Back to Journals » International Journal of General Medicine » Volume 15
Prevalence and Risk Factors of Abnormal Carotid Artery in Young Adults without Overt Cardiovascular Disease
Authors Teng Y, Wang K, Fan X, Yang X
Received 29 January 2022
Accepted for publication 13 April 2022
Published 3 May 2022 Volume 2022:15 Pages 4595—4601
DOI https://doi.org/10.2147/IJGM.S360437
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yunjie Teng1 *, Kaiyang Wang2 *, Xue Fan,1 Xiaoping Yang1
1Center of Health Management, First Affiliated Hospital of Xinjiang Medical University, Urumqi, People’s Republic of China; 2Department of Cardiology, First Affiliated Hospital of Xinjiang Medical University, Urumqi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoping Yang, Center of Health Management, First Affiliated Hospital of Xinjiang Medical University, Urumqi, People’s Republic of China, Email [email protected]
Objective: The current study was to evaluate the prevalence of increased carotid artery intimal-medial thickness (IMT) and carotid plaque in young individuals and factors associated with increased IMT and carotid plaque were also assessed.
Methods: Individuals between 18 and 44 years old who underwent an annual health examination and without cardiovascular disease were included. The value of IMT ≥ 0.1 cm was defined as increased IMT and IMT ≥ 0.15 cm was defined as carotid plaque. Based on the IMT, participants were divided into normal and abnormal groups.
Results: A total of 551 individuals were included and the mean age was 38.9 years old, with women accounting for 32.5% (n=179) and 238 (43.2%) individuals with abnormal IMT. Those with abnormal IMT was older, more likely to be male and smoking, had higher blood pressure (BP) and body mass index (BMI). Individuals with abnormal MIT also had worse lipid profiles, higher serum levels of fasting plasma glucose (FPG), HbA1c, homocysteine, and uric acid. Age, male sex, elevated systolic and diastolic BP, BMI, HbA1c, FPG, triglyceride, total cholesterol, LDL-C, homocysteine, and uric acid were positively correlated with IMT, while HDL-C was negatively correlated with IMT. Factors associated with increased IMT and carotid plaque included age, male sex, BMI, triglyceride, LDL-C, homocysteine, uric acid, and smoking.
Conclusion: Among apparent healthy young individuals, the prevalence of increased IMT was high and there were several factors associated with increased IMT. Further studies are needed to evaluate how to be better in preventing the development of subclinical atherosclerosis among young individuals.
Keywords: intimal-medial thickness, carotid plaque, risk factors
Introduction
Despite advances in primary prevention being achieved in the last two decades, atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of morbidity and mortality in China and worldwide.1–4 Prior studies have demonstrated that the factors contributing to the initiation and progress of atherosclerosis are diverse, including advancing age, smoking, obesity, diabetes mellitus, dyslipidemia, and hypertension, among others.5,6 Notably, most of these findings were derived from middle-to-older age populations with established ASCVD, and the data on the apparent healthy young populations are limited. Furthermore, these data are remarkably lacking in the Chinese populations.
Carotid artery intimal-medial thickness (IMT) is a marker of early atherosclerosis.7–9 With the progress of atherosclerosis, carotid plaque may develop subsequently.10 Prior studies have shown that increased IMT or the presence of carotid plaque portends an increased risk of developing ischemic stroke and myocardial infarction.8,11 Therefore, it is critically important to assess the carotid artery with ultrasound so as to identify high-risk populations.
Prior epidemiologic studies show that in the last two decades, the prevalence of ASCVD has increased significantly in China, especially among young individuals, which is due to smoking, physical inactivity, environmental pollution, and unhealthy lifestyle, among others.1,6,12 Therefore, it is clinically relevant to determine the prevalence of subclinical ASCVD, such as increased IMT or prevalent carotid plaque, in the young populations, which in turn can help inform effective targeted preventive therapy. To the best of our knowledge, there are few studies which have evaluated the prevalence of subclinical ASCVD in individuals between the ages of 18–44 years old. In addition, factors associated with the prevalence of subclinical ASCVD in young populations are also unknown. Herein, through collecting data from apparently healthy young individuals during annual health examination in the outpatient department of our hospital, the aims of the current study are to evaluate: 1) the prevalence of subclinical ASCVD (namely increased IMT and carotid plaque) in the young individuals; and 2) factors associated with increased IMT and carotid plaque.
Methods
Study Design and Participants Enrollment
This is a cross-sectional study and the current study was approved by the Clinical Research Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University. Written informed consent was obtained before participants’ enrollment. Individuals between the ages of 18–44 years who underwent an annual health examination were screened for eligibility of the current study. All the examinations were conducted in accordance with the Declaration of Helsinki. Individuals who had a documented history of hypertension, diabetes mellitus, abnormality in liver or kidney function, coronary artery disease, infectious disease, malignant disease, systemic inflammatory disease, or therapy with lipid lower medications were excluded.
Data Collection
Data was collected during the health examination. Demographics (eg, age and sex) and anthropometrics (eg, body weight and height) were collected and entered into the standardized health record form. Body weight in kilograms and height in meters were used to calculate body mass index (BMI) based on the formula as follows: BMI=weight (kg)/height (m2). Fasting venous blood was used to measure lipid profiles, fasting plasma glucose (PFG), glycated hemoglobin A1c (HbA1c), renal function, uric acid, and homocysteine. Blood pressure (BP) was measured according to the China hypertension guideline recommendation. Specifically, participants were required to stay at rest in a sitting position for 5 minutes, and two BP measurements were performed with a 1-minute interval with the arm positioned at the heart level using an Omron HEM-7051 device (Omron HealthCare, Kyoto, Japan). The average value of two BP readings was used. If the first two BP readings differed by >5 mm Hg, an additional measurement was performed and the mean value of three readings was used.
Assessment of Carotid Artery Using Ultrasound
Assessment of the carotid artery was performed using a 7.5–10 MHz linear array transducer (Siemens ACUSON Cypress) by experienced ultrasonographers who were blinded to the characteristics of all participants. Common carotid artery (1 mm below the carotid artery bifurcation) was chosen to evaluate IMT, and measurements were performed 3-times on both sides. The values of IMT were averaged by the left- and right-sided IMT values, and the largest average value was used in the current study. In brief, IMT ≥0.1 cm was defined as increased IMT and IMT ≥0.15 cm was defined as carotid plaque accordingly.13 Based on the IMT, participants were divided into normal (IMT <0.1 cm) and abnormal (IMT ≥0.1 cm) groups.
Statistical Analysis
Continuous variables with normal distribution were expressed as mean±standard deviation, or presented as median (interquartile range). Categorical variables were presented as frequencies and percentages. Student’s t-test was used to compare continuous variables with normal distribution and Mann–Whitney U-test was used to evaluate variables with skewed distribution. Comparisons of categorical variables were performed using Chi-squared test or Fisher’s exact test. Pearson or Spearman correlation analysis was performed to evaluate the relationship between IMT and factors of interest. Univariate binary logistic regression analyses were performed to evaluate the association between factors with increased IMT or carotid plaque. In addition, factors in the univariate analysis with a P-value <0.1 were entered into the multivariate logistic regression analyses to further evaluate the association between factors with increased IMT or carotid plaque. Odds ratio (OR) and 95% confidence interval (CI) were reported. All analyses were performed with SPSS version 17.0 for Windows, and a two-sided P-value of less than 0.05 was considered to indicate statistical significance.
Results
Baseline Characteristics
A total of 551 individuals aged 18–44 years old were included for the current analysis. The mean age was 38.9±5.7 years old, women accounted for 32.5% (n=179), and 238 individuals had abnormal IMT (43.2%). As presented in Table 1, compared to individuals with normal IMT, those with abnormal IMT were older, more likely to be male and smoking, and had higher blood pressure and BMI. In addition, individuals with abnormal MIT also had worse lipid profiles, higher serum levels of FPG, HbA1c, homocysteine, and uric acid. Among individuals with abnormal IMT, 117 (49.2%) had increased IMT, 114 (47.9%) had isolated carotid plaque, and seven (2.9%) had multiple carotid plaque, respectively.
 |
Table 1 Baseline Characteristics |
Factors Correlated with IMT
As presented in Table 2, age, male sex, systolic and diastolic BP, BMI, HbA1c, FPG, triglyceride, total cholesterol, low density lipoprotein-cholesterol, homocysteine, and uric acid were positively correlated with IMT, while high density lipoprotein-cholesterol was negatively correlated with IMT. The correlation coefficient was the largest with BMI and followed by age.
 |
Table 2 Factors Correlated with IMT |
Association Between Factors with Increased IMT and Carotid Plaque
In the univariate binary logistic regression analysis (Table 3), factors associated with increased IMT included age, male sex, BMI, triglyceride, low density lipoprotein-cholesterol, homocysteine, uric acid, and smoking. These factors were also associated with carotid plaque. After multivariate regression analysis, factors which remained associated with increased IMT included age, BMI, low density lipoprotein-cholesterol, homocysteine, and smoking; and factors which remained associated with carotid plaque included age, male sex, BMI, triglyceride, low density lipoprotein-cholesterol, homocysteine, and smoking (Table 4).
 |
Table 3 Association Between Factors with Increased IMT and Carotid Plaque (Univariate Analysis) |
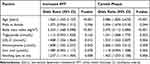 |
Table 4 Association Between Factors with Increased IMT and Carotid Plaque (Multivariate Analysis) |
Discussion
There are two potentially clinical important findings of the current study: 1) among apparent healthy young individuals, the prevalence of subclinical atherosclerosis, including increased IMT or the presence of carotid plaque, was high, with a prevalence of 43.2%; and 2) there were several factors associated with increased IMT and carotid plaque. These findings together suggest that it is warranted to routinely assess IMT in apparent healthy young individuals and interventions are needed to target several common risk factors such as BP and metabolic disorder.
Prior studies from western populations have shown that an increase in BP, low density lipoprotein cholesterol, fasting plasma glucose, smoking, physical inactivity, and obesity were associated with endothelial dysfunction, systemic inflammation, and oxidative stress.14–16 These pathophysiological alterations together contribute to the initiation of subclinical atherosclerosis. Notably, the carotid artery is one of the vessels which develops subclinical atherosclerosis at an early stage. Epidemiologic studies have demonstrated the relationship between increased IMT and cardiovascular outcomes.17–19 However, most of these data were from middle-to-old age Caucasian populations. The data about the prevalence of subclinical atherosclerosis in the apparent young Chinese individuals is limited. In addition, factors associated with subclinical atherosclerosis are also undetermined.
In the current study, we included 551 individuals aged 18–44 years without prevalent hypertension, dyslipidemia, diabetes mellitus, and overt cardiovascular disease. The results suggested the prevalence of increased IMT was above 40%, suggesting that subclinical atherosclerosis developed during the young age. Notably, beyond traditional risk factors, genetic background, unhealthy diet, environment pollution, and mental stress during young age, among others have also been identified as potential risk factors for ASCVD. Indeed, an epidemiologic study from Chinese adolescents shows that the prevalence of obesity was increased in the last three decades which were partly due to the unhealthy diet.20–22 In addition, the Chinese adolescent did not have sufficient physical activity after school. Furthermore, environment pollution in the last two decades might also contribute to the early onset of atherosclerosis in the young individuals. These findings have significant clinical implications. First, we should routinely assess IMT during annual health examination for the apparent healthy young individuals. Second, targeted intervention, such as losing weight, should be implemented. Third, strategies focused on multifaceted levels are needed. In addition to body weight reduction, we consider that mitigating other risk factors, such as dyslipidemia, diabetes mellitus, and hypertension, should also be important approaches. Indeed, several studies have demonstrated that lipid lowering medications, antidiabetic drugs, and antihypertensive therapy can reduce IMT and retard carotid plaque. Further studies are needed to explore whether these strategies are effective for the apparent healthy young individuals with increased IMT and carotid plaque.
We also investigated factors associated with increased IMT and carotid plaques. Notably, age, BMI, laboratory parameters of metabolic disorders, and smoking were associated with the subclinical atherosclerosis. Notably, among these factors, most are modifiable except for age. Through regular exercise and healthy diet, it is feasible to decrease BMI and improve lipid metabolism and reduce uric acid. Discontinuation of smoking is also feasible with positive reinforcement and family support. Homocysteine is a marker which is associated with endothelial dysfunction, increased platelet activity and pro-coagulation status.23,24 Improvements in diet and physical activity are also able to reduce the homocysteine level. These findings suggest that among young individuals without comorbidities and overt cardiovascular disease, adherence to a healthy lifestyle is essential to prevent the development of subclinical atherosclerosis.
The current study included apparent healthy young individuals and the results suggested a high prevalence of increased IMT and carotid plaque in these populations. Since increased IMT and carotid plaque are associated with cardiovascular event, we consider that preventive and therapeutic strategies are needed for these populations group. Since obesity, hypertension, dyslipidemia and diabetes mellitus are the four common risk factors for atherosclerosis, strictly controlling these risk factors through maintaining a healthy lifestyle and regular moderate-to-vigorous exercise could provide a cost-effective approach to prevent carotid plaque and reduce IMT in a population-level.
There are some limitations of the current study. First, this was an observational study and the findings could only be used for hypothesis generation. Second, we included apparent healthy young individuals and the findings might not be able to extrapolate to those with prevalent comorbidities or cardiovascular disease. Third, data were from annual health examination and whether these findings can be extrapolated to outpatient clinic patients is also unknown. Fourth, since only one person assessed the participants, there was a possible bias introduced since ultrasound is operator-dependent. Fifth, since this was a single institutional study, the findings might not be extrapolated to other population groups. Last but not the least, although we postulated that the early onset of subclinical atherosclerosis might be due to unhealthy diet and environment pollution, among others, we did not capture these data and future studies are needed to collect these data so as to better understand the mechanisms underlying early onset subclinical atherosclerosis.
Conclusion
In conclusion, results of the current study show that, among apparent healthy young individuals, the prevalence of increased IMT was high and there were several traditional factors associated with increased IMT. Further studies are needed to evaluate how be better prevent the development of subclinical atherosclerosis among young individuals.
Acknowledgments
We appreciate very much all the participants and their families. Yunjie Teng and Kaiyang Wang are co-first authors for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ma LY, Chen WW, Gao RL, et al. China cardiovascular diseases report 2018: an updated summary. JGC. 2020;17(1):1–8. doi:10.11909/j.issn.1671-5411.2020.01.001
2. Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi:10.1016/j.jacc.2020.11.010
3. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi:10.1038/s41569-018-0119-4
4. Du X, Patel A, Anderson CS, Dong J, Ma C. Epidemiology of cardiovascular disease in china and opportunities for improvement: JACC International. J Am Coll Cardiol. 2019;73(24):3135–3147. doi:10.1016/j.jacc.2019.04.036
5. Roth GA, Forouzanfar MH, Moran AE, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372(14):1333–1341. doi:10.1056/NEJMoa1406656
6. Yusuf S, Rangarajan S, Teo K, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371(9):818–827. doi:10.1056/NEJMoa1311890
7. Bos D, Arshi B, Van den Bouwhuijsen QJA, et al. Atherosclerotic carotid plaque composition and incident stroke and coronary events. J Am Coll Cardiol. 2021;77(11):1426–1435. doi:10.1016/j.jacc.2021.01.038
8. Kopczak A, Schindler A, Bayer-Karpinska A, et al. Complicated carotid artery plaques as a cause of cryptogenic stroke. J Am Coll Cardiol. 2020;76(19):2212–2222. doi:10.1016/j.jacc.2020.09.532
9. Liao H, Li Z, Zheng D, et al. Increased Hs-CRP/adiponectin ratio is associated with increase carotid intima-media thickness. Lipids Health Dis. 2014;13:120. doi:10.1186/1476-511X-13-120
10. Finn AV, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol. 2010;30(2):177–181. doi:10.1161/ATVBAHA.108.173609
11. Vesa SC, Vlaicu SI, Vacaras V, et al. CYP4F2 and VKORC1 polymorphisms amplify the risk of carotid plaque formation. Genes. 2020;11(7):822. doi:10.3390/genes11070822
12. Feng Z, Liu C, Guan X, Mor V. China’s rapidly aging population creates policy challenges in shaping a viable long-term care system. Health aff. 2012;31(12):2764–2773. doi:10.1377/hlthaff.2012.0535
13. Mukherjee D, Yadav JS. Carotid artery intimal-medial thickness: indicator of atherosclerotic burden and response to risk factor modification. Am Heart J. 2002;144(5):753–759. doi:10.1067/mhj.2002.124865
14. Greenfield JR, Samaras K, Jenkins AB, et al. Obesity is an important determinant of baseline serum C-reactive protein concentration in monozygotic twins, independent of genetic influences. Circulation. 2004;109(24):3022–3028. doi:10.1161/01.CIR.0000130640.77501.79
15. Allison MA, Tiefenbrun J, Langer RD, Wright CM. Atherosclerotic calcification and intimal medial thickness of the carotid arteries. Int J Cardiol. 2005;103(1):98–104. doi:10.1016/j.ijcard.2004.12.039
16. Zhu W, Chen T, Jin L, et al. Carotid artery intimal medial thickness and carotid artery plaques in hypertensive patients with non-arteritic anterior ischaemic optic neuropathy. Graefe’s Arch Clin Exp Ophthalmol. 2017;255(10):2037–2043. doi:10.1007/s00417-017-3744-4
17. Everson-Rose SA, Mendes de Leon CF, Roetker NS, Lutsey PL, Alonso A. Subclinical cardiovascular disease and changes in self-reported mobility: multi-ethnic study of atherosclerosis. J Gerontol a Biol Sci Med Sci. 2018;73(2):218–224. doi:10.1093/gerona/glx103
18. Guo W, Gong Y, Li J, et al. Association of serum proprotein convertase subtilisin/kexin type 9 with early atherosclerosis in newly diagnosed type 2 diabetes mellitus. NMCD. 2019;29(8):815–821. doi:10.1016/j.numecd.2019.04.006
19. Wong ND, Zhao Y, Quek RGW, et al. Residual atherosclerotic cardiovascular disease risk in statin-treated adults: the multi-ethnic study of atherosclerosis. J Clin Lipidol. 2017;11(5):1223–1233. doi:10.1016/j.jacl.2017.06.015
20. Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9(6):373–392. doi:10.1016/S2213-8587(21)00045-0
21. Han Y, Hu Y, Yu C, et al. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur Heart J. 2021;42(34):3374–3384. doi:10.1093/eurheartj/ehab413
22. Zhang X, Zhang M, Zhao Z, et al. Geographic variation in prevalence of adult obesity in china: results from the 2013–2014 national chronic disease and risk factor surveillance. Ann Intern Med. 2020;172(4):291–293. doi:10.7326/M19-0477
23. Pushpakumar S, Kundu S, Sen U. Endothelial dysfunction: the link between homocysteine and hydrogen sulfide. Curr Med Chem. 2014;21(32):3662–3672. doi:10.2174/0929867321666140706142335
24. Ahmad A, Corban MT, Toya T, et al. Coronary microvascular endothelial dysfunction in patients with angina and nonobstructive coronary artery disease is associated with elevated serum homocysteine levels. J Am Heart Assoc. 2020;9(19):e017746. doi:10.1161/JAHA.120.017746
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
