Back to Journals » Clinical Interventions in Aging » Volume 18
Prevalence of Sarcopenia in Africa: A Systematic Review
Authors Mballa Yene BV , Lee SY, Park KS , Kang YJ, Seo SH , Yoo JI
Received 9 February 2023
Accepted for publication 27 June 2023
Published 4 July 2023 Volume 2023:18 Pages 1021—1035
DOI https://doi.org/10.2147/CIA.S407917
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Bryan Vincent Mballa Yene,1 Sang-Yeob Lee,2 Ki-Soo Park,3 Yang Jae Kang,4 Sung Hyo Seo,2 Jun-Il Yoo5
1Department of Bio & Medical Big Data, Gyeongsang National University Hospital, Jinju, South Korea; 2Department of Biomedical Research Institute, Gyeongsang National University Hospital, Jinju, South Korea; 3Department of Preventive Medicine, School of Medicine, Gyeongsang National University, Jinju, South Korea; 4Division of Life Science Department, Gyeongsang National University, Jinju, South Korea; 5Department of Orthopaedic Surgery, Inha University Hospital, Incheon, South Korea
Correspondence: Jun-Il Yoo, Department of Orthopaedic Surgery, Inha University Hospital, 27 Inhang-ro, Jung-gu, Incheon, 22332, South Korea, Tel +82-32-890-3663, Email [email protected]
Objective: The world population gradually getting older, age-related sarcopenia is becoming more frequent. Known to be highly prevalent in high income countries, relative data in Africa are still scarce. This review aims to estimate the prevalence of sarcopenia in Africa and its characteristics.
Study Design and Setting: A literature search in PubMed, Web of Science, Google Scholar, and Scopus was conducted in October 2022. All studies reporting the prevalence of sarcopenia in Africa within 15 years were included, and we did an assessment of bias with Hoy et al’s risk bias assessment tool. The estimated prevalence of sarcopenia was the outcome and we performed secondary analyses by age, gender, and diagnostic criteria. The random effect model was used for the prevalence estimation. The prevalence of sarcopenia and 95% confidence interval (95% CI) were calculated using the inverse-variance method.
Results: A total of 17 studies met our eligibility criteria, for a study population of 12,690 participants with 44.3% males and 55.7% females. The overall prevalence of sarcopenia was 25% (95% CI: 19– 30%). The prevalence of sarcopenia among 50 years old and older was 23% (95% CI: 17– 29%). We had a higher prevalence of sarcopenia among males (30%, %95 IC: 20– 39%) than females (29%, %95 IC: 21– 36%). The prevalence of sarcopenia was different depending on the diagnosis criteria used.
Conclusion: The prevalence of sarcopenia in Africa was relatively high. However, the fact that the majority of included studies were hospital-based studies shows the necessity of further community-based studies in order to have a more accurate representation of the situation in the general population.
Keywords: sarcopenia, prevalence, Africa, meta-analysis
Introduction
Sarcopenia is a term derived from the Greek phrase poverty of flesh. Sarcopenia is a progressive and generalized skeletal muscle disorder that is associated with increased likelihood of adverse outcomes including falls, fractures, physical disability and mortality.1 Despite having been the main subject of research for several decades, it was only recently that sarcopenia was officially recognized as a muscle disease.2 Thus, scarcity of sarcopenia-related research in Africa is not surprising. However, with a growing part of the African population, as everywhere else in the world, continuously getting older, the number of studies on sarcopenia is increasing.
Sarcopenia has been defined as a progressive and generalized skeletal muscle disorder that involves the accelerated loss of muscle mass and function.3 The high frequency of negative outcomes caused by muscle wasting among older adults especially, has been the trigger of first studies on the subject. Unfortunately, as many other newly researched topics in medicine or in science, the absence of a clear definition and cutoff values of sarcopenia components caused a great heterogeneity in study results.4 In a need of a clear consensus among the research community, several definitions and associated cutoff values have been proposed. One of the most widely recognized is the definition of the European Working Group on Sarcopenia in Older People (EWGSOP) which after a first definition in 2010,5 published an update (EWGSOP2) presenting low muscle strength as the primary parameter of sarcopenia and the most reliable measure of the muscle function. More specifically, low muscle strength refers to probable sarcopenia and the presence of low muscle quantity or quality and low physical performance was considered as severe sarcopenia.1 In clinical practice, several methods have been developed for the diagnosis of sarcopenia according to EWGSOP2; muscle strength, assistance with walking, rising from a chair, climbing stairs, and falls (SARC-F) questionnaire and the Ishii screening tool;6,7 for muscle strength, grip strength and chair stand test; for skeletal muscle mass, appendicular skeletal muscle mass (ASM) by dual-energy X-ray absorptiometry (DXA), whole-body skeletal muscle mass (SMM) or ASM predicted by bioelectrical impedance analysis (BIA) and lumbar muscle cross-sectional area by CT (computed tomography) or MRI (magnetic resonance imaging); for physical performance, gait speed, short physical performance battery (SPPB), timed-up-and-go test (TUG) and 400-meter walk or long-distance corridor walk (400-m walk).
The EWGSOP2 also provided cut-off points for the different assessment methods: low grip strength (<27 kg for male, <16 kg for female), low strength by chair (>15s for five rises), ASM (<20 kg for male, <15 kg for female), ASM/height2 (<7.0 kg/m2 for male, <5.5 kg/m2 for female), gait speed <0.8m/s, SPBB ≤8 point score, TUG ≥20 s, 400m walk test (Non-completion or ≥6 min for completion).1
In Asia, the Asian Working Group for Sarcopenia (AWGS) also defined cut-off values adapted to the Asian population: muscle mass by dual X-ray absorptiometry (<7.0 kg/m2 for male, <5.4 kg/m2 for female) and by bioimpedance analysis (<7.0 kg/m2 for male, <5.7 kg/m2 for female); handgrip strength (<28 kg for male and <18 kg for female); criteria for low physical performance are 6-m walk <1.0 m/s, Short Physical Performance Battery score ≤9, or 5-time chair stand test ≥12 seconds.8
Similarly, the International Working Group on Sarcopenia (IWGS) defined a diagnosis of sarcopenia with a gait speed <1 m/s and an objectively measured low muscle mass (ASM/height2 ≤7.23 kg/m2 in male and ≤5.67 kg/m2 in female).9
The Foundation for the National Institutes of Health (FNIH) Sarcopenia Project in 2014 described the following cut-offs: grip strength <26kg for male and <16kg for female, and for low lean mass, lean mass adjusted for body mass index <0.789 for male and <0.512 for female.10 The FNIH ASM cut-point had a great specificity and sensitivity to detect low functional ability in older black South African women.11
In South Africa, a cut-point of appendicular skeletal muscle mass index (SA ASMI) <4.94 kg/m2 was described.11 This cut-point is one of the few described to the best of our knowledge which was specific to Africans.
The prevalence of sarcopenia highly variates according to the definition used but also to the population studied.12,13 For example, prevalence of 4.8% in Brazil, 6.8% in the United Kingdom and 17.4% among Chinese community dwelling older adults has been found.14–16 Unfortunately, the literature concerning sarcopenia in Africa is not as furnished as in other continents. Therefore, we conducted a systematic review aiming to assess the prevalence of sarcopenia in Africa.
Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.17 This review is a prevalence study, so ethics approval was not required. The protocol of this systematic review was registered at PROSPERO with the number CRD42022374573.
Search Strategy and Eligibility Criteria
We included every study in which the participants were people living in Africa. Studies were excluded if they were reviews, meeting abstracts, study protocols without data, letters to editors, studies for which the full text could not be obtained, and studies published in languages other than French or English.
Studies that did not report an estimated prevalence or provide any sarcopenia diagnosis criteria enabling the extraction of the prevalence were excluded. To include the most recent studies, we arbitrary restricted our study within 15 years.
We performed an electronic search in PubMed and Web of Science with the following descriptors: “sarcopenia”, “prevalence”, “epidemiology”, “incidence”, “Africa”. The complete research strategy was: PubMed: ((((sarcopenia[MeSH Terms]) OR (sarcopenias[Title/Abstract])) AND (((prevalence[MeSH Terms]) OR (epidemiology[Title/Abstract])) OR (incidence[Title/Abstract])))); Web of science (TS=(sarcopenia) AND TS=(prevalence OR epidemiology OR incidence) AND AD=Africa) AND PY=(2007–2022). In addition, starting from a hospital provided article database, a forward and backward citation search was performed using Google Scholar for the forward citation search and Scopus, then Web of Science if not retrieved in Scopus for the backward citation search.
A single reviewer, using the free web-tool for systematic review Rayyan, screened titles and abstracts of relevant studies. If multiple papers came from the same project, we chose the one with the largest sample size and more consistent with the data extraction rule of this review. Choices were secondly assessed and double checked by a second reviewer.
Data Extraction and Quality Assessment
We extracted data with Microsoft Excel 2019, these included study characteristics (first author, publication year, study design), the population information (age, area, gender and sample size), diagnostic criteria for sarcopenia, assessment method used for each parameter (muscle mass, muscle strength and muscle performance), cutoff values of each parameter, and sarcopenia prevalence. We calculated prevalence as the number of people with sarcopenia divided by the whole sample size. We extracted the baseline data from the cohort studies if the prevalence could be calculated from them.
We used Hoy et al’s18 tool for prevalence study for risk of bias assessment. The tool consists of 10 items addressing four domains of bias plus a summary risk of bias assessment. We rated items as high or low risk of bias, and a summary assessment of bias risk was rated as low, moderate, and high. Studies with insufficient information on an item were rated high risk. The risk of bias will be presented in a table.
Data Synthesis and Analysis
The prevalence of sarcopenia was described in percentage with an inverse variance method. Studies have been stratified by age and gender if possible. Gender was male or female, heterogeneity between the studies was assessed through the I2 test, and I2 values greater than 50% were considered moderate to high. A random or fixed-effects model was used according to the degree of heterogeneity. A funnel plot was used to assess publication bias, and plot asymmetry was assessed by Begg’s test and Egger’s test. The overall quality of evidence was summarized using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system. We used Cochrane’s Review manager (Revman) and R environment for our statistics analysis.
Results
Study Selection and Characteristics
We conducted a forward and backward citation search from a hospital provided database from which, after screening, we retrieved 18 reports. The search of electronic databases identified 1379 records; after removing duplicates, we assessed 1371 reports. After title and abstract screening, followed by inclusion criteria assessment, we retrieved 4 reports. Among those 22 reports, 6 were from the same study for a final total of 17 studies included.11,19–34 The study selection is presented in a PRISMA flow diagram (Figure 1).
 |
Figure 1 PRISMA flowchart presenting the summary of searches carried out in the literature. |
Included study characteristics are presented in Supplementary Table S1. We identified studies published between 2015 and 2022 from the whole continent, with 10 studies from South Africa and 2 from Cameroon. Among these studies 15 were cross sectional-studies and 2 were prospective cohort studies. The smallest sample size was 68 and the largest 4302, with 2 studies of less than 100 participants.24,25 The total population included is 12,690 participants for 7070 females and 5620 males. Four studies were only made of females11,23,27,31 and 1 only of males.33 Eight studies reported participants aged more than 50 years old, some just reported the mean age of the participants. Sarcopenia was mainly diagnosed using criteria from the EWGSOP and the FNIH. One study used the hand grip strength alone as defining criteria.32
Quality Assessment
The overall quality of evidence according to the GRADE was very low (downgraded because of inconsistency related to heterogenous results), the risk of bias assessed by Hoy’s tool is presented in Table 1. We assessed 23.5% (n = 4) of studies as moderate risk of bias and 76.5% (n = 13) as low risk of bias. The overall risk of bias was assessed as low.
 |
Table 1 Quality Assessment of Included Studies Using Hoy’s Tool |
Prevalence of Sarcopenia
Overall Prevalence
Our meta-analysis showed an overall pooled prevalence of sarcopenia in Africa of 25% with a 95% confidence interval (95% CI): 19–30% and a high level of heterogeneity (I2 = 98%, P < 0.01) (Figure 2).
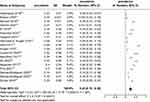 |
Figure 2 Forest plot of the prevalence of sarcopenia. Abbreviations: SE, Standard error; CI, confidence interval; IV, Inverse Variance. |
Age and Gender
The prevalence of participants aged more than 50 years old was 23% (%95 CI: 17–29%, I2 = 96%, P < 0.01%). Participants aged less than 50 years old had a prevalence of 27% (21–34%, I2 = 35%, P < 0.01) (Figure 3). The male gender showed a prevalence of sarcopenia (30%, %95 CI: 20–39%, I2 = 98%, P < 0.01) similar to the female gender (29%, %95 CI: 21–36%, I2 = 98%, P < 0.01) (Figure 4).
 |
Figure 3 Subgroup analysis of the prevalence of sarcopenia by age. Abbreviations: SE, Standard error; CI, confidence interval; IV, Inverse Variance. |
 |
Figure 4 Subgroup analysis of the prevalence of sarcopenia by gender. Abbreviations: SE, Standard error; CI, confidence interval; IV, Inverse Variance. |
Diagnostic Criteria
The diagnostic criteria of the EWGSOP identified a prevalence of 16% (%95 CI: 12–22%, I2 = 95%, P < 0.01). The FNIH criteria reported a prevalence of 28% (%95 CI: 12–45%, I2 = 99%, P < 0.01); and the SA ASMI was used to identify 9% (%95 CI: 6–12%, I2 = 0%, P = 1). Studies using the muscle mass to define sarcopenia reported a prevalence of 49% (%95 CI: 35–63%, I2 = 90%, P < 0.01) (Figure 5).
Risk Factors of Sarcopenia
The risk factors mentioned in our primary studies were female gender with an odds ratio (OR) of 3.08 (%95 CI: 1.48–6.41), SARC-F score >4 (OR: 5.36, %95 CI: 2.42–11.85), increasing age (OR: 1.090, 1.034–1.149), age >75 years (OR: 6.50, %95 CI: 1.20–35.30), malnutrition (OR: 5.817, %95 CI:1.471–24.434), absence of formal education (OR: 2.810, %95 CI: 1.043–7.57), bone erosion (OR: 0.057, %95 CI: 0.006–0.532), overfat BMI (OR: 12.3, %95 CI: 2.27–67.6), increased waist circumference (OR: 0.176, %95 CI: 0.038, 0.980) (Table 2).
 |
Table 2 Risk Factors of Sarcopenia |
Sensitivity Analysis
We conducted a sensitivity analysis by removing each study and pulling the others to determine which ones influenced the overall pooled effect. We did not find any significant statistical difference as shown in Figure 6.
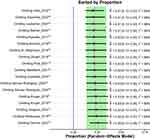 |
Figure 6 Sensitivity analysis. |
Publication Bias
We assessed publication bias with a slightly asymmetric funnel plot (Figure 7), an Egger’s test with a P = 0.1942 (Figure 8) and a Begg’s test with a P = 0.7332. However, the trim-and-fill method imputed 3 extra studies and the newly created funnel plot was symmetrical with P < 0.01 (Figure 9). These results are to be considered with caution knowing the high heterogeneity of our study.35,36
 |
Figure 7 Begg’s Funnel plot. |
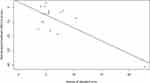 |
Figure 8 Egger’s test. |
 |
Figure 9 Trimmed and filled funnel plot. |
Discussion
Our results showed that the prevalence of sarcopenia in Africa was 25%. The male gender had a slightly higher prevalence of sarcopenia than female gender and prevalence was highly influenced by the diagnosis criteria used to define sarcopenia. In addition, the risk factors associated to sarcopenia were female gender, SARC-F score >4, increasing age, age >75 years, malnutrition, absence of formal education, bone erosion, overfat BMI, increased waist circumference.
The prevalence of sarcopenia we found is higher than the prevalence found in Korea (13.1%),37 in Brazil (16%)38 or in Asia.13 However, our prevalence is much closer to the prevalence found in hospitals in China (male: 29.7%; female: 23.0%)39 or in Switzerland (22.6%).40 This difference can be explained by the fact that most of our sample has been assessed in clinical setting like the Swiss and Chinese studies; on the opposite of the former studies which only include community-dwelling participants. These results are in accordance with those of a review in different regions around the world which found higher prevalence of sarcopenia in nursing homes, followed by hospitals and then community general population.41 The preponderance of hospital-based studies could be due to the relative affordability and easiness to conduct of these studies compared to community-based studies which need more resources. Nevertheless, hospitalized individuals might represent an additional risk factor for sarcopenia and functional decline because of reduced caloric intake, low physical activity or prolonged bed-rest.42
We found a slightly higher prevalence of sarcopenia among male participants than female participants. This is in line with results found in Korea37 and in Japan;43,44 but contrasts with those found in Brazil.38 As a matter of fact, literature results showing association between gender and sarcopenia are globally inconsistent. Some studies state that male might be more susceptible to develop sarcopenia because of difference in diet and lifestyle, especially alcohol and tobacco consumption.37 Other studies showed that hormonal changes which enhance the decrease of muscle mass occur more slowly in male than in female leading to a higher prevalence of sarcopenia among females.13 After menopause, the hormone level drastically drop in female compared to a continuous slow decrease in male.45,46 This difference in decrease of anabolic acting androgens might be the cause of a higher prevalence of sarcopenia among females. Moreover, regarding the predominance of females in our sample these results must be considered cautiously.
Most of our primary studies used the EWGSOP or the FNIH criteria to define sarcopenia. The EWGSOP for many years has been the only available international consensus definition of sarcopenia and the FNIH criteria showed an unexpected good performance in assessing sarcopenia among black people.11 The prevalence of sarcopenia depending on the defining criteria was highly heterogeneous as found in other studies.12,13,16 In addition, the South African ASMI cut-off described by Kruger et al despite outperforming other criteria in the assessment of sarcopenia in African setting11 was not used most of the time. Considering the few numbers of studies using the same diagnosis criteria in our review, it is difficult to interpret the pooled prevalence of each diagnosis criteria. However, the pooled prevalence found using our most representative criteria from the EWGSOP (16%) is similar to a Brazilian counterpart using the same diagnosis criteria.38
Sarcopenia is an age-related disease characterized by increasing occurrences among older. Therefore, it is quite surprising that we found a prevalence of sarcopenia higher among participants younger than 50 years old compared to those older. First of all, although 50 years old could be considered as quite young to define older age, if we consider specificities of Africa with lower life expectancy than other continents this age could be taken as older age.47 In addition, most of our primary studies did not use the same intervals to classify the age of participants. Moreover, as mentioned before, our sample comprised many hospital-based studies that might have quite influenced our results. Despite being an elderly disease, sarcopenia may develop secondarily to conditions like prolonged states of chronic inflammation, oxidative stress, and mitochondrial alterations or liver cirrhosis.3,33,48 Nevertheless, sarcopenia is an ageing disease and it has been proven than older age corresponds to higher prevalence of sarcopenia and to higher number of bad outcomes like falls.1,49–51 Furthermore, we identified only two studies with participants aged less than 50 years old and the prevalence of sarcopenia among participants older than 50 years old was almost equal to our overall prevalence (23%). Thus, once again the result of our subgroup analysis on age must be interpreted with caution.
We found several risk factors associated with sarcopenia. Female gender was a risk factor of sarcopenia and this is similar to results found in China.52 As mentioned before, gender interaction with sarcopenia is not very well established. However, due to earlier and more important hormonal changes, female gender might be a risk factor of sarcopenia.45 SARC-F score >4 also predicted sarcopenia. This is not surprising knowing the fact that it is a reliable and efficient tool for sarcopenia screening.6 Increasing age was a risk factor of sarcopenia like in many other studies.52–55 Sarcopenia being an age-related disease, it becomes more prevalent in the elderly. After 75 years old we found a higher risk in a similar manner than an Indonesian study that found a significant lower grip strength after that age.56 Malnutrition was associated with sarcopenia like found elsewhere.55–59 This can be explained by the fact that protein, vitamin D/calcium and acid base balance of the diet have a role in maintaining muscle mass and muscle strength or physical performance.60 We found the absence of education could be a risk factor of sarcopenia. This is in line with a Chinese study that found that the higher the level of education the better the lifestyle and the income are, and therefore the lower the prevalence of sarcopenia.52 Moreover, we found bone erosion to be associated with sarcopenia. This might be explained by the key role played by chronic inflammation in the pathophysiology of both sarcopenia and bone chronic inflammatory diseases.61 Overfat BMI and increased waist circumference were risk factors of sarcopenia. Although the prevalence of obesity and in a same way of sarcopenic obesity is continuously increasing around the world,62 this result is opposite to what we can find in many studies.52,54,55,59,63–65 Age-related muscle loss triggers a muscle weakness and is associated with a decreased physical activity and also a diminished total energy expenditure leading to a weight gain especially in the abdominal area.66 However, it has been proven that this overweight muscle mass is negatively associated with muscle quality and performance measures.67
Limitations
We encountered numerous limitations in this study. First, although we aimed to retrieve studies across Africa, some regions like East Africa are not represented in this study. Second, even though our primary studies had different sample populations, different assessment criteria and even different study designs, our results are still highly heterogeneous and therefore could be quite distant from the true effect. Finally, our subgroup analyses did not include the whole of the primary studies due to a lack of data from some studies. Therefore, subgroup analyses pooled prevalence must be considered cautiously.
Conclusion
To the best of our knowledge, the present study is one of the first systematic reviews aiming to assess the prevalence of sarcopenia in Africa. The prevalence of sarcopenia in Africa is 25%. Despite its numerous limitations, this review points out that sarcopenia is becoming a public health problem in Africa and that future community-based studies should be conducted with clear and similar diagnosis criteria to assess the true reality of the disease in the general population and propose suitable interventions.
Acknowledgments
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea, Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI22C0494).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
1. Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi:10.1093/ageing/afy169
2. 2023 ICD-10-CM diagnosis code M62.84: sarcopenia. Available from: https://www.icd10data.com/ICD10CM/Codes/M00-M99/M60-M63/M62-/M62.84.
3. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–2646. doi:10.1016/S0140-6736(19)31138-9
4. Batsis JA, Barre LK, Mackenzie TA, Pratt SI, Lopez-Jimenez F, Bartels SJ. Variation in the prevalence of sarcopenia and sarcopenic obesity in older adults associated with different research definitions: dual-energy X-ray absorptiometry data from the National Health and Nutrition Examination Survey 1999–2004. J Am Geriatr Soc. 2013;61(6):974–980. doi:10.1111/jgs.12260
5. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing. 2010;39(4):412–423. doi:10.1093/ageing/afq034
6. Malmstrom TK, Miller DK, Simonsick EM, Ferrucci L, Morley JE. SARC‐F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. 2016;7(1):28–36. doi:10.1002/jcsm.12048
7. Ishii S, Tanaka T, Shibasaki K, et al. Development of a simple screening test for sarcopenia in older adults. Geriatr Gerontol Int. 2014;14 Suppl 1:93–101. doi:10.1111/ggi.12197
8. Chen LK, Woo J, Assantachai P, et al. Asian working group for sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300–307.e2. doi:10.1016/j.jamda.2019.12.012
9. Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults. current consensus definition: prevalence, etiology, and consequences. international working group on sarcopenia. J Am Med Dir Assoc. 2011;12(4):249–256. doi:10.1016/j.jamda.2011.01.003
10. Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol. 2014;69(5):547–558. doi:10.1093/gerona/glu010
11. Kruger HS, Micklesfield LK, Wright HH, Havemann-Nel L, Goedecke JH. Ethnic-specific cut-points for sarcopenia: evidence from black South African women. Eur J Clin Nutr. 2015;69(7):843–849. doi:10.1038/ejcn.2014.279
12. Mayhew AJ, Amog K, Phillips S, et al. The prevalence of sarcopenia in community-dwelling older adults, an exploration of differences between studies and within definitions: a systematic review and meta-analyses. Age Ageing. 2019;48(1):48–56. doi:10.1093/ageing/afy106
13. Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord. 2017;16(1). doi:10.1186/s40200-017-0302-x
14. da AT, Duarte de S, Santos JLF, Lebrão ML. Prevalence and associated factors of sarcopenia, dynapenia, and sarcodynapenia in community-dwelling elderly in São Paulo - SABE study. Rev Bras Epidemiol Braz J Epidemiol. 2019;21(Suppl 02):e180009. doi:10.1590/1980-549720180009.supl.2
15. Patel HP, Syddall HE, Jameson K, et al. Prevalence of sarcopenia in community-dwelling older people in the UK using the European Working Group on Sarcopenia in Older People (EWGSOP) definition: findings from the Hertfordshire Cohort Study (HCS). Age Ageing. 2013;42(3):378–384. doi:10.1093/ageing/afs197
16. Ren X, Zhang X, He Q, et al. Prevalence of sarcopenia in Chinese community-dwelling elderly: a systematic review. BMC Public Health. 2022;22(1):1702. doi:10.1186/s12889-022-13909-z
17. The BMJ. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. Available from: https://www.bmj.com/content/372/bmj.n160.
18. Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–939. doi:10.1016/j.jclinepi.2011.11.014
19. Dlamini SN, Norris SA, Mendham AE, et al. Targeted proteomics of appendicular skeletal muscle mass and handgrip strength in black South Africans: a cross-sectional study. Sci Rep. 2022;12(1):9512. doi:10.1038/s41598-022-13548-9
20. Gregson CL, Madanhire T, Rehman A, et al. Osteoporosis, rather than sarcopenia, is the predominant musculoskeletal disease in a rural South African community where human immunodeficiency virus prevalence is high: a cross-sectional study. J Bone Miner Res off J Am Soc Bone Miner Res. 2022;37(2):244–255. doi:10.1002/jbmr.4464
21. Irwin NEA, Fabian J, Hari KR, Lorentz L, Mahomed A, Botha JF. Myosteatosis, the more significant predictor of outcome: an analysis of the impact of myosteatosis, sarcopenia, and sarcopenic obesity on liver transplant outcomes in Johannesburg, South Africa. Exp Clin Transplant off J Middle East Soc Organ Transplant. 2021;19(9):948–955. doi:10.6002/ect.2021.0083
22. Pina I, Mendham AE, Tomaz SA, et al. Intensity matters for musculoskeletal health: a cross-sectional study on movement behaviors of older adults from high-income Scottish and low-income South African Communities. Int J Environ Res Public Health. 2021;18(8):4310. doi:10.3390/ijerph18084310
23. Mendham AE, Goedecke JH, Micklesfield LK, et al. Understanding factors associated with sarcopenic obesity in older African women from a low-income setting: a cross-sectional analysis. BMC Geriatr. 2021;21(1):247. doi:10.1186/s12877-021-02132-x
24. Essomba MJN, Atsa D, Noah DZ, et al. Geriatric syndromes in an urban elderly population in Cameroon: a focus on disability, sarcopenia and cognitive impairment. Pan Afr Med J. 2020;37:229. doi:10.11604/pamj.2020.37.229.26634
25. Laubscher CV, Burger MC, Conradie MM, Conradie M, Jordaan JD. Prevalence of sarcopenia in older South African patients following surgery for fragility fractures of the Hip. Geriatr Orthop Surg Rehabil. 2020;11:2151459320971560. doi:10.1177/2151459320971560
26. Salinas-Rodríguez A, Rivera-Almaraz A, Scott A, Manrique-Espinoza B. Severity levels of disability among older adults in low- and middle-income countries: results from the study on global ageing and adult health (SAGE). Front Med. 2020;7:562963. doi:10.3389/fmed.2020.562963
27. Kruger HS, Havemann-Nel L, Ravyse C, Moss SJ, Tieland M. Physical activity energy expenditure and sarcopenia in black South African urban women. J Phys Act Health. 2016;13(3):296–302. doi:10.1123/jpah.2015-0078
28. Ngeuleu A, Allali F, Medrare L, Madhi A, Rkain H, Hajjaj-Hassouni N. Sarcopenia in rheumatoid arthritis: prevalence, influence of disease activity and associated factors. Rheumatol Int. 2017;37(6):1015–1020. doi:10.1007/s00296-017-3665-x
29. Adebusoye LA, Ogunbode AM, Olowookere OO, Ajayi SA, Ladipo MM. Factors associated with sarcopenia among older patients attending a geriatric clinic in Nigeria. Niger J Clin Pract. 2018;21(4):443–450. doi:10.4314/njcp.v21i4
30. Zengin A, Jarjou LM, Prentice A, Cooper C, Ebeling PR, Ward KA. The prevalence of sarcopenia and relationships between muscle and bone in ageing West‐African Gambian men and women. J Cachexia Sarcopenia Muscle. 2018;9(5):920–928. doi:10.1002/jcsm.12341
31. Barnard SA, Pieters M, Nienaber-Rousseau C, Kruger HS. Degree of obesity influences the relationship of PAI-1 with body fat distribution and metabolic variables in African women. Thromb Res. 2016;146:95–102. doi:10.1016/j.thromres.2016.09.003
32. Essomba MJ, Noah D, Sylvain Raoul SN, Ashuntantang G. Facteurs associés à la sarcopénie chez des patients âgés de 55 Ans et plus dans un service de médecine interne au cameroun sarcopenia and associated factors in patients aged 55 and over in an i nternal medicine department in Cameroon. Health Sci Dis. 2022;23:58–61.
33. El Maghraoui A, Ebo’o FB, Sadni S, Majjad A, Hamza T, Mounach A. Is there a relation between pre-sarcopenia, sarcopenia, cachexia and osteoporosis in patients with ankylosing spondylitis? BMC Musculoskelet Disord. 2016;17:268. doi:10.1186/s12891-016-1155-z
34. B H, E MM, R A, A RA, A A, S A. Baseline sarcopenia is associated with lack of response to therapy, liver decompensation and high mortality in hepatocellular carcinoma patients. Asian Pac J Cancer Prev APJCP. 2020;21(11):3285–3290. doi:10.31557/APJCP.2020.21.11.3285
35. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L, Moreno SG. Assessing publication bias in meta-analyses in the presence of between-study heterogeneity. JR Stat Soc Ser a Stat Soc. 2010;173(3):575–591. doi:10.1111/j.1467-985X.2009.00629.x
36. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Performance of the trim and fill method in the presence of publication bias and between-study heterogeneity. Stat Med. 2007;26(25):4544–4562. doi:10.1002/sim.2889
37. Choo YJ, Chang MC. Prevalence of sarcopenia among the elderly in Korea: a meta-analysis. J Prev Med Pub Health. 2021;54(2):96–102. doi:10.3961/jpmph.21.046
38. Diz JBM, Leopoldino AAO, de MB, et al. Prevalence of sarcopenia in older Brazilians: a systematic review and meta-analysis. Geriatr Gerontol Int. 2017;17(1):5–16. doi:10.1111/ggi.12720
39. Chen Z, Li WY, Ho M, Chau PH. The prevalence of sarcopenia in Chinese older adults: meta-analysis and meta-regression. Nutrients. 2021;13(5):1441. doi:10.3390/nu13051441
40. Bertschi D, Kiss CM, Beerli N, Kressig RW. Sarcopenia in hospitalized geriatric patients: insights into prevalence and associated parameters using new EWGSOP2 guidelines. Eur J Clin Nutr. 2021;75(4):653–660. doi:10.1038/s41430-020-00780-7
41. Papadopoulou SK, Tsintavis P, Potsaki P, Papandreou D. Differences in the prevalence of sarcopenia in community-dwelling, nursing home and hospitalized individuals. a systematic review and meta-analysis. J Nutr Health Aging. 2020;24(1):83–90. doi:10.1007/s12603-019-1267-x
42. Martone AM, Bianchi L, Abete P, et al. The incidence of sarcopenia among hospitalized older patients: results from the Glisten study. J Cachexia Sarcopenia Muscle. 2017;8(6):907–914. doi:10.1002/jcsm.12224
43. Shimokata H, Ando F, Yuki A, Otsuka R. Age-related changes in skeletal muscle mass among community-dwelling Japanese: a 12-year longitudinal study. Geriatr Gerontol Int. 2014;14 Suppl 1:85–92. doi:10.1111/ggi.12219
44. Makizako H, Nakai Y, Tomioka K, Taniguchi Y. Prevalence of sarcopenia defined using the Asia Working Group for Sarcopenia criteria in Japanese community-dwelling older adults: a systematic review and meta-analysis. Phys Ther Res. 2019;22(2):53–57. doi:10.1298/ptr.R0005
45. Burger HG, Dudley EC, Robertson DM, Dennerstein L. Hormonal changes in the menopause transition. Recent Prog Horm Res. 2002;57:257–275. doi:10.1210/rp.57.1.257
46. Juul A, Skakkebaek NE. Androgens and the ageing male. Hum Reprod Update. 2002;8(5):423–433. doi:10.1093/humupd/8.5.423
47. Kowal P. Definition of an older person. Proposed working definition of an older person in Africa for the MDS Project. Available from: https://www.academia.edu/19489000/Definition_of_an_older_person_Proposed_working_definition_of_an_older_person_in_Africa_for_the_MDS_Project.
48. Saeki C, Takano K, Oikawa T, et al. Comparative assessment of sarcopenia using the JSH, AWGS, and EWGSOP2 criteria and the relationship between sarcopenia, osteoporosis, and osteosarcopenia in patients with liver cirrhosis. BMC Musculoskelet Disord. 2019;20(1):615. doi:10.1186/s12891-019-2983-4
49. Trevisan C, Vetrano DL, Calvani R, Picca A, Welmer AK. Twelve-year sarcopenia trajectories in older adults: results from a population-based study. J Cachexia Sarcopenia Muscle. 2022;13(1):254–263. doi:10.1002/jcsm.12875
50. Bischoff-Ferrari HA, Orav JE, Kanis JA, et al. Comparative performance of current definitions of sarcopenia against the prospective incidence of falls among community-dwelling seniors age 65 and older. Osteoporos Int. 2015;26(12):2793–2802. doi:10.1007/s00198-015-3194-y
51. Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol. 2001;54(8):837–844. doi:10.1016/s0895-4356(01)00349-3
52. Chen F, Xu S, Wang Y, et al. Risk factors for sarcopenia in the elderly with type 2 diabetes mellitus and the effect of metformin. J Diabetes Res. 2020;2020:3950404. doi:10.1155/2020/3950404
53. Hwang J, Park S. Gender-specific risk factors and prevalence for sarcopenia among community-dwelling young-old adults. Int J Environ Res Public Health. 2022;19(12):7232. doi:10.3390/ijerph19127232
54. Chen X, Hou L, Zhang Y, Dong B. Analysis of the prevalence of sarcopenia and its risk factors in the elderly in the Chengdu community. J Nutr Health Aging. 2021;25(5):600–605. doi:10.1007/s12603-020-1559-1
55. Simsek H, Meseri R, Sahin S, et al. Prevalence of sarcopenia and related factors in community-dwelling elderly individuals. Saudi Med J. 2019;40(6):568–574. doi:10.15537/smj.2019.6.23917
56. Riviati N, Setiati S, Laksmi PW, Abdullah M. Factors related with handgrip strength in elderly patients. Acta Med Indones. 2017;49(3):215–219.
57. Beaudart C, Sanchez-Rodriguez D, Locquet M, Reginster JY, Lengelé L, Bruyère O. Malnutrition as a strong predictor of the onset of sarcopenia. Nutrients. 2019;11(12):2883. doi:10.3390/nu11122883
58. Shen Y, Chen J, Chen X, Hou L, Lin X, Yang M. Prevalence and associated factors of sarcopenia in nursing home residents: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(1):5–13. doi:10.1016/j.jamda.2018.09.012
59. Chatzipetrou V, Bégin MJ, Hars M, Trombetti A. Sarcopenia in chronic kidney disease: a scoping review of prevalence, risk factors, association with outcomes, and treatment. Calcif Tissue Int. 2022;110(1):1–31. doi:10.1007/s00223-021-00898-1
60. Mithal A, Bonjour JP, Boonen S, et al. Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA. 2013;24(5):1555–1566. doi:10.1007/s00198-012-2236-y
61. Clynes MA, Gregson CL, Bruyère O, Cooper C, Dennison EM. Osteosarcopenia: where osteoporosis and sarcopenia collide. Rheumatology. 2021;60(2):529–537. doi:10.1093/rheumatology/keaa755
62. Batsis JA, Villareal DT. Sarcopenic obesity in older adults: aetiology, epidemiology and treatment strategies. Nat Rev Endocrinol. 2018;14(9):513–537. doi:10.1038/s41574-018-0062-9
63. Dodds RM, Granic A, Davies K, Kirkwood TBL, Jagger C, Sayer AA. Prevalence and incidence of sarcopenia in the very old: findings from the Newcastle 85+ Study. J Cachexia Sarcopenia Muscle. 2017;8(2):229–237. doi:10.1002/jcsm.12157
64. Darroch P, O’Brien WJ, Mazahery H, Wham C. Sarcopenia prevalence and risk factors among residents in aged care. Nutrients. 2022;14(9):1837. doi:10.3390/nu14091837
65. Senior HE, Henwood TR, Beller EM, Mitchell GK, Keogh JWL. Prevalence and risk factors of sarcopenia among adults living in nursing homes. Maturitas. 2015;82(4):418–423. doi:10.1016/j.maturitas.2015.08.006
66. Nair KS. Aging muscle. Am J Clin Nutr. 2005;81(5):953–963. doi:10.1093/ajcn/81.5.953
67. Mesinovic J, McMillan LB, Shore-Lorenti C, De Courten B, Ebeling PR, Scott D. Metabolic syndrome and its associations with components of sarcopenia in overweight and obese older adults. J Clin Med. 2019;8(2):145. doi:10.3390/jcm8020145
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


