Back to Journals » Infection and Drug Resistance » Volume 16
Prevalent Dominant Acinetobacter baumannii ST191/195/208 Strains in Bloodstream Infections Have High Drug Resistance and Mortality
Authors Niu T, Guo L, Kong X, He F, Ru C, Xiao Y
Received 18 January 2023
Accepted for publication 16 March 2023
Published 24 April 2023 Volume 2023:16 Pages 2417—2427
DOI https://doi.org/10.2147/IDR.S403604
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Tianshui Niu,1,2,* Lihua Guo,2,* Xiaoyang Kong,2,* Fei He,1 Chuhui Ru,1 Yonghong Xiao2
1Department of Respiratory and Critical Care Medicine, Affiliated Hangzhou Chest Hospital, Zhejiang University School of Medicine, Hangzhou, 310058, People’s Republic of China; 2State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, The First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, Zhejiang, 310003, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yonghong Xiao, State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, National Clinical Research Center for Infectious Diseases, Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, The First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, Zhejiang, 310003, People’s Republic of China, Tel/Fax +86 571 87236421, Email [email protected]
Background: Different sequence types of Acinetobacter baumannii (AB) have their own epidemiological characteristics, drug resistance, and toxicity.
Methods: AB bloodstream infection (BSI) in the First Affiliated Hospital of Medical College of Zhejiang University from January 2012 to December 2017 were classified by multilocus sequence typing. Clinical data of patients were retrospectively analyzed, drug resistance and toxicity were respectively studied by drug sensitivity and complement killing tests.
Results: 247 unduplicated AB strains were collected, and ST191/195/208, the main epidemic dominant strain, accounted for 70.9%. Patients with ST191/195/208 on infection had higher white blood cell (10.8 vs 8.9, p = 0.004), neutrophil% (89.5 vs 86.9, p = 0.005), neutrophil count (9.5 vs 7.1, p = 0.021), D-dimer (6.7 vs 3.8, p = 0.000), total bilirubin (27.0 vs 21.5, p = 0.038), pronatriuretic peptide (324 vs 164, p = 0.042), C-reactive protein (82.5 vs 56.3, p = 0.048), clinical pulmonary infection score (CPIS; 7.33 ± 2.30 vs 6.50 ± 2.72, p = 0.045), and acute physiology and chronic health evaluation-II (APACHE-II; 19.620 ± 5.1850 vs 17.648 ± 6.1251, p = 0.011). Patients with ST191/195/208 had more complications, including pulmonary infection (p = 0.041), septic shock (p = 0.009), and multiple organ failure (p = 0.019). Patients with ST191/195/208 had higher 3 day mortality (24.6% vs 13.9%, p = 0.043), 14 day mortality (46.8% vs 26.8%, p = 0.003), and 28 day mortality (55.0% vs 32.4%, p = 0.001). ST191/195/208 strains had higher drug resistance to most antibiotics, and higher survival rate at 90% normal serum concentration (p < 0.001).
Conclusion: ST191/195/208 strains predominate in the hospital and prevails in patients with severe infections with increased multidrug antimicrobial resistance and excessive mortality compared to any other AB stains.
Keywords: Acinetobacter baumannii, bloodstream infection, MLST, mortality, toxicity
Introduction
Acinetobacter baumannii (AB) is one of the most common pathogens causing hospital-acquired infections, some of which can prove fatal.1 AB was the most common pathogen in bloodstream infections (BSIs) acquired in hospitals in a multicenter cohort study conducted across 24 countries.2 According to data from the China Bacterial Resistance Monitoring Network (CHINET) from 2019 to 2020, AB accounted for 6.9% of all isolated strains.3 Carbapenem antibiotics are the main drugs for treating AB infections. However, due to the widespread use of these antibiotics, the resistance rate of AB to carbapenem antibiotics has increased rapidly.4 Globally, ~45% of AB isolates are resistant to carbapenems, with a resistance rate almost four times higher than that of other Gram-negative pathogens.5 The mortality of patients infected with carbapenem -resistant AB (CRAB) can be as high as 29–63%.6,7 Therefore, in 2017, the World Health Organization classified CRAB as a class of pathogens that pose a serious threat to global health, that require continuous public health surveillance and prevention, and for which priority should be given to the research and development of new antimicrobial therapies.8
Unlike Escherichia coli and Klebsiella pneumoniae, AB are considered low-virulent strains, but in recent years, reports on invasive AB with high virulence have emerged. Jacobs et al reported that for the highly virulent strain AB5075, in Galleria mellonella infection and mouse pneumonia models, the survival rate of infected animals was always <25%, much lower than for other strains.9 The highly virulent strain LAC-4 showed rapid replication 24 h after pulmonary inoculation, resulting in significant extrapulmonary dissemination and severe bacteremia. Moreover, all mice died within 48 h after inoculation with 108 colony-forming units (CFU)/mL, demonstrating strong toxicity.10 Therefore, it is necessary to reassess the toxicity of AB to develop more effective treatments.
Multilocus sequence analysis (MLST) is widely used in epidemiological studies of bacteria, and data show that clonal complex 92 (CC92) is the most widely distributed AB worldwide.11 A number of domestic studies have also shown that CC92 strains account for >80% of isolates.12–14 Their strong drug resistance and invasiveness make studying AB important, especially drug resistance, toxicity, and molecular mechanisms. Using AB isolated from blood, we analyzed the epidemic strain types of AB in eastern China and assessed the clinical characteristics, drug resistance, and toxicity to provide a basis for clinical treatment.
Materials and Methods
Collection of Clinical Data and Strains
AB bloodstream infection (AB-BSI) in the First Affiliated Hospital of Zhejiang University from January 2012 to December 2019 was assessed according to the CDC diagnostic criteria for BSI.15 This study was approved by the Ethics Committee of the First Affiliated Hospital of Zhejiang University (batch number: 2017–699). (1) AB strains were isolated from blood cultures one or more times, and where a patient’s results were positive many times, data from the first positive result were used. (2) All patients showed clinical manifestations such as body temperature >38.0°C or body temperature <36.0°C, chills, hypotension, or systemic poisoning symptoms.
Clinical data collected included demographic parameters, patient comorbidities, vital signs, laboratory-reported data at admission and at the time of infection, acute physiology and chronic health evaluation (APACHE-II) score, clinical pulmonary infection score (CPIS), bacteriology, and antibiotic use prior to BSI. These data were acquired from the Hospital Information System (HIS). To more accurately assess the impact of bacterial infection on the functions of various organs in patients, we chose to collect laboratory test data at the time of admission and the time of positive culture results. Strains were isolated from non-repetitive AB strains cultured from the blood of patients diagnosed with BSIs. The flow chart of this study is shown in Figure 1.
Microbiological Studies: MLST Typing
AB isolated from blood cultures of patients included in the clinical analysis were collected for MLST typing. MLST was performed using Oxford typing criteria. Seven housekeeping genes (gltA, gyrB, gdhB, recA, cpn60, GPI, and rpoD) of AB were amplified by PCR, using AB DNA as a template, and sequenced. Typing was performed using the MLST database (http://pubmlst.org/abaumannii). The minimal inhibitory concentration (MIC) of each antibiotic was determined by the broth microdilution method accord to EUCAST V7. 1 (http://clincalc.com/eucast/).
Toxicity Testing of Bacteria
For in vitro complement killing tests, serum from healthy BALB/C mice was collected and centrifuged to obtain the upper serum (normal serum). This was incubated in a water bath at 56°C for 30 min to inactivate complement (heated-inactivated serum). Twelve strains of ST191/195/208 and five strains of other types were randomly selected according to the proportion, and freshly cultured bacterial solution was diluted to 2×106CFU/mL. Next, 180 μL of normal rat serum and 20 μL of heat-inactivated serum were respectively taken, mixed with bacterial suspension, and incubated in a water bath at 37°C for 1 h. Bacterial solution was diluted 100-fold and plated for colony counting. The formula for calculating the survival rate of bacteria was as follows: bacterial survival rate = (number of colonies in normal serum / number of colonies in inactivated serum) × 100%.
Statistical Methods
SPSS 22.0 was used to analyze data. Categorical variable comparisons were made using t-test or Wilcoxon rank-sum test, and comparisons were made using chi-square or Fisher’s exact tests with continuous variables. We used the Kaplan-Meier method to estimate the survival distribution curve of patients infected with different types of AB, and p < 0.05 was considered statistically significant. For statistical analysis of in vitro complement killing test results, values are presented as means ± standard deviation (SD) from three independent experiments, and p < 0.05 was considered statistically significant.
Results
Epidemiology of AB
A total of 247 unduplicated strains of AB-BSI were collected from 2012 to 2017, and the MLST type isolation rates of each strain were ST191 = 21.5%, ST195 = 40.1%, ST208 = 9.3%, and the other ST strains = 29.1% (Table 1). We found that AB ST191, ST195, and ST208 isolated from BSI patients from 2012 to 2017 belonged to the CC92 type, and they were the clinically prevalent dominant strains, accounting for 70.9% of all isolated strains. In 2012, ST191/195/208 accounting for 52.2%, while in 2013–2017, ST191/195/208 accounting for over 70% of all isolated strains (Figure 2).
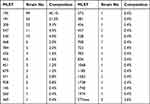 |
Table 1 Multilocus Sequence Type (MLST) Classification of Isolated Strains |
Clinical Characteristics of AB Infection
The clinical characteristics of 247 patients with AB infection were analyzed (Table 2), and there were no differences in gender between the two groups. Patients with ST 191/195/208 were younger than those with other sequence types (STs) (p = 0.02). There was no significant difference between the two groups in the length of hospital stay before BSI and total hospital stay. Compared with other ST strains, patients with ST191/195/208 tended to use two or more antibiotic therapies (p = 0.051) and carbapenems (p = 0.054), but differences were not significant. Use of cephalosporins (p = 0.034) and quinolones (p = 0.045) was less frequent before AB-BSI.
 |
Table 2 Clinical Characteristics of Patients with Acinetobacter baumannii Blood Infection |
We also collected the test indicators of patients on admission and on infection, which can reflect the damage status of bacteria for various organs. At the time of admission, only the proportion of neutrophils in patients with ST191/195/208 was significantly higher than that in patients with other ST strains. At the time of infection, as shown in Table 2, laboratory markers of sepsis and multiple organ functional impairment are worse in patient with the ST191/195/208 than patients with other AB strains, such as white blood cell count, neutrophil percentage, neutrophil count, D-dimer, total bilirubin, pronatriuretic peptide, C-reactive protein, CPIS, and APACHE-II.
After AB-BSI, patients with ST191/195/208 had a higher frequency of complications than patients with other ST strains, including pulmonary infection (p = 0.041), septic shock (p = 0.009), and multiple organ failure (p = 0.019). Moreover, APACHE-II (p = 0.011) was higher in ST191/195/208 patients, and the 3 day mortality (24.6% vs 13.9%, p = 0.043), 14 day mortality (46.8% vs 26.8%, p = 0.003), and 28 day mortality (55.0% vs 32.4%, p = 0.001) of ST191/195/208 patients were higher and significantly different (Table 3). Analysis of Kaplan-Meier survival curves showed that 28 day mortality of patients with ST191/195/208 was higher than that of patients with other strains (Figure 3).
 |
Table 3 Comparison of Drug Resistance Rate Between ST191/195/208 Strains and Other ST Strains |
 |
Figure 1 A flow chart of the study. |
Drug Susceptibility results of AB
Compared with other ST strains, ST191/195/208 strains were more resistant to most antibiotics, and the resistance rates to cefepime, ceftazidime, ciprofloxacin, gentamicin, tobramycin, ampicillin/sulbactam, and imipenem/cilastatin were significantly different from those of other ST strains. The drug resistance rate of ST191/195/208 strains to cefepime, ciprofloxacin, imipenem, and piperacillin/tazobactam was >90%, and the drug resistance rate to cefoperazone/sulbactam was 76.0%. There was no significant difference in resistance rates to tigecycline between the two groups (Table 3).
Results of in vitro Complement Killing Tests
Serum complement killing assays were employed to analyze the virulence of each strain type. The results showed that at 90% of the normal serum concentration, the average survival rate of ST191/195/208 strains was 40.56%. However, the average survival rate of other ST strains was only 13.78%, and differences were significant (p < 0.001; Figure 4).
 |
Figure 2 Proportion of ST191195208 in allisolates. |
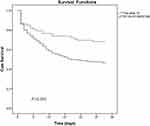 |
Figure 3 Kaplan Meier survival analysis curve to evaluate the mortality of patients infected with ST191/195/208 strains and other ST strains. |
 |
Figure 4 Comparison of complement killing results between ST191/195/208 strains and Other ST strains. |
Discussion
CC92 is the most widely distributed AB clonal complex worldwide, covering Asia, Europe, America, Australia, and other regions.11 In many regions of China, the results showed that ST191, ST195, and ST208 were the three most common STs,12–14 our results consistent with the STs of epidemic strains in other regions, which shows that ST191/195/208 has a wide range of epidemic characteristics and is a type that needs much attention.
We found that ST191/195/208 had high resistance many antibiotics commonly used in the clinic, and the resistance rate was significantly different from other ST strains. This suggests that ST191/195/208 strains are not only widespread but also more resistant than other ST strains. It was found that ST191/195/208 strains had strong drug resistance and carried the bla OXA-23 gene, carried on a plasmid in ST191 and on the chromosome in ST195/208.14 In one multicenter study, 94.4% of ST195 and ST208 strains carried carbapenem-resistant bla OXA-23.15 The gene encoding OXA-23 (bla OXA-23) was first discovered in Scotland and confirmed to be related to carbapenem resistance of AB,16 and it is also the most common gene related to carbapenem resistance in China.17 There are other drug resistance genes such as OXA-66, ADC-25, and TEM-1D in AB.18 Genomic studies on ST195 strains showed that the genomes contain two antibiotic resistance islands, including resistance genes to aminoglycosides, macrolides, carbapenems, tetracyclines, and sulfonamides, as well as genes encoding drug transporters and efflux pumps.19 It was also reported that the transposon carrying the bla OXA-23 resistance gene is duplicated in ST208 and ST191 strains, and there was a linear relationship between the number of gene copies and the MIC for carbapenems, indicating that it was associated with high drug resistance.20 Therefore, ST191/195/208 has unique advantages, including high epidemic potential and high drug resistance in BSI.
Our current study found that the laboratory markers of patients infected with ST191/195/208 strains were significantly higher than those of patients infected with other ST strains. These results indicate that infection with ST 191/195/208 can lead to disruption of coagulation, damage to liver and heart functions, and serious pulmonary infection. This is the first evaluation of the effect of ST191/195/208 infection on the functional status of various organs in patients. Furthermore, mortality at 3, 7, 14, and 28 days after infection with pathogenic bacteria showed that at all stages, the mortality of patients with ST191/195/208 strains was higher than those of patients with other ST strains. According to our preliminary toxicity test results, ST191/195/208 had stronger anticomplement killing ability than other ST strains. In previously reported toxicity tests on G. mellonella, the survival rate when infected with ST191 isolate was similar to that of AB5057 with high virulence, hence ST191 was considered to be a highly virulent strain.21 Studies in southern China showed that the 7 day and 28 day mortality rates of ST195/208 were higher than other types of strains.22 Although the drug resistance rate of ST 191/195/208 was higher than that of other ST strains, carbapenem resistance was not a risk factor for mortality.7,23–25 In other work, the clinical outcome of AB patients was not related to drug resistance of infected strains.26 Therefore, the unique virulence mechanism of ST191/ST195/ST208 strains leads to enhancement of their toxicological effects, thus increasing the mortality rate of patients.
AB infection requires a variety of bacterial virulence factors to work together, and having a special virulence gene can make pathogens more efficient at infecting hosts.27 For example, the LAC-4 strain has 615 potential toxicity-related genes involving transcription activator proteins, Fe2+ transport system proteins, polysaccharide export outer membrane proteins, and many other toxic genes.10 AB5075 also has many toxic factors such as MerR regulator family members, genes encoding type IV pili, Fur family members, heme uptake systems, and heme oxygenases.9 However, there are few reports on the genomics and transcriptomics of ST191/195/208 systems. Genomic studies have found that the virulence factor cap8E, which encodes capsular polysaccharide synthase, is positive in ST191 isolates.28 ST195 and ST208 isolates were found to be positive for biofilm-forming genes such as CSU and Bap, and they also carry PGA and OmpA genes.29,30 ST191/195/208 strain is the dominant type widely prevalent in the clinic and possesses high drug resistance. And high mortality. The more terrible effect is the higher mortality of ST191/195/208 strains after infection. Previous literature reports28–30 and the results of complement killing experiments have preliminarily confirmed that ST195 has higher toxicity, but its high toxicity characteristics need to be further verified in animal models, and its toxicity mechanism also needs further study.
This study has some limitations. It is a retrospective study, and all patients with AB were from a single hospital. Due to differences in prevalent strains, treatment options, and detection methods, the study samples may not be widely representative.
Conclusions
ST191/195/208 strains predominate in the hospital, with increased multidrug antimicrobial resistance and excessive mortality compared to any other STs AB stains. We should continue to monitor the epidemic characteristics of ST191/195/208 strains, and further study the mechanism of its high toxicity and high drug resistance to guide clinical treatment.
Ethics/Copyright
This study complied with the declaration of Helsinki and all methods were performed in accordance with the relevant guidelines and regulations of the Ethics Committee of the First Affiliated Hospital of Zhejiang University (batch number: 2017-699). This study used data collected from patient records while maintaining patient anonymity. Because this study presented no more than minimal risk of harm to patient subjects, the institutional review board approved a waiver of patient informed consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Key Research and Development Program of China (2021YFC2300302); Zhejiang Provincial Natural Science Foundation of China under Grant (LQ21H190001); Medical Science and Technology Project of Zhejiang Province (No.2020KY735). Hangzhou Medical and Health Science and Technology Project (A20210054); Hangzhou Chest Hospital affiliated to Zhejiang University Medical College and Zhejiang University Medical College Joint pre-research project (ZAYY2).
Disclosure
No potential conflict of interest was reported by the authors.
References
1. Decker BK. Too much too soon or too little too late: the challenge of preventing acinetobacter transmissions. Crit Care Med. 2017;45(7):1252–1253. doi:10.1097/CCM.0000000000002418
2. Garnacho-Montero J, Dimopoulos G, Poulakou G, et al. European society of intensive care medicine. task force on management and prevention of acinetobacter baumannii infections in the ICU. Intensive Care Med. 2015;41(12):2057–2075. doi:10.1007/s00134-015-4079-4
3. Chen YB, Ji JR, Ying CQ, et al. BRICS report of 2020: the bacterial composition and antimicrobial resistance profile of clinical isolates from bloodstream infections in China. Chin J Clin Infect Dis. 2021;14(06):413–426. doi:10.3760/cma.j.issn.1674-2397.2021.06.002
4. Onorato L, Macera M, Calò F, et al. The effect of an antimicrobial stewardship programme in two intensive care units of a teaching hospital: an interrupted time series analysis. Clin Microbiol Infect. 2020;26(6):782.e1–782.e6. doi:10.1016/j.cmi.2019.10.021
5. Giammanco A, Calà C, Fasciana T, Dowzicky MJ. Global assessment of the activity of Tigecycline against multidrug-resistant gram-negative pathogens between 2004 and 2014 as part of the tigecycline evaluation and surveillance trial. mSphere. 2017;2(1):e00310–16. doi:10.1128/mSphere.00310-16
6. Nutman A, Glick R, Temkin E, et al. A case-control study to identify predictors of 14-day mortality following carbapenem-resistant Acinetobacter baumannii bacteraemia. Clin Microbiol Infect. 2014;20(12):O1028–1034. doi:10.1111/1469-0691.12716
7. Niu T, Xiao T, Guo L, et al. Retrospective comparative analysis of risk factors and outcomes in patients with carbapenem resistant Acinetobacter baumannii bloodstream infections: cefoperazone–sulbactam associated with resistance and tigecycline increased the mortality. Infect Drug Resist. 2018;26(11):2021–2030. doi:10.2147/IDR.S169432
8. Willyard C. The drug-resistant bacteria that pose the greatest health threats. Nature. 2017;543(7643):15. doi:10.1038/nature.2017.21550
9. Jacobs AC, Thompson MG, Black CC, et al. AB5075, a highly virulent isolate of acinetobacter baumannii, as a model strain for the evaluation of pathogenesis and antimicrobial treatments. MBio. 2014;5(3):e01076–14. doi:10.1128/mBio.01076-14
10. Ou HY, Kuang SN, He XY, et al. Complete genome sequence of hypervirulent and outbreak-associated acinetobacter baumannii strain LAC-4: epidemiology, resistance genetic determinants and potential virulence factors. Sci Rep. 2015;5:8643. doi:10.1038/srep08643
11. Karah N, Sundsfjord A, Towner K, Samuelsen Ø. Insights into the global molecular epidemiology of carbapenem non-susceptible clones of Acinetobacter baumannii. Drug Resist Updat. 2012;15(4):237–247. doi:10.1016/j.drup.2012.06.001
12. Jiang LL, Liang YC, Yao W, Ai JT, Wang X, Zhao ZG. Molecular epidemiology and genetic characterisation of carbapenem-resistant Acinetobacter baumannii isolates from Guangdong Province, South China. J Glob Antimicrob Resist. 2019;17:84–89. doi:10.1016/j.jgar.2018.11.002
13. Jiang MJ, Liu LJ, Ma YH, et al. Molecular epidemiology of multi-drug resistant acinetobacter baumannii Isolated in Shandong, China. Front Microbiol. 2016;7:1687. doi:10.3389/fmicb.2016.01687
14. Ning NZ, Liu X, Bao CM, et al. Molecular epidemiology of blaOXA-23-producing carbapenem-resistant Acinetobacter baumannii in a single institution over a 65-month period in north China. BMC Infect Dis. 2017;17:14. doi:10.1186/s12879-016-2110-1
15. Chen T, Fu Y, Hua X, et al. Acinetobacter baumannii strains isolated from cerebrospinal fluid (CSF) and bloodstream analysed by cgMLST: the dominance of clonal complex CC92 in CSF infections. Int J Antimicrob Agents. 2021;58(4):106404. doi:10.1016/j.ijantimicag.2021.106404
16. Boo TW, Walsh F, Crowley B. First report of OXA-23 carbapenemase in clinical isolates of Acinetobacter species in the Irish Republic. J Antimicrob Chemother. 2006;58:1101–1102. doi:10.1093/jac/dkl345
17. Ruan Z, Chen Y, Jiang Y, et al. Wide distribution of CC92 carbapenem-resistant and OXA-23-producing Acinetobacter baumannii in multiple provinces of China. Int J Antimicrob Agents. 2013;42(4):322–328. doi:10.1016/j.ijantimicag.2013.06.019
18. Lv W, Zhang X, Hou M, Han D, Li Y, Xiong W. Draft genome sequence of an OXA-23, OXA-66, ADC-25 and TEM-1D co-producing Acinetobacter baumannii ST195 isolated from a patient with neonatal pneumonia in China. J Glob Antimicrob Resist. 2019;16:1–3. doi:10.1016/j.jgar.2018.11.008
19. Lean SS, Yeo CC, Suhaili Z, Thong KL. Whole-genome analysis of an extensively drug-resistant clinical isolate of Acinetobacter baumannii AC12: insights into the mechanisms of resistance of an ST195 clone from Malaysia. Int J Antimicrob Agents. 2015;45(2):178–182. doi:10.1016/j.ijantimicag.2014.10.015
20. Yoon EJ, Kim JO, Yang JW, et al. The blaOXA-23-associated transposons in the genome of Acinetobacter spp. represent an epidemiological situation of the species encountering carbapenems. J Antimicrob Chemother. 2017;72(10):2708–2714. doi:10.1093/jac/dkx205
21. Hu L, Shi Y, Xu Q, et al. Capsule thickness, not biofilm formation, gives rise to mucoid acinetobacter baumannii phenotypes that are more prevalent in long-term infections: a study of clinical isolates from a hospital in China. Infect Drug Resist. 2020;13:99–109. doi:10.2147/IDR.S230178
22. Zhou K, Tang X, Wang L, et al. An Emerging Clone (ST457) of Acinetobacter baumannii clonal complex 92 with enhanced virulence and increasing endemicity in South China. Clin Infect Dis. 2018;67(S2):S179–S188. doi:10.1093/cid/ciy691
23. Li YJ, Pan CZ, Fang CQ, et al. Pneumonia caused by extensive drug-resistant Acinetobacter baumannii among hospitalized patients: genetic relationships, risk factors and mortality. BMC Infect Dis. 2017;17(1):371. doi:10.1186/s12879-017-2471-0
24. Yang S, Sun J, Wu X, Zhang L. Determinants of mortality in patients with nosocomial acinetobacter baumannii bacteremia in Southwest China: a five-year case-control study. Can J Infect Dis Med Microbiol. 2018;2018:3150965. doi:10.1155/2018/3150965
25. Brotfain E, Borer A, Koyfman L, et al. Multidrug resistance acinetobacter bacteremia secondary to ventilator-associated pneumonia: risk factors and outcome. J Intensive Care Med. 2017;32(9):528–534. doi:10.1177/0885066616632193
26. Qu JY, Yu RJ, Wang QJ, Feng CL, Lv XJ. Synergistic antibacterial activity of combined antimicrobials and the clinical outcome of patients with carbapenemase-producing acinetobacter baumannii infection. Front Microbiol. 2020;11:541423. doi:10.3389/fmicb.2020.541423
27. Harding CM, Hennon SW, Feldman MF. Uncovering the mechanisms of Acinetobacter baumannii virulence. Nat Rev Microbiol. 2018;16(2):91–102. doi:10.1038/nrmicro.2017.148
28. Casella LG, Weiss A, Pérez-Rueda E, Antonio Ibarra J, Shaw LN. Towards the complete proteinaceous regulome of acinetobacter baumannii. Microb Genom. 2017;3(3):mgen000107. doi:10.1099/mgen.0.000107
29. Bian X, Liu X, Zhang X, et al. Epidemiological and genomic characteristics of Acinetobacter baumannii from different infection sites using comparative genomics. BMC Genomics. 2021;22(1):530. doi:10.1186/s12864-021-07842-5
30. Ali HM, Salem MZM, El-Shikh MS, Megeed AA, Alogaibi YA, Talea IA. Investigation of the virulence factors and molecular characterization of the clonal relations of multidrug-resistant acinetobacter baumannii isolates. J AOAC Int. 2017;100(1):152–158. doi:10.5740/jaoacint.16-0139
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
