Back to Journals » International Journal of General Medicine » Volume 16
Prevalence of Hypertension and Its Association with Cardiovascular Risk Factors in College Students in Hunan, China
Authors Li M, Cui X, Meng Y, Cheng M, He J, Yuan W, Ni J , Liu J
Received 24 June 2022
Accepted for publication 18 January 2023
Published 3 February 2023 Volume 2023:16 Pages 411—423
DOI https://doi.org/10.2147/IJGM.S379957
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mingpeng Li,1,2,* Xiaorui Cui,3,* Yanbin Meng,4 Mengli Cheng,4 Jinsong He,3 Wei Yuan,3 Jing Ni,5 Jianping Liu6
1Department of Cardiovascular, Chenzhou No. 1 People’s Hospital, Chenzhou, People’s Republic of China; 2The First Affiliated Hospital of Xiangnan University, Chenzhou, People’s Republic of China; 3Department of Neurology, Affiliated Hospital of Xiangnan University, Chenzhou, People’s Republic of China; 4Xiangnan University, Chenzhou, People’s Republic of China; 5Hunan University of Science and Technology, Xiangtan, People’s Republic of China; 6Institute of Cardiovascular and Cerebrovascular Diseases, Xiangnan University, Chenzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianping Liu, No. 25 Renmin West Road, Chenzhou, 423000, People’s Republic of China, Email [email protected]
Background: Although the prevalence of hypertension has been well studied in middle age and elderly populations, few studies have systematically investigated the prevalence of hypertension and its association with cardiovascular and cerebrovascular risk factors in young populations.
Objective: This study examined the prevalence of hypertension in college students and its correlation with cardiovascular and cerebrovascular risk factors, such as neck circumference and body mass index (BMI).
Methods: This population-based study recruited a total of 1719 students (723 were junior, 502 were sophomore, and 494 were freshman), including 996 males (average age: 20.8 years) and 723 females (average age: 20.4 years). Hypertension was defined by the 2018 revised edition of the Chinese Guidelines for Prevention and Treatment of Hypertension. Blood and pulse pressure were measured using standard protocols. Circulating levels of lipids, glucose, glycosylated hemoglobin (GHb), leptin, and adiponectin were determined using standard methods. The Chi-squared (χ2) test was used for comparison of significant differences between groups. Linear and logistic regression analyses were used to explore risk factors that significantly influence hypertension.
Findings: The prevalence of hypertension was 10.59% in the total cohort, and sophomores had a higher prevalence of hypertension than freshmen and juniors (χ2 = 19.372; P < 0.001). In addition, male students had a significantly higher prevalence of hypertension (10.24%) and abnormal pulse pressure (8.13%) than female students (1.4% and 0.83%) (χ2 = 327.424, P < 0.001 for high SBP and χ2 = 60.49, P < 0.001 for high DBP, respectively). Correlation analysis revealed that hypertension was significantly correlated with neck circumference and BMI (r = 0.509, P < 0.001; r = 0.474, P < 0.001), but not significantly correlated with the other parameters examined.
Conclusion: The prevalence of hypertension in college students is closely correlated with two obesity indicators, neck circumference and BMI.
Keywords: cardiovascular and cerebrovascular events, college students, correlation, hypertension, risk factors
Introduction
Cardiovascular and cerebrovascular diseases are the leading cause of death worldwide, and hypertension is the major risk factor for the development of cardiovascular and cerebrovascular diseases.1 A recent review on the global epidemic of hypertension suggested that the prevalence of hypertension in the adult population globally was 31.1% (1.39 billion);2 it is higher in older adults than younger adults.3 The risk factors for hypertension have been well documented, two of which are gender and age. For example, a survey performed in 2016 suggested that 70% of the older population had hypertension, compared with 32% of the population aged 40–59 years, and 7.5% of the population aged 20–34 years.3
It has also been well established that men have a higher prevalence of hypertension than women before the onset of menopause.3,4 In addition, it has been well documented that cardiovascular and cerebrovascular diseases have other risk factors, such as obesity and blood lipids.5,6 These demographic and epidemic data are important for designing guidelines to prevent hypertension to reduce the incidence of cardiovascular and cerebrovascular diseases in the general population.
Although the prevalence of hypertension has been well studied in middle age and elderly populations, the systemic investigation of hypertension prevalence in younger populations has not been well explored to date, particularly in China. Previously, three large-scale epidemiological surveys of hypertension were performed in 1959, 1979, and 1991 in China,7 to gain insights into the prevalence of hypertension and played an important role in defining guidelines for its prevention and treatment. However, in these guidelines and revisions, there was a lack of guidelines for the prevention and treatment of hypertension in younger populations—particularly college students. In 2012, one survey reported that the national prevalence of hypertension among adults aged ≥ 18 years was approximately 25.2%.8 However, that study not only included young people around 18–25 years old, but it also included those aged over 40 years.
Although some studies have investigated the prevalence of hypertension in college students in different cities of China, given that the epidemiology of hypertension is related to race and social customs, including eating habits,9 it is important to conduct a survey on the prevalence of hypertension in college students in Hunan, China. Moreover, it is imperative to elucidate the potential correlations between hypertension and those risk factors in young populations.
In the present study, we investigated the prevalence of hypertension in a cohort of college students in Hunan, China. Given that obesity, high blood lipids, blood glucose, and glycosylated hemoglobin (GHb) are all known risk factors for cardiovascular and cerebrovascular diseases, we also systemically examined the correlations between hypertension and these factors in our study cohort. This study aimed to uncover the prevalence of hypertension in college students and its correlation with cardiovascular and cerebrovascular risk factors.
Materials and Methods
Subject Selection
This population-based study was conducted in 2016. This study enrolled freshman (2015 enrollment), sophomore (2014 enrollment), and junior (2013 enrollment) students at a college in the southern part of Hunan Province, China, using a multistage stratified random cluster sampling method. Briefly, 20,000 college students in Xiangnan University in southern Hunan were first divided into two groups: medical majors and non-medical majors. Then, in each group, the freshman, sophomore, and junior students were randomly selected according to the proportion of the number of classes in the grade. A total of 1795 students aged 17–26 years were initially randomly selected for this study, including 1151 medical students, 356 science and engineering students, and 288 music and physical education students.
A total of 1722 students answered the questionnaire. Among them, 3 students had no blood pressure (BP) measurement data, and eventually 1719 students who provided valid BP data were enrolled in this study, including 996 males with an average age of 20.797 years and 723 females with an average age of 20.448 years. These 1719 participants included 1117 medical students, 335 science and engineering students, and 267 music and physical education students, among whom 723 were juniors, 502 were sophomores, and 494 were freshmen.
The study protocol was approved by the ethics committee of the Affiliated Hospital of Xiangnan University, and all participants were aware of this study and signed informed consent forms. All study procedures were conducted in accordance with the principles of the Declaration of Helsinki.
BP Measurement
Blood pressure (BP) was measured according to “China Blood Pressure Measurement Guide.”10 Briefly, participants rested for about 15 minutes and were not allowed to smoke during the 2 hours prior to BP measurement. Participants were also required to empty their bladder, avoid drinking coffee, and avoid betel nuts and other foods that could affect BP. The rooms where the BP measurement took place were equipped with an air conditioner, tables, and high back chairs that could be adjusted to be suitable for BP measurement of subjects in the sitting position. The BP in the brachial artery of each subject’s right upper arm was measured twice over a 2-minute interval using a desktop sphygmomanometer (Hangzhou Yuyue, China) and a stethoscope (Hangzhou Yuyue, China); the average of the two measurements was used for the data analysis.
BP was classified into the following three levels based on the 2018 revised edition of the Chinese Guidelines for Prevention and Treatment of Hypertension:11 (1) hypertension if a systolic blood pressure (SBP) was ≥ 140 mmHg and/or a diastolic blood pressure (DBP) ≥ 90 mmHg; (2) high-normal BP (ie, prehypertension) if a SBP was 120–139 mmHg and/or a DBP was 80–89 mmHg; and (3) normal BP if a SBP/DBP was <120/80 mmHg. Hypertension was then further classified and stratified according to the diagnostic criteria for hypertension.
Neck Circumference Measurement
Participants sat in a vertical position, looking straight ahead, breathing calmly, and a soft tape measure was placed on the lower edge of participants’ laryngeal knot. The neck circumference was measured horizontally to the nearest 0.1 cm. Women with a neck circumference ≥35 cm and men with a neck circumference ≥40 cm were defined as being obese.
Measurement of Waist and Hip Circumference
Participants stood upright with their arms slightly extended, with their feet together and weight evenly loaded, and breathing calmly. Using a soft tape measure placed close to the skin, waist circumference was measured 2 cm above the level of the umbilicus, and hip circumference was measured at the tip of the trochanter. The measurement was accurate to 0.1 cm. Women with a waist circumference greater than or equal to 85 cm, and men with a waist circumference greater than or equal to 90 cm were defined as being obese.
Height and Weight Measurements
Participants took off their shoes and hats (if any), stood upright, looked straight ahead, removed heavier items from their pockets, and wore thin underwear. Weight and height were measured with an accuracy to 0.1 cm and to 0.1 kg, respectively.
Waist-to-Height Ratio and Body Mass Index (BMI)
The waist-to-height ratio was calculated as the ratio of the waist circumference to height, and was generally below 0.5. BMI was defined as body weight divided by height squared (kg/m2). Criteria to evaluate the relationship between body weight and obesity were as follows: low body weight (< 18.5 kg/m2), normal body weight (18.5–23.9 kg/m2), overweight (24.0–27.9 kg/m2), and obesity (≥ 28 kg/m2).
Measurements of neck circumference, waist circumference, height, body mass index (BMI), and their association with obesity were based on the “Guidelines for the Prevention and Control of Overweight and Obesity in Adults in China”.12
Statistical Analysis
All researchers were appropriately trained to perform physical examinations, including BP measurement and data collection. A database was generated by double entry by two researchers using EpiData Entry v3.1 software. All statistical analyses were performed using SPSS v20.0 (IBM SPSS, Statistics, Chicago, IL, USA) statistical software. Data normality was tested using the Kolmogorov–Smirnov method. The measurement data are expressed as mean ± standard deviation (SD), and the count data are expressed as n (%). The Chi-squared (χ2) test was used for comparison of significant differences between groups, as appropriate. Linear and logistic regression analyses were used to explore risk factors affecting SBP, DBP, and PP with regression coefficients and 95% confidence intervals. “Crude model” was a single factor analysis, in which the regression coefficient value and 95% credible interval were obtained after each independent variable was taken into account. “Model 1” was the multi-factor adjustment analysis, in which multiple variables were taken into account, including the correlation between sample size and independent variables. A P-value ≤ 0.05 indicates that the difference was statistically significant, and a P-value < 0.001 indicates that the difference was very significant.
Results
Comparison of Demographic and Baseline Characteristics of All Subjects Among Grades
A total of 1719 college students were eventually enrolled in this study. Demographic and baseline characteristics of all subjects based on grades are listed in Table 1. Notably, sophomores had the highest SBP, DBP, and PP, as well as BMI and waist among these three grades. In addition, neck circumference, waist circumference, and waist-to-hip ratio showed significant differences among these three grades.
 |
Table 1 Comparison of Demographic and Baseline Characteristics of All Subjects Among Three Grades |
Prevalence of Hypertension Among College Students
The prevalence of hypertension in this study cohort was 10.59%; the prevalence of hypertension based on the increase in both SBP and DBP was 2.44%, based on only the increase in SBP ≥ 140 mmHg, it was 4.07%, and based on only the increase in DBP ≥ 90 mmHg, it was 4.07% (Figure 1A).
Students who had a SBP ≥ 140 mmHg accounted for 6.5% of the total, those who had a SBP of 120–139 mmHg accounted for 32.58%, and those who had a SBP of < 120 mmHg accounted for 60.91%. Students who had a DBP ≥ 90 mmHg accounted for 6.52%, those who had a DBP of 80–89 mmHg accounted for 25.36%, and those who had a DBP ≤ 80 mmHg accounted for 68.12% (Figure 1B).
Among those 182 hypertensive students, the prevalence of hypertension in sophomore students was higher than that in freshman and junior students (χ2 = 19.372; P < 0.001). There were significant differences in BP between sophomores and freshman (χ2 = 15.79; P < 0.001) and between sophomore and junior (χ2 = 11.225; P < 0.001), but no difference in BP between freshmen and juniors was observed (χ2 = 1.170, P < 0.279) (Figure 1C).
Abnormal BP of College Students is Concentrated in Level 1 Hypertension and High–Normal BP
Based on the hypertension classification of SBP, students with (1) SBP of grade 3 hypertension (≥ 180 mmHg) accounted for 0.12%, (2) SBP of grade 2 hypertension (160–179 mmHg) accounted for 0.93%, (3) SBP of grade 1 hypertension (140–159 mmHg) accounted for 5.47%, (4) high–normal SBP (120–139 mmHg) accounted for 32.58%, and (5) normal SBP < 120 mmHg accounted for 60.91% (Table 2).
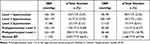 |
Table 2 Classification and Stratification of Blood Pressure Among College Students |
In addition, based on the hypertension classification of DBP, students with (1) DBP of grade 3 hypertension (≥ 110 mmHg) accounted for 0.41%, (2) DBP of grade 2 (100–109 mmHg) accounted for 1.05%, (3) DBP of grade 1 (90–99 mmHg) accounted for 5.24%, (4) DBP of the high–normal BP range (80–89 mmHg) accounted for 25.36%, and (5) normal DBP < 80 mmHg accounted for 67.9% (Table 2). Taken together, the abnormal BP groups were mainly of hypertension grade 1 and high–normal BP. The prevalence of abnormal BP, including both hypertension and high–normal BP, in college students was 51.31% (Tables 2 and 3).
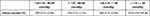 |
Table 3 Analysis of High–Normal BP of College Students |
Male Students Have a Significantly Higher Prevalence of Hypertension Than Female Students
Among those 112 students with a SBP ≥ 140 mmHg, 102 (91.07%) were males, and 10 (8.92%) were females (χ2 = 327.424, P < 0.001) (Table 4). Among the 112 students with a DBP ≥ 90 mmHg, 91 (81.25%) were male and 21 (18.75%) were female (χ2 = 60.49, P < 0.001) (Table 5). We conclude that the prevalence of hypertension is significantly higher in male students than in female students.
 |
Table 4 Comparison of SBP Between Male and Female Students |
 |
Table 5 Comparison of DBP Between Male and Female Students |
Identification of Factors Affecting SBP, DBP and PP
We used multivariable linear regression models to identify factors that can significantly affect SBP, DBP and PP. After multi-factor adjustment, gender, BMI, and neck circumference were the influencing factors of SBP, and the correlations between other variables and SBP were not statistically significant. After multi-factor adjustment, the selected variables and DBP had no significant correlation, but gender and BMI had significant associations with PP. Since the age range was too narrow in this study cohort, whether using age as a variable in this study was of little significance (Table 6).
 |
Table 6 Identification of Factors That Significantly Affect SBP, DBP, and PP |
Among these 1719 students, 136 (7.91%) had a pulse pressure ≥ 60 mmHg, 274 (15.94%) had a pulse pressure of 50–59 mmHg, 391 (22.94%) had a pulse pressure of 41–49 mmHg, and 918 (53.40%) had a pulse pressure ≤ 40 mmHg (Table 7). Our analysis suggested that male students had a significantly higher prevalence of abnormal pulse pressure than female students (Table 6). Given that BMI is currently one of the most commonly used indicators of obesity, we further examined the correlation between abnormal BP and BMI in details. Among these subjects, 228 (13.33%) were overweight (24 ≤ BMI < 28), and 57 (3.33%) were obese (BMI ≥ 28) (Table 8). In the overweight and obese groups, the occurrence rates of hypertension and high–normal BP were significantly higher than those in the normal BMI group (Table 7).
 |
Table 7 Stratification of Pulse Pressure |
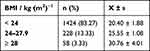 |
Table 8 BMI Distribution Among College Students |
Identification of Risk Factors Associated with Hypertension, High SBP and High DBP
We next used multivariable logistic regression models to identify risk factors that are associated with hypertension, high SBP and high DBP. After multi-factor adjustment, gender was the influencing factor of hypertension (the risk of hypertension in men is 2.29 times that of women), and no significant associations between other variables and hypertension were observed. On the other hand, increased neck circumference was the only risk factor for isolated high SBP (Table 9).
 |
Table 9 Identification of Risk Factors Associated with Hypertension, High SBP, and High DBP |
Correlation Between Hypertension and Blood Lipids, Glucose, GHb, Leptin, and Adiponectin in College Students
We measured the circulating levels of blood lipids, glucose, GHb, leptin, and adiponectin in these students, and then examined their correlations with SBP/DBP. As shown in Tables 6 and 8, no other significant correlations between SBP/DBP with any of these parameters were identified, with the exception that correlation analysis showed that SBP was weakly correlated with glucose in the hypertension group.
Discussion
In the present study, we investigated the prevalence of hypertension in college students in Hunan, China, along with its association with other cardiovascular and cerebrovascular disease risk factors. Our major findings were that the (1) abnormal BP of college students was primarily in hypertension grade I and high–normal BP groups, (2) prevalence of hypertension was higher in male students than in female students, (3) prevalence of hypertension was significantly correlated with neck circumference and BMI, (4) pulse pressure was greater in male students than in female students, and (5) no significant correlations existed between hypertension and circulating levels of lipids, glucose, GHb, leptin, and adiponectin.
Previously, the Tianjin Jinnan District Center for Disease Control and Prevention of China reported that the prevalence of hypertension among university freshmen was 7.72%.13 In another study carried out in 2016, the prevalence of high–normal BP in college students in Jilin Province of China was 31.5%.14
In this study, we reported that the prevalence of hypertension among 1719 college students was 10.59%. In addition, students with a high–normal BP accounted for 32.58% of the total students examined. Our findings are in line with those of previous reports. On the other hand, the China Nutrition and Health Survey (CHNS) published a survey showing that the age-standardized prevalence of high–normal BP increased from 23.9% in 1991 to 33.6% in 2011.15 Based on findings from our group and others, we believe that some young populations have a greater risk of developing hypertension. Since the BP level in youth can reliably predict the BP level in the future,16 early intervention by prevention and/or treatments of hypertension is expected to reduce the risk of cardiovascular and cerebrovascular events in the future in older populations.17 In addition, given that the vast majority of students with abnormal BP were in the hypertension level 1 and high–normal BP groups, we believe that early prevention and treatment should be feasible and will be effective in delaying or stopping the progression of abnormal BP to the next level of hypertension.
In the present study, we selected neck circumference, waist circumference, waist-to-height ratio, and BMI as indicators of overweight and obesity. While waist circumference, waist-to-height ratio, and BMI are well-recognized criteria for the evaluation of overweight and obesity,18,19 the application of neck circumference for the assessment of obesity remains controversial, as it is probably dependent on age and race.20–22
Using Pearson’s statistical analysis, we found that these four indicators, waist circumference, waist-to-height ratio, BMI, and neck circumference, were correlated with SBP and DBP, indicating that obesity and hypertension exhibited a strong correlation.
We also observed that there were positive correlations between hypertension and neck circumference and BMI. BMI was also found to be linked to the risk of hypertension in the middle- and older-age populations in China.23 Moreover, the correlation of hypertension with neck circumference and BMI was independent of other factors, such as gender and age.
Waist circumference and hip circumference are related to the development of secondary sexual characteristics. Male fat is concentrated in the abdomen and hips, while female fat is concentrated in the chest and buttocks. As a result, the waist circumference data of male and female students were quite different, which affected the accuracy of the statistical analysis.
Therefore, compared with waist and hip circumference, neck circumference is a more reliable indicator for evaluating abnormal BP in college students, as it is less affected by gender. In addition, there was a difference in the effect of obesity on SBP and DBP (ie, obesity had more effect on SBP than DBP), although the underlying mechanisms remain undetermined.
Intriguingly, in this study, we found that the prevalence of hypertension in sophomore students was significantly higher than in freshman and junior students, but there was no significant difference in the prevalence of hypertension between freshman and junior students. The exact mechanisms underlying this phenomenon are unclear.
Firstly, we suppose that freshman students had just entered college, and so their course work was not yet as heavy as that of the sophomore students. In addition, prior to entering college, freshman students were required to participate in military training for 1 month, which was intensive physical education that benefited their health. Thus, it was possible that freshman students were more relaxed than sophomore students, which was reflected in their lower BP.
Secondly, junior students generally started professional courses, which require hands-on learning. Thus, the psychological pressure junior students faced was lower than that of sophomore students, which might have a lowering effect on BP.
Thirdly, since sophomore students started the professional basic courses at the time of the study, these required more study time, and students needed to adapt to their difficulty level. Hence, they probably experienced more learning pressure, which might have had a negative impact on BP. In summary. Further studies are warranted to reveal the underlying mechanisms to offer more appropriate guidelines for the prevention of hypertension in college students.
Compared to older adults, we should note that hypertension in young adults is different with regards to hypertension progression and management, especially since older people are more susceptible to frailty.24,25 Hypertensive older adults with frailty may have comorbidities such as cognitive impairment that require additional medications.26 Therefore, hypertension in older adults is more difficult to manage and control than in young adults,27 and usually leads to more adverse cardiovascular outcomes if management is not appropriate and comes timely.28
Previous studies have shown that hypertension is closely associated with the circulating levels of blood lipids, glucose, and GHb.29–31 In addition, the close association between hypertension and the levels of serum leptin and adiponectin in aging populations was also reported. However, we did not detect a significant link between hypertension and any of the above-mentioned factors, although hypertension was closely related to obesity. The discrepancy between our findings and previous ones was probably attributed to the following. Firstly, the study cohorts were different. Our study focused on a young population, and those previous studies were primarily focused on (or included) older populations. Secondly, our sample size was relatively small. Hence, multiple-center studies with a large cohort of young populations are needed to further corroborate our findings in the future.
Conclusion
In conclusion, according to our findings, hypertension in college students is closely correlated with two obesity indicators: neck circumference and BMI. Since abnormal BP in college students is mainly hypertension level I and high–normal BP (ie, pre-hypertension), preventative measures and treatments should be appropriately administered to delay the progression of hypertension to the next level, which may lead to an increased incidence of cardiovascular and cerebrovascular events in older populations.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article [and its Supplementary Information Files].
Ethics and Consent
The study protocol was approved by the ethics committee of the Affiliated Hospital of Xiangnan University, and all participants were aware of this study and signed informed consent forms. All study procedures were conducted in accordance with the principles of the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Key Research of Hunan Provincial Department of Education (17A198), Programs for Science and Technology Development of Hunan Provincial Department of Science and Technology in 2015 (2015SK2011), Scientific Research Plan Project of Hunan Provincial Health Commission (202103071713), Scientific and Technological Development Program of Chenzhou Bureau of Science and Technology (ZDYF201927), and Scientific and Technological Development Program of Chenzhou Bureau of Science and Technology (ZDYF2020170).
Disclosure
The authors declare that they have no competing interests.
References
1. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75(2):285–292. doi:10.1161/HYPERTENSIONAHA.119.14240
2. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223–237. doi:10.1038/s41581-019-0244-2
3. Buford TW. Hypertension and aging. Ageing Res Rev. 2016;26:96–111. doi:10.1016/j.arr.2016.01.007
4. Ramirez LA, Sullivan JC. Sex differences in hypertension: where we have been and where we are going. Am J Hypertens. 2018;31(12):1247–1254. doi:10.1093/ajh/hpy148
5. Chen R, Yan J, Liu P, Wang Z, Wang C. Plasminogen activator inhibitor links obesity and thrombotic cerebrovascular diseases: the roles of PAI-1 and obesity on stroke. Metab Brain Dis. 2017;32(3):667–673. doi:10.1007/s11011-017-0007-3
6. Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;143(21):e984–e1010. doi:10.1161/CIR.0000000000000973
7. Liu B, Yin F, Ma C, et al. Analysis of risk factors for normal young adults with hypertensive family history. Chine J Hypertension. 2008;1(5):441–444.
8. Li L, Rao K, Kong L, et al. Survey on healthy nutrition and status of Chinese residents in 2002. Chine J Epidemiol. 2005;26(7):478–484.
9. Lackland DT. Racial differences in hypertension: implications for high blood pressure management. Am J Med Sci. 2014;348(2):135–138. doi:10.1097/MAJ.0000000000000308
10. Joint Committee for guideline revision. 2010 Chinese Guidelines for Prevention and Treatment of Hypertension. Chine J Hypertension. 2011;9(8):702–709.
11. Liu LS, Wu ZS, Wang JG. 2018 Chinese Guidelines for Prevention and Treatment of Hypertension-A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol. 2019;16(3):182–241. doi:10.11909/j.issn.1671-5411.2019.03.014
12. Chinese Working Group on Obesity. Guidelines for Prevention and Control of Overweight and Obesity in Chinese Adults. Chine J Nutrition. 2004;26(1):1–4.
13. Jin H. Analysis of overweight, obesity and hypertension among freshmen in a university between 2008 to and 2012. J Appl Preventive Med. 2018;24(04):285–287.
14. Zhao L, Zhang X, Wu F, et al. Correlation between prehypertension and obesity, autonomic nervous function, mental health and lifestyle among college students. Modern Preventive Medicine. 2018;45(12):2176–2179+2199.
15. Chinese Cardiovascular Disease Report Writing Group. Summary of “China Cardiovascular Disease Report 2016”. Chine J Circulation. 2017;32(6):521–530.
16. Yang L, Magnussen CG, Yang L, Bovet P, Xi B. Elevated blood pressure in childhood or adolescence and cardiovascular outcomes in adulthood: a systematic review. Hypertension. 2020;75(4):948–955. doi:10.1161/HYPERTENSIONAHA.119.14168
17. Williams B, Mancia G, Spiering W, et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. Blood Press. 2018;27(6):314–340. doi:10.1080/08037051.2018.1527177
18. Seloka MA, Matshipi M, Mphekgwana PM, Monyeki KD. Obesity Indices to Use for Identifying Metabolic Syndrome among Rural Adults in South Africa. Int J Environ Res Public Health. 2020;17(22):8321. doi:10.3390/ijerph17228321
19. Yang H, Xin Z, Feng JP, Yang JK. Waist-to-height ratio is better than body mass index and waist circumference as a screening criterion for metabolic syndrome in Han Chinese adults. Medicine. 2017;96(39):e8192. doi:10.1097/MD.0000000000008192
20. Saka M, Türker P, Ercan A, Kiziltan G, Baş M. Is neck circumference measurement an indicator for abdominal obesity? A pilot study on Turkish Adults. Afr Health Sci. 2014;14(3):570–575. doi:10.4314/ahs.v14i3.11
21. Magalhães EI, Sant’Ana LF, Priore SE. [Waist circumference, waist/height ratio, and neck circumference as parameters of central obesity assessment in children]. Rev Paul Pediatr. 2014;32(3):273–281. Portuguese [Perímetro da cintura, relação cintura/estatura e perímetro do pescoço como parâmetros na avaliação da obesidade central em crianças]. doi:10.1590/0103-0582201432320
22. Tantawy SA, Kamel DM, Alsayed N, Rajab E, Abdelbasset WK. Correlation between body mass index, neck circumference, and waist-Hip ratio as indicators of obesity among a cohort of adolescent in Bahrain: a preliminary cross-sectional study. Medicine. 2020;99(17):e19950. doi:10.1097/MD.0000000000019950
23. You Y, Teng W, Wang J, et al. Hypertension and physical activity in middle-aged and older adults in China. Sci Rep. 2018;8(1):16098. doi:10.1038/s41598-018-34617-y
24. Liu P, Li Y, Zhang Y, Mesbah SE, Ji T, Ma L. Frailty and hypertension in older adults: current understanding and future perspectives. Hypertens Res. 2020;43(12):1352–1360. doi:10.1038/s41440-020-0510-5
25. Ma L, Zhang L, Sun F, Li Y, Tang Z. Frailty in Chinese older adults with hypertension: prevalence, associated factors, and prediction for long-term mortality. J Clin Hypertens. 2018;20(11):1595–1602. doi:10.1111/jch.13405
26. Mone P, Gambardella J, Pansini A, et al. Cognitive impairment in frail hypertensive elderly patients: role of hyperglycemia. Cells. 2021;10(8):2115. doi:10.3390/cells10082115
27. Firdaus M, Sivaram CA, Reynolds DW. Prevention of cardiovascular events by treating hypertension in older adults: an evidence-based approach. J Clin Hypertens. 2008;10(3):219–225. doi:10.1111/j.1751-7176.2008.07428.x
28. Oliveros E, Patel H, Kyung S, et al. Hypertension in older adults: assessment, management, and challenges. Clin Cardiol. 2020;43(2):99–107. doi:10.1002/clc.23303
29. Yan Q, Sun D, Li X, et al. Association of blood glucose level and hypertension in Elderly Chinese Subjects: a community based study. BMC Endocr Disord. 2016;16(1):40. doi:10.1186/s12902-016-0119-5
30. Zhang Y, Zhou C, Li J, et al. Serum alkaline phosphatase levels and the risk of new-onset diabetes in hypertensive adults. Cardiovasc Diabetol. 2020;19(1):186. doi:10.1186/s12933-020-01161-x
31. Bower JK, Appel LJ, Matsushita K, et al. Glycated hemoglobin and risk of hypertension in the atherosclerosis risk in communities study. Diabetes Care. 2012;35(5):1031–1037. doi:10.2337/dc11-2248
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

