Back to Journals » Risk Management and Healthcare Policy » Volume 16
Prevalence and Risk Factors Underlying Occupational Stress and Depression Among Clinical Nurses in Secondary and Tertiary Hospitals of China During COVID-19 Setting
Authors Liu XK, Huang DL , Meng LP, Cheng W , Li YY, Qin LL , Yang A, Zeng F , Zou Q, Li QF
Received 25 April 2023
Accepted for publication 11 July 2023
Published 1 August 2023 Volume 2023:16 Pages 1377—1389
DOI https://doi.org/10.2147/RMHP.S415349
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Xiao-kun Liu,1,* Dan-ling Huang,1,2,* Li-ping Meng,1 Wei Cheng,1 Yi-yi Li,1 Lu-lu Qin,3 Ao Yang,4 Fan Zeng,5 Qin Zou,1 Qi-fu Li6
1Clinical Psychology Department, The First Affiliated Hospital of Hainan Medical University, Haikou City, Hainan Province, People’s Republic of China; 2Neurology Department, Graduate School of Tianjin Medical University, Tianjin City, People’s Republic of China; 3Department of Social Medicine and Health Management, School of Medicine, Hunan Normal University, Changsha City, Hunan Province, People’s Republic of China; 4Health Management Department, School of Management of Hainan Medical University, Haikou City, Hainan Province, People’s Republic of China; 5Graduate School of Hainan Medical University, Haikou City, Hainan Province, People’s Republic of China; 6Neurology Department, The First Affiliated Hospital of Hainan Medical University, Haikou City, Hainan Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiao-kun Liu; Qi-fu Li, Email [email protected]; [email protected]
Aim: This study was designed to develop an effective measurement tool for occupational stress among medical staff and to identify the underlying risk factors among clinical nurses in China under depression during and after COVID-19.
Methods: In the first stage, an occupational stress scale was developed for medical staff based on qualitative and quantitative methods. The dimensions of the scale were based on childhood stress and seven other parameters of working stress. In the second stage, a provincial survey was conducted among clinical nurses in Hainan. The structure of Medical Staff Occupational Stress Scale was tested in secondary and tertiary hospitals. The socio-demographic information, occupational stress (measured using the developed scale), and current depression symptoms (assessed with the nine‐item Patient Health Questionnaire) were evaluated. The risk factors for occupational stress-induced depression were tested using multivariate logistic regression.
Results: The Medical Staff Occupational Stress Scale consisted of 42 items under eight dimensions with strong reliability and validity. Almost 80% of the clinical nurses reported obvious symptoms of depression. Based on multivariate logistical regression analysis, the significant risk factors for depression in nurses at secondary hospitals and tertiary hospitals were childhood stress, teaching stress, relationship with patient stress, and administration stress.
Conclusion: The Medical Staff Occupational Stress Scale utilized in nursing population is based on strong psychometric features. Childhood stress contributes to occupational stress in nurses. The selection of nurses for clinical work may require evaluation of past history for childhood stress to prevent occupational depression. Teaching stress, relationship with patient stress and administration stress play significant roles in the prevention of depression among clinical nurses.
Keywords: occupational stress, depression, teaching stress, relationship with patient stress, nurses
Introduction
Occupational stress among clinical nurses is a major challenge,1 which not only affects nurses’ physical and mental health but also patients’ diagnosis and treatment as well as their overall health. During COVID‑19, the increased levels of occupational stress among clinical nurses2 resulted in the development of depressive disorders. Studies suggested that most major depression is preceded by life stressors.3 Preclinical studies indicate that chronic stress alters the shape and number of neurons in the brain, resulting in mood disorders.4 Notably, the COVID-19 pandemic exacerbated occupational stress among clinical nurses.5,6 The risk factors for occupational stress associated with depression in nurses warrant further investigation.
In November 1989, the Ministry of Health of China implemented a hierarchical system for the accreditation of hospitals. The hospitals were divided into three levels based on function and scale, technical construction, management and service quality.7 The first-level grassroots hospitals directly provide preventive services and medical treatment, health care, and rehabilitation to the community. The second-level hospitals provide comprehensive services to multiple communities and undertake teaching and scientific research tasks. The third-level hospitals, referred to as tertiary hospitals, provide high-level specialized medical and health services and perform advanced teaching and scientific research in multiple regions. Therefore, clinical nurses in secondary and tertiary hospitals of China provide a wide range of services, including teaching tasks and scientific research. Teaching tasks include lectures and demonstration of clinical skills and related tutoring before examination for medical students. The teaching tasks are supervised regularly in each academic semester. Nurses also experience research stress during scientific paper writing and project management. Instruments currently available to evaluate occupational stress among clinical nurses at secondary and tertiary hospitals, such as the Nurse Stressor Scale,8 the Nursing Stress Scale,9 the Occupational Stress Inventory and its revised edition,10,11 and the General Job Stress Questionnaire,12 do not measure all the relevant stressors. Occupational stress among clinical nurses in China working in secondary and tertiary hospitals is a multidimensional construct, suggesting the need for a comprehensive scale.
The association between multidimensional occupational stress and depression among clinical nurses in secondary and tertiary hospitals of China is seldom reported. This study therefore investigated the risk factors for occupational stress underlying depression in nurses during and after the COVID-19 epidemic. This study was conducted in Hainan, the southeastern province of China, where the Hainan Free Trade Port Law was adopted on June 10, 2021. The law laid the legal foundation required to transform the entire island of Hainan into a globally influential free trade port (FTP). The local medical staff in Hainan experience significant stressors under the FTP environment. Therefore, an Occupational Stress Scale was developed for medical staff. A provincial survey of clinical nurses was conducted involving 26 hospitals to identify the risk factors associated with occupational stress contributing to depression. Based on the results, targeted strategies for the prevention or reduction of depression symptoms and stress management were suggested for clinical nurses.
Methods
This study was granted ethical approval by the Institutional Review Board of Hainan Medical University. The study was conducted in accordance with the tenets of the Declaration of Helsinki. The participants were asked to sign written informed consent. The results of the survey will be used solely for scientific reporting and the promotion of nurses’ mental health. Personal information identifying any individual respondent will not be released.
Literature review, in-depth interviews with medical staff, and discussions with experts were used to generate the item pool of the Medical Staff Occupational Stress Scale. Based on qualitative research involving clinical nurses, eight dimensions of occupational stress were identified: childhood stress, working environment stress, contagion stress, teaching stress, research stress, relationship with patients stress, workplace violence stress, and administration stress. Previous scales disregarded the long-term impact of childhood stress on occupational stress in adulthood. Studies have demonstrated that individuals who experienced stress or trauma in childhood are prone to mental disorders in adulthood.13–19 Therefore, the effect of childhood stress on occupational stress response was considered during the assessments.
The survey was conducted by a team led by a principal investigator majoring in clinical nursing. Certified clinical nurses from a specific tertiary hospital were recruited to respond and validate the psychometric efficiency of the scale from August to December 2021. In total, 800 questionnaires were distributed, and 650 individuals responded, with a response rate of 81.25%. The data for assessing occupational stress were randomly divided into two groups for Exploratory Factor Analysis (EFA) and Confirmatory Factor Analysis (CFA). Data were analyzed using SPSS 26.0 and Amos software. The scale construct was further validated by clinical nurses in hospitals designed for teaching and scientific research in Hainan. The first-level hospitals do not perform teaching and research tasks, and were therefore excluded. The study included secondary and tertiary hospitals in Hainan Province. An online cross-sectional survey of certified clinical nurses was conducted from January 1 to June 30, 2022. Nursing assistants and temporary workers undertaking nursing jobs were excluded.
Socio-demographic conditions, occupational stress, and correlates were surveyed in this study. The Chinese version of the Patient Health Questionnaire Depression Module (PHQ-9) was used to identify each participant’s depressive symptoms.20 Each item was measured in terms of the frequency of depressive symptom occurrence on a scale of 0 (“never”) to 3 (“daily”). A higher total score (possible range of 0–27) indicated a greater degree of depressive symptoms. The Chinese PHQ-9 had a Cronbach’s alpha of 0.86.21 SPSS 26.0 statistical software was used to conduct the statistical analyses. Descriptive statistics was used to identify symptoms of depression among the nurses included in the sample. Multivariate logistic regression analyses of risk factors associated with occupational stress underlying depression in clinical nurses were performed, and ORs and 95% CIs were determined. CFA was performed using Mplus 7 software package.
Results
Study 1. Development of the Medical Staff Occupational Stress Scale
A Medical Staff Occupational Stress Scale (MSOSS) was generated (shown in Appendix 1). The Likert 5-point scoring system was used to assess both the frequency and mental stress due to occupational stressors. The frequency of occupational stressors was scored as follows: not occurred = 1, rarely encountered= 2, sometimes encountered = 3, often encountered = 4, and almost every day encountered = 5. A mental score of 1 indicated absence of stress; a score of 2 reflected mild stress; 3, moderate stress; 4, severe stress; and 5, extremely severe stress.
In the first stage, 650 samples were randomly divided into two groups, with 325 participants each. Items with a correlation coefficient with the total scale score less than 0.4 were deleted. As shown in Table 1, explorative factor analysis (EFA) was conducted: 1) Item 3 with factor loading <0.4 was deleted and 2) Items belonging to two or more dimensions were also deleted. EFA of the first dataset indicated that 56 items were divided into eight dimensions, which included items 1, 8, 13, 14, 15, 24, 25, 30, 31, 50, 51, 52, 56, and 57 without loading in any dimension. These 14 items with no loading were deleted, leaving 42 items. Based on the EFA outcomes, eight correlated dimensions were differentiated into workplace violence stress, F4-the largest dimension and includes nine items; F7-relationship with patient stress, including six items; F5-teaching stress, including four items; F6-research stress, including four items; F1-childhood stress, including five items; F3-contagion stress including six items; F2-working environment stress including five items; and F8-administration stress including three items. CFA of the other group was then performed using Mplus 7. The results (shown in Figure 1 and Table 2) suggested a χ2/df value of 1.637 <3. The RMSEA value was 0.044 <0.05. The CFI value was 0.930. As shown in Table 3, the Cronbach’s coefficient alpha of the scale was 0.968, and the test–retest reliability at a 2-week interval was 0.653.
 |
Table 1 EFA of Item Pool |
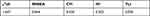 |
Table 2 CFA of MSOSS |
 |
Table 3 Reliability of MSOSS |
 |
Figure 1 CFA for scale development. |
In the second stage, CFA was firstly evaluated in a province-wide sample of clinical nurses working in secondary hospitals. The results (Table 4 and Figure 2) showed a χ2/df value of 2.804 <3, with CFI, IFI, and TLI values of approximately 0.90, indicating that the model fit was good. Then, CFA was evaluated in a province-wide sample of clinical nurses in tertiary hospitals. The results (Table 5 and Figure 3) showed that the χ2/df value was 2.904 <3. The CFI, IFI, and TLI values were approximately 0.90, indicating a good model fit.
 |
Table 4 CFA of MSOSS in Nurses Working in Secondary Hospitals in the Province |
 |
Table 5 CFA of MSOSS in Nurses Working in Tertiary Hospitals in the Province |
 |
Figure 2 CFA of nurses from secondary hospital. |
 |
Figure 3 CFA of nurses from tertiary hospital. |
Study 2. Prevalence and Risk Factors Associated with Depression in Clinical Nurses
The sociodemographic characteristics of the participants were detailed in Table 6. Of the 2988 participants, 1638 nurses from secondary hospitals and 1350 nurses were from tertiary hospitals. As shown in Table 6, 77.80% of the nurses in secondary hospitals and 77.60% of the nurses in tertiary hospitals reported moderate-to-severe depression symptoms on the PHQ-9 scale.
 |
Table 6 Participants’ Sociodemographics |
Distribution of occupational stress among nurses from different hospitals was shown in Table 7. Statistically significant differences in the four dimensions of stress were detected in secondary and tertiary hospitals. The clinical nurses in the secondary hospitals scored significantly higher under childhood stress, working environment stress, contagion stress, workplace violence stress, and overall stress compared with those working in tertiary hospitals. .
 |
Table 7 Occupational Stress Status Among Participants |
The risk factors associated with depression were analyzed via logistic regression. The significance threshold of group differences was set at p < 0.05. PHQ ≥10 was marked as 1 or otherwise as 0 according to previous studies.22,23 Gender, age, childhood stress and other seven sub-stressors were included. As shown in Table 8, the multivariate logistical regression analysis differentiated the significant risk factors for depression in secondary hospitals as childhood stress (OR 1.030; 95% CI 1.000 to 1.060), teaching stress (OR 1.025; 95% CI 1.013 to 1.037), relationship with patient stress (OR 1.033; 95% CI 1.023 to 1.043), and administration stress (OR 1.038; 95% CI 1.011 to 1.066). The multivariate logistical regression analysis (Table 9) showed that significant risk factors for depression among nurses in tertiary hospitals were childhood stress (OR 1.052; 95% CI 1.015 to 1.091), teaching stress (OR 1.021; 95% CI 1.010 to 1.033), relationship with patient stress (OR 1.021; 95% CI 1.011 to 1.032), and administration stress (OR 1.061; 95% CI 1.030 to 1.092).
 |
Table 8 Risk Factors for Stress-Induced Depression Among Clinical Nurses in Secondary Hospitals |
 |
Table 9 Risk Factors for Stress-Induced Depression Among Nurses in Tertiary Hospitals |
Discussion
Occupational stress among medical staff is an important and serious problem, especially in the COVID-19 setting, and is associated with physical burnout and mental disorders.24 Previous scales failed to consider the long-term impact of childhood stress on occupational stress in adulthood. Numerous studies have pointed out that individuals who experienced childhood stress were associated with mental disorders in adulthood.13–19 Therefore, the role of childhood stress in occupational stress response should be considered in any occupational stress assessment or prevention. This study provides a new tool (see Appendix 1) for occupational stress measurement in medical staff. The scale represents the most up-to-date and broad-range assessment tool for assessing occupational stress among clinical nursing staff under eight dimensions: childhood stress; working environment stress; contagion stress; workplace violence stress; teaching stress; research stress; relationship with patient stress; and administration stress (Figures 1–3 and Appendix 1).
The item generation of the MSOSS was based on both qualitative and quantitative methods. Literature review and in-depth interviews were scientifically robust and effectively avoided subjective bias. Quantitative surveys and psychometric indices were used to validate the MSOSS. Reliability indices ranging from 0.80 to 0.90 are considered sufficient, and measures above 0.90 are considered good.25 The Cronbach’s coefficient of the total scale developed in this study was 0.968, with each dimension scoring >0.8. This supports the reliability of the measure. CFA showed that the structural validity of the scale was good, and most items represented latent variables with loadings above 0.5. The results indicated that the measure was psychometrically sound. The factor models identified in the large-scale sample set included clinical nurses working in secondary and tertiary hospitals, based on CFA. The results demonstrated that the scale consists of 42 items, with eight stable dimensions. CFA for cohorts in two different level hospitals showed that MSOSS had stable dimensions for clinical nurses.
Depression is one of the most prevalent psychiatric disorders attributed to biochemical and psychosocial factors.26 Many previous studies supported the stress-depression linkage.3,27 Consistent with previous studies, the current study found that exposure to childhood stress, teaching stress, relationship with patient stress, and administration stress were risk factors for depression in clinical nurses working in secondary and tertiary hospitals of China. Chang et al reported that the mechanisms underlying stress and depression were related to upregulation of transferrin (TF) in the liver and the peripheral blood, and in multiple brain regions in an experimental mouse model of stress-induced depression.28 Ancelin et al suggested that variability in the serotonin transporter (5-HTTLPR) gene affected the risk of depression associated with adverse stress.29 Other mechanisms associated with the pathology of stress and depression have also been reported, including low levels of neurotrophic factors, especially brain-derived neurotrophic factor,30 chronic inflammation,31 and dysregulation of the hypothalamic-pituitary-adrenal axis.29,32 Amounts of studies supported the association between stress and depression.
The global prevalence of major depression has increased during the COVID-19 pandemic.33 Nearly 80% of the nurses in this study reported significant depression symptoms, warranting serious intervention. This study found that childhood stress affected adult stress experience in the workplace, which is consistent with previous studies.17,34,35 Findings of the study add to prior knowledge and understanding about potential long-term effects of childhood stress on current stress and adult depression. Childhood stress exacerbated occupational stress experienced by adults. According to the theory of attachment, the earliest relationships may form the template for the internal model affecting subsequent expectations and explain the emotional interaction with other people36 and thereby influence their social experiences. Therefore, the selection of clinical nurses may require the assessment of childhood stress to prevent occupational depression.
The study suggested that teaching stress was a significant risk factor for depression in clinical nurses in both secondary and tertiary hospitals. Currently, scientific research is acknowledged and rewarded in Chinese hospitals, while teaching tasks are mandatory and no reward. In addition, the national impact due to COVID-19 pandemic had a significant impact on clinical education. The COVID-19 pandemic prompted the closure of all educational institutions at all levels.37 The Chinese Ministry of Education promoted online teaching from 2020 to 2022 for prevention and control of COVID-19.38 In response to government’s request for online teaching, teachers at medical universities utilized Internet, which increased the stress response of clinical nurses. It is essential to reduce the teaching stress to prevent and alleviate depression among clinical nurses. Given the high prevalence of depression, it is imperative to ensure health care by managing stress among clinical nurses. Healthcare support is essential to alleviate teaching stress-induced depression. Regular screening for teaching stress and psychological support for teaching work and intervention to reduce teaching stress are needed. Interventions may include mindfulness-based stress reduction39,40 and exercises conducted in the forest.41
A stressful relationship with patients can decrease the job satisfaction of nurses, leading to burnout,42,43 and deterioration in nursing quality.44 Psychological interventions, such as mindfulness-based stress recovery management,45,46 and Balint group intervention can reduce the stress involving patients. An administrative environment in which occupational stress can be prevented is essential to ensure that nurses are efficient at work and maintain professional well-being. Administration stress can be managed by promoting an open atmosphere in the communication of work issues. Other measures such as respect, understanding, support, and care for the opinions of clinical nurses can alleviate administrative stress.
Limitations
The study outcomes reflect a single geographical area, Hainan Province in China. Therefore, caution is needed to generalize the findings for nurses in other regions. Prospective longitudinal studies based on clinical diagnoses are needed to determine the causal relationship between occupational stress and depression.
Conclusion
The selection of clinical nurses may require assessment of their childhood stress experience in an effort to prevent occupational depression. Teaching stress among clinical nurses must be evaluated to prevent depression, particularly in the post-COVID-19 environment. Stressful relationship with patients and administration stress in clinical nurses should be evaluated to prevent or reduce occupational depression.
Funding
(1) Hainan healthcare project: 20A200377, (2) Youth scientist cultivation project of the First Affiliated Hospital of Hainan Medical University: HYYFYPY201902, (3) Humanistic Medicine Research Center of Hainan province: QRYZH201805(YB), (4) Students’ innovation project: X202011810121, (5) Research Project of Education and Teaching Reform in Hainan Province: Hnjg2020-62, (6) Key Program of Educational and Scientific Research Reform in Hainan Medical University: HYZ201913 and (7) Hainan Clinical Medicine Center.
Disclosure
Xiao-kun Liu and Dan-ling Huang are the coordinated first authors. The authors report no conflicts of interest in this work.
References
1. Dharra S, Kumar R. Promoting mental health of nurses during the coronavirus pandemic: will the rapid deployment of nurses’ training programs during COVID-19 improve self-efficacy and reduce anxiety? Cureus. 2021;13(5):e15213. doi:10.7759/cureus.15213
2. Sriharan A, Ratnapalan S, Tricco AC, et al. Occupational stress, burnout, and depression in women in healthcare during COVID-19 pandemic: rapid scoping review. Front Glob Womens Health. 2020;1. doi:10.3389/fgwh.2020.596690
3. Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1(1):293–319. doi:10.1146/annurev.clinpsy.1.102803.143938
4. Duman RS. Neuronal damage and protection in the pathophysiology and treatment of psychiatric illness: stress and depression. Dialogues Clin Neurosci. 2022;11(3):239–255. doi:10.31887/DCNS.2009.11.3/rsduman
5. Zhang X, Zhao K, Zhang G, et al. Occupational stress and mental health: a comparison between frontline medical staff and non-frontline medical staff during the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11. doi:10.3389/fpsyt.2020.555703
6. Li X, Jiang T, Sun J, Shi L, Liu J. The relationship between occupational stress, job burnout and quality of life among surgical nurses in Xinjiang, China. BMC Nurs. 2021;20(1). doi:10.1186/s12912-021-00703-2
7. Ya-min L, You-qin H, Yan L, Jin-wu G, Chun-ling S. History, problems and measures on hospital accreditation in China. Soft Sci Health. 2008;22(3):215–217.
8. Zhang J-P. The Development of Nurse Stressor Scale. China: Central South University; 2005.
9. French E, Lenton R, Walters V, et al. An empirical evaluation of an expanded nursing stress scale. J Nurs Meas. 2000;8(2):161–178. doi:10.1891/1061-3749.8.2.161
10. Cooper CL. The Occupational Stress Indicator. Nfernelson Publishing Company Limited; 1988.
11. Osipow SH. Occupational Stress Inventory.
12. Hurrell JJ, McLaney MA. Exposure to job stress-a new psy chometric instrument. Scand J Work Environ Health. 1988;14:27–28.
13. Infurna MR, Reichl C, Parzer P, Schimmenti A, Bifulco A, Kaess M. Associations between depression and specific childhood experiences of abuse and neglect: a meta-analysis. J Affect Disord. 2016;190:47–55. doi:10.1016/j.jad.2015.09.006
14. Li X, Guo W, Tang W, et al. The interactions between childhood adversities and recent stress were associated with early‐adulthood depression among Chinese undergraduate students. Depress Anxiety. 2021;38(9):961–971. doi:10.1002/da.23201
15. Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry. 2007;64:49–56. doi:10.1001/archpsyc.64.1.49
16. Gibb BE, Alloy LB, Whitehouse W, et al. History of childhood maltreatment, negative cognitive styles, and episodes of depression in adulthood. Cognit Ther Res. 2001;25(4):425–446. doi:10.1023/A:1005586519986
17. Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry. 2018;210(2):96–104. doi:10.1192/bjp.bp.115.180752
18. McKay MT, Cannon M, Chambers D, et al. Childhood trauma and adult mental disorder: a systematic review and meta‐analysis of longitudinal cohort studies. Acta Psychiatr Scand. 2021;143(3):189–205. doi:10.1111/acps.13268
19. Walker AE, Fenstermacher E, Ross DA. Telomeres, trauma, and training. Biol Psychiatry. 2019;86(9):e29–e30. doi:10.1016/j.biopsych.2019.08.019
20. Zimmerman M, Walsh E, Friedman M, Boerescu DA, Attiullah N. Are self-report scales as effective as clinician rating scales in measuring treatment response in routine clinical practice? J Affect Disord. 2018;225:449–452. doi:10.1016/j.jad.2017.08.024
21. Wang W, Bian Q, Zhao Y, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36(5):539–544. doi:10.1016/j.genhosppsych.2014.05.021
22. Manea L, Gilbody S, McMillan D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen Hosp Psychiatry. 2015;37(1):67–75. doi:10.1016/j.genhosppsych.2014.09.009
23. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. 2012;184(3):E191–E196. doi:10.1503/cmaj.110829
24. Das A, Kumar R, Singh V, Gupta P, Bahurupi Y. Rapid survey of psychological status of health-care workers during the early outbreak of COVID-19 pandemic: a single-centre study at a tertiary care hospital in Northern India. J Med Evid. 2021;2(3):213. doi:10.4103/JME.JME_8_21
25. Evers A, Sijtsma K, Lucassen W, Meijer RR. The Dutch review process for evaluating the quality of psychological tests: history, procedure, and results. Int J Test. 2010;10:295–317. doi:10.1080/15305058.2010.518325
26. Tanaka M, Vecsei L. Editorial of special issue crosstalk between depression, anxiety, and dementia: comorbidity in behavioral neurology and neuropsychiatry. Biomedicines. 2021;9:517. doi:10.3390/biomedicines9050517
27. Monroe SM, Depue RA. Life stress and depression. In: Becker J, Kleinman A, editors. Psychosocial Aspects of Depression. Routledge; 1991:101–130.
28. Chang X, Ma M, Chen L, Song Z, Zhao Z, Wu H. Identification and characterization of elevated expression of transferrin and its receptor TfR1 in mouse models of depression. Brain Sci. 2022;12(10):1267. doi:10.3390/brainsci12101267
29. Ancelin M-L, Scali J, Norton J, et al. Heterogeneity in HPA axis dysregulation and serotonergic vulnerability to depression. Psychoneuroendocrinology. 2017;77:90–94. doi:10.1016/j.psyneuen.2016.11.016
30. Castren E, Monteggia LM. Brain-derived neurotrophic factor signaling in depression and antidepressant action. Biol Psychiatry. 2021;90:128–136. doi:10.1016/j.biopsych.2021.05.008
31. Faugere M, Micoulaud-Franchi JA, Faget-Agius C, Lancon C, Cermolacce M, Richieri R. Quality of life is associated with chronic inflammation in depression: a cross-sectional study. J Affect Disord. 2018;227:494–497. doi:10.1016/j.jad.2017.11.061
32. Tanaka M, Szabo A, Spekker E, Polyak H, Toth F, Vecsei L. Mitochondrial impairment: a common motif in neuropsychiatric presentation? The link to the tryptophan-kynurenine metabolic system. Cells. 2022;11:2607. doi:10.3390/cells11162607
33. Santomauro DF, Mantilla Herrera AM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi:10.1016/S0140-6736(21)02143-7
34. Scott KM, McLaughlin KA, Smith DA. Childhood maltreatment and DSM-IVadult mental disorders: comparison of prospective and retrospective findings. Br J Psychiatry. 2012;200(6):469–475. doi:10.1192/bjp.bp.111.103267
35. Kessler RC, McLaughlin KA, Green JG. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197(5):378–385. doi:10.1192/bjp.bp.110.080499
36. Bm W. Relational schemas and the processing of social information. Psychol Bull. 1992;112:461–484. doi:10.1037/0033-2909.112.3.461
37. The World Bank. The COVID-19 pandemic: shocks to education and policy responses. 2022. https://wwwworldbankorg/en/topic/education/publication/the-covid19-pandemic-shocks-to-education-and-policy-responses.
38. China MoEoPsRo. The Ministry of Education issued a guideline to organize and manage online teaching in colleges and universities during the epidemic prevention and control period. 2020. http://www.moe.gov.cn/jyb_xwfb/gzdt_gzdt/s5987/202002/t20200205_418131.html.
39. Errazuriz A, Schmidt K, Undurraga EA. Effects of mindfulness-based stress reduction on psychological distress in health workers: a three-arm parallel randomized controlled trial. J Psychiatry Res. 2022;145:284–293. doi:10.1016/j.jpsychires.2020.11.011
40. Tement S, Ketiš ZK, Miroševič Š, et al. The impact of Psychological Interventions with Elements of Mindfulness (PIM) on empathy, well-being, and reduction of burnout in physicians: a systematic review. Int J Environ Res Public Health. 2021;25(18(21):11181.
41. Stier-Jarmer M, Throner V, Kirschneck M, Immich G, Frisch D, Schuh A. The psychological and physical effects of forests on human health: a systematic review of systematic reviews and meta-analyses. Int J Environ Res Public Health. 2021;18(4):1770. doi:10.3390/ijerph18041770
42. Kafle S, Paudel S, Thapaliya A, Acharya R. Workplace violence against nurses: a narrative review. J Clin Transl Res. 2022;13(5):421–424.
43. Duan X, Ni X, Shi L, et al. The impact of workplace violence on job satisfaction, job burnout, and turnover intention: the mediating role of social support. Health Qual Life Outcomes. 2019;30(1):93.
44. Jun J, Ojemeni MM, Kalamani R, et al. Relationship between nurse burnout, patient and organizational outcomes: systematic review. Int J Nurs Stud. 2021;2021:119.
45. Schellinger TM. Mindfulness-based stress reduction for nurses: an integrative review. J Holist Nurs. 2022;2022:1–20.
46. Khoury B, Sharma M, Rush SE, Fournier C. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosom Res. 2015;78(6):519–528. doi:10.1016/j.jpsychores.2015.03.009
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
