Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 13
Prevalence of Intestinal Parasitic Infections and Associated Risk Factors Among Schoolchildren in Ibb Governorate, Southwest Yemen: A Cross-Sectional Study
Authors Al-Fakih AA, Al-wrafi EA, Al-motawkil AAHAAJ, Shabalah AZA, Aqeel AF, Mahdi MA, Al-hubaishi HA, Marsh YM, Joyer BH, Al-shoga'a GH
Received 26 May 2022
Accepted for publication 30 August 2022
Published 19 September 2022 Volume 2022:13 Pages 325—333
DOI https://doi.org/10.2147/PHMT.S374475
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Abdulkawi Ali Al-Fakih,1,2 Essam Ali Al-wrafi,3 Amat Al-haleem Abdu Al-jabar Al-motawkil,3 Al-zahra Ali Shabalah,3 Asma Faisal Aqeel,3 Mohammed Abdallah Mahdi,3 Haneen Abdualkareem Al-hubaishi,3 Yahya Mansour Marsh,3 Bothina Hassan Joyer,3 Ghada Hossain Al-shoga’a3
1Department of Medical Microbiology, Faculty of Science, Ibb University, Ibb, Yemen; 2Faculty of Allied Medical Sciences, Aljazeera University, Ibb, Yemen; 3Department of Medical Laboratories, Faculty of Allied Medical Sciences, Aljazeera University, Ibb, Yemen
Correspondence: Abdulkawi Ali Al-Fakih, Department of Medical Microbiology, Faculty of Science, Ibb University, Ibb, Yemen, Tel +967 771950569, Fax +967 04413766, Email [email protected]
Introduction: Intestinal parasitic infections (IPIs) among schoolchildren are important public health problem, especially in developing countries, and monitoring of such infections and associated risk factors are necessary for intervention strategies. In line with this view, the aim of this study was to determine the prevalence of IPIs and associated risk factors among schoolchildren in Ibb governorate, southwest Yemen.
Methods: A cross-sectional study was carried out during February to April 2020 on 600 schoolchildren selected from 6 districts of Ibb governorate. Fecal specimens were examined using saline and iodine wet mount and formal-ether concentration techniques. Socio-demographic data were collected using pre-designed, structured questionnaires. The results were analyzed using SPSS for Windows version 25 (SPSS Inc., Chicago, IL, USA).
Results: Out of 600 participants, the overall prevalence of IPIs was 66.3% (398/600). The prevalence rate of protozoan infections (56.3%, 338/600) was largely higher than helminthic infections (10%, 60/600). The most common intestinal parasite was E. histolytica/dispar (28.5%, 171/600). S. mansoni infection showed higher infection rate in males (5.3%) than in females (0.4%), with statistically significant difference (P = 0.001). Univariate analysis showed that the age was only significantly associated with protozoan infections, with statistically significant differences (P = 0.002). Regarding to clinical symptoms, the presence of IPIs was significantly associated with diarrhea, dysentery, and abdominal pain.
Conclusion: The present study revealed that there was a relatively high prevalence of IPIs, especially protozoan parasites, in schoolchildren of the study area, with E. histolytica/dispar being the most prevalent parasite. The results showed that age was only significantly associated with IPIs. According to the results of this study, IPIs are still among the main public health problems in the study area. Thus, effective prevention and control strategies are important to reduce the incidence of IPIs in this area of the country.
Keywords: prevalence, intestinal parasitic infections, schoolchildren, Yemen
Introduction
Intestinal parasitic infections (IPIs), caused by enteric protozoa and helminths, are among the main public health problems, which increase the morbidity and mortality among infected people in the world.1 About 25% of the world population are infected with intestinal parasites, with high prevalence in developing countries.2 The main reasons for the high prevalence of IPIs in developing countries are poor sanitation conditions, increasing population density, poor personal hygiene, inadequate toilet facilities, inadequate water sanitation, contaminated food and water, and malnutrition as a consequence of poverty.3 In comparison with people of other ages, the high prevalence of IPIs has been reported in children.4 This age group is predisposed to heavy infection with intestinal parasites, because children have not fully developed immune systems and due to their habits related to playing with soil, which may be fecal contaminated.5 The main clinical signs and symptoms of IPIs include abdominal pain, nausea and vomiting, bloating, and weight loss.6 The serious complications of IPIs in children can include malabsorption, dyspepsia, iron deficiency anemia, growth retardation, vitamin A deficiency, weight loss, poor educational performance, and other physical and mental consequences.6
Amebic dysentery (caused by Entamoeba histolytical) and giardiasis (caused by Giardia lamblia) are the two most prevalent protozoan infections, infecting about 500 million and 200 million people, respectively.7 With respect to helminthic infections, Ascaris lumbricoides, Trichuris trichiura, and hookworms are the most predominant causes and have been estimated to affect more than two billion people in the world.8
Many studies on the prevalence of IPIs and associated risk factors have been conducted in different countries worldwide. There are few studies on IPIs conducted in different places in Yemen, including Sana’a,9,10 Taiz,11,12 Ibb,5,13 Hadhramout,14 Al-Mahweet,15 and Sadah.16 In Ibb governorate, the previous studies, with their scarcity, were not representative for the governorate and risk factors for IPIs were not included. Therefore, the main objective of this study was to determine the prevalence of IPIs (both protozoans and helminths) and associated factors among schoolchildren in Ibb governorate. Such studies are important to design and implement effective prevention and control strategies, as well as to provide complementary data to convince policymakers that these infections remain important.
Methods
Study Area
This study was carried out in Ibb governorate, southwest Yemen, which is located about 193 km south of Sana’a at the geographical coordinates of 13°58′N 44°10′E. It has an area of 5344 km,2 and it is the third largest governorate in the country in terms of population (2,892,000), which constitutes 10.8% of the total country population. The governorate has a mild climate throughout the year, and the annual precipitation rate is more than 1000 mm. Agriculture is the main economic activity in this governorate.
Study Design and Population
A cross-sectional study was conducted during the period February to April 2020 in Ibb governorate. The target population was schoolchildren of the basic education (from grade 1 to 9). Out of 20 districts of Ibb governorate, only 6 districts, namely Al-Qafr, Reef Ibb, Badan, Al-Mashannah, Al-Udayn, and Giblah districts (Figure 1), were randomly selected. Schoolchildren were divided into three age groups. By using age category, the actual number of schoolchildren participated in this study were selected by simple random sampling technique.
 |
Figure 1 Map of Yemen showing Ibb governorate and the six surveyed districts. |
Sample Size Determination
The total number of enrolled schoolchildren in Ibb governorate in the academic year 2019/2020 was 640,198 (346,072 males and 294,126 females). The sample size adequate for estimating prevalence of IPIs was determined according to the formula: n = Z2 P (1-P)/d2, where P = prevalence of IPIs from a previous study in the area, d = marginal error (at 5%), and Z = standard score corresponds to 1.96. Since there was a previous study conducted in some regions of Ibb governorate,5 57.4% prevalence rate of IPIs was taken. Accordingly, the minimum sample size determined for this study was 376. To increase the precision of the results, the sample size was increased to be 600 participants.
Socio-Demographic Information
After explaining the purpose of study and before specimen and data collection, consent for participation was taken from the parents/guardians of the schoolchildren. Socio-demographic data of schoolchildren were collected through pre-designed, structured questionnaires. The questionnaire was initially developed in English and then translated into Arabic language (participant’s mother tongue). The schoolchildren (parents or guardians in the case of younger children) were interviewed to obtain information about gender, age, water supply status, contact with domestic animals, contact with soil, and clinical symptoms.
Stool Specimen Collection and Examination
After collecting the socio-demographic data, fecal specimens were collected and processed according to WHO guidelines.17 A single fresh stool specimen (~2 g) was collected from each schoolchild into a clean and labeled plastic container with an applicator stick and properly mixed with 10 mL of 10% formalin for preservation. All fecal specimens were transported to the Laboratory of Parasitology, Faculty of Allied Medical Sciences, Aljazeera University. All specimens were examined macroscopically to identify the presence of adult or segments of helminths. After macroscopic examinations, all fecal specimens were processed using saline and iodine wet mount and formal-ether concentration techniques to identify the presence of protozoa (cysts or trophozoites) and helminths (ova or larvae) according to their size and morphology. The slides were examined initially using a magnification power of 10x objective and then by 40x objective of the compound microscope.
Statistical Analysis
Data were analyzed using SPSS for Windows version 25 (SPSS Inc., Chicago, IL, USA) based on the study purposes. Pearson’s Chi-square (χ2) test was performed where appropriate to identify any association between the prevalence of IPIs and socio-demographic characteristics. Adjusted odds ratios (AOR) with 95% confidence intervals (CI) were estimated to assess the strength of associations. Logistic regression was used to detect risk factors of IPIs. The P values <0.05 were considered significant.
Results
Socio-Demographic Profile of the Study Participants
A total of 600 schoolchildren were participated in this study. Among participants, 373 (62.2%) were males and 227 (37.8%) were females. The age of the participants ranged from 7 to 15 years and was grouped into three age categories (i.e. 7–9, 10–12, and 13–15 years). The category 7–9 years comprised 213 (35.5%), while the categories 10–12 and 13–15 years comprised 256 (42.7%) and 131 (21.8%), respectively. A total of 213 (35.5%) of the participants were used treated water. A total of 346 (57.7%) of the participants were reported to be in contact with domestic animals and 469 (78.2%) of the participants were in contact with the soil.
Prevalence of IPIs
The overall prevalence of IPIs among schoolchildren in the study area was 66.3% (398/600), but the prevalence rate of protozoan infections (56.3%, 338/600) was largely higher than helminthic infections (10%, 60/600). Nine species of intestinal parasites were identified from the stool specimens of the study participants; six species were identified as helminths and the other three species were protozoans (Table 1). The most common intestinal parasite was E. histolytica/dispar (28.5%, 171/600), followed by Entamoeba coli (19.5%, 117/600), G. lamblia (8.3%, 50/600), Schistosoma mansoni (3.5%, 21/600), and Hymenolepis nana (3.2%, 19/600). The least frequently encountered parasites were Enterobius vermicularis (1.5%, 9/600), Taenia saginata (1.1%, 7/600), T. trichiura (0.5%, 3/600), and A. lumbricoides (0.2%, 1/600).
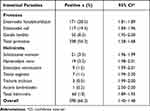 |
Table 1 Prevalence of Intestinal Parasitic Infections Among Schoolchildren in Ibb Governorate, Southwest Yemen, from February to April 2020 (n = 600) |
Distribution of IPIs Based on Gender
According to the results presented in Table 2, there was no statistically significant difference between the overall infection rates with protozoa according to the gender. The results showed comparable infection rates in males and females with E. histolytica/dispar (26.5 vs 31.7%, respectively) and G. lamblia (8 vs 8.8%, respectively), with no statistically significant differences. The same finding was also observed in helminthic infections. However, S. mansoni infection showed higher infection rate in males (5.3%) than in females (0.4%), with statistically significant difference (P = 0.001).
 |
Table 2 Prevalence of Intestinal Parasitic Infections by Gender Among Schoolchildren in Ibb Governorate, Southwest Yemen, from February to April 2020 |
Distribution of IPIs in Different Age Groups
Based on the results presented in Table 3, the results showed comparable overall infection rates among different age groups (7–9, 10–12, and 13–15 years) for protozoan infections (61, 58.9, and 43.5%, respectively), with statistically significant differences (P = 0.002). The results also showed comparable overall infection rates among different age groups for helminthic infections (7.9, 8.9, and 15.2%, at the same order), with no statistically significant differences (P = 0.222).
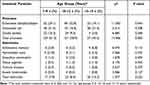 |
Table 3 Prevalence of Intestinal Parasitic Infections by Age Among Schoolchildren in Ibb Governorate, Southwest Yemen, from February to April 2020 |
Risk Factors Associated with IPIs
The results of the univariate analysis to evaluate the risk factors associated with IPIs were presented in Table 4. The results showed that no significant associations were found between IPIs and gender (P = 0.144), treatment of drinking water (P = 0.660), contact with domestic animals (P = 0.817), and contact with soil (P = 0.855). However, the results showed that the age (P = 0.011) was only significantly associated with IPIs among the participants.
 |
Table 4 Risk Factors Associated with IPIs Among Schoolchildren in Ibb Governorate, Southwest Yemen, from February to April 2020 |
Clinical Features Associated with IPIs
Regarding the clinical symptoms (Table 5), the presence of IPIs was significantly associated with diarrhea (P = 0.040), dysentery (P = 0.000), and abdominal pain (P = 0.048). However, there was no significant difference regarding nausea and vomiting (P = 0.114).
 |
Table 5 The Clinical Features Among Schoolchildren in Ibb Governorate, Southwest Yemen, from February to April 2020 |
Discussion
Yemen is one of the poorest countries in the world, with more than 60% of the population residing in rural areas,18 making it vulnerable to the spread of parasitic infections. In the present study, the overall prevalence of IPIs was 66.3%, with a predominance of protozoan compared to helminthic infections (56.3 vs 10%). The finding of the present study was higher than that reported among schoolchildren in a previous study in some regions of Ibb governorate (57.4%)5 and in Sana’a (54.8%).9 However, lower rates of IPIs were reported among schoolchildren in Sahar, Sadah (14.9%)16 and in Taiz (27.8%).11 In contrast, a higher prevalence rate was reported among primary schoolchildren in Al-Mahweet city (90.0%).15 In comparison with other countries, the result of this study was nearly similar to prevalence rate reported by Sitotaw et al3 in Jawi town, Ethiopia (57.9%) and higher than reports from Jeddah, Saudi Arabia (5.3%)19 and Derna, Libya (31%).20 The differences between the prevalence rates can be attributed to varied characteristics of the study population, differences in sample size, socio-economic conditions, hygienic conditions, geographical distribution, and diagnostic techniques employed on the participants. High prevalence of IPIs is a direct manifestation of poor environmental sanitation and low level of awareness.21 A huge variation in the sensitivity of wet mount and formal-ether concentration techniques in the diagnosis of intestinal parasites was documented.22 However, low prevalence rates may reflect either the outstanding and hygienic care or the fault pertained in sample selection.
In the present study, the most prevalent intestinal parasite was E. histolytica/dispar, with prevalence rate of 28.5%, which was lower than the finding of Alsubaie et al5 (33.7%) from some regions of Ibb governorate, but to some extent, it was in agreement with those reported among schoolchildren in Sana’a, Yemen (21.5%),9 and Bahir Dar, Ethiopia (24.5%).21 However, the present finding revealed high prevalence of E. histolytica/dispar in comparison with 16.4% in Taiz, Yemen,11 15.5% in Khartoum, Sudan,23 and 6.6% in Derna, Libya.20 In contrast to the finding of this study, high prevalence rates of E. histolytica/dispar were reported from Al-Mahweet, Yemen (64%),15 Burkina Faso, West Africa (66.5%),24 and Kigali, Rwanda (54.5%).25 The differences in prevalence rates of E. histolytica/dispar from different studies might attribute to potable water contamination, food contamination, and unhygienic practices, such as not washing hands before eating foods or meals.
Although E. coli was the second most prevalent parasite among schoolchildren in the present study (19.5%), it is non-pathogenic. Therefore, G. lamblia was considered the second most prevalent pathogenic parasite, with a prevalence rate of 8.3%, which was lower than the finding of Alsubaie et al5 from the same study area (23.6%), and with those reported among schoolchildren from Taiz, Yemen (2.1%),11 Sana’a, Yemen (16.1%),9 Hadhramout, Yemen (19.2%),14 and Bahir Dar, Ethiopia (11.4%).21 These variations in the prevalence rates of G. lamblia infection in different studies could be attributed to the difference in levels of water contamination and parasitological methods used during the study. In the present study, the overall prevalence of IPIs in schoolchildren, who used untreated water (56.3%), was slightly higher than those used treated water (54.4%), but with no statistical difference (P = 0.660).
Regarding the helminthic infections, they showed low prevalence rates in comparison with protozoan infections, which was in agreement with other findings reported from some regions of the study area.5,13 Among helminths, S. mansoni (3.5%) and H. nana (3.2%) were the most prevalent parasites in the present study, whereas negligible rates of 1.5, 1.1, 0.5, and 0.2% were observed for E. vermicularis, T. saginata, T. trichiura, and A. lumbricoides, respectively. S. mansoni infections were reported among schoolchildren from different parts of Yemen, notably Ibb (3.1%),5 Sadah (2.2%),15 Sana’a (2.6%),9 and Taiz (0.8%).11 These low rates could be attributed to the praziquantel mass administration campaigns to schoolchildren accompanied with health education by local media.
A. lumbricoides was the lowest prevalent parasite in this study (0.2%). This result does not agree with previous reports that reported high prevalence rates for this parasite (1.6–21%) in different parts of the country.5,9–11,13,15 On the other hand, the absence of hookworms and Strongyloides stercoralis among schoolchildren in the present study is consistent with other previous studies.9,10,13 However, low prevalence rates of 1.2 and 0.8% were reported for hookworms and S. stercoralis, respectively, among schoolchildren in some regions of the same study area.5 Low rates of helminthic infections are due to the mass albendazole administration campaigns to schoolchildren and may also account for the lower rates of infections with helminths than those with protozoa in the present study.
Although being easily persistent infection due to autoinfection, the present study revealed low prevalence rates of H. nana (3.2%) and E. vermicularis (1.5%) among schoolchildren in Ibb governorates. In general, the rates of 1.4–17.5% for H. nana and <0.5–13% for E. vermicularis were reported among schoolchildren from different Yemeni governorates.5,9–11,13–15,26 The presence of T. saginata among the participants of the present study was compatible with the findings of other studies in the country, with prevalence rates of 0.5–3%.10,14,15 Generally, the low rates of helminthic infections in the study area could be attributed to the annual campaigns, which are effective in lowering the prevalence and transmission of the helminthic infections. Therefore, the minimal package of activities to control helminthic infections should be continued.
With respect to the risk factors tested, age, but not the gender or other risk factors, was a predictor of increased risk of exposure to IPIs among schoolchildren in Ibb governorate. Such a difference could be justified by the fact that the youngest group is more exposed to infection sources as a result of its habits related to playing and other outdoor activities and this finding was inconsistent with that reported among schoolchildren in some regions of the study area5 and with a recent finding among schoolchildren from Taiz,11 but did not agree with a previous study carried out in Sana’a,9 which reported that gender was a predictor of increased risk of exposure to IPIs.
Considering the clinical symptoms, the results of this study showed that there were significant associations (P < 0.05) between the presence of IPIs and the presence of diarrhea, dysentery, and abdominal pain. Diarrhea is considered as one of the most reported symptoms due to IPIs. E. histolytica can cause severe dysentery, tenesmus, colitis, and extra-intestinal amebiasis, while G. lamblia is responsible for acute diarrhea, steatorrhea, and malabsorption.6
Compared to other studies conducted in some regions of Ibb governorate, the strengths of this study are the large sample size, coverage of different areas in the governorate, and evaluation of the risk factors for IPIs.
There were some limitations in this study. The major limitation of this study is examination of single stool specimen of each study participant. Analysis of three consecutive stool samples could have increased the diagnostic sensitivity. Another limitation was the absence of financial support, which restricted the authors not to use more advanced methods, such as Kato-Katz, Harada-Mori, and Baermann techniques.
Conclusion
The present study revealed that there was a relatively high prevalence of IPIs, especially protozoan parasites, in schoolchildren of Ibb governorate, southwest Yemen, with E. histolytica/dispar being the most prevalent parasite. The results showed that age was only significantly associated with IPIs. In addition, the presence of IPIs was significantly associated with diarrhea, dysentery, and abdominal pain. According to the results of the current study, IPIs continue to be among the main public health problems in the study area. Thus, a mass chemotherapeutic intervention and effective prevention strategies are important to reduce the incidence of IPIs in schoolchildren of the study area.
Ethics Approval and Consent to Participate
The research proposal was initially submitted to the Department of Medical Laboratories, Aljazeera University, which referred it to the Ethical Review Committee of the Faculty of Allied Medical Sciences, Aljazeera University, and ethical approval (Reference Number: 0112/on 29 December 2019) was obtained for this study. For formal communication with the schools of selected districts, a letter describing the objective of the study was written to the Education Office of Ibb governorate. After explaining the purpose and benefit of the study and before specimen and data collection, consent for participation was taken from the parents/guardians of schoolchildren. This study was fully conducted in accordance with the Declaration of Helsinki. Schoolchildren with positive results of IPI were communicated to their parents or guardians, who were advised to contact the nearest health center for proper treatment.
Acknowledgments
The authors would like to thank Aljazeera University, Ibb, Yemen, for providing the facilities and labs to conduct this study. Special thanks are extended to the head teachers and staff of the schools of study area for their assistance, as well as for the schoolchildren for their participation in the study. The authors would also like to thank Dr Hady Al-Sulaihi for his assistance in drawing the map of Yemen showing the study area.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gholipoor Z, Khazan H, Azargashb E, et al. Prevalence and risk factors of intestinal parasite infections in Mazandaran Province, North of Iran. Clin Epidemiol Glob Health. 2020;8(1):17–20. doi:10.1016/j.cegh.2019.03.010
2. World Health Organization. Urges governments to increase investment to tackle neglected tropical diseases; 2015. Available from: https://www.afro.who.int/news/who-urges-governments-increase-investment-tackle-neglected-tropical-diseases.
3. Sitotaw B, Mekuriaw H, Damtie D. Prevalence of intestinal parasitic infections and associated risk factors among Jawi primary school children, Jawi town, north-west Ethiopia. BMC Infect Dis. 2019;19(1):341. doi:10.1186/s12879-019-3971-x
4. Gebretsadik D, Tesfaye M, Adamu A, et al. Prevalence of intestinal parasitic infection and its associated factors among school children in two primary schools in Harbu Town, North East Ethiopia: cross-sectional study. Pediatric Health Med Ther. 2020;11:179–188. doi:10.2147/PHMT.S252061
5. Alsubaie ASR, Azazy AA, Omer EO, et al. Pattern of parasitic infections as public health problem among school children: a comparative study between rural and urban areas. J Taibah Univ Med Sci. 2016;11(1):13–18. doi:10.1016/j.jtumed.2015.10.006
6. Paniker CKJ. Paniker’s Textbook of Medical Parasitology.
7. Barry MA, Weatherhead JE, Hotez PJ, et al. Childhood parasitic infections endemic to the United States. Pediatr Clin North Am. 2013;60(2):471–485. doi:10.1016/j.pcl.2012.12.011
8. World Health Organization. Soil-transmitted helminthiases: eliminating as public health problem soil-transmitted helminthiases in children: progress report 2001–2010 and strategic plan 2011–2020; 2012. Available from: https://apps.who.int/iris/handle/10665/44804.
9. Al-Mekhlafi AM, Abdul-Ghani R, Al-Eryani SM, et al. School-based prevalence of intestinal parasitic infections and associated risk factors in rural communities of Sana’a, Yemen. Acta Trop. 2016;163:135–141. doi:10.1016/j.actatropica.2016.08.009
10. Azazy AA, Al-Tiar S. A study survey on intestinal and blood parasites among school children in Sana’a province, Yemen. Saudi Med J. 1999;20(6):422–424.
11. Alharazi T, Bamaga OA, Al-Abd N, et al. Intestinal parasitic infection: prevalence, knowledge, attitude, and practices among schoolchildren in an urban area of Taiz city, Yemen. AIMS Public Health. 2020;7(4):769–777. doi:10.3934/publichealth.2020059
12. Al-Shamiri A, Al-Zubairy A, Al-Mamari R. The prevalence of Cryptosporidium spp. in children, Taiz District, Yemen. Iran J Parasitol. 2010;5(2):26–32.
13. Qasem EA, Edrees WH, Al-Shehari WA, et al. Frequency of intestinal parasitic infections among schoolchildren in Ibb City-Yemen. Univers J Pharm Res. 2020;5(2):42–46.
14. Al-Haddad AM, Baswaid SH. Frequency of intestinal parasitic infection among children in Hadhramout governorate (Yemen). J Egypt Soc Parasitol. 2010;40(2):479–488.
15. Alwabr GMA, Al-Moayed EE. Prevalence of intestinal parasitic infections among school children of Al-Mahweet Governorate, Yemen. Eur J Biol Res. 2016;6:2.
16. Raja’a YA, Mubarak JS. Intestinal parasitosis and nutritional status in schoolchildren of Sahar district, Yemen. East Mediterr Health J. 2006;12(Suppl 2):S189–S194.
17. World Health Organization. Basic laboratory methods in medical parasitology; 1991. Available from: https://apps.who.int/iris/handle/10665/40793.
18. The World Bank. World development indicators: rural environment and land use; 2017. Available from: http://wdi.worldbank.org/table/3.1.
19. Bakarman MA, Hegazi MA, Butt NS. Prevalence, characteristics, risk factors, and impact of intestinal parasitic infections on school children in Jeddah, Western Saudi Arabia. J Epidemiol Glob Health. 2019;9(1):81–87. doi:10.2991/jegh.k.190219.001
20. Sadaga GA, Kassem HH. Prevalence of intestinal parasites among primary schoolchildren in Derna District, Libya. J Egypt Soc Parasitol. 2007;37(1):205–214.
21. Hailegebriel T. Prevalence of intestinal parasitic infections and associated risk factors among students at Dona Berber primary school, Bahir Dar, Ethiopia. BMC Infect Dis. 2017;17(1):362. doi:10.1186/s12879-017-2466-x
22. Yimer M, Hailu T, Mulu W, et al. Evaluation performance of diagnostic methods of intestinal parasitosis in school age children in Ethiopia. BMC Res Notes. 2015;8:820. doi:10.1186/s13104-015-1822-4
23. Muhajir A, Hajissa K, Mohamed Z, et al. Prevalence of intestinal parasitic infection among children in al-kalakla, Khartoum, Sudan. World Appl Sci J. 2017;35(2):219–222. doi:10.5829/idosi.wasj.2017.219.222
24. Erismann S, Diagbouga S, Odermatt P, et al. Prevalence of intestinal parasitic infections and associated risk factors among schoolchildren in the Plateau Central and Centre-Ouest regions of Burkina Faso. Parasit Vectors. 2016;9(1):554. doi:10.1186/s13071-016-1835-4
25. Niyizurugero E, Ndayanze JB, Bernard K. Prevalence of intestinal parasitic infections and associated risk factors among Kigali Institute of Education students in Kigali, Rwanda. Trop Biomed. 2013;30(4):718–726.
26. Al-Mekhlafi HM. The neglected cestode infection: epidemiology of Hymenolepis nana infection among children in rural Yemen. Helminthologia. 2020;57(4):293–305. doi:10.2478/helm-2020-0038
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
