Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Prevalence, Patterns and Predictors of Chronic Complications of Diabetes Mellitus at a Large Referral Hospital in Ethiopia: A Prospective Observational Study
Authors Sheleme T , Mamo G , Melaku T , Sahilu T
Received 24 September 2020
Accepted for publication 15 November 2020
Published 11 December 2020 Volume 2020:13 Pages 4909—4918
DOI https://doi.org/10.2147/DMSO.S281992
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Antonio Brunetti
Tadesse Sheleme,1 Girma Mamo,2 Tsegaye Melaku,2 Tamiru Sahilu3
1Department of Pharmacy, College of Health Science, Mettu University, Mettu, Ethiopia; 2School of Pharmacy, Institute of Health, Jimma University, Jimma, Ethiopia; 3Department of Pharmacy, College of Health Science, Assosa University, Assosa, Ethiopia
Correspondence: Tadesse Sheleme
Department of Pharmacy, College of Health Science, Mettu University, P.O. Box: 318, Mettu, Ethiopia
Tel +251 910830835
Email [email protected]
Purpose: Diabetes mellitus complications are responsible for increased disability, morbidity, and mortality. This study aimed to assess prevalence, patterns, and predictors of chronic complications of diabetes among people with diabetes.
Patients and Methods: The study was conducted using a prospective observational study design which was done on people with diabetes attending the ambulatory clinic of Mettu Karl Referral Hospital. The data were collected using a consecutive type of sampling technique from April 15 to August 9, 2019. The data were entered into Epidata manager version 4.4.2. Logistic regression analysis was done to identify predictors of chronic complications of diabetes.
Results: A total of 330 participants were included in this study. The mean age of participants was 49.9± 14.2, and 156 (47.3%) were 41 to 60 years old. About 127 (38.5%) had one or more chronic complications. The predictors of chronic diabetes complications were resident in urban areas [AOR: 1.94; 95% CI: (1.17, 3.20); p = 0.010], duration of diabetes 10 years [AOR: 2.05, 95% CI: (1.21, 3.47); p = 0.007], hypertension [AOR: 4.19; 95% CI: (2.54, 6.91); p < 0.001] and poor glycemic control [AOR: 2.82; 95% CI: (1.53, 5.21); p = 0.001].
Conclusion: Almost two-fifth of the study participants had chronic complications of diabetes. Residents in urban areas, longer duration of diabetes, hypertension and poor glycemic control were predictors of chronic diabetes complications. It is important to achieve good glycemic control and manage comorbid diseases like hypertension to minimize the risk of chronic diabetes complications.
Keywords: diabetes mellitus, chronic complications, Mettu Karl Referral Hospital, Ethiopia
Introduction
Diabetes mellitus (DM) is a chronic disease characterized by metabolic disorder and hyperglycemia. Globally, DM is the most common non-communicable disease and one of the main threats to human health.1 Huge increments in diabetes prevalence have been seen throughout the world, with a current estimation of 463 million people worldwide. The global prevalence of people with diabetes is expected to increase from the current estimate of 463 million to 578 million in 2030 and 700 million in 2045. It is also estimated that 4.7% of adult people are living with diabetes in the African region. The largest increase in the number of people with diabetes is expected in this region by 2045.2,3 A study showed that an estimated 2.6 million people with diabetes are living in Ethiopia.4
An increment in DM prevalence will increase the number of chronic complications of diabetes which affects patients’ quality of life, health services demand and economic costs.2 The chronic complications of DM can be classified into vascular and nonvascular complications. The vascular complications include microvascular and macrovascular complications. Microvascular complications are neuropathy, retinopathy and nephropathy. Macrovascular complications include peripheral vascular disease, coronary artery disease, and cerebrovascular disease. Problems such as gastroparesis, skin changes, and sexual dysfunction due to diabetes are classified as nonvascular complications.1,5
A multinational study which included 28 countries showed that macrovascular complications and microvascular complications were 27.2% and 53.5%, respectively.6 A study conducted in China identified that among patients with diabetes, 76.4% reported at least one kind of complication.7 A study reported that neuropathy (25%), retinopathy (32%) and nephropathy (23%) were common chronic complications of diabetes in Spain.8 The ocular complications of diabetes were found in 14–18% and signs of neuropathy were present in up to 48% of diabetics in sub-Saharan Africa.9 Diabetic foot ulcers developed in 10–15% of people with diabetes at some stage of their lives and almost 50% of all DM-related admissions are due to diabetic foot problems in sub-Saharan Africa.10 A previous study in Ethiopia identified that 29.4% of people with diabetes have experienced at least one chronic complication. The study also expressed that peripheral neuropathy (20.5%), retinopathy (19.8%) and chronic kidney disease (4.6%) were the three most common chronic complications.11
It is identified that poor blood glucose control, diabetes duration, age, hypertension, obesity, smoking, dyslipidemia, and genetics are important risk factors for most diabetic complications.12 A systematic review in Ethiopia explored that gender, longer diabetes duration, poor glycemic control, negative attitude of DM, poor adherence to diabetic medications, and poor knowledge about the disease and its management are common risk factors for diabetic complications.13
Although treatment and attention for DM has become better, complications of DM are important impediments to glycemic control for most people with diabetes and result in increased morbidity and early mortality.14 Diabetes complications are responsible for increased disability, morbidity, and mortality. Diabetes complications are also a threat to the global economy.15 Treating diabetes-related complications costs more than controlling the disease.1 In the United States (US), the inpatient care for management of DM complications cost nearly 40% of the total cost of DM.16 An increased hospital mortality has been associated with diabetic foot ulcers and diabetic cardiovascular disease in Ethiopia.17
People with diabetes have more outpatient department visits, and require more long-term care than non-diabetic patients.18 Assessing the prevalence of diabetes complications is important to take necessary measures like preparing preventive and treatment strategies to minimize the impact of the complications. The identification of the prevalence of diabetes complications and factors contributing to its occurrence are also important for the modification of practices and policies in the management of diabetes. Thus, it is imperative to study about diabetes complications and its associated factors from time to time in order to detect the changing trends to plan out the course of action. However, there was no study conducted to determine diabetes-related complications and associated factors in Mettu Karl Referral Hospital. Therefore, this study aimed to determine diabetes-related chronic complications and contributing factors.
Patients and Methods
Study Area and Period
This study was done at the ambulatory clinic of Mettu Karl Referral Hospital. The hospital is located in Mettu town, Oromia Region, Southwest Ethiopia, 600 km from Addis Ababa, Ethiopia’s capital city. It provides services to 2.5 million people from Ilu Aba Bor Zone, Gambella Region and Southern People Region. The hospital health services cover outpatient department, inpatient services, critical care and emergency service. Approximately 13,453 inpatient and 80,000 outpatient attendances obtain health services from this hospital per year. The study was done from April 15 to August 9, 2019.
Study Design and Population
Prospective observational study design was used to conduct this study. The source population was all people with diabetes attending the ambulatory clinic of Mettu Karl Referral Hospital. The study population was all an adult diabetes patient population who visited the hospital during the data collection period and fulfilled the inclusion criteria. Since this study was part of a study previously conducted by Sheleme et al,19 the study population share a similarity.
Eligibility Criteria
Participants included in the study were patients with type 1 and type 2 diabetes whose ages were 18 years or above and who have already started antidiabetes medications. The one-month follow-up schedule for data collection was used to avoid repetition of the cases. Patients who were not willing to participate in the study and who were not fasting were excluded from the study.
Sample Size Determination and Sampling Technique
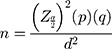
This work was done alongside our recently published paper on glycemic control. Originally, the study had glycemic control and diabetes complications as primary outcomes. The sample size calculation was done considering both outcomes and “glycemic control” gave us the maximum sample size. Since there was no study done to assess glycemic control status or diabetes complications in our study area, the proportion of outcomes were taken from a study conducted in a nearby area. The proportion of patients with diabetes with poorly controlled blood glucose was 59.4% which is reported from an earlier study conducted at the Jimma university medical center among the diabetes patient population.20 The required sample size was estimated using the single population proportion formula.
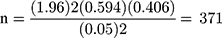
Where: n = the desirable sample size, Zα/2 = 1.96, p = 0.594, d = 0.05, and q = 1-p
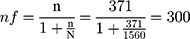
There were 1560 people with diabetes on follow-up at Mettu Karl Referral Hospital. A finite correction formula was applied to obtain final sample size (nf).
10% was added to cater for non-response, 300+30 = 330.
A consecutive type of sampling technique was used to collect data from the diabetes patient population which fulfilled the inclusion criteria.
Study Variables
The presence of chronic complications of diabetes was a dependent variable. The independent variables were socio-demographic factors (age, sex, educational status, residence, income, occupation and body mass index), disease-related variables (DM duration, family history of DM, hypertension and glycemic control), self-monitoring of blood glucose (SMBG) and medication-related variables (type of antidiabetes medication).
Data Collection Tool and Procedure
The data were collected using a structured questionnaire and abstraction format. The questionnaire and data extraction format contains details of patient, investigations, medications, and clinical characteristics. The questionnaire was translated into the local languages Afan Oromo and Amharic. The data collectors were healthcare workers.
Fasting blood glucose (FBG) was measured at baseline, month-1, month-2 and month-3 of the study period. The baseline FBG was obtained on the first day the patient visited hospital during the study period. The month-1 FBG was taken on next month from the initial visit in the study period. The month-2 and month-3 FBG were obtained on the second and third month from the initial visit of the study period, respectively. The average of FBG measurements of three consecutive months was taken to categorize patients’ blood glucose as controlled or uncontrolled.
Weights were measured by an Adult Scale Astor with the patient having light clothes and bare feet or with stockings. Heights were measured using a standard height board. The patient’s body mass index (BMI) was calculated as weight in kg divided by height in meters squared. BMI was categorized as underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2) and obese (≥30.0 kg/m2).21
Diabetes-Related Complications Determination
The primary outcome was chronic complications of diabetes. The identified chronic complications were retinopathy, neuropathy, nephropathy, ischemic heart disease, stroke, impotency and foot ulcer. Screening for diabetic complications was performed by a physician. The complications were assessed at baseline and then every month for the 3 months of the study period.
The presence of neuropathy was assessed by orally asking the patients for numbness, burning, tingling, and paraesthesia in the extremities and confirmed by touch sensation detection using a 10-g monofilament test. The 10-g monofilament was first demonstrated to the patient on a proximal site and the patient then closed his/her eyes while being tested. The monofilament was placed at 10 sites on each foot of the patient and held against the skin for approximately 2 seconds. The patient was asked to respond yes or no to whether the filament was felt. Less than seven correct responses indicated reduced sensation, and no correct responses indicated absent sensation. The test was done by a general practitioner.
Retinopathy was diagnosed by an ophthalmologist and was confirmed by fundus examination. Nephropathy was assessed using renal function test and also other features like the presence of protein in the urine. A 10 mL sample of morning urine was obtained from each patient for determination of urine protein. The presence of protein in urine (proteinuria) was assessed by urine dipstick analyses. A 5 mL blood sample was obtained for the determination of serum creatinine concentration. An enzymatic colorimetric test method was used to measure serum creatinine and analysis was done on a fully automated analyzer HumaStar 200. The estimated glomerular filtration rate (eGFR) for each patient was then estimated from the serum creatinine, using the Modification of Diet in Renal Disease (MDRD) formula. The laboratory measurements were performed by the laboratory technologists and the diagnosis of diabetic nephropathy was done by a general practitioner.
There were no new diagnoses of ischemic heart disease and stroke during the follow-up of the study period and they were taken if the patients had such problems at the time of the study started. Diabetic foot ulcer was diagnosed if the patient had a current or previous history of diabetic foot ulcers. Impotency was evaluated by the sexual history of the patient.
Data Quality Assurance and Management
The principal investigator provided training for data collectors and supervisors. The pretest was done on 17 (5%) diabetic patients at the ambulatory clinic of Jimma University Medical Center to check the consistency, applicability and understandability of the questionnaire. Collected data were evaluated for completeness, accuracy, clarity and consistency by the principal investigator on an everyday basis.
Data Processing and Statistical Analysis
Before data entry, it was edited and coded properly by the principal investigator. Then it was entered into Epidata manager version 4.4.2 and double entry verification was made. Statistical Package for Social Science (SPSS) version 24.0 was used for analysis. Bivariate logistic regression analysis was used to find factors associated with chronic diabetes complications. Factors found significant at p-value < 0.25 in bivariate analysis were included in multivariate logistic regression analysis. Multivariate logistic regression analysis was conducted to identify predictors of chronic diabetes complications. Statistical significance was declared at p-value less than 0.05.
Operational Definitions
Glycemic control status was classified as good glycemic control if an average FBG at three months was found within the range of 80–130 mg/dl. If it was greater than 130 mg/dl, it was classified as poor glycemic control.22
Fasting blood glucose is a blood glucose measured after at least 8 hours of fasting.22
Self-monitoring of blood glucose: If a diabetic patient performed self-monitoring of blood glucose at his/her home for more than 3 days during the last seven days.
Chronic diabetes complications: If a diabetic patient has currently or a history of at least one known chronic complication of diabetes.23
Results
Socio-Demographic and Clinical Characteristics of the Study Participants
A total of 330 study participants were included in this study. One hundred ninety eight (60.0%) participants were males. The mean age of respondents was 49.9±14.2 and 156 (47.3%) were 41 to 60 years old. The educational status of the study population showed that 114 (34.5%) had attained primary school education. In terms of occupation, 113 (34.2%) study participants were farmers. More than half (53.6%) of respondents were urban residents. The BMI of the study participants revealed that overweight and obese patients were 17.9% and 12.7%, respectively. The mean ± SD diabetes duration of participants was 7.8 ± 5.9 years and 30.9% had a duration of 10 or more years. On assessing the family history of diabetes, 28.8% reported having a positive family history of diabetes. The presence of hypertension was significant among study participants and identified in 39.1% (Table 1).
 |
Table 1 Socio-Demographic and Clinical Characteristics of Study Participants at Mettu Karl Referral Hospital, Southwest Ethiopia, 2019 |
Medication Usage Pattern Among Study Population
About 45.5% of study participants were on oral antidiabetes medications. Of the patients on oral antidiabetes medications, 27.6% were on a metformin and glibenclamide combination, 15.2% were on metformin monotherapy and 2.7% were on glibenclamide monotherapy. Insulin injection was given to 40.3% of the study patients. The combination of oral antidiabetes medications and insulin were prescribed in 14.2% of the study patients (Table 2).
 |
Table 2 Antidiabetes Medication Usage Pattern Among Study Participants at Mettu Karl Referral Hospital, Southwest Ethiopia, 2019 |
Prevalence and Patterns of Chronic Diabetes Complications Among Study Participants
Overall, 127 (38.5%) study participants had one or more chronic diabetes complication. The prevalence of chronic complications was higher among type 2 diabetic patents than type 1 diabetic patents. It was 72.4% in type 2 diabetic and 27.6% in type 1 diabetic patients. Microvascular complications were the most common chronic complication identified. Diabetic neuropathy was the most commonly identified microvascular complication which counted for 23.9%. Retinopathy and nephropathy was found in 12.4% and 9.7%, respectively. Macrovascular complications observed were ischemic heart disease found in 2.1% and stroke found in 0.61%. About 2.1% of study participants experienced sexual dysfunction. Diabetic foot ulcer was identified in 0.61% of participants (Table 3).
 |
Table 3 Type of Chronic Diabetes Complications Among Study Participants at Mettu Karl Referral Hospital, Southwest Ethiopia, 2019 |
Factors Associated with Chronic Diabetes Complications
Urban residents were 1.94 times more likely to have diabetes-related chronic complications when compared to rural residents [AOR: 1.94; 95% CI: (1.17, 3.20); p = 0.010]. The likelihood of chronic diabetes complications occurrence was 2.05 times more among participants who had duration of diabetes ≥ 10 years when compared to those who had duration of diabetes < 10 years [AOR: 2.05, 95% CI: (1.21, 3.47); p = 0.007]. Chronic diabetes complications were 4.19 times more likely among participants who had hypertension when compared to participants who had no hypertension [AOR: 4.19; 95% CI: (2.54, 6.91); p < 0.001]. Participants who had poor blood glucose control were 2.82 times more likely to have chronic complications when compared to those who had good glycemic control [AOR: 2.82; 95% CI: (1.53, 5.21); p = 0.001] (Table 4).
 |
Table 4 Bivariate and Multivariate Analysis of Predictors of Chronic Diabetes Complications Among Study Participants at Mettu Karl Referral Hospital, Southwest Ethiopia, 2019 |
Discussion
Diabetes-related complications may result in many disabilities which cause a reduction of patients’ quality of life and increase the burden on the healthcare system.12 Development of microvascular and macrovascular complications cause significant morbidity and mortality among people with diabetes.24 People with diabetes with uncontrolled blood glucose are at increased risk of developing these complications.25 Achieving the goal of glycemic control is the most effective way to avoid or delay the occurrence of diabetes complications.26 In addition to achieving the glycemic control goal, managing factors like blood pressure can prevent or delay the onset of diabetes complications among people with diabetes.16
In this study, the prevalence of chronic diabetes complications was 38.5%. This result was similar to a previous study done in Ethiopia which revealed chronic complications of diabetes was presented in 31.3% of participants.27 Another study done in Ethiopia by Tesfaye et al28 reported that 46.2% of participants were found to have at least one chronic complication which was also comparable with our finding. Our finding was also similar with study conducted in Saudi Arabia which identified that 42.7% of people with diabetes had one or more chronic complication.29 However, our finding was lower than the results of studies from Northeast Ethiopia (58.8%), Southwest Ethiopia (60.7%), and China (52.0%).30–32 This discrepancy might be due to a difference in the social and cultural health service demand. The behavioral difference in disclosing complications like sexual dysfunction might also contribute to this discrepancy.
This study found that neuropathy (23.9%), retinopathy (12.4%) and nephropathy (9.7%) were the most common chronic complications of diabetes. This correlated with a study done in Gondar, Northwest Ethiopia which reported that retinopathy (17.7%), neuropathy (7.9%), nephropathy (4.4%) were the most common complications.27 A study done by Arambewela et al12 in Sri Lanka identified similar results which found retinopathy in 26.1%, neuropathy in 62.6%, and nephropathy in 50.8% of participants. A study performed by Ramanathan et al33 in India demonstrated similar findings in which retinopathy (42%), neuropathy (38%) and nephropathy (35%) were the three most common diabetes complications. A study from Pakistan also found retinopathy in 43%, neuropathy in 39.6% and nephropathy in 20.2% in which they were the most common complications.34
This study identified that urban participants were more likely to have chronic diabetes complications when compared with rural participants. It was consistent with a study done in China which showed that participants in the rural area tended to have less diabetes-related complications.35 It was also similar with a study conducted in Bangladesh which reported that an urban area of residence was found to be associated chronic diabetes complications.36 It is identified that urban residents are more likely to have risk factors of diabetes complications including obesity, physical inactivity and irregular eating habits.35 In this study, it was also observed that urban residents were more overweight and obese.
DM patients who have lived with diabetes for more than or equal to 10 years were more likely to develop chronic diabetes complications when compared with patients who have lived less than 10 years with diabetes. In accordance with our finding, the studies conducted in the US and Bangladesh showed that there is a significant association between chronic diabetes complications and duration of diabetes.37,38 A study done in Kuwait also revealed that the longer duration of diabetes increases the risk of chronic complications. The study further stated that the risk of complications was double among patients who had diabetes for a duration of 10 to 19 years as compared with those who had less than 10 years and it was triple among those who had diabetes for 20 or more years.39 The longstanding hyperglycemia damages blood vessels. The damage to blood vessels can lead to heart attack and stroke, and problems with the kidneys, eyes, feet and nerves.40 Thus, a longer duration of uncontrolled diabetes increases the risk of diabetes-related complications.
The results of this study demonstrated that participants who had hypertension were more likely to develop diabetes-related chronic complications. This result was similar with a previous study conducted in Ethiopia which identified that the presence of hypertension was an independent predictor for the occurrence of diabetes complications.41 It was also consistent with a study done in the US.33 A study conducted in Saudi Arabia identified that hypertension was encountered as a comorbid disease in almost half of the participants and it was a predictor of diabetes complications.42 It is identified that diabetes and hypertension have underlying risk factors and complications in common. The macrovascular complications of diabetes can also occur due to hypertension. It is also identified that hypertension increases the risk of microvascular complications occurrence, especially for nephropathy.43,44
Our study observed that there was a higher likelihood of diabetes-related chronic complications among participants who had uncontrolled blood glucose when compared with those who had controlled their blood glucose. This result correlated with previous studies done in Ethiopia which reported that complications of DM were higher in people with diabetes with uncontrolled blood glucose.27,31 It was also similar with a study done in Turkey which revealed that chronic complications of diabetes such as nephropathy, retinopathy, neuropathy and cardiovascular diseases were significantly associated with uncontrolled blood glucose.45 A study done in Brazil also expressed that people with diabetes with uncontrolled blood glucose have a higher chance of developing diabetic retinopathy.46 Clinical trials demonstrated that prolonged uncontrolled blood glucose increases the occurrence of diabetes-related complications.47,48 Therefore, it is essential to optimize blood glucose levels to mitigate these complications.
One of the limitations of this study was using fasting blood glucose to assess glycemic control status instead of a HbA1c test. The other limitation was that the study did not determine severity and outcomes of the chronic complications.
Conclusion
Almost two-fifth of the study population had chronic diabetes complications. Diabetic neuropathy was the most commonly identified chronic complication, followed by diabetic retinopathy and nephropathy. This study also demonstrated that residence in an urban area, longer diabetes duration, the presence of hypertension and poor glycemic control were predictors of chronic diabetes complications. It is important to achieve good glycemic control to minimize the occurrence of chronic diabetes complications. Comorbid diseases, like hypertension, should be monitored and managed to reduce the risk of the complications.
Ethics and Consent
The ethical approval was obtained from the Institutional Review Board of Jimma University. A letter of permission was presented to Mettu Karl Referral Hospital administration. The study was conducted in accordance with the Helsinki Declaration. Each patient provided written informed consent. All data collected were treated with strict confidentiality at all stages of data processing.
Acknowledgments
We thank Jimma University for funding the study. We would like to extend our thanks for Mettu Karl Referral Hospital staff, data collectors and study participants for their cooperation to accomplish this study successfully.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Jimma University. The funding body had no role in study design, data collection, data analysis, data interpretation or in writing the manuscript.
Disclosure
All authors declare that they have no conflicts of interest.
References
1. Tripathi BK, Srivastava AK. Diabetes mellitus: complications and therapeutics. Med Sci Monit. 2006;12(7):RA130–RA47.
2. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. 2019;62(1):3–16. doi:10.1007/s00125-018-4711-2
3. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157(107843):10. doi:10.1016/j.diabres.2019.107843
4. Gebreyohannes EA, Netere AK, Belachew SA, Hirst JA. Glycemic control among diabetic patients in Ethiopia: a systematic review and meta-analysis. PLoS One. 2019;14(8):e0221790. doi:10.1371/journal.pone.0221790
5. Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes. 2011;29(3):116–122. doi:10.2337/diaclin.29.3.116
6. Litwak L, Goh SY, Hussein Z, Malek R, Prusty V, Khamseh ME. Prevalence of diabetes complications in people with type 2 diabetes mellitus and its association with baseline characteristics in the multinational achieve study. Diabetol Metab Syndr. 2013;5(1):1758–5996. doi:10.1186/1758-5996-5-57
7. Mao W, Yip CW, Chen W. Complications of diabetes in China: health system and economic implications. BMC Public Health. 2019;19(1):019–6569.
8. Goday A. Epidemiology of diabetes and its non-coronary complications. Rev Esp Cardiol. 2002;55(6):657–670. doi:10.1016/S0300-8932(02)76674-8
9. Ekoru K, Doumatey A, Bentley AR, et al. Type 2 diabetes complications and comorbidity in Sub-Saharan Africans. EClinicalMedicine. 2019;16:30–41. doi:10.1016/j.eclinm.2019.09.001
10. Sarpong C, Nsiah K, Mensah F, Agyeman-Duah E, Ahmed F. Prevalence of the Complications of Diabetes in Developing Countries. Arch Clin Biomed Res. 2017;1(5):235–241. doi:10.26502/acbr.50170026
11. Ahmed M, Yirdachew E, Tefera G. Diabetic complications among follow-up patients: a cross-sectional study at Jimma University specialized hospital diabetic clinic. J Clin Mol Endocrinol. 2018;3(1):45.
12. Arambewela MH, Somasundaram NP, Jayasekara H, et al. Prevalence of chronic complications, their risk factors, and the cardiovascular risk factors among patients with type 2 diabetes attending the diabetic clinic at a tertiary care hospital in Sri Lanka. J Diabetes Res. 2018;23:4504287.
13. Abebe N, Kebede T, Addise D. Diabetes in Ethiopia 2000–2016-prevalence and related acute and chronic complications; a systematic review. Afri J Diabetes Med. 2017;25(2).
14. Ou HT, Lee TY, Li CY, Wu JS, Sun ZJ. Incidence of diabetes-related complications in Chinese patients with type 1 diabetes: a population-based longitudinal cohort study in Taiwan. BMJ Open. 2017;7(6):2016–015117. doi:10.1136/bmjopen-2016-015117
15. Papatheodorou K, Papanas N, Banach M, Papazoglou D, Edmonds M. Complications of Diabetes 2016. J Diabetes Res. 2016;6989453(10):16.
16. Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. 2008;88(11):1254–1264.
17. Gizaw M, Harries A, Ade S, et al. Diabetes mellitus in Addis Ababa, Ethiopia: admissions, complications and outcomes in a large referral hospital. Public Health Action. 2015;5(1):74–78.
18. Meetoo D. Diabetes: complications and the economic burden. Br J Healthc Manag. 2014;20(2):60–67. doi:10.12968/bjhc.2014.20.2.60
19. Sheleme T, Mamo G, Melaku T, Sahilu T. Glycemic control and its predictors among adult diabetic patients attending Mettu Karl Referral Hospital, Southwest Ethiopia: a prospective observational study. Diabetes Ther. 2020;11(8):1775–1794.
20. Cheneke W, Suleman S, Yemane T, Abebe G. Assessment of glycemic control using glycated hemoglobin among diabetic patients in Jimma University specialized hospital, Ethiopia. BMC Res Notes. 2016;9(1):96.
21. Status WP. The use and interpretation of anthropometry. WHO Tech Rep Series. 1995;854(9).
22. American Diabetes Association. 2. Classification and diagnosis of Diabetes: standards of medical care in Diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S13–S28. doi:10.2337/dc18-S002
23. Pantalone KM, Hobbs TM, Wells BJ, et al. Clinical characteristics, complications, comorbidities and treatment patterns among patients with type 2 diabetes mellitus in a large integrated health system. BMJ Open Diabetes Res Care. 2015;3(1):e000093. doi:10.1136/bmjdrc-2015-000093
24. Handoko H, Rahardjo SS, Murti B. Predictors of macro and microvascular complication in type 2 diabetes mellitus patients at Dr. Moewardi Hospital, Surakarta. Indones J Med. 2018;3(1):1–13. doi:10.26911/theijmed.2018.03.01.01
25. Alsulaiman TA, Al-Ajmi HA, Al-Qahtani SM, et al. Control of type 2 diabetes in King Abdulaziz Housing City (Iskan) population, Saudi Arabia. J Family Community Med. 2016;23(1):1. doi:10.4103/2230-8229.172221
26. AL-Eitan LN, Nassar AM, Saadeh NA, Almomani BA. Evaluation of glycemic control, lifestyle and clinical characteristics in patients with type 2 diabetes treated at King Abdullah university hospital in Jordan. Can J Diabetes. 2016;40(6):496–502. doi:10.1016/j.jcjd.2016.04.009
27. Fasil A, Biadgo B, Abebe M. Glycemic control and diabetes complications among diabetes mellitus patients attending at University of Gondar Hospital, Northwest Ethiopia. Diabetes Metab Syndr Obes. 2019;12:75. doi:10.2147/DMSO.S185614
28. Tesfaye DJ. Coexistence of chronic complications among diabetic patients at nigist eleni mohammed memorial hospital, hossana, south Ethiopia. Open Access Library J. 2015;2(01):1.
29. Ageely H. Long-term diabetes-related severe complications among individuals with T2DM in Jazan, Saudi Arabia. J Acute Dis. 2019;8(2):72–77.
30. Abejew AA, Belay AZ, Kerie MW. Diabetic complications among adult diabetic patients of a tertiary hospital in Northeast Ethiopia. Adv Public Health. 2015;2015:1–7. doi:10.1155/2015/290920
31. Gebre BB, Assefa ZM. Magnitude and associated factors of diabetic complication among diabetic patients attending Gurage zone hospitals, South West Ethiopia. BMC Res Notes. 2019;12(1):780. doi:10.1186/s13104-019-4808-9
32. Liu Z, Fu C, Wang W, Xu B. Prevalence of chronic complications of type 2 diabetes mellitus in outpatients - a cross-sectional hospital based survey in urban China. Health Qual Life Outcomes. 2010;8(1):1477–7525. doi:10.1186/1477-7525-8-62
33. Ramanathan R. Correlation of duration, hypertension and glycemic control with microvascular complications of diabetes mellitus at a tertiary care hospital. J Neurol Exp Neural Sci. 2016;2017:1–5.
34. Shera A, Jawad F, Maqsood A, Jamal S, Azfar M, Ahmed U. Prevalence of chronic complications and associated factors in type 2 diabetes. J Pak Med Assoc. 2004;54(2):54–59.
35. Du G-L, Su Y-X, Yao H, et al. Metabolic risk factors of type 2 diabetes mellitus and correlated glycemic control/complications: a cross-sectional study between rural and urban Uygur residents in Xinjiang Uygur Autonomous Region. PLoS One. 2016;11(9):e0162611. doi:10.1371/journal.pone.0162611
36. Afroz A, Zhang W, Wei Loh AJ, Jie Lee DX, Billah B. Macro- and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab Syndr. 2019;13(5):2939–2946.
37. Islam SMS, Alam DS, Wahiduzzaman M, et al. Clinical characteristics and complications of patients with type 2 diabetes attending an urban hospital in Bangladesh. Diabetes Metab Syndr. 2015;9(1):7–13. doi:10.1016/j.dsx.2014.09.014
38. Ramanathan RS. correlation of duration hypertension and glycemic control with microvascular complications of diabet mellitus at a tertiary care hospital. J Neurol Exp Neural Sci. 2017.
39. El-Shazly M, Al-Shammer R, Moula A, Ismail A, Ismail W. Prevalence and factors associated with chronic diabetic complications among patients attending primary health care, a multi-centric study In Kuwait. Alexandria Med J. 2010;46(2):165–176.
40. Cade WT. Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther. 2008;88(11):1322–1335.
41. Wolde HF, Atsedeweyen A, Jember A, et al. Predictors of vascular complications among type 2 diabetes mellitus patients at University of Gondar Referral Hospital: a retrospective follow-up study. BMC Endocr Disord. 2018;18(1):52. doi:10.1186/s12902-018-0280-0
42. Albasheer OB, Sani M, Abbas A-B, et al. Prevalence, patterns and predictors of diabetes complications among patients with type 2 diabetes at Jazan Diabetic Centre, Saudi Arabia. Med Sci. 2020;24(101):83–89.
43. Long AN, Dagogo‐Jack S. Comorbidities of diabetes and hypertension: mechanisms and approach to target organ protection. J Clin Hypertens. 2011;13(4):244–251. doi:10.1111/j.1751-7176.2011.00434.x
44. De Boer IH, Bangalore S, Benetos A, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(9):1273–1284. doi:10.2337/dci17-0026
45. Kayar Y, Ilhan A, Kayar NB, et al. Relationship between the poor glycemic control and risk factors, life style and complications. 2017.
46. Lima VC, Cavalieri GC, Lima MC, Nazario NO, Lima GC. Risk factors for diabetic retinopathy: a case-control study. Int J Retina Vitreous. 2016;2(21):016–0047.
47. Group UPDS. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–853. doi:10.1016/S0140-6736(98)07019-6
48. Nathan DM, Genuth S, Lachin J, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.