Patients with delayed or very delayed triple therapy also showed evidence of more severe disease, such as greater use of maintenance treatments, including rescue medications, and more frequent pulmonologist visits in the year before their index exacerbation. Though prior studies have described prompt (≤30 days) and delayed (31–180 days) initiators of triple therapy,16,24 this study shows that patients who delay triple therapy for >6 months to 1 year carry an even greater comorbidity burden and underlying disease severity, thus highlighting a population of very high-risk patients who may not be receiving optimal care. Patients with delayed or very delayed triple therapy were more likely than prompt initiators to have baseline evidence of every comorbidity examined, including some that may be expected to require substantial attention from providers, such as diabetes, heart failure, and neurological disorders. It is possible that COPD is deprioritized by healthcare providers when patients present with multiple other acute and/or chronic comorbidities. Additionally, the observed descriptive association between disease severity and delayed/very delayed triple therapy may be confounded by other factors not examined. For example, differences in provider characteristics between patients with prompt and delayed/very delayed triple therapy may be of interest for future studies given that delayed/very delayed patients appear to be receiving more medications and seeing pulmonologists more frequently, thus suggesting that some providers may be late in recognizing the need for treatment escalation, or that patients may be hesitant to change their treatments.
Patients with delayed or very delayed triple therapy were more likely than prompt initiators to be female and covered by Medicaid insurance. About 37% of delayed and 43% of very delayed patients had Medicaid, compared to 31% of prompt patients. This difference may point to a number of socioeconomic factors and/or state-level coverage and reimbursement policies that could negatively impact access and adherence to timely treatment following an exacerbation. Though examination of such factors is outside the scope of this study, inequalities in healthcare access and outcomes among COPD patients based on socioeconomic status and other demographics should be acknowledged and addressed.
The current findings are consistent with prior studies showing lower exacerbation risk and healthcare costs, including prescription costs, among patients with prompt vs delayed initiation of any maintenance therapy after a COPD exacerbation, though few have specifically examined delayed triple therapy.16,24 This is also one of few studies to examine the effects of 30-day increments of delayed triple therapy, as most earlier studies simply dichotomized patients into “prompt” and “delayed” categories. Using 30-day increments, this study demonstrates that longer time to triple therapy after a recent history of exacerbations resulted in greater odds of experiencing any subsequent exacerbation event, experiencing a severe event, and having a greater number of total events in the subsequent year. Each 30-day delay of triple therapy also increases healthcare utilization and costs after the index event. Since the definitions of “prompt” and “delayed” treatment employed in a research context may not always translate adequately to real-world practice, demonstrating the incremental effect of time to triple therapy on clinical and economic outcomes offers a more useful way to understand and estimate the risks associated with delaying triple therapy.
While earlier initiation of triple therapy was associated with lower risk of future exacerbations, it is likely that the delay of triple therapy resulted in avoidable exacerbations and further lung function decline in some patients.18,25 Future studies are warranted to examine the association of delayed and very delayed triple therapy with lung function decline, disease progression, and the risk of exacerbations after triple therapy initiation.
This study also showed that patients who delayed triple therapy used more short-acting “rescue” medication after their index exacerbation, suggesting that they experienced more symptoms. These patients may not be fully reporting their symptoms to their provider, and/or some providers may fail to recognize these symptomatic patients, thus resulting in the delay of necessary escalation of treatment.
Finally, this analysis included patients with a history of moderate exacerbations, including non-ED outpatient visits, rather than only ED visits or inpatient admissions. In the current study, patients with ≥2 moderate exacerbations in a year were more likely to have delayed/very delayed triple therapy (74% vs 56%), and they were more likely to have ≥1 post-index exacerbation (80% vs 67%), compared to patients with a severe exacerbation requiring hospitalization. This suggests that when a patient experiences an exacerbation that does not require hospitalization their treatment is not adjusted appropriately. This lack of timely treatment escalation may lead to further exacerbations and disease progression.
Limitations
The results of this study should be considered in the context of some limitations. No direct measures of disease severity are available in the MarketScan Databases; the definition of moderate vs severe exacerbations was limited to what is captured in claims (ie, diagnoses, healthcare settings). There is potential for misclassification of disease status, study outcomes, and covariates since claims data are subject to coding limitations. Medication usage was based on filled outpatient prescriptions; patients were assumed to take the medications as prescribed, though adherence and persistence were not assessed. Medications received as samples from physicians, inpatient medications, and prescriptions paid for exclusively out-of-pocket by patients are not captured. It should also be noted that no standard definition for open triple therapy has been applied across prior studies, so our requirement of a minimum number of overlapping days of supply was developed to minimize risk of misclassification of patients who were switching between individual triple therapy components rather than truly initiating triple therapy. This study was limited to patients with commercial, Medicare, or Medicaid insurance; results may not be generalizable to uninsured patients or those with other insurance. Patients who died or disenrolled <12 months after their index exacerbation were excluded and may be systematically different from patients who met enrollment criteria.
All cohort comparisons of patients with prompt vs delayed vs very delayed triple therapy are subject to confounding by indication. A physician may provide a different level of counseling to patients with more severe exacerbations and symptoms, and those patients may be more likely to fill their medication, fill it sooner, and/or use it regularly. Multivariable regression addressed this bias to some extent, as the type of index exacerbation (moderate vs severe) and proxies for baseline disease severity (eg, medication usage, pulmonologist visits) were included in the models. Given that the presence and timing of triple therapy initiation was based on claims for filled outpatient prescriptions, we did not assess the clinical or economic outcomes of patients who did not fill any prescriptions for triple therapy after their index exacerbation. It is possible that some patients were prescribed triple therapy but failed to fill those prescriptions. It is therefore important that patient education include the importance of adhering to prescribed treatments, as well as other factors important for preventing exacerbations, such as proper inhaler technique and lifestyle modifications.
Given the index treatment window in this study (January 2010 to March 2019), and the timing of closed triple therapy approval in the US (September 2017), only about 3% of study patients received closed triple therapy as their index treatment; thus, our ability to compare outcomes between open vs closed triple therapy initiators was limited. Such comparisons should be considered for future analysis. Future studies are also warranted to compare outcomes between patients escalating to triple therapy from dual therapy vs monotherapy vs no prior maintenance treatment.
Healthy adherer bias may also be present, as patients following their doctors’ recommendations and promptly filling a prescription may be more likely to follow other important behaviors for COPD (eg, not smoking). Multivariable modeling attempted to mitigate this bias by controlling for use of other medications and baseline tobacco use, though other health behaviors cannot be measured in claims data.
Conclusion
Prompt initiation of triple therapy decreases risk of future exacerbations and is associated with lower all-cause and COPD-related healthcare utilization and costs, including lower prescription drug costs. In addition to care coordination and patient education, timely consideration of triple therapy after a single severe exacerbation or two moderate exacerbations could decrease overall patient morbidity and lessen the economic burden of COPD.
Acknowledgments
JT and KAE had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Programming and statistical services were provided by Helen Varker, Diana Stetsovsky, and David Smith of IBM Watson Health.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
JT was employed by IBM Watson Health at the time of the study, and KAE is employed by IBM Watson Health, which received funding from AstraZeneca to conduct this study. MP, AS, NF, and SP are employed by AstraZeneca. DRT, EP, and CS are paid consultants of AstraZeneca. DRT reports personal fees from Monument Analytics, outside the submitted work. CS reports personal fees from GlaxoSmithKline; grants from NuVaira, CSA Medical, Grifols, Pulmonx, and AstraZeneca, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Mannino D, Buist A. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(7589):765–773. doi:10.1016/S0140-6736(07)61380-4
2. National Center for Health Statistics. Percentage of COPD, emphysema, or chronic bronchitis for adults aged 18 and over. United States: National Health Interview Survey; 2019.
3. Centers for Disease Control and Prevention. Behavioral risk factor surveillance system: web enabled analysis tool; 2019.
4. Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi:10.1164/rccm.201204-0596PP
5. Foster TS, Miller JD, Marton JP, Caloyeras JP, Russell MW, Menzin J. Assessment of the economic burden of COPD in the US: a review and synthesis of the literature. COPD. 2006;3(4):211–218. doi:10.1080/15412550601009396
6. Schwab P, Dhamane AD, Hopson SD, et al. Impact of comorbid conditions in COPD patients on health care resource utilization and costs in a predominantly medicare population. Int J Chron Obstruct Pulmon Dis. 2017;12:735–744. doi:10.2147/COPD.S112256
7. Dalal AA, Christensen L, Liu F, Riedel AA. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chron Obstruct Pulmon Dis. 2010;5:341–349. doi:10.2147/COPD.S13771
8. Zafari Z, Li S, Eakin MN, Bellanger M, Reed RM. Projecting long-term health and economic burden of COPD in the United States. CHEST. 2021;159(4):1400–1410. doi:10.1016/j.chest.2020.09.255
9. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease; 2021.
10. Baker CL, Zou KH, Su J. Long-acting bronchodilator use after hospitalization for COPD: an observational study of health insurance claims data. Int J Chron Obstruct Pulmon Dis. 2014;9:431–439. doi:10.2147/COPD.S59322
11. Coutinho AD, Lokhandwala T, Boggs RL, et al. Prompt initiation of maintenance treatment following a COPD exacerbation: outcomes in a large insured population. Int J Chron Obstruct Pulmon Dis. 2016;11:1223–1231. doi:10.2147/COPD.S102570
12. Dalal AA, Shah M, D’Souza AO, Crater GD. Rehospitalization risks and outcomes in COPD patients receiving maintenance pharmacotherapy. Respir Med. 2012;106(6):829–837. doi:10.1016/j.rmed.2011.11.012
13. Dalal AA, Shah MB, D’Souza AO, Dhamane AD, Crater GD. Outcomes associated with timing of maintenance treatment for COPD exacerbation. Am J Manag Care. 2012;18(9):e338–e345.
14. Dalal AA, Shah MB, D’Souza AO, Lunacsek OE, Nagar SP, Crater GD. Observational study of the outcomes and costs of initiating maintenance therapies in patients with moderate exacerbations of COPD. Respir Res. 2012;13:41. doi:10.1186/1465-9921-13-41
15. Buikema AR, Brekke L, Anderson A, et al. The effect of delaying initiation of umeclidinium/vilanterol in patients with COPD: an observational administrative claims database analysis using marginal structural models. Multidiscip Respir Med. 2018;13(38). doi:10.1186/s40248-018-0151-6
16. Mainar AS, Huerta A, Artieda RN, Monso E, Landis SH, Ismaila AS. Economic impact of delaying initiation with multiple-inhaler maintenance triple therapy in Spanish patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulm Dis. 2019;14:2121–2129. doi:10.2147/COPD.S211854
17. Demeyer H, Costilla-Frias M, Louvaris Z, et al. Both moderate and severe exacerbations accelerate physical activity decline in COPD patients. Eur Respir J. 2018;51(1):1702110. doi:10.1183/13993003.02110-2017
18. Halpin DMG, Decramer M, Celli BR, Mueller A, Metzdorf N, Tashkin DP. Effect of a single exacerbation on decline in lung function in COPD. Respir Med. 2017;128:85–91. doi:10.1016/j.rmed.2017.04.013
19. Sansbury L, Lipson DA, Bains C, Anley G, Ismaila A, Quasny H. The unmet need of moderate exacerbations among chronic obstructive pulmonary disease (COPD) patients who initiated inhaled maintenance therapy in United Kingdom (UK) general practice. Am J Respir Crit Care Med. 2020;201:A3305.
20. Agency for Healthcare Research and Quality. Prevention quality indicator #5 (PQI #5): chronic obstructive pulmonary disease (COPD) or asthma in older adults, admission rate. Available from: https://qualityindicators.ahrq.gov.
21. Centers for Medicare and Medicaid Services. ACO #9 – prevention quality indicator (PQI): ambulatory care sensitive conditions: admissions for chronic obstructive pulmonary disease (COPD) or asthma in older adults. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/ACO-9.pdf.
22. US Bureau of Labor Statistics. Measuring price change in the CPI: medical care; 2020. Available from: https://www.bls.gov/cpi/factsheets/medical-care.htm.
23. Agency for Healthcare Research and Quality. Creation of elixhauser comorbidity index scores, comorbidity index, version 1.0. Available from: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comindex2012-2015.txt.
24. Bogart M, Glassberg MB, Reinsch T, Stanford RH. Impact of prompt versus delayed initiation of triple therapy post COPD exacerbation in a US-managed care setting. Respir Med. 2018;145:138–144. doi:10.1016/j.rmed.2018.10.013
25. Singh D, Fabbri LM, Vezzoli S, Petruzzelli S, Papi A. Extrafine triple therapy delays COPD clinically important deterioration vs ICS/LABA, LAMA, or LABA/LAMA. Int J Chron Obstruct Pulm Dis. 2019;14:531–546. doi:10.2147/COPD.S196383
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.