Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 12
Prevalence of HIV/AIDS Among Elderly People and Associated Factors in Habru Woreda, Amhara Region, Northeast Ethiopia
Authors Fentaye S, Yibeltal D , Tessema Z
Received 15 June 2020
Accepted for publication 28 August 2020
Published 9 September 2020 Volume 2020:12 Pages 411—423
DOI https://doi.org/10.2147/HIV.S265101
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Shegaw Fentaye,1 Desalegn Yibeltal,2 Zenaw Tessema2
1Integrity Consultancy Service, Addis Ababa, Ethiopia; 2Department of Pharmacy, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Correspondence: Zenaw Tessema
Department of Pharmacy, College of Health Sciences, Debre Markos University, Debre Markos, Ethiopia
Email [email protected]
Introduction: Sub-Saharan African countries are the most affected region by HIV/AIDS. Data from Demographic and Health Survey (DHS) indicated that in Ethiopia older adults who are HIV positive were 2.1% which accounted 17.7% from all HIV positive people aged ≥ 15. Scarce data are available regarding the prevalence of HIV and associated factors among elderly peoples in Habru district.
Objective: To assess the prevalence of HIV and associated factors among older people ≥ 50 years’ age in the study area.
Methods: A community-based cross-sectional study was employed. A multi-stage simple random sampling technique was employed and a total of 1689 study subjects were involved. Data were collected by trained health professionals and analyzed using descriptive and analytical statistics. Binary and multivariate logistic regressions were used to identify factors associated with the prevalence of HIV. P-value ≤ 0.05 was considered statistically significant.
Results: Total of 1689 participants were involved and tested for HIV sero-status of which 51.1% were females and the mean age was 62.4± 12.34 years. The prevalence for HIV+ was 6.2%. From the multivariate regression model, significant association between prevalence and condom use at last sexual intercourse [AOR= 11.099; 95% CI (2.357,52.268)], condom use at high-risk sexual intercourse [AOR=0.088; 95% CI (0.020, 0.398)], marital status [AOR= 0.409; 95% CI (0.252,0.666)], religion [AOR= 0.431; 95% CI (0.241, 773)], types of previous work [AOR= 0.301; 95% CI (0.117, 0.770)], older people self-perception to risk of HIV infection [AOR= 3.731; 95% CI (2.280, 6.104)], care for HIV infected and non-infected grand children [AOR= 0.434; 95% CI (0.235, 800)], presence of care and support program [AOR= 6.128; 95% CI (1.532, 24.514)] was noticed.
Conclusion: The prevalence of HIV in Habru was higher (6.2%) than the national level (2.1%) and efforts should be concentrated on designing new HIV intervention programs targeting older people aged ≥ 50years.
Keywords: HIV/AIDS, elderly, prevalence
Introduction
Globally, the number of elderly HIV-infected patients is increasing. Estimates show that the percentage of people living with HIV aged 50 years and above had increased to more than 17% over the past decade. In sub-Saharan Africa (SSA), estimates show that the percentage will triple by the year 2040. Previous data showed that HIV associated morbidity and mortality were higher in elderly patients as compared to their younger counterparts. More recent studies have also found that old age is associated with rapid progression to AIDS.1 In Canada,8% of the HIV cases and 12% of Acquired immune deficiency disease patients were 50 years and older. In Australia, 14% of individuals with the age of 50 and above were affected by HIV infection of which 90% were men and the death was 17% due to the infection. But in the UK, for the same age group; the case to men and women was 8.5% and 3.8%, respectively. In the united states, around one million persons are infected with HIV and about 40,000 new HIV infections happen every year. Of new HIV/AIDS cases described to the Centers for Disease Control (CDC) in 2005, more than 15% were of 50 ages and older and closely 2% of new identifies were of above 65 years of age.2–4
Most investigations by the United Nations (UN) considered individuals aged 15–49 years. But as compared to this age group, HIV infection is dramatically infecting older aged individuals than ever before.5
The degree of attention countries given to HIV/AIDS infection is different and in some countries, it is limited owing to various reasons. For example, United States provide insignificant attention than the glob due to; Initial, older persons either who have infected themselves or who are pretentious through the infection of others devastatingly are outside the United States, a country represented for less than 2.5% of the thirty-six million persons existing with HIV/AIDS at the close of 2000 where 70% of the infected are from sub-Saharan Africa, and 16% are in South and Southeast Asia.
Second, the degree and nature of the influence on older persons possibly differ in areas of the world where the epidemic is most severe and where the social, cultural, economic, and political backgrounds are dissimilar. Finally, most exploration in the United States emphasize on older persons who are either themselves infected or at high risk of infection and disregards the broader range of consequences that are pertinent for understanding how the epidemic affects older persons internationally.6
The newly described cases of HIV infection in Western Europe reported in 2007 for people of 50 or older were about 12.9% which is higher than central Europe (10%) and Eastern Europe (3.7%).7
Older patients are at an advanced risk of HIV disease headway, due to their intention to be diagnosed at a more progressive stage; slower immunological response to highly active antiretroviral therapies, and being at a higher risk of chronic complications.8
An examination of UNAIDS and World population prospects data recommends that roughly 3 million adults aged ≥50 years are living with HIV in sub-Saharan Africa. People in this age group account for about 14.3% of all HIV seropositive people >15 years of age.3
A study in rural Cameroon presented a prevalence of 2.6% HIV infection among both sex aged 55–70 years, and a study among people admitted to hospital in Dare Salaam, United Republic of Tanzania, stated prevalence of 15% among those aged ≥55. Reviewed data from Demographic and Health Survey (DHS) by WHO for sub-Saharan Africa indicate that the prevalence of older adults who are HIV seropositive people in Ethiopia was 2.1% and HIV positive older adults as a proportion of all HIV positive People aged ≥15 was 17.7%.8 In Ethiopia, the annual number of HIV-infected people showed declining trends since 2002. Over the past two decades, HIV prevalence rate decreased from 3.3% in 2000 to 0.9% in 2017, and AIDS-related deaths from 83 000 deaths in 2000 to 15 600 in 2017. The number of HIV infections among adult Ethiopians was estimated at 722,248 in 2017, increasing by 3748 infections from 2016.9 Literatures revealed that socio-demographic factors, socioeconomic factors, knowledge of HIV/AIDS, behavioural factors, traditions and cultures, risk sexual behaviour and access to HIV health service determined the prevalence of HIV/AIDS (Figure 1).
 |
Figure 1 Conceptual framework on factors showing the commonness of HIV in elderly people. The double arrow point indicated that the variables in each factor affects one another and vice versa. |
Objective
The main aim of this study was to determine the prevalence of human immunodeficiency virus among older people age ≥50 years and to identify associated factors.
Methodology
Study Area
It was conducted in Habru woreda, North Wollo Zone, Amhara Region state, Ethiopia which is 491 Km away from Addis Ababa; the capital city of Ethiopia. It has a latitude and longitude of 11° 44ʹ 59.99” N and 39° 39ʹ 59.99” E, respectively. The total population of the woreda was 210,830, of which 113,867 are males.
Study Period and Design
Community-based quantitative cross-sectional study was performed from March 1/2018- November 30, 2019.
Source Population
The source populations were all older people aged ≥50 years old in Habru woreda, North Wollo zone, Amhara Regional State, North-East Ethiopia.
Study Population
The study populations were all older people aged ≥50 years old who were selected randomly from 8 selected kebeles of the woreda.
Inclusion Criteria
All older people aged ≥50 years old without considering their previous HIV status in Habru woreda.
Exclusion Criteria
Older people aged ≥50 years old who are mentally and physically ill and unable to participate in the study during data collection.
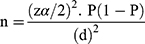
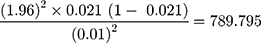
The required Sample size for this study was calculated as per10 assuming that CI =95%; Margin of error (Degree of precision) =1% (0.01); P =2.1%;11 Non-response Rate = 10%; Design effect = 2.
The required sample size was 1738 (adding 10% non-response rate and design effect 2) (Table 1 and Figure 2). A multi-stage Simple Random sampling technique was used for the selection of study subjects. The first eight kebeles (around 21% of all the woreda Kebeles) were selected randomly to represent the woreda. Then, all older people aged ≥50 years old were registered in each randomly selected kebeles before the actual data collection process. After the total number of all older people aged ≥50 years old in each selected kebeles was listed, the sample was proportionally allocated to represent each kebele. Then, by simple random sampling technique, the required sample was taken from the kebeles and the study subjects were called to the nearby Village centers to be provided with mass health education. Each individual was independently asked and counseled for HIV test and an interview was made for the associated factors.
 |
Table 1 Proportional Sample Size Allocation for Each Randomly Selected Study Kebeles in Habru District, Amhara Region, November 2019 |
Study Variables
Presence or Absence of HIV.
- Age, sex, education, marital status, residence, religion.
- Working condition, access to radio and other communication facilities.
- Women decision-making power.
- Condom use.
- Access to HIV-related services.
- The care given by/for older people.
- Behavioral factors.
- Traditions and cultures.
- High-risk sexual behavior.
- Knowledge of HIV/AIDS.
- HIV test.
Sampling Frame
The list of the elderly individuals was recorded at each selected kebele and then this list was used to select the participants systematically by dividing the sample size to the total population and gaining the interval in each kebele.
Data Collection Tools and Procedures
All older people aged ≥50 years old were registered in each randomly designated kebeles and the sample was equivalently assigned to represent each kebele. Then, the data were collected by trained nurses, VCT counselors, and Medical Laboratory professionals to test those individuals for HIV status and two supervisors were involved in the data assortment process. Questionnaires were used to collect data about all the relevant variables. The questionnaires were also pre-tested to identify a possible problem such as; sequences of wording, unanticipated interpretations, and cultural objections to any of the questions in 5% of the respondents having similar characteristics with the study subjects nearby the study area.
Data Processing and Analysis
The data were entered, cleaned, edited, and analyzed by using SPSS version 16. Descriptive statistics were calculated and frequencies, tables, percentages, means, and standard deviations were used to present data. Bivariate analysis was done mainly to check which variables have an association with the dependent variables.
Variables found to have an association with the dependent variables at 0.2 probabilities were entered into multivariate logistic regression for controlling the possible effect of confounders and finally the variables which have significant association was identified based on Odds Ratio (OR), with 95% CI and 0.05 p-values to fit into the final regression model.
Data Quality Assurance
Data collectors and the supervisors were trained on data collection techniques and the data collection tools were pre-tested on non-selected study participants; to check for ambiguity and sequencing of questions, before the actual data collection time. Besides, the completeness, accuracy, and consistency of the collected data were checked daily during the data collection time.
Ethical Approval and Consent
The study was conducted in accordance with the Declaration of Helsinki. A letter for ethical approval and consent from the ethical review board of the Institute of public health, the University of Gondar was taken to North wollo Zonal health department, and zonal Administration. The individuals were told about the aim and the benefit of the study and ensured that there was no harm to them. Then, full consent was obtained from the participants before the commencement of the study. Participants were represented by a unique code to ensure data confidentiality.
Results
Socio-Demographic Characteristics of the Study Population
From the total participants,1689 (97.18%) were tested for HIV serostatus of which 863 (51.1%) were females and the mean age of the respondents was 62.4±12.34 years. The median age of the respondents was 65 with the Interquartile range (IQR) (50–109) years. Of the participants, 60% were married, 63.2% were Muslims, 79.4% were unable to read and write, 91.3% were farmers and 57.7% were rural residents.
Access to HIV/AIDS-Related Services
In this study, the respondents that had access to HIV/AIDS-related services and information in their locality were 79.9% and 67.5%, respectively, and 66.5% of them were asked to pay for HIV test.
The Care Given for or Given by Older People
The majority of the respondents (67.8%) reported that they had the responsibility to give care for their HIV infected and non-infected orphaned grandchildren of which 34.4% had used protective devices and methods during care provisions such as avoiding common use of sharps and needles and use glove. More than half (72.5%) knew the risk of the unprotected provision of care for their HIV infected, grandchildren, adult children, and their spouse as it exposes to HIV infection. Almost all (99%) of the participants stated that there is no care and support program targeted to HIV infected older peoples in the study area.
Behavioral Factors
Of the participants, 41% had practiced alcohol drinking of which 93.93% drunk alcohol on daily basis. From the total drinkers, 55.5% had sexual intercourse while they drink. In the study area, chat chewing was common practice (75.45%) of which 7.45% chewed on daily basis.
Traditions and Cultures
As per the response of the participants, 34.4% were believed that there was a tradition of wife inheritance in the study area. Regarding polygamy; 27.9% responded that tradition of polygamy is still existing and 2.4% of them were engaged in polygamous union type.
High-Risk Sexual Behavior
More than half of the study subjects (62.2%) had two and above sexual partners, in their lifetime, and the mean number of life year sexual partners was 4.4 with Median of 2. Those who had no high-risk sexual partners in the past twelve months accounted for 96.34%. But those with one and two sexual partners in the past twelve months were 1.5% and 1.1%, respectively.
Condom Use
Almost 79% of the respondents did not have access to communication about condom use and 60.1% did not know where the condom is available. Also, around 50.6% did not trust condom as a protective mechanism of HI/AIDS which is evidenced that only 7.3% of the participants were using a condom during sexual activity.
Knowledge of HIV/AIDS
The majority of study subjects (67.5%) did not know about modes of HIV transmission and 71.3% of them did not know currently practiced methods of HIV prevention. From the study group, about 49.1% perceived that older people are at risk of HIV infection. Concerning study subject’s self-perception to risk of HIV infection, 88.86% perceived that themselves were at risk of HIV infection due to unsafe sexual intercourse (34.5%), an experience of unprotected care given for HIV-infected individuals at the household level (30.8%), a common use of sharps and needles (29.7%) and Having HIV-infected partners (1.62%).
HIV Test
Almost half of the participants (49%) reported that when they went to health facilities due to health problems other than HIV, they were not invited for HIV tests by health professionals. More than half (53.3%) were not ever tested for HIV in their lifetime and only (18.9%) were tested for HIV serostatus in the past three months. The major reasons for untested HIV were that they feel they were not exposed to HIV infection (96.2%) and the absence of health workers’ invitation to HIV tests.
Prevalence of HIV and Associated Factors Among Older People Age ≥50 Years
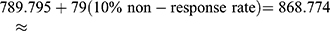
The HIV serostatus assessment revealed that 6.2% of the study subjects were seropositive for rapid HIV test with higher proportion (3.7%) in female [P=0.024, OR= 0.630; 95% CI (0.421–0.944)]. The comparison of HIV negative and HIV positive people for sociodemographic characteristics like age, sex, religion, education status was depicted by (Table 2).
 |
Table 2 Association Between the Prevalence of HIV and Associated Factors Among Older Peoples Age ≥50 Years, in Habru District, North Wollo, Amhara, a Region, 2012 |
Bivariate Findings
As depicted in Table 3, the prevalence of HIV and associated factors on bivariate analysis revealed that sex, religion, marital status, educational status, current types of work, previous types of work, decision-making, condom use during sex, condom use at last sexual intercourse, condom use at high-risk sexual intercourse, communication with a sexual partner to use a condom, trust in condom, knowledge of the place where a condom is available, care given for orphanage by elderly, care and support program targeted for older people, alcohol drinking, knowledge of HIV transmission, knowledge of HIV prevention mechanisms, self-suspicion for HIV infection, reasons for self HIV infection suspicion, lifetime HIV test, and reasons for late HIV test were found to be associated with the occurrence of HIV infection.
 |
Table 3 Bivariate Logistic Regression on the Prevalence of HIV and Associated Factors Among Older People Age ≥50 Years in Habru District, Amhara Region, November 2012 |
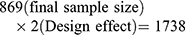
Multivariate Findings
The multivariate regression model, constructed by including the factors revealed that, condom use at last sexual intercourse in the past 12 months, condom use at high-risk sexual intercourse in the past 12 months, marital status, religion, types of previous work, older people self-perception to the risk of HIV infection, care for HIV infected and non-infected grandchildren, presence of care and support program were found to be significantly associated with HIV infection (Table 4).
 |
Table 4 Multivariate Logistic Regression on the Prevalence of HIV and Associated Factors Among Older People Aged ≥50 Years in Habru District, Amhara Region, November 2019 |
Discussions
Community-based cross-sectional assessment of the prevalence of HIV and associated factors among older people is limited in the study area and this study was conducted to assess the prevalence of HIV and associated factors among older people aged ≥50 years. The prevalence of HIV among older people aged ≥50 years in the woreda is found to be 6.2% and various sociodemographic factors, types of work, household decision-making, condom use before sex, condom use at last sexual intercourse in the past twelve months, condom use at high-risk sexual intercourse in the past twelve months, trust in condom, knowledge of HIV transmission methods and prevention mechanism were associated with HIV prevalence.
The prevalence in this study (6.2%) was higher than Addis Ababa and most other regions of Ethiopia12 may be attributed due to an increased survival rate of HIV-infected individuals following the use of highly active antiretroviral therapy.1
According to this study, there was a statistical difference in the magnitude of HIV infection between males and females [OR=0.630; 95% CI (0.421,0.944)] where most cases occur in females which is in agreement with findings from different Sub-Saharan countries.13,14
The magnitude of HIV infection among older people was a decline as the age increases according to this study: 4.3% for the age group 50–65; 1.5 for the age group 66–75 and 0.4% for the age group 76–85 which is consistent with the findings from rural Malawi.15
Concerning prevalence based on religion, Muslim communities (4.7%) were highly affected as wife inheritance and polygamy is practiced commonly. It has been suggested that several of the religiously motivated behaviors practiced by Muslims are favorable for HIV prevention and have led to lower HIV prevalence rates among Muslims. These factors include higher rates of circumcision, fewer self-reported instances of extramarital sexual intercourse.16
In the study area, educationally illiterate participants were highly vulnerable (4.6%) for HIV infection which is in line with a study done in same economical class Sub-Saharan country, Tanzania,14 which may be due to low consciousness about means of HIV transmission and its prevention mechanism.17 Unmarried study subjects, as this study showed; [AOR=0.409; 95% CI, (0.252,0.666)] were less likely to have HIV infection than married study subjects. Significant association [AOR=0.301; 95% CI (0.117,0.770)] was found with previous working types like GO, NGO workers, merchants, and daily laborers. Absence of communication facilities (4.6%) took significant impart for the prevalence and the participants mainly have information about HIV/AIDS from health professionals, community conversation facilitators, friends and others (53.7%) which is against a study done on socio-economic factors and health-related quality of life in older adults living with HIV/AIDS18 where television was the main sources of information. The limited source of information and absence of communication contributes to greater prevalence for rural populations (3.5%) than the urban population (2.7%) though there is no significant association between living in either rural or urban with the prevalence (p=0.832).
Not using a condom before sex in their lifetime [OR= 4.033; 95% CI (2.4936.524)] and not using a condom at last sexual intercourse in the past 12 months [OR=11.099; 95% CI (2.357,52.268)] were the risk factor for elderly HIV infection according to this study which indicates that there was a very low rate of condom use among older adults. Other studies from America revealed that the prevalence of condom use at last intercourse was highest among those aged 50–59 years (24.3%) and declined with age, with a 17.1% prevalence among those aged 60–69 years.19
It is also noticed that lack of appropriate communication/discussion with a sexual partner to use a condom [OR= 3.35; 95% CI (1.426,3.560)], low trust on a condom for the prevention of HIV infection (p=0.011) [OR= 1.689; 95% CI (1.124,2.538)] and lack of knowledge where a condom is available (p=0.000) [OR= 2.068; 95% CI (1.385,3.088)] have a significant association with a higher prevalence of HIV/AIDS among elderly patients according to this study and studies from Nigeria confirmed that use of condom as a protective method is mostly neglected. Even though HIV/AIDS in older patients carry a high mortality, it is many times neglected by even healthcare providers because of the belief that older persons are no longer sexually active.20,21
According to the responses from the participants in this study, 64.1% of them had the responsibility to give care for HIV-infected adult children and 67.8% of them had responsibilities to care HIV infected and non-infected orphaned grandchildren that contributes to increasing the prevalence of HIV/AIDS among them (4.3%). Those who did not have such duties were less likely to have HIV infection [AOR=0.434; 955 CI (0.235,0.800)] which is consistent with the study in Tanzania.14
Absence of care and support program targeted for HIV infected older people was the biggest risk factor for the highest prevalence of HIV infection [OR=6.128; 95% CI (1.532,24.514)], may be resulted from the inadequate awareness of policymakers, health planners, health professionals and older people themselves towards the prevalence of HIV. Multiple challenges faced by older adults that need attention in ensuring continuous engagement in HIV care. Targeted HIV care for older adults would, therefore, significantly improve their access to and experience of HIV care.22
According to this study, alcohol drinking is 2.3 times more a risk factor for HIV infection [OR= 2.302; 95% CI (1.4502,3.6499)] than do not drink as it increases sexual drive and leads unprotective sexual practices. The use of alcohol is believed to alter one’s moods or emotional state either through the sustained release or inhibition of neurotransmitters, thereby enhancing or dampening the response of the individual. It is harmful, leading to, increased risk of contracting HIV, and other sexually transmitted diseases.23 On the other hand, studies revealed that Older people living with HIV (OPLWH) have higher rates of substance use (tobacco, alcohol, and other drugs) than their HIV-negative peers.24
The proportion of older people’s misconception about older people risk to HIV infection was high (51%) and the lowest proportion of elderly invitation for HIV test by health workers (49%) was similar to a study done regarding human immunodeficiency virus (HIV) positive people.25
Having high-risk sexual partner (p=0.008), self-suspicion reasons to have HIV infection such as unsafe sex and common use of sharps and needles [OR=1.685; 95% CI (0.782,3.624)], unprotected care given for HIV victims at home [OR=7.710; 95% CI (4.749,12.518)], absence of lifetime sexual partner (53.3%) [OR= 1.605; 95% CI (1.075,2.398)] and every three months HIV test (81.05%) [OR=2.425; 95% CI (1.587,3.705)] were the major risk factors for elderly HIV infection. Ever use of condoms, poor knowledge on HIV prevention and perception of risk on HIV,26 greater food insecurity,27 being employed and lack of education28 were significantly associated with HIV infection.
Lack of knowledgeable about modes of HIV transmission [OR=1.711; 95% CI (1.146,2.556)] and methods of HIV prevention [OR=1.557; 95% CI (1.034,0.346)] were increasing HIV infection among older people as well as the highest HIV prevalence was found among those who did not suspect themselves for HIV infection [AOR=3.731; 95% CI (2.280,6.104)], which is evidenced by CDC Behavioral Risk Factor Surveillance System.29
Conclusion
The prevalence of HIV among older people in the study area was higher (6.2%). From the multivariate regression model, condom use at last sexual intercourse in the past 12 months, marital status, religion, types of previous work, older people’s self-perception to the risk of HIV infection, care for HIV infected and non-infected grandchildren, presence of care and support program were significantly associated with HIV infection.
Recommendations
Different stakeholders should design well-organized care and support program within the community that targets HIV infected and vulnerable older people in HIV control program and planners, and Health Policymakers at different levels should provide more attention for the component of HIV infection among older people in HIV control activities. Besides, 100% condom promotion and utilization programs should be established targeted for older people vulnerable to HIV infection.
Acknowledgment
The Authors would like to Acknowledge the North Wollo Zonal Health Department, Zonal Administration Office, and Habru Woreda Administration Office for their welcome and contribution for the better accomplishment of the paper.
Disclosure
The authors report no conflicts of interest regarding the publication of this paper.
References
1. Mpondo BCT. HIV infection in the elderly: arising challenges. J Aging Res. 2016;2016:1–10. doi:10.1155/2016/2404857
2. Nguyen N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3(3):454–456.
3. Cumming JNRG. HIV infection in older adults in sub-Saharan Africa. Bull World Health Organ. 2010;4–15.
4. Pratt G, Gascoyne K, Cunningham K, Tunbridge A. Human immunodeficiency virus (HIV) in older people. Age Ageing. 2010;39:289–294.
5. Negin J, Mills EJ, Albone R. Continued neglect of aging of HIV epidemic at UN meeting. Lancet. 2011;37:768.
6. Knodel J, Watkins S, VanLandingham M. AIDS and older persons: an international perspective. J Acquir Immune Defic Syndr. 2003;33(Sup 2):S153–S165. doi:10.1097/00126334-200306012-00012
7. Lazarus JV, Nielsen KK. HIV and people over 50 years old in Europe. HIV Med. 2010;11(7):479–581. doi:10.1111/j.1468-1293.2009.00810.x
8. Cardoso SW, Torres TS, Santini-Oliveira M, Marins LM, Veloso VG, Grinsztejn B. Aging with HIV: a practical review. Braz J Infect Dis. 2013;17(4):464–479. doi:10.1016/j.bjid.2012.11.007
9. Kibret GD, Ferede A, Leshargie CT, Wagnew F, Ketema DB, Alebel A. Trends and spatial distributions of HIV prevalence in Ethiopia. Infect Dis Poverty. 2019;8(1):90. doi:10.1186/s40249-019-0594-9
10. Methodology S. Sampling methods and sample size calculation for the SMART methodology; 2012. Available from: www. smart methodology. org.
11. Negin J, Cumming RG. HIV infection in older adults in sub-Saharan Africa: extrapolating prevalence from existing data. Bull World Health Organ. 2010;88(11):847–853. doi:10.2471/BLT.10.076349
12. Adal M. Systematic review on HIV situation in Addis Ababa, Ethiopia. BMC Public Health. 2019;19(1):1544. doi:10.1186/s12889-019-7885-8
13. Hegdahl HK, Fylkesnes KM, Sandøy IF, Faragher EB. Sex differences in HIV prevalence persist over time: evidence from 18 countries in sub-Saharan Africa. PLoS One. 2016;11(2):e0148502. doi:10.1371/journal.pone.0148502
14. Nyigo V, Kilale A, Kilima S, et al. Magnitude of HIV infection among older people in Mufindi and Babati districts of the Tanzania mainland. HIV/AIDS (Auckland, Nz). 2014;6:75.
15. Freeman E, Anglewicz P. HIV prevalence and sexual behavior at older ages in rural Malawi. Int J STD AIDS. 2012;23(7):490–496. doi:10.1258/ijsa.2011.011340
16. Zou J, Yamanaka Y, John M, Watt M, Ostermann J, Thielman N. Religion and HIV in Tanzania: influence of religious beliefs on HIV stigma, disclosure, and treatment attitudes. BMC Public Health. 2009;9(1):75. doi:10.1186/1471-2458-9-75
17. Anokye R, Acheampong E, Budu-Ainooson A, et al. Knowledge of HIV/AIDS among older adults (50 years and above) in a peri-urban setting: a descriptive cross-sectional study. BMC Geriatr. 2019;19(1):304. doi:10.1186/s12877-019-1335-4
18. Worthington C, Krentz HB. Socio-economic factors and health-related quality of life in adults living with HIV. HIV Social Behav Epidemiol Stud. 2008;1–2.
19. Pilowsky DJ, Wu LT. Sexual risk behaviors and HIV risk among Americans aged 50 years or older: a review. Subst Abuse Rehabil. 2015;6:51. doi:10.2147/SAR.S78808
20. Philip-Ephraim EE, Gyuse AN, Udonwa NE, Peters EJ, Anyanechi CC. Knowledge and perception of HIV prevention through condom use among midlife and older adults in Calabar, Nigeria. West Indian Med J. 2010;59(4):429.
21. Odor K. Elderly condom use and perception: a barrier to family planning and mitigation of HIV/AIDS in high-risk urban slums in Nigeria. BMC Proc. 2011;5(6):1.
22. Kiplagat J, Mwangi A, Chasela C, Huschke S. Challenges with seeking HIV care services: perspectives of older adults infected with HIV in western Kenya. BMC Public Health. 2019;19(1):929. doi:10.1186/s12889-019-7283-2
23. Malaju MT, Asale GA. Association of Khat and alcohol use with HIV infection and age at first sexual initiation among youths visiting HIV testing and counseling centers in Gamo-Gofa Zone, South West Ethiopia. BMC Int Health Hum Rights. 2013;13(1):10. doi:10.1186/1472-698X-13-10
24. Soboka M, Tesfaye M, Feyissa GT, Hanlon C. Alcohol use disorders and associated factors among people living with HIV who are attending services in southwest Ethiopia. BMC Res Notes. 2014;7(1):828. doi:10.1186/1756-0500-7-828
25. Maes CAaL CA, Louis M. Behaviors among older adults. Knowledge of AIDS, perceived risk of AIDS, and at-risk sexual behaviors among older adults. J Am Acad Nurse Pract. 2003;15(11):509. doi:10.1111/j.1745-7599.2003.tb00340.x
26. Swai SJ, Damian DJ, Urassa S, et al. Prevalence and risk factors for HIV among people aged 50 years and older in Rombo district, Northern Tanzania. Tanzan J Health Res. 2017;19(2).
27. Govender K, Beckett SE, George G, et al. Factors associated with HIV in younger and older adult men in South Africa: findings from a cross-sectional survey. BMJ Open. 2019;9(12):e031667. doi:10.1136/bmjopen-2019-031667
28. Ibrahim SA, Sabitu K, Abubakar A, et al. Demographic factors associated with HIV infection between low and high prevalence areas in Nigeria, 2015. Pan Afr Med J. 2019;32(Suppl 1). doi:10.11604/pamj.supp.2019.32.1.13330
29. Ford CL, Godette DC, Mulatu MS, Gaines TL. Recent HIV testing prevalence, determinants, and disparities among US older adult respondents to the behavioral risk factor surveillance system. Sex Transm Dis. 2015;42(8):405. doi:10.1097/OLQ.0000000000000305
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.