Back to Journals » Infection and Drug Resistance » Volume 15
Prevalence of Tuberculosis and the Determinants of Lose to Follow-Up the Treatment for Tuberculosis Patients in Case of Buno Bedele and Ilu Ababor Zones, Oromia, Ethiopia
Authors Ababu DG , Gobena WE , Getahun AM
Received 15 May 2022
Accepted for publication 10 August 2022
Published 8 September 2022 Volume 2022:15 Pages 5321—5329
DOI https://doi.org/10.2147/IDR.S373230
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Dereje Gebeyehu Ababu,1 Woldemariam Erkalo Gobena,2 Azmeraw Misganaw Getahun2
1Department of Statistics, College of Natural Science, Salale University, Fitche, Ethiopia; 2Department of Statistics, College of Natural and Computational Sciences, Mettu University, Mettu, Ethiopia
Correspondence: Dereje Gebeyehu Ababu, Salale University, PO.Box 245, Fitche, Ethiopia, Tel +251921204863, Email [email protected]
Background: Tuberculosis (TB) is a potentially serious infectious disease that mainly affects the lungs. The bacteria, Mycobacterium tuberculosis (MTB), that cause tuberculosis are spread from one person to another person through tiny droplets released into the air via coughs and sneezes. The study aimed to investigate the prevalence of tuberculosis and determinants of lose to follow-up from TB treatment.
Methods: A retrospective study design is used to analyze the prevalence of tuberculosis and the determinants of lose to follow-up from TB treatment who follow the treatment from 2006 to 2017. The collected data were analyzed using descriptive statistics and statistical model.
Results: The study showed that among 375 TB patients, who started TB treatments, about 24.8% were lost to follow-up from TB treatment and 75.2% were censored at the end of the study. The median survival time of TB patients was 199 days. The results from the Log rank test showed that marital status, HIV co-infection, diabetes mellitus, cancer, and anemia cases had a significant difference between the survival experiences at a 5% level of significance. The result of the Cox-proportion hazard model showed that age (p-value=0.002; CI: (0.9831144, 0.9962526)), HIV co-infection (p-value=0.016; CI: (1.112293, 2.774715)), and anemia (p-value=0.021; CI: (1.089895, 2.938783)) had a significant effect on tuberculosis patients’ lose to follow-up from TB treatment at a 5% level of significance.
Conclusion: From 375 patients who started TB treatments, about 24.8% were lost to follow-up from TB treatment, and 75.2% were censored at the end of the study. The median survival time of TB patients was 199 days. The variables marital status, HIV co-infection, diabetes mellitus, cancer, and anemia cases had a significant difference between the survival experiences survival time of TB patients at a 5% level of significance. The result also showed that age, HIV co-infection, and anemia had a significant effect on tuberculosis patients.
Keywords: Cox regression, HIV co-infection, TB dropouts, tuberculosis, Log rank
Introduction
Tuberculosis (TB) is a potentially serious infectious disease that mainly affects the lungs. The bacteria (Mycobacterium tuberculosis (MTB)) that cause tuberculosis are spread from one person to another person through tiny droplets released into the air via coughs and sneezes. TB typically affects the lungs (pulmonary tube) but can affect other parts of the body as well. A recent publication4,8 showed that in 2020, there were 10 million new cases of TB worldwide, 1.1 lose to follow-up from TB treatment among HIV-negative people, and an additional 0.35 million lose to follow-up from TB treatment with HIV-associated. The World Health Organization (WHO) report indicates that there are about nine million new TB cases every year. Out of these new cases, about three million died. It is also known that out of the newly registered cases in developing countries, 98% were lost to follow-up from TB treatment. Generally, 75% of the persons in the productive age group (15–64 years) are mostly affected. The spread and expansion of HIV/AIDS pose a great challenge in the prevention and control of tuberculosis. Hence, it requires concerted efforts by communities at large. In 2015, 10.4 million people fell ill with TB and 1.8 million died of the disease.6,8
According to the 2015 global TB report, TB is a major global health problem. It causes ill-health among millions of people each year and ranks alongside HIV which is a leading cause of lose to follow-up from TB treatment worldwide. In 2014, there were an estimated 9.6 million new TB cases and there were also 1.5 million among adult people lose to follow-up from TB treatment globally. Of the estimated new cases, the majority were in South-East Asia (4.0 million), followed by Africa (2.7 million). In the same year, the report showed that there were an estimated 1.0 million new TB cases worldwide among children. Of the estimated new cases, the majorities were in Africa (330 thousand) next to South-East Asia (340 thousand).5
According to the 2016 WHO report, the TB incidence rate and the number of deaths from TB continue to fall globally. In 2015, an estimated 1.4 million people died from this largely curable disease with a further 400,000 deaths from TB reported among people living with HIV. The global tuberculosis report showed that TB now ranks above HIV as a leading cause of death worldwide.2
The previous study showed that the occurrence of late presentation for HIV care among HIV/TB co-infected patients was only 59.9%. The study also showed that HIV/TB co-infected participants for these non-users of tobacco were 50% less likely to present late for HIV care as compared to tobacco users.7 TB is the leading killer among HIV-infected people by weakened immune systems. A quarter of a million lose to follow-up from TB treatment were HIV associated, with 98% of lose to follow-up from TB treatment were in the developing world in that young adults were mostly affected.3
Some hospital-based pilot studies showed that in Buno Bedele and Ilu Ababor Zones, TB treatment lose to follow-up from TB treatment is high. As a result, this research tries to investigate which factors are the main responsible/causes. To the best of our knowledge, no study has been conducted in Buno Bedele and Ilu Ababor Zones regarding the prevalence of TB and the determinants of lose to follow-up from TB treatment of TB patients in the case of Buno Bedele and Ilu Ababor Zones, Oromia, Ethiopia.
Methods
Study Area
Buno Bedele and Ilu Ababor Zones are parts of Oromia Region that are located in the south-west of the country, Ethiopia, and 600 km far from the capital city (Addis Ababa). These zones are well-known places for coffee production, ever green forest, and a variety of tourist attractions such as Sor Rivers.
Design and Data of the Study
A retrospective study design was used to analyse the prevalence of tuberculosis and the determinants of lose to follow-up from TB treatment who follow the treatment in the health sectors of the two zones from 2006 to 2017.
Inclusion and Exclusion Criteria
Patients with TB whose record data were missing were excluded from the study. Patients with complete demographic and clinical data were included in the study.
Operational Definition
Treatment Completed
A patient with TB who completed treatment without evidence of failure, but with no record of sputum smear or culture results, in the last month of treatment.
Censored
The observations are considered as “censored” for cases that do not experience the event by the end of the study.
Lose to Follow-Up
A TB patient who did not start treatment or whose treatment was interrupted for 2 consecutive months or more. In this study, the lose to follow-up is an event of interest.
Died
A TB patient who died from any cause during treatment.
Sample Size and Techniques
The target populations for this study were all TB patients in health sectors of some selected woredas from Ilu Abba Bora and Buno Bedele Zones. Some districts were selected by using a simple random sampling (SRS) technique. A total of 375 TB patients who were admitted and visited health sectors were included in our sampling frame based on the inclusion and exclusion criteria.
Variables of the Study
The response variable for this study was time to lose to follow-up (event of interest) from TB treatment which was measured in days. Several predictors were included in this study: sex, age, marital status, TB/HIV co-infection, phase of TB treatment, TB type, TB category, previous TB history, anemia, and physical inactive.
Statistical Analysis
In this research, statistical analysis was performed using R and SPSS 20 statistical software.
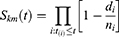
Kaplan–Meier Estimator
Kaplan–Meier survival analysis is a non-parametric statistic that is used to estimate the survival function. It is used to measure the fraction of patients living for a certain amount of time after treatment and the function is given by
where  is the ordered times of lose to follow-up from TB treatment and
is the ordered times of lose to follow-up from TB treatment and  and
and  denote the number of events and the number of individuals still at risk at time
denote the number of events and the number of individuals still at risk at time , respectively.
, respectively.
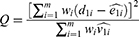
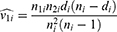
Log Rank Test
The Log rank test is a non-parametric test that is used for comparing two or more independent survival curves. The Log rank test statistic for comparing two groups is given by
where  is the number of rank-ordered event times,
is the number of rank-ordered event times,  is the observed number of events in group one at event time
is the observed number of events in group one at event time  ,
,  is the expected number of events corresponding to
is the expected number of events corresponding to  ,
,  is the number of individuals at risk in group 1 just prior to event time
is the number of individuals at risk in group 1 just prior to event time  , and
, and  is the number of individuals at risk in group 2 just prior to event time
is the number of individuals at risk in group 2 just prior to event time  ,
,
where  is the variance of the number of events
is the variance of the number of events  at time
at time  ,
,  and
and  are the number of individuals at risk and number of vascular complication in both groups (ie, group 1 and group 2) just prior to event time
are the number of individuals at risk and number of vascular complication in both groups (ie, group 1 and group 2) just prior to event time  , respectively.
, respectively.
The Cox (Semi-Parametric) Proportional Hazards Model
The Cox (proportional hazards or PH) model is the most commonly used multivariate approach for analysing survival time data in medical research. It is a survival analysis regression model, which describes the relationship between the event incidence as expressed by the hazard function and a set of covariates.
Mathematically, the Cox model is given by
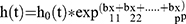 where the hazard function h(t) is dependent on (or determined by) a set of p covariates (x1, x2, …, xp), whose impact is measured by the size of the respective coefficients (b1, b2, bp). The term h0 (t) is called the baseline hazard and is the value of the hazard if all the xi are equal to zero (the quantity exp (0) equals 1). The “t” in h (t) reminds us that the hazard may vary over time.
where the hazard function h(t) is dependent on (or determined by) a set of p covariates (x1, x2, …, xp), whose impact is measured by the size of the respective coefficients (b1, b2, bp). The term h0 (t) is called the baseline hazard and is the value of the hazard if all the xi are equal to zero (the quantity exp (0) equals 1). The “t” in h (t) reminds us that the hazard may vary over time.
Likelihood ratio test, Score test, and Wald test were used to test the null hypothesis of the regression parameters. Akaike’s information criterion and the Bayesian information criterion were used to carry out the comparison of non-nested models.1
Multivariable Cox Regression
Model Testing
After getting the regression model, we go for assessing the significance of the coefficients as well as the construction of the confidence interval. Three different tests were used to test the null hypothesis of the regression parameters:
- Partial likelihood ratio test
- Score test
- Wald test
Results
Demographic Characteristics and Descriptive Statistics
A total of 375 TB patients who follow the treatment were included in the study. The study showed that from the total of 375 TB patients, 282(75.2%) were censored and 93 (24.8%) patients were lost to follow-up from TB treatment. The median survival time of TB patients was 199 days. The descriptive result also showed that 186 (49.6%) and 189(50.4%) were females and males, respectively. Among the total of 375 TB patients, 172(45.9%) had previous TB history and 203 (54.1%) had no previous TB history (new case) (Table 1).
 |
Table 1 Demographic Characteristics of Categorical Covariate |
Survival Curve Estimate of TB Patients
The result from the Kaplan–Meier estimator showed that the curves declined as the survival time increased, and it showed that most of lose to follow-up from TB treatment occurred in the first 150 days of treatment initiation (Figure 1).
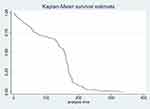 |
Figure 1 The Kaplan–Meier survival curve of the overall TB patients’ treatment. |
The result also showed that patients with no HIV Co-infection had a higher survival time than patients with HIV Co-infection (Figure 2).
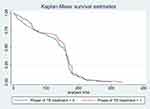 |
Figure 2 The Kaplan–Meier survival curve of the TB patients regarding phase of TB. |
Comparison of Survival Time to Lose to Follow-Up from TB Treatment
The result from the Log rank test showed that marital status, HIV/TB co-infection, diabetes mellitus, cancer, and anemia had significant differences between the survival experiences at a 5% level of significance (Table 2).
 |
Table 2 Comparison of Survival Experience of TB Patients |
Univariable Analysis Cox Regression Model
Factors that are significant at a 5% level of significance in univariable Cox-proportional hazard analysis were included in multivariable Cox-proportional hazard analysis. The follow-up time of TB patients was significantly related to covariate age, HIV co-infection, diabetes mellitus, cancer, phase of TB treatment, and anemia, at 25% significance levels (Table 3).
 |
Table 3 Univariable Cox PH Analysis |
The result from multivariate Cox regression showed that age, HIV/TB co-infection, and anemia were the variables that significantly affected the follow-up time of TB patients at a 5% significant level (Table 4).
 |
Table 4 Multivariable Cox PH Analysis |
Model Checking
Since the p-value (0.4596) was not significant at a 5% level of significance for the global test (chi-square=5.68), the proportional hazard assumption is satisfied (Table 5).
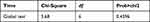 |
Table 5 Test of Proportional-Hazards Assumption |
Discussion
This research was conducted to achieve the research objective which was the prevalence of tuberculosis and the determinants of lose to follow-up from TB treatment. The study revealed that of the included patients in the study, 282 (75.2%) were censored and 93(24.8%) patients were lost to follow-up from TB treatment. This result implied that 75.2% of the patients followed the treatment whether or not they were cured or not until the end of the study. In the other case, the result showed that 24.8% were lost to follow-up from TB treatment due to different factors that were discussed under the results of multivariable Cox-regression. This finding is consistent with previous studies.3–6,8
The result also showed that 186 (49.6%) and 189(50.4%) were females and males, respectively. This finding is similar to previous studies conducted in Southern Ethiopia and North-eastern Ethiopia.8,9 The prevalence of new TB cases among the patients in this study was 203 which accounts for the higher percentage (54.1%). This result is consistent with previous studies conducted in different areas.4–6
The result from the Kaplan–Meier estimator showed that patients with no HIV co-infection had a higher survival time than patients with HIV co-infection.4 The reason for this finding is concerned that patients who have HIV co-infection might be lost to follow-up from TB treatment. Results from multivariate Cox-regression showed that the age of patients was significantly associated with lose to follow-up from TB treatment. This result is similar to the previous studies conducted in Geneva and north-eastern Ethiopia.6,8,9 This result might be due to the reason that as age increases, there is a high probability to have TB (Table 4). The results also showed that HIV/TB co-infection was significantly associated with lose to follow-up from TB treatment.4 This finding is consistent with previous studies conducted in different areas of the world.2–4,6,7 Moreover, the results revealed that anemia was significantly associated with lose to follow-up from TB treatment. This result might be due to the case that those who have anemia disease lose to follow-up from TB treatment.
Conclusions
Of the 375 patients who started TB treatments, about 24.8% were lost to follow-up from TB treatment, and 75.2% were censored at the end of the study. The median survival time of TB patients was 199 days. The results from multivariate Cox regression showed that age, HIV co-infection, and anemia had a significant effect on tuberculosis patients.
Abbreviations
AIC, Akaike’s information criterion; BIC, Bayesian information criterion; AIDS, acquired immune deficiency syndrome; HIV, human immunodeficiency virus; MTB, Mycobacterium tuberculosis; TB, tuberculosis; WHO, World Health Organization.
Data Sharing Statement
If needed, the data in Excel format is available for this article up on request to the corresponding author.
Ethics Approval and Informed Consent
This study complied with the Declaration of Helsinki and approved by the Institutional Review Board of Mettu University (Reference No: Meu/902/1043). Permission was obtained from the health hospital administration before data collection. Due to the retrospective nature of the study, the patient data obtained do not require the patient’s informed consent; the Ethics Committee of Mettu University waived the need for informed consent. Patient records were anonymized and de-identified prior to data analysis to ensure confidentiality of individual patient information.
Acknowledgments
The authors would like to thank study participants, health sectors and data collectors for their contribution for this research.
Funding
The author(s) received no specific funding for this work.
Disclosure
The authors declare that there are no competing interests.
References
1. Akaike H. Information measures and model selection, bulletin of the international statistical. Int Stat Inst. 1983;44:277–290.
2. Hosmer DW, Lemeshow S. Regression Modeling of Time-to-Event Data. New York: Wiley; 1999.
3. World Health Organization. Feasibility Study and Orientation. Dr IkushiOnozaki. World Health Organization; 2008.
4. World Health Organization. “Global Tuberculosis Control: World Health Organization Report. Geneva: World Health Organization; 2020.
5. World Health Organization. Global Tuberculosis Control: World Health Organization Report. Geneva, Switzerland: World Health Organization; 2015.
6. World Health Organization Report. “Global Tuberculosis Report: Global Actions and Investments Fall Far Short of Those Needed to End the Global TB”. Geneva: World Health Organization Report; 2016.
7. Gesesew H, Tsehaineh B, Massa D, Tesfay A, Kahsay H, Mwanri L. The role of social determinants on tuberculosis/HIV co-infection mortality in southwest Ethiopia: a retrospective cohort study. BMC Res Notes. 2016;9:1–8.
8. Gebrezgabiher G, Romha G, Ejeta E, Asebe G, Zemene E, Ameni G. Treatment outcome of tuberculosis patients under directly observed treatment short course and factors affecting outcome in Southern Ethiopia: a five-year retrospective study. PLoS One. 2016;11(2):e0150560. doi:10.1371/journal.pone.0150560
9. Mekonnen D, Derbie A, Desalegn E. TB/HIV co-infections and associated factors among patients on directly observed treatment short course in Northeastern Ethiopia: a 4 years retrospective study. BMC Res Notes. 2015;8:666. doi:10.1186/s13104-015-1664-0
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.