Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Prevalence and Risk Factors of Anxiety Among Adult Patients with Chronic Pharyngitis in Wuhu, China
Authors Zha Z, Gao S, Liu S, Hu G
Received 19 April 2023
Accepted for publication 23 May 2023
Published 31 May 2023 Volume 2023:19 Pages 1313—1319
DOI https://doi.org/10.2147/NDT.S415938
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Zhihong Zha,1,* Shuang Gao,2,* Shaofeng Liu,3 Guoqin Hu1
1Department of Otolaryngology Head and Neck Surgery, The Second People’s Hospital of Hefei, Hefei Hospital Affiliated to Anhui Medical University, Hefei, Anhui, People’s Republic of China; 2Anhui Public Health Clinical Center, The First Affiliated Hospital of Anhui Medical University North District, Hefei, Anhui, People’s Republic of China; 3Department of Otolaryngology Head and Neck Surgery, Yijishan Hospital of Wannan Medical College, Wuhu, Anhui, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Guoqin Hu, Department of Otolaryngology Head and Neck Surgery, The Second People’s Hospital of Hefei, Hefei Hospital Affiliated to Anhui Medical University, Hefei, Anhui, People’s Republic of China, Email [email protected]
Objective: Chronic pharyngitis (CP) is a common disease, which has a long duration and a wide range of onset. Anxiety is considered to be a common complication in patients with CP. The purpose of this study was to evaluate the anxiety level and potentially influencing factors in patients with CP, to provide insights for the management of anxiety in patients with CP.
Methods: A total of 104 adult patients with CP meeting the inclusion/exclusion criteria were enrolled from a single center in Wuhu, China between October 2015 and December 2016. A Self-rating Anxiety Scale (SAS) was used to measure the status of anxiety. The relationship between SAS scores and illness period in patients with CP was analyzed by Pearson correlation test. Univariate analysis and binary logistic regression analysis were performed to analyze the risk factors of anxiety in patients with CP.
Results: The average SAS score of 104 patients with CP was (44.17 ± 8.38), including 82 cases (78.85%) without anxiety and 22 cases (21.15%) with anxiety. Moreover, the illness period was found to be positively related to SAS scores in patients with CP (r = 0.378, P = 0.001). Furthermore, the results of univariate analysis showed that there were significant differences in anxiety state among CP patients with different age, illness period, source of treatment payment, and marital status (P < 0.05). Additionally, the results of binary logistic regression analysis showed that age, source of treatment payment, and marital status were the independent risk factors affecting the anxiety status of patients with CP (P < 0.05).
Conclusion: These results suggested that CP patients with advanced age, self-pay, and unmarried status had higher risk for anxiety.
Keywords: chronic pharyngitis, risk factor, self-rating anxiety scale, anxiety, prevalence
Introduction
Chronic pharyngitis (CP) is a frequent pharyngeal mucosa inflammation that causes serious issues in everyday living, ranging from morning throat soreness to voice changes.1,2 The etiology of CP is complex. The most important cause is bacterial infection, which is followed by non-infectious causes such as occupational exposure, obstructive sleep apnea and hypopnea syndrome.3 It has been reported that the number of outpatient visits for CP in the United States ranges from 7,000,000 to 11,000,000.4,5 In China, it has been suggested that the prevalence of CP may be high due to the severe air pollution.6 Because of the large population and enormous burden, CP is increasingly recognized as a global public health issue.
Anxiety, a psychological and physiological condition characterized by strong feelings of worry, unease, or fear that interfere with work and daily life, is the most common mental health problem worldwide.7 Due to the long course of CP, difficulty in self healing, complex etiology, multiple complications, and high treatment costs, as well as family and social factors, physical and psychological disorders including anxiety, are common among patients with CP, seriously affecting their quality of life. Besides, anxiety can impede the confidence of CP patients to self-manage, leading to non-adherence with treatment.8 Therefore, it is of great clinical significance to evaluate the anxiety level and potentially influencing factors in patients with CP, with the aim to provide insights for the management of anxiety of CP patients.
Currently, the prevalence and risk factors of anxiety in adult patients with CP in China remain unclear. In the present study, in order to evaluate the anxiety level and potentially influencing factors in adult patients with CP in China, we performed a study to determine the anxiety status in adult patients with CP from a single center in Wuhu, China, and analyze the related impact factors, providing helpful information for medical staff to identify high-risk CP patients for anxiety before commencement of clinical evaluation.
Materials and Methods
Study Design and Participants
A total of 104 adult patients with CP meeting the inclusion/exclusion criteria were enrolled from Yijishan Hospital of Wannan Medical College in Wuhu, China between October 2015 and December 2016. Patients diagnosed with CP based on the diagnostic criteria of chronic simple pharyngitis (CSP) and chronic hypertrophic pharyngitis (CHP) in the Practice of Otolaryngology-Head and Neck Surgery (2nd edition) by an experienced researcher were enrolled in the present study. Common criteria for patient inclusion were as follows: (1) being between the ages of 18–65; (2) meeting diagnostic criteria of CP; (3) No obvious bacterial formation is found in the general bacterial culture in the laboratory. Common criteria for patient exclusion were as follows: (1) Major psychiatric disorders or neurodegenerative illness history; (2) Allergic diseases: allergic rhinitis and allergic pharyngitis; (3) Patients unable or unwilling to cooperate with the study. This procedure was approved by the ethics committee of Yijishan Hospital of Wannan Medical College and was conducted according to the principles of the Declaration of Helsinki. Informed consent was obtained from all the participants.
Measurement of Anxiety Status
The SAS scale was compiled by Zung, which is widely used in clinical and medical research as a norm-referenced scale to assess anxiety symptoms for the past few decades.9 There are 20 items in total, with 1–4 points for each item and 15 forward scores and 5 reverse scores, respectively. The rough score is the sum of the scores of the 20 items.10 SAS scores ranging from 50 to 59 were diagnosed as mild anxiety, those from 60 to 69 as moderate anxiety, and ≥ 70 as severe anxiety according to the Chinese norm. SAS scale has been translated into Chinese versions, with a high reliability coefficient for different populations in China. The Cronbach α coefficient of the scale is 0.82.11,12
Data Collection
Face-to-face interviews of participants were conducted using a structured questionnaire with detailed information on demographic and sociological information of the patient, including the patient’s age, gender, illness period, level of education, work status, monthly income, source of treatment payment, marital status, residence, history of smoking, and history of drinking.
Statistical Analysis
Sample size was determined based on the expression  ,13 where N is the minimum sample size, z is the standard normal deviation, usually set at 1.96 which corresponds to the 95% confidence interval, p is the proportion (7.5%) in the target population estimated to have anxiety according to a pre-investigation, and b is the degree of accuracy desired, usually set at 5%. Consequently, a sample size of 100 was calculated.
,13 where N is the minimum sample size, z is the standard normal deviation, usually set at 1.96 which corresponds to the 95% confidence interval, p is the proportion (7.5%) in the target population estimated to have anxiety according to a pre-investigation, and b is the degree of accuracy desired, usually set at 5%. Consequently, a sample size of 100 was calculated.
Statistical analysis was calculated using SPSS (version 17.0; IBM Corp., Armonk, NY, USA). The statistical significance was set at P < 0.05. The normality of the distribution of continuous variables was analyzed using the one-sample Kolmogorov–Smirnov test. The continuous values were presented as mean and standard deviation (SD), and t tests or ANOVA tests were performed for data comparison. Chi-square tests were used for categorical data. Pearson’s correlation test was used for correlation analyses. Binary logistic regression analysis was conducted to identify the potential risk factors for anxiety in patients with CP.
Results
Assessment Results of SAS in 104 Patients with CP
The average SAS score of 104 patients with CP was (44.17 ± 8.38), including 82 cases (78.85%) without anxiety and 22 cases (21.15%) with anxiety.
Univariate Analysis of the Influencing Factors of Anxiety in Patients with CP
Univariate analysis of the differences in anxiety across variables are shown in Table 1. There were significant differences in anxiety state among CP patients with different ages, illness period, source of treatment payment, and marital status (P < 0.05). However, there was no statistical significance in anxiety of patients with CP with different gender, level of education, work status, monthly income, residence, history of smoking or history of drinking (P > 0.05).
 |
Table 1 Univariate Analysis of Anxiety in Patients with CP |
Correlation Between SAS Scores and Illness Period in Patients with CP
The relationship between SAS scores and illness period in patients with CP was analyzed by Pearson correlation test. The illness period was found to be positively related to SAS scores in patients with CP (r = 0.378, P = 0.001; Figure 1).
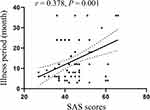 |
Figure 1 Correlation between SAS scores and illness period in patients with CP. |
Binary Logistic Regression Analysis of the Influencing Factors of Anxiety in Patients with CP
Binary logistic regression analysis was used to analyze the influencing factors of anxiety state in patients with CP. The anxiety status of patients was taken as dependent variable, and the factors with significant differences in Table 1 were included as independent variables in the logistic regression model. The assignment of dependent variables and independent variables is given in Table 2.
 |
Table 2 Variable Assignment Table of Binary Logistic Regression Analysis of Anxiety in Patients with CP |
The results of binary logistic regression analysis showed that age, source of treatment payment, and marital status were the independent risk factors affecting the anxiety status of patients with CP (P < 0.05; Table 3). Specifically, CP patients with advanced age, self-pay, and unmarried status had higher risk for anxiety.
 |
Table 3 Binary Logistic Regression Analysis of Anxiety in Patients with CP |
Discussion
To the best of our knowledge, this is the first study to evaluate the anxiety level and potentially influencing factors in patients with CP, with the aim to provide insights for the management of anxiety in CP patients. Three main findings emerged in the present study. Firstly, the average SAS score of 104 patients with CP was (44.17 ± 8.38), including 22 cases (21.15%) with anxiety. Secondly, the illness period was found to be positively related to SAS scores in patients with CP. Thirdly, age, source of treatment payment, and marital status were the independent risk factors affecting the anxiety status of patients with CP.
SAS, a self-report questionnaire that includes 40 items on a 4-point rating scale, can accurately reflect and differentiate the subjective feelings of anxious psychopaths and healthy people.14 SAS was used to assess the patients’ anxious status in numerous studies.15–17 The Chinese version of SAS has good reliability and validity.18 Thus, SAS was selected to measure the status of anxiety in patients with CP in the present study.
Psychiatric disorders are prevalent in pharyngitis patients. In the present study, the incidence of anxiety in patients with CP was 21.15% (22/104). To the best of knowledge, this is the first report on the incidence of anxiety in patients with CP in China. According to the latest nationwide survey of mental disorders in China, the lifetime prevalence of anxiety disorders is 7.6%.19 Our results suggested that the incidence rate of anxiety is significantly higher in patients with CP than in the general population. This phenomenon may be attributed to two reasons: (1) CP has the characteristics of long illness duration, easy recurrence, long treatment time, and high treatment cost, which may easily increase the anxiety level of patients; (2) patients with CP are concerned about the possibility of consequences such as aphasia and malignant tumors. Moreover, the illness period was found to be positively related to the level of anxiety in patients with CP in the present study. Thus, it is suggested that patients with repeated symptoms of CP should also receive psychiatric assessment and support.20
Our results showed that CP patients with advanced age had higher risk for anxiety. Common anxiety disorder is the most common among mental disorders in patients of advanced age group.21 It has been reported that anxiety symptoms can always increase with age.22 Recently, advanced age was found to be associated with high-level of anxiety in 2625 adults in the community and 1363 patients at health center.23 Being in the age of 45 and older has a two-fold increased chance of having severe anxiety symptoms compared to being in age 18 to 24.23 Mechanistically, a rate model study has revealed that in response to behavioral changes, certain regions of the fear/anxiety circuit (amygdala, hippocampus, and hypothalamus) in the brain experience age-related modifications.24 Thus, clinicians should pay attention to the anxiety state of CP patients, especially those with advanced age.
Previous studies suggested that common mental illnesses, including significant levels of anxiety symptoms, can be prevented by having a high degree of social and economic status.25 Anxiety at a high level is negatively influenced by lower wealth status.23 In a prospective study, low household income was found to increase the risk of high-level anxiety symptoms and other common mental disorders, while living in a good economic class significantly reduces the risk of high-level anxiety symptoms.26 In the present study, self-pay patients had higher risk for anxiety compared to those with healthcare payment. However, there was no statistical significance in anxiety of patients with CP with different monthly income. It has been reported that monthly income was shown to have significant impacts on anxiety symptoms among stroke patients,27 patients with liver transplantation,28 and dialysis patients.29 It is unclear why monthly income of patients with CP had no impact on anxiety symptoms in the present study. Since this study is a single-center study and the sample size is relatively small, the differences in anxiety symptoms among CP patients with different monthly incomes should be confirmed by multicentric studies.
Social relationships or integration are crucial for improving lifelong mental health.30 As a social being, human requires belonging as a fundamental requirement for good social relationships. In contrast, loneliness increases the risk of anxiety symptoms, leading to serious mental health problems.31,32 Living alone was found to be a greater risk factor for high levels of anxiety than living with a family, and participants’ living conditions have been linked to high levels of anxiety.23 Consistently, the results of the present study showed that CP patients with unmarried status exhibited higher level of anxiety.
There are some limitations to this study. Firstly, the small sample size and single-center design of the current study may indicate sampling bias. Secondly, the ability to examine the relationships between cause and effect for all factors was limited due to the cross-sectional study design. Longitudinal studies are needed. Thirdly, the information on these comorbidities including Globus Hystericus, Laryngopharyngeal Reflux, and Gastroesophageal Reflux was not collected. Patients with CP should be classified according to these complications and the differences in anxiety symptoms among these groups should be compared to observe the effect of these complications on anxiety symptoms of CP patients.
In conclusion, the incidence of anxiety in patients with CP is high. Clinicians should pay extra attention to the anxiety state of CP patients, especially those with advanced age, self-pay, and unmarried status. Further research is warranted to confirm the potential benefit of psychological intervention for anxiety disorders in individuals with CP.
Disclosure
Authors have no conflict of interest to declare.
References
1. Shen Y, Liu C, Luo J, Wang J, Zhang D. 16SrDNA-based detection technology in patients with chronic pharyngitis to analyze the distribution characteristics of pharyngeal bacteria. J Healthc Eng. 2022;2022:5186991. doi:10.1155/2022/5186991
2. Li Z, Huang J, Hu Z. Screening and diagnosis of chronic pharyngitis based on deep learning. Int J Environ Res Public Health. 2019;16:1688.
3. Badran H, Salah M, Fawzy M, Sayed A, Ghaith D. Detection of bacterial biofilms in chronic pharyngitis resistant to medical treatment. Ann Otol Rhinol Laryngol. 2015;124(7):567–571. doi:10.1177/0003489415570934
4. Soderholm AT, Barnett TC, Sweet MJ, Walker MJ. Group A streptococcal pharyngitis: immune responses involved in bacterial clearance and GAS-associated immunopathologies. J Leukoc Biol. 2018;103(2):193–213. doi:10.1189/jlb.4MR0617-227RR
5. Kalra MG, Higgins KE, Perez ED. Common questions about streptococcal pharyngitis. Am Fam Physician. 2016;94:24–31.
6. Kang Q, Chen G, Lu J, Yu H, Federici S. Health disparities by type of disability: health examination results of adults (18–64 years) with disabilities in Shanghai, China. PLoS One. 2016;11(5):e0155700. doi:10.1371/journal.pone.0155700
7. Chellappa SL, Aeschbach D. Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev. 2022;61:101583. doi:10.1016/j.smrv.2021.101583
8. Pumar MI, Gray CR, Walsh JR, Yang IA, Rolls TA, Ward DL. Anxiety and depression-Important psychological comorbidities of COPD. J Thorac Dis. 2014;6:1615–1631. doi:10.3978/j.issn.2072-1439.2014.09.28
9. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–379. doi:10.1016/S0033-3182(71)71479-0
10. Dunstan DA, Scott N. Norms for zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20:90. doi:10.1186/s12888-019-2427-6
11. Wang C, Zhao H. The impact of COVID-19 on anxiety in Chinese university students. Front Psychol. 2020;11:1168. doi:10.3389/fpsyg.2020.01168
12. Song S, Yang X, Yang H, et al. Psychological resilience as a protective factor for depression and anxiety among the public during the outbreak of COVID-19. Front Psychol. 2020;11:618509. doi:10.3389/fpsyg.2020.618509
13. Iloh GU, Ikwudinma AO, Obiegbu NP. Obesity and its cardio-metabolic co-morbidities among adult Nigerians in a primary care clinic of a tertiary hospital in South-Eastern, Nigeria. J Family Med Prim Care. 2013;2:20–26. doi:10.4103/2249-4863.109936
14. Zeng Y, Huang X, Chen C, et al. A randomized, controlled clinical trial of combining therapy with traditional Chinese medicine-based psychotherapy and Chinese herbal medicine for menopausal women with moderate to serious mood disorder. Evid Based Complement Alternat Med. 2019;2019:9581087. doi:10.1155/2019/9581087
15. Hu LX, Tang M, Hua W, et al. Psychological disturbances and their association with sleep disturbance in patients admitted for arrhythmia diseases. Neuropsychiatr Dis Treat. 2022;18:1739–1750. doi:10.2147/NDT.S370128
16. Azhar A, Mahmood A, Hasan F, Tauseef A, Shahzad A, Tarin TA. Association of working environment and anxiety levels in clinical professionals during the COVID-19 pandemic. Cureus. 2021;13:e17450. doi:10.7759/cureus.17450
17. Yang M, He P, Xu X, et al. Disrupted rhythms of life, work and entertainment and their associations with psychological impacts under the stress of the COVID-19 pandemic: a survey in 5854 Chinese people with different sociodemographic backgrounds. PLoS One. 2021;16:e0250770. doi:10.1371/journal.pone.0250770
18. Li R, Yan R, Cheng W, Ren H. Effect of resistance training on heart rate variability of anxious female college students. Front Public Health. 2022;10:1050469. doi:10.3389/fpubh.2022.1050469
19. Lu J, Xu X, Huang Y, et al. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2021;8(11):981–990. doi:10.1016/S2215-0366(21)00251-0
20. Eyigor H, Arihan G, Ergin F, Barlik Y. Kronik farenjitli hastalarda psikiyatrik hastalik profili [Psychiatric disorder profile in patients with chronic pharyngitis]. Kulak Burun Bogaz Ihtis Derg. 2006;16:178–182. Turkish
21. Lieb R, Becker E, Altamura C. The epidemiology of generalized anxiety disorder in Europe. Eur Neuropsychopharmacol. 2005;15(4):445–452. doi:10.1016/j.euroneuro.2005.04.010
22. Nikbakhsh N, Moudi S, Abbasian S, Khafri S. Prevalence of depression and anxiety among cancer patients. Caspian J Intern Med. 2014;5:167–170.
23. Misgan E, Belete H. High-level of anxiety and depressive symptoms among patients with general medical conditions and community residents: a comparative study. BMC Psychiatry. 2021;21(1):324. doi:10.1186/s12888-021-03336-6
24. Meyza KZ, Boguszewski PM, Nikolaev E, Zagrodzka J. Age increases anxiety and reactivity of the fear/anxiety circuit in Lewis rats. Behav Brain Res. 2011;225(1):192–200. doi:10.1016/j.bbr.2011.07.011
25. Lund C, Breen A, Flisher AJ, et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med. 2010;71(3):517–528. doi:10.1016/j.socscimed.2010.04.027
26. Sareen J, Afifi TO, McMillan KA, Asmundson GJG. Relationship between household income and mental disorders: findings from a population-based longitudinal study. Arch Gen Psychiatry. 2011;68(4):419–427. doi:10.1001/archgenpsychiatry.2011.15
27. Wang X, Shang S, Yang H, et al. Associations of psychological distress with positive psychological variables and activities of daily living among stroke patients: a cross-sectional study. BMC Psychiatry. 2019;19(1):381. doi:10.1186/s12888-019-2368-0
28. Akbulut S, Ozer A, Saritas H, Yilmaz S. Factors affecting anxiety, depression, and self-care ability in patients who have undergone liver transplantation. World J Gastroenterol. 2021;27(40):6967–6984. doi:10.3748/wjg.v27.i40.6967
29. Hao W, Tang Q, Huang X, Ao L, Wang J, Xie D. Analysis of the prevalence and influencing factors of depression and anxiety among maintenance dialysis patients during the COVID-19 pandemic. Int Urol Nephrol. 2021;53(7):1453–1461. doi:10.1007/s11255-021-02791-0
30. Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655–672. doi:10.1177/0164027504268574
31. Beutel ME, Klein EM, Brahler E, et al. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17(1):97. doi:10.1186/s12888-017-1262-x
32. Wang Z, Shu D, Dong B, Luo L, Hao Q. Anxiety disorders and its risk factors among the Sichuan empty-nest older adults: a cross-sectional study. Arch Gerontol Geriatr. 2013;56(2):298–302. doi:10.1016/j.archger.2012.08.016
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
