Back to Journals » International Journal of General Medicine » Volume 15
Prevalence of Thyroid Dysfunction Among Patients with Heart Failure at a Tertiary Hospital in Mogadishu, Somalia
Authors Mohamud MA , İbrahim İG , Ahmed SA , Karataş M, Jeele MOO
Received 21 April 2022
Accepted for publication 25 July 2022
Published 28 July 2022 Volume 2022:15 Pages 6335—6339
DOI https://doi.org/10.2147/IJGM.S371697
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mohamed Abdullahi Mohamud,1 İsmail Gedi İbrahim,2 Said Abdirahman Ahmed,1 Mesut Karataş,1 Mohamed Osman Omar Jeele3
1Department of cardiology, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Benadir, Somalia; 2Department of radiology, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Benadir, Somalia; 3Department of internal medicine, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Benadir, Somalia
Correspondence: Mohamed Abdullahi Mohamud, Department of cardiology, Mogadishu Somalia Turkish Training and Research Hospital, Digfer street, Mogadishu, Benadir, Somalia, Tel +252 616983961, Email [email protected]
Introduction: Thyroid disease is an independent predictor of heart failure in patients. This study aimed to investigate the prevalence of thyroid dysfunction among patients with heart failure in Mogadishu, Somalia.
Methods: From January 2019 to January 2021, a total of 250 patients diagnosed with heart failure admitted to the cardiology outpatient and emergency departments were evaluated retrospectively. The demographic characteristics, the cause of heart failure, and the kind of heart failure were recorded. Patients were categorized into subclinical hypothyroidism, hypothyroidism, low T3 syndrome, subclinical hyperthyroidism, and hyperthyroidism.
Results: A total of 250 heart failure patients. The prevalence of thyroid dysfunction among heart failure patients was 35.6%. The mean age of the patients was 59.8± 14 years. Males outnumbered females by 159 (63.2%). The prevalence of thyroid dysfunction was 35.6%. Out of the 250 patients that were examined, most of the patients 30(33.3%) had subclinical hypothyroidism. 23 (25.6%) had overt hypothyroidism, 15 (16.7%) had overt hyperthyroidism, 20 (22.2%) had low T3 syndrome, and two cases had subclinical hyperthyroidism. Regarding the gender status of the thyroid dysfunction, 43(48.3%) were male, and 46(51.7%) were female. Regarding heart failure types among thyroid dysfunction patients, most patients were HFrEF (n=64, 71.9%), and 25(28.1%) were HFpEF. Patients with heart failure and reduced ejection fraction (HFrEF) were more likely to have thyroid dysfunction than those with preserved ejection fraction (p = 0.012). Regarding comorbidities among heart failure patients with thyroid dysfunction, approximately half of the patients had hypertension (40.4%).
Conclusion: Thyroid problems are one of the most prevalent endocrine abnormalities in our practice. Subclinical hypothyroidism was the most common type of thyroid dysfunction among this population. We suggest that thyroid function be evaluated with cardiac function in patients with heart failure and followed up and treated together with heart failure.
Keywords: thyroid dysfunction, heart failure, prevalence, Somalia, East Africa
Introduction
Heart failure (HF) is a complex clinical syndrome characterized by the reduced ability of the heart to pump and fill blood.1 Heart failure affects around 64.3 million people throughout the world. In developed countries, the prevalence of acknowledged heart failure is between 1 to 2% of the general adult population. Heart failure occurs at a rate of 1 to 9 per 1000 person-years in Europe and the United States.2 According to hospital studies, the prevalence rates in Sub-Saharan Africa range from 9.4 to 42.5%.3 Despite breakthroughs in HF treatment during the last 15 years, the outlook for this disorder remains terrible.4 Overt, untreated hyperthyroidism and hypothyroidism have been discovered as common causes of heart failure in the last decades.5 Additionally, persistent subclinical thyroid dysfunction has recently been associated with HF development in patients with or without underlying heart disease.6 Comorbidities that can affect the outcome of heart failure include diabetes, hypertension, dyslipidemia, and renal failure. Endocrine diseases, such as thyroid abnormalities, are also important.7 Low T3 syndrome (LT3S) affects 20 to 30% of people with chronic heart failure and is characterized by a decrease in Free triiodothyronine (FT3) with normal levels of free thyroxine (FT4) and thyroid stimulating hormone (TSH).8 Other studies show that fT3 supplementation increases life expectancy in these patients.9 Given the importance of thyroid abnormalities in patients with chronic HF and their impact on prognosis, thyroid function should be checked regularly in these patients, according to the American Heart Association.10 Despite the importance of this topic, there have been no studies on the variety of prevalence of thyroid dysfunction among patients with heart failure in Somalia. The main purpose of this study is to investigate the prevalence of thyroid dysfunction among heart failure patients at a tertiary hospital in Mogadishu, Somalia.
Methods and Materials
This single-center retrospective cohort study was conducted in Mogadishu, Somali Turkish Training and Research Hospital, Between January 2019 and January 2021. Our hospital is the region’s largest multidisciplinary tertiary referral hospital. The research ethics committee of our hospital approved this study (22.11.2021- MSTH/8129). This study was carried out following the Helsinki Declaration’s contents. Patients gave their informed permission. We followed the protocols of our work center. The data were obtained from electronic medical records of patients diagnosed with thyroid disease via the hospital information system.Patients diagnosed with heart failure were included in the study.
A total of 250 heart failure patients, regardless of age and sex, who had no missing data were selected for the study. Patients younger than 30 years and those with missing data in the hospital database were excluded from this study. Age, cause of heart failure, and type were among the examined variables. Patients were categorized into five groups subclinical hypothyroidism, hypothyroidism, low t3 syndrome, subclinical hyperthyroidism, and hyperthyroidism. The normal range for thyroid function assays in our institution is TSH 0.35–5.10 μIU/mL, FT4 0.60–1.20 ng/mL, and FT3 1.80–4.20 pg/mL. Hypothyroidism was defined as FT4 < 0.60 ng/mL and TSH > 5.1 μIU/mL, and subclinical hypothyroidism was defined as normal free hormone levels and a TSH > 5.1 μIU/mL. Hyperthyroidism was defined as FT4 > 1.20 ng/mL and TSH < 0.35 μIU/mL, and subclinical hyperthyroidism was defined as normal free hormone levels, TSH < 0.35 μIU/mL, low t3 syndrome was defined as normal free hormone levels, and a TSH > 5.1 μIU/mL and FT3 < 4.20 pg/mL. Thyroid function tests were measured by a Roche e411 Immunoassay Analyzer (Roche Diagnostics Corporation, Indianapolis, IN).11 The epidemiological and clinical importance of OA and CA in patients with heart failure with mid-range ejection fraction (HFmrEF, defined as LVEF between 40 and 49%) and heart failure with preserved ejection fraction (HFpEF, defined as LVEF between 40 and 49%) (HFpEF, defined as LVEF greater than 50%.12,13 The data was collected using Microsoft excel and was analyzed using Statistical Package for Social Sciences (SPSS) software version 26. Descriptive data analysis and Pearson correlation were mainly used in this study. A P-value of less than 0.05 was considered statistically significant.
Results
We included this study with a total of 250 heart failure patients. The prevalence of thyroid dysfunction among heart failure patients was 35.6% (89/250) (Figure 1). The mean age of the patients was 59.8±14 years. According to the gender distribution among heart failure patients, 159(63.2%) were male, and 91(36.4%) were female.The thyroid disorder patients were grouped into five categories; most of the patients were subclinical hypothyroidism (n=30, 33.3%), while 23(25.6%) were overt hypothyroidism, 15(16.7%) were overt hyperthyroidism, 20(22.2%) were low t3 syndrome, and 2 cases were subclinical hyperthyroidism (Table 1). Regarding the gender status of the thyroid dysfunction patients, 43(48.3%) were male, and 46(51.7%) were female. There was no statistically significant association between age groups and thyroid dysfunction (p = 0.80).The heart failure patients were classified into two groups, most of the patients (n=147, 58.8%) were HFrEF, and 103(41.2%) were HFpEF (Figure 2). Regarding heart failure types among thyroid dysfunction patients, most patients were HFrEF (n=64, 71.9%), and 25(28.1%) were HFpEF. Patients with heart failure and reduced ejection fraction (HFrEF) were more likely to have thyroid dysfunction than those with preserved ejection fraction (p = 0.012).Regarding Comorbidities among heart failure patients with thyroid dysfunction, approximately half of the patients had hypertension (40.4%), ischemic heart disease (31.5%), valvular heart disease (20.2%), and cardiomyopathy at 9% (Figure 3).The drugs used for heart failure in thyroid dysfunction patients were as follows: ACE Inhibitors at 97.8%, Beta-Blockers at 98.9%, Spironolactone at 77.5%, and Lasix at 80.7%. Thyroid drugs at about 19.1% and Levothyroxine at about 38.2%.
 |
Table 1 Thyroid Dysfunction Types |
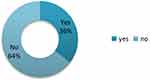 |
Figure 1 Thyroid dysfunction among heart failure patients. |
 |
Figure 2 Types of heart failure patients regarding ejection fraction. |
 |
Figure 3 Comorbidities associated with heart failure. |
Discussion
The current global prevalence of heart failure is expected to be 64.34 million cases (8.52 per 1000 inhabitants, with 29% moderate heart failure, 19% intermediate, and 51% severe heart failure), or 9.91 million YLDS (11.61 per 1000 YLD).14 Hospitalization is common among HF patients, with 83% admitted at least once and 43% admitted three to four times. Heart failure is more common in the elderly.15 Because it is regarded to have a poorer prognosis than most malignancies.16 Thyroid hormone regulates the cardiovascular system, especially when heart failure is prevalent(HF). With over 23 million people diagnosed worldwide, heart failure is a major public health concern.17 Hyperthyroidism and hypothyroidism cause changes in cardiac contractility, myocardial oxygen consumption, cardiac output, blood pressure, and systemic vascular resistance (SVR).18 The current study is the first study to examine the prevalence of thyroid dysfunction among heart failure patients in Somalia. Thyroid disease is the most common endocrine disorder worldwide, second to diabetes mellitus in terms of endocrine diseases, particularly in Africa.19 Hyperlipidemia and ventricular arrhythmias are caused by insufficient thyroid hormone, while atrial arrhythmias are caused by excess thyroid hormone, and both cause hypertension and heart failure. These heart irregularities are usually reversible if the underlying thyroid disease is treated. Thyroid disorder patients were grouped into four categories. Most of our patients had subclinical hypothyroidism, followed by overt hypothyroidism and overt hyperthyroidism, with similar findings reported by Mfeukeu-Kuate et al.8 Another study from Cameroon conducted by Yemele Honoré, Kemnang et al revealed that approximately two-thirds of their study participants had euthyroid, while 25 (39.7%) were dysthyroid (30).Bernad et Biondi et al conducted a study in Italy and suggested that the SHypo with TSH >10 mU/l is a significant risk factor for HF in older patients. A meta-analysis of six prospective cohort studies involving a total of 2068 patients with SHypo recently validated these findings. In hyperthyroid patients with underlying cardiac problems such as ischemic, hypertensive, or valvular disease, and/or atrial fibrillation, the risk of HF and low ejection fraction is raised. About 7–8% of middle-aged hyperthyroid patients develop atrial fibrillation or flutter; this risk rises to 10–20% in elderly patients and up to 20–35% in those over 65.8 Lippi G, Sanchis-Gomar F et al studied the prevalence and types of thyroid dysfunction in patients with chronic HF in Africa, as well as the factors that contribute to it. They reported that hypertension (52.4%) and valvular heart disease (14.3%) were the most common causes of HF.20 Similarly, in our study, approximately half of the patients (40.4%) had hypertension, 31.5% had ischemic heart disease, 20.2% had valvular heart disease, and 9% had cardiomyopathy.This study has certain limitations, including 1. It is a single-center retrospective study 2. A number of the patients is small, and data cannot be generalized. Besides these limitations, this is the first study regarding thyroid dysfunction among heart failure patients reported from Somalia. The main objective of this study is in its epidemiological, descriptive nature; further studies are needed to distinguish the true thyroid dysfunction and low t3, which arise secondary to HF.
Conclusion
Thyroid problems are one of the most prevalent endocrine abnormalities in our practice. Subclinical hypothyroidism was the most common type of thyroid disease in our study, followed by overt hypothyroidism and low t3 syndrome among the heart failure population. Thyroid disease has become a major endocrine problem in Somalia. As a result, public health programs involving the supply of iodine-fortified foods, prenatal fe, and iodine vitamin supplements, as well as boosting public awareness of thyroid problems through the media, may be beneficial in the prevention of thyroid disorders.
Abbreviations
EF, Ejection Fraction; HFpEF, Heart Failure with Preserved Ejection Fraction; HFrEF, Heart Failure with Reduced Ejection Fraction; ICD-10, International Classification of Diseases 10; TSH, thyroid stimulating hormone; T3, Triiodothyronine; T4, thyroxine; SPSS, Statistical Package for Social Sciences.
Data Sharing Statement
The data is available from the corresponding author and can be accessed upon request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that they have no funding source for this research.
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3(1):7.
2. Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. 2020;22(8):1342–1356.
3. Ogah O, Adebiyi A, Sliwa K. Heart Failure in Sub-Saharan Africa. Top Hear Fail Manag. 2019;1:987.
4. Roger VL, Weston SA, Redfield MM, et al. Trends in heart failure incidence and survival in a community-based population. J Am Med Assoc. 2004;292(3):344–350.
5. Biondi B, Kahaly GJ. Cardiovascular involvement in patients with different causes of hyperthyroidism. Nat Rev Endocrinol. 2010;6(8):431–443. doi:10.1038/nrendo.2010.105.
6. Nanchen D, Gussekloo J, Westendorp RGJ, et al. Subclinical thyroid dysfunction and the risk of heart failure in older persons at high cardiovascular risk. J Clin Endocrinol Metab. 2012;97(3):852–861.
7. Kannan L, Shaw PA, Morley MP, et al. Thyroid dysfunction in heart failure and cardiovascular outcomes. Circ Hear Fail. 2018;11(12):547.
8. Yemele Honoré K, Ama Moor VJ, Mfeukeu Kuate L, Martine E. Frequency and Relevance of Thyroid Dysfunction in Patients with Chronic Heart Failure: a Cross Sectional Study at Yaoundé Central Hospital, Cameroon. Arch Clin Biomed Res. 2021;5(1):129.
9. Savinova OV, Liu Y, Aasen GA, et al. Thyroid hormone promotes remodeling of coronary resistance vessels. PLoS One. 2011;6(9):755.
10. Hunt SA, Baker DW, Chin MH, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the 1995 guidel. Circulation. 2001;104(24):2996–3007.
11. Hassan-Kadle MA, Adani AA, Eker HH, et al. Spectrum and Prevalence of Thyroid Diseases at a Tertiary Referral Hospital in Mogadishu, Somalia: a Retrospective Study of 976 Cases. Int J Endocrinol. 2021;2021:25.
12. Borrelli C, Gentile F, Sciarrone P, et al. Central and Obstructive Apneas in Heart Failure With Reduced, Mid-Range and Preserved Ejection Fraction. Front Cardiovasc Med. 2019;6(September):4–87.
13. Dunlay SM, Roger VL, Redfield MM. Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol. 2017;14:591–602.
14. Lippi G, Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Med J. 2020;5:15.
15. Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure: preventing disease and death worldwide. ESC Hear Fail. 2014;1(1):4–25.
16. Braunwald E. The war against heart failure: the Lancet lecture. Lancet. 2015;385(9970):812–824. doi:10.1016/S0140-6736(14)61889-4
17. Stanciu AE, Zamfir-Chiru-Anton A, Stanciu MM, Gheorghe DC. Impact of Thyroid Disease on Heart Failure. Role Clin Card Electrophysiol Manag Congest Hear Fail. 2017;1:87.
18. Klein I, Danzi S. Thyroid disease and the heart. Circulation. 1725–35;116:2007.
19. Mfeukeu-Kuate L, Yemele HK, Jingi AM, et al. Burden, Type, and Associated Factors of Thyroid Dysfunction in Patients with Heart Failure in Sub-Saharan Africa: a Cross-Sectional Study. World J Cardiovasc Dis. 2021;11(11):485–497.
20. Lippi G, Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Med J. 2020;5(March):15.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
