Back to Journals » Advances in Medical Education and Practice » Volume 13
Prevalence and Determinants of Mental Health Problems and Mental Health Stigma Among Medical Students of Different Nationalities in Qatar
Authors Mahgoub Y, Daher-Nashif S, Al-Shebly R, Wali HS, Khan A, Almarkhi A, Al-Motawa M, AlObaidan G, Al-Muhannadi Z
Received 16 April 2022
Accepted for publication 8 August 2022
Published 24 August 2022 Volume 2022:13 Pages 969—979
DOI https://doi.org/10.2147/AMEP.S371053
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Yasmine Mahgoub,1 Suhad Daher-Nashif,2 Rafal Al-Shebly,1 Hamza Said Wali,1 Aisha Khan,1 Ameera Almarkhi,1 Maryam Al-Motawa,1 Ghalya AlObaidan,1 Zamzam Al-Muhannadi1
1College of Medicine, QU Health, Qatar University, Doha, Qatar; 2Population Medicine Department, College of Medicine, QU Health, Qatar University, Doha, Qatar
Correspondence: Suhad Daher-Nashif, Population Medicine Department, College of Medicine, QU Health, Qatar University, Doha, Qatar, Email [email protected]; [email protected]
Introduction: Past studies have shown high prevalence of mental illness among medical students. This is often linked to the demands of the medical curriculum, and to mental health stigma that prevents students from seeking help. This study aimed to examine experiences of mental health problems among medical students of different nationalities in Qatar and to uncover sociodemographic factors related to their prevalence and associated stigma.
Methods: A cross-sectional online survey was conducted with medical students in their second through fifth years at the College of Medicine at Qatar University. The survey began with a consent form, and those agreed to take the survey were directed to the questionnaire. The survey comprised 64 items across three sections. The first section collected sociodemographic data. The second section screened depressive symptoms using the PHQ-9; anxiety symptoms using GAD-7; and psychological distress symptoms using Kessler-6. The third section included 27 questions adopted from Schwenk et al, which evaluate students’ perceptions of stigma and their attitudes toward seeking help with their mental health.
Results: One hundred and eighty-two students participated in the study. The prevalence of self-reported symptoms of severe depression, anxiety, and psychological distress was 4.4% (95% CI 2– 9), 10.4% (95% CI 7– 16), and 39.6% (95% CI 33– 47), respectively; the prevalence of high stigma was 31.9% (95% CI 25– 39). Parental education, repetition of an academic year, progress in medical studies, gender, and nationality had statistically significant correlations with mental health problems and stigma.
Conclusion: In addition to the impact of the requirements of medical study, the high prevalence of reported mental illness among medical students is impacted by sociodemographic factors and the mental health stigma that constitutes a barrier to seeking help. Preventive wellbeing programs should be an essential component of medical curricula.
Keywords: mental health problems, mental health stigma, medical students, problem based learning curriculum, sociodemographic factors, Middle East
Introduction
Several studies have demonstrated an increased prevalence of mental illness among medical students relative to the general population.1–4 For example, Gaspersz et al found that the incidence of common mental disorders (including depression, anxiety, stress, and post-traumatic stress disorder [PTSD]) among medical students was 54% in the pre-clinical phase, and 48% in the clinical phase.5 A meta-analysis of 59 studies providing a comprehensive summary of the mental health of medical students in Brazil found the prevalence of depression, stress, common mental disorders, and burnout to be 30.6%, 49.9%, 31.5%, and 13.1% respectively.6 These and other studies recommend acknowledging and making attempts to alleviate the mental health consequences of studying medicine.7,8 Experiencing mental illness during medical studies has implications for students’ ability to apply cognitive, social, and clinical skills, ultimately leading to reduced competency in providing future patient care.9 Several researchers in the Arab region have addressed the high prevalence of mental illness among medical students. In a systematic literature review, Elzubeir et al asserted that studies on Arab medical students’ mental health report a high prevalence of perceived stress, depression, and anxiety.10 A study conducted in Jordan reported a high level of exhaustion (91%), disengagement (87%), and “minor” psychiatric illness (92%) among medical students.11 The same study also used the CAGE questionnaire to evaluate alcohol use among students, and found that 8% of students qualified as possibly alcoholic.11 Another study conducted among medical students in Oman, a Gulf state with a socioeconomic context similar to Qatar’s, found that the prevalence of Burnout Syndrome and depressive symptoms were 7.4% and 24.5% respectively; these figures were higher among preclinical stage undergraduates than among clinical stage students.12 These and other studies highlight the importance of addressing medical students’ mental health problems and call for a deeper understanding of the factors behind them. Mental health stigma (MHS) is a major barrier to seeking help for mental health problems among medical students, leading to the exacerbation of the symptoms of mental health disorders.1,13 Erving Goffman described stigma as a process by which an individual with an attribute that is deeply discredited by their society is rejected as a result of that attribute.14 Based on this definition, the World Health Organization (WHO) refers to stigma as “a mark of shame, disgrace or disapproval which results in an individual being rejected, discriminated against, and excluded from participating in a number of different areas of society”.15 In 2001, the WHO identified MHS as a key barrier to effective treatment of mental illness due to its negative impact on individuals’ willingness to seek treatment.16 Studies conducted in Western contexts show a correlation between MHS, hesitancy to seek help, and increasing symptom burden.1,17–19 For example, a cross sectional study of medical students at Michigan University identified stigma as an explicit barrier to the use of mental health services for 30% of first- and second-year medical students experiencing depression.1 In another study conducted in Poland, both medical students and psychiatrists reported negative implicit attitudes towards mental illness.18 Maalouf et al point out that stigma is scarcely addressed in mental health reports coming from the Arab region.19 Similarly, Dardas and Simmons argue that little is known about how MHS manifests within the Arab community, making it difficult to design and test interventions.20
Despite this gap in the literature, a few studies have reported on the impact of sociocultural values and religious beliefs on MHS. For instance, Ghuloum et al found that over a third of respondents in Qatar’s general population (40.6%) believed that people with mental health disorders are intellectually disabled (their study used the term “mentally retarded”), and 48.3% believed that mental illness is a punishment from God.21 Shehata et al’s study of stigmatizing beliefs about mental illness among health sciences students and medical students in Egypt found that the majority of students held stigmatizing beliefs.22 The positive correlation between MHS and medical students’ reluctance to seek help has been evidenced by several researchers.1,13 The prevalence of MHS among medical students can impact whether and how they seek help when they face mental health problems, which may lead to poor academic performance, substance abuse, damaged self-image, and eventually a decline in clinical practice and fitness to work with patients in the future.
In this study we aim to determine the prevalence of mental illnesses among medical students in Qatar, taking the students in College of Medicine (CMED) at Qatar University as a case study to represent medical students in similar Middle Eastern contexts. This is the first study of its type in Qatar, and as such, it contributes valuable knowledge for building tailored mental health preventive and intervention programs for medical students. This study is also the first to investigate these issues in the context of a problem-based learning (PBL) curriculum in the Arab region; Elzubeir et al10 noted that literature on medical students’ mental health in this specific type of academic programme was lacking in the region.
Methods
Study Design
A cross-sectional survey was conducted using the online survey platform Google Forms in August and September 2019, targeting all 250 medical students in the second to fifth years of the programme. Participants were required to complete a consent form before accessing the survey. The survey consisted of three parts. The first gathered sociodemographic data on each student; the second identified the prevalence of mental health problems among the students using standardized screening tools; and the third examined students’ views on stigma. Since the instruction language in the college is English and students are fully proficient in the English language, all materials were distributed using the original English versions.
Setting
The College of Medicine (CMED) at Qatar University was established in 2015, and is one of the only two medical schools in Qatar. The medical program in CMED at Qatar University consists of six years. The first year is transition phase, in which students study the basic core subjects that prepare them for the medical curriculum. This is followed by two and a half years, which constitute the pre-clerkship phase, in which students study the basic medical sciences using a problem-based learning pedagogical approach. Finally, in the last two and a half years, known as the clerkship phase, students continue their studies in hospitals and other clinical environments. The students are of different nationalities, with a majority of Arab-Muslims and a minority of Muslims non-Arabs from Asian countries such as Pakistan, Bangladesh, and the Philippines. All non-Qatari students are children of expatriates and were born and raised in Qatar.
Inclusion and Exclusion Criteria
The inclusion criteria included respondents who were in at least their second year and were actively enrolled in medical studies. The study excluded Phase I students, who were not yet studying basic medical sciences. The study also excluded students who had dropped out. At the time of the study, there were no sixth-year students.
Survey Instruments
The survey consisted of a total of 64 questions divided among the three sections.
Sociodemographic Data
This section was based on the sociodemographic section of the WHO’s Study of Global Aging and Adult Health (SAGE). SAGE is a longitudinal study implemented in several countries with the primary goal of generating valid, reliable, and comparable information on a range of health and well-being outcomes that hold importance to public health.22 It is a standardized survey instrument which collects basic sociodemographic data such as age, gender, nationality, marital status, current accommodation status, family income, and parents’ level of education and employment history. In addition we added two questions about year of study, and a year repetition.
Symptoms of Depression, Anxiety, and Psychological Distress
The second section collected data on the students’ mental health using three standardized screening tools: the Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder (GAD-7), and Kessler Psychological Distress Scale (K6). These tools have been previously validated for screening purposes globally and regionally, and they are commonly used in Qatar in clinical settings and for research and screening purposes with the general population.23–25
The American Psychological Association (APA) reports, based on previous studies assessing the PHQ-9, that the tool exhibits good diagnostic validity; scores greater than 10 had a sensitivity and specificity of 88% for Major Depressive Disorder.26 It also has high internal consistency and well-constructed psychometric properties.26 Accordingly, the Diagnostic and Statistical Manual of Mental Disorders (DSM)-5 recommends its use as a tool to evaluate the severity of depression.27 This study utilized the 9-item PHQ-9 to assess for self-reported symptoms of depression. A score of 5–9 indicates mild symptoms, a score of 10–14 moderate symptoms, a score of 15–19 moderately severe symptoms, and a score of 20–27 severe symptoms.
Several international studies conducted in Bangladesh, Korea, Portugal, United States, Iran, Germany and Peru have examined the validity and reliability of the GAD-7 tool across many different populations and found it to have high internal consistency as well as good convergent validity.28 Spitzer et al29 confirm that the GAD-7 has good reliability, in addition to criterion, construct, factorial, and procedural validity, indicating that it is a valid and efficient tool for the assessment GAD in research and in clinical practice. A score of 6–10 on the GAD-7 indicates mild anxiety, a score of 11–15 moderate anxiety, and a score of 16–21 severe anxiety.
Country-specific validation studies assessing the K-6 tool in different languages, including English, have come to the consensus that this tool has good internal consistency reliability (0.69–0.92 in Cronbach’s alpha) and factor-based and other construct validity (ie, correlations with other mental health measures) across various populations. Furthermore, multiple studies have demonstrated its effectiveness in measuring non-specific psychological distress in non-clinical populations, including Arab populations and student populations.30,31 A score of 1–5 on the K-6 indicates mild distress, a score of 6–10 moderate distress, and a score of 11–24 severe distress.
Mental Health Stigma
The third and final section consisted of 27 questions adopted from Schwenk et al1 which were used to evaluate respondents’ levels of stigmatizing beliefs about mental health and their attitudes toward seeking help. The items in this section addressed points identified in previous studies and implemented both positive and negative framing to allow for an internal consistency check. Section three also included validated instruments on stigma used in studies of the general population. Focus group discussions and pilot-testing were performed to modify the questions. These items were specifically tailored to fit medical students.1 Cronbach’s alpha was used as a measure of internal consistency reliability for this section and was found to be 0.789, which represents acceptable internal consistency.
Study Size and Bias
The population of our study was well-defined and small, since the medical student community in Qatar is limited; therefore, total population sampling was used to minimize potential bias occurring through sampling technique. Five responses were eliminated due to possible response bias, as these participants had selected extreme values on the Likert scales for all items.
Statistical Data Analysis
Statistical analyses of the survey responses were performed using the STATA 16.0 software package.
Determination of Depression, Generalized Anxiety, and Psychological Distress
To evaluate the prevalence of depression, generalized anxiety, and psychological distress, the scores for the three screening tools in the second section of the survey were calculated. The established standardized cut-off scores for each screening tool were then used to classify respondents as exhibiting “no”, “mild”, “moderate”, “moderately severe”, or “severe” symptoms of depression and “no”, “mild”, “moderate”, or “severe” symptoms of anxiety and psychological distress (see Supplementary Materials - Table S1). To further facilitate statistical analysis, students were then divided into “low-risk” and “high-risk” groups for each disorder using standardized cut-off scores that indicate a highly likely requirement for medical intervention (Supplementary Materials - Table S2). Separate stepwise logistic regressions were run to test the correlation between the risk of depression, anxiety, and psychological distress and each of the sociodemographic factors to assess the impact of these factors on the students’ mental health.
Determination of Mental Health Stigma
The questions in the third section of the survey were classified as positive or negative with regard to the respondents’ viewpoints on stigma. Positive questions were those for which a response of “agree” demonstrated stigmatizing view; therefore, “agree” responses were assigned a score of 1 and “disagree” a score of 0. Negative questions were those for which an “agree” response revealed no evidence of stigma; therefore, “agree” responses for such questions were assigned a score of 0 and “disagree” a score of 1. An overall stigma score was calculated for each respondent. The MHS scores were then divided into three quantiles, with the two lower quantiles defined as students holding lower levels of stigma and the upper quantile as students with high stigma. Stepwise regression using a p-value <0.2 was used to determine which sociodemographic factors were associated with high stigma.
Ethics and Informed Consent
This study complies with the Declaration of Helsinki, and received ethical approval from Qatar University’s Institutional Review Board (reference number: QU-IRB 1052-E/19). Participants gave informed consent using an online form, which they were required to complete prior to accessing the survey questions. As this study was anonymous, participants who were found to have severe depression, anxiety, or psychological stress could not be referred for care; however, the survey included a section that advised the students to call a hotline operated by Hamad Medical Corporation if they answered certain questions positively.
Results
Characteristics of the Participants
The overall survey response rate was 74.8%. The response rates for second, fourth, and fifth-year students were 83%, 85%, and 76% respectively. The response rate for third-year students was lower, at 48%. Five responses were eliminated due to response bias, as these participants had selected extreme values on the Likert scales for all items. Of the remaining sample of students (n=182), 68.1% were female and 31.9% were male. 36.3% of respondents were Qatari, 45.1% were from other GCC and Middle Eastern countries, and 18.9% were from other countries. The largest age groups represented in the sample were 17–20 (47.3%) and 21–25 (51.1%). The mean age of the students was 21, with a standard deviation of 9.1 (Table 1).
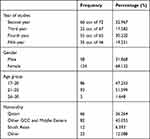 |
Table 1 Participants’ Characteristics |
Prevalence of Self-Reported Symptoms of Mental Health Disorders
Depression
The prevalence was 31% (95% CI 25–38) for mild depressive symptoms and 30% (95% CI 24–37) for moderate depressive symptoms. Eight students exhibited severe depressive symptoms and 32 had moderately severe depressive symptoms, representing a prevalence of 4.4% (95% CI 2–9) and 17.6% (95% CI 13–24) respectively. When categorized into low- and high-risk groups, 52.2% (95% CI 45–59) of the students were classified as having a high risk of depression.
Generalized Anxiety
The rates of mild and moderate symptoms of generalized anxiety were 29% (95% CI 23–36) and 27.5% (95% CI 21–34) respectively. Additionally, 10.4% (95% CI 7–16) of the students exhibited severe symptoms of generalized anxiety. When classified into low- and high-risk groups, 37.9% (95% CI 31–45) of the students were found to have a high risk of anxiety.
Psychological Distress
A total of 60 students, or 33% of participants (95% CI 26–40), were found to demonstrate mild symptoms of psychological distress, while 44 students, or 24% (95% CI 18–31), showed moderate symptoms. The prevalence of severe symptoms of psychological distress was 39.6% (95% CI 33–47). When categorized into low- and high-risk groups, 22% (95% CI 17–29) exhibited a high risk of psychological distress.
Association Between Sociodemographic Factors and Risk of Depressive Symptoms
Stepwise logistic regression indicated that students whose fathers had graduate or postgraduate degrees had lower odds of developing symptoms of depression than those whose fathers had only a primary or secondary education, as indicated by an odds ratio (OR) of 0.14 (95% CI 0.045–0.46; p-value=0.001) and an OR of 0.15 (95% CI 0.046–0.48; p-value=0.001) respectively (Table 2).
 |
Table 2 Logistic Regression for the Association Between Student Sociodemographic Factors and Depression, Anxiety, and Psychological Distress |
Association Between Sociodemographic Factors and Risk of Symptoms of Anxiety
Students whose fathers held graduate or postgraduate degrees also had lower odds of developing symptoms of anxiety compared to students whose fathers had only completed primary or secondary school. This was shown by an OR of 0.26 (95% CI 0.098–0.68; p-value=0.005) and an OR of 0.25 (95% CI 0.097–0.63; p-value=0.006), respectively (Table 2).
Association Between Sociodemographic Factors and Risk of Symptoms of Psychological Distress
Students whose mothers were never employed had higher odds of developing symptoms of psychological distress compared to students with working mothers, as shown by the OR of 3.65 (95% CI 1.84–11.2; p-value=0.024) (Table 2).
Stigma Analysis
The calculation and categorization of students’ stigma scores revealed that 31.9% (95% CI 25 −39) of the students exhibited signs of high stigma against mental illness. Stepwise logistic regression revealed several associated factors, including nationality, whether the student had repeated an academic year, the year of studies the student was currently in, and maternal and paternal levels of education (Table 3).
 |
Table 3 Logistic Regression for the Association Between Student Sociodemographic and High Stigma Perception |
Discussion
Prevalence of Mental Illness Symptoms
In this study, we used self-report screening tools to measure mental illness symptoms. Our findings indicate a higher prevalence of depression among medical students compared to the general population of Qatar.20,32,33 Sharkey argues that “the reported numbers [in the general population] are likely to be underestimated because of the limited diagnostic abilities of primary care doctors” [p20]34. The gap between our findings and past studies on the general population may be explained by the excellent access to and preexisting relationships with research subjects that our context and sample afforded, and/or to our use of screening tools that depend on self-reporting—and thus reflect experience of symptoms—rather than official diagnosis of mental illness. However, the discrepancy remains alarming.
52.2% of the students in our study had moderate to severe levels of depression. This is in line with the results of other studies of medical students in the Arab region, including studies in Saudi Arabia, Jordan, Egypt, and Oman.8–11,35 For instance, a study conducted recently in Oman reported high prevalence of depressive symptoms among medical students.11 The similar environmental and cultural backgrounds in these countries could explain these comparable levels of depression among medical students. These findings are also supported by a meta-analysis conducted by Puthran et al, who found that the global prevalence of depression among medical students is 28%, and medical students in the Middle East are more likely than non-Middle Eastern students to be depressed.36
The prevalence of generalized anxiety disorder among medical students in our study, based on the GAD-7 scale, was found to be 67%. This is also substantially higher than the prevalence among the general population, which has been measured at 10.3%.20,32 It is also higher than the global figure reported in a meta-analysis of 69 studies conducted in February 2019, which reported the prevalence of anxiety among medical students as 33.3%.3
Our study found the prevalence of psychological distress among participants to be 96.71%, with 63.83% reporting moderate to severe symptoms. This is higher than prevalence of psychological distress among medical students in Saudi Arabia and Egypt.8,38,39
Our analysis suggests that these high levels of stress may be attributable to both academic and non-academic factors. The medical curriculum and workload do contribute to the reported stress levels, but MHS and sociodemographic factors also help to explain the numbers amongst medical students in Qatar and other nearby countries.37
Association Between Sociodemographic Factors and Reported Mental Health Problems
We found correlations between mental health and several sociodemographic factors, including parents’ education, academic year, year repetition, gender, and nationality. Our study found that students whose fathers had higher education were less likely to develop depression and anxiety. This is in line with Park et al, who found that the children of mothers with less than a secondary school education had higher odds of experiencing a major depressive episode (MDE).40 They concluded that a low level of maternal education was associated with MDE in early adulthood, independent of paternal education and other childhood and early-adulthood risk factors. This may be because parents with higher education are more aware of the challenges and stressors of academic life and are therefore better able to support their children during their journeys.
Students in their fifth year reported a higher prevalence of depression and anxiety symptoms than students in other years. This finding is in line with other studies conducted in the Middle East,41 but differs from studies conducted elsewhere.35 As a result, there is no consensus in the impact of the year of studies on medical students’ mental health. The differences could be explained by the different medical curricula employed in each college, and the different sociocultural factors between the Middle East, north Africa and the Gulf.
We found that Arab students were at higher odds of developing anxiety compared to their peers from other nationalities and cultural backgrounds. This is consistent with Quek et al, who found that medical students of Middle Eastern and Asian origin are at higher odds of anxiety than students from other parts of the world.3 This could be attributed to the fact that MHS in Middle Eastern societies is considerably higher than in other regions, which could discourage students experiencing mental health challenges from seeking help. This stigmatization leads them to reject being labeled as mentally ill, exacerbating their mental health symptoms due to delays in seeking help, suboptimal treatment, and poor outcomes.39,40 Hankir et al found a positive correlation between MHS and reluctance to seek help among medical students. They posited that medical students hesitated to seek help due to fear of being perceived as less capable and discredited by their colleagues and mentors.12 MHS in general is also a barrier for applying for jobs, renting homes, finding partners, and more.44
Our findings reveal that male students were at twice the odds of developing psychological distress compared to female students. We believe that these findings are due to the patriarchal beliefs common in Middle Eastern cultures, in which men are shamed for revealing mental health problems and those who do are perceived as weak and unworthy, or “not a man”.42 Another possible explanation is the higher mental health literacy among women.45
Our study also found that students whose mothers had never been employed were at greater odds of experiencing psychological distress. This differs from the results reported by others, such as Ibrahim et al, who found lower anxiety risk among students with unemployed mothers, but a higher risk for those with unemployed fathers.37 We argue that the interplay between the medical curriculum and social and sociodemographic factors explains these diverging results in different contexts.
Association Between Sociodemographic Factors and Stigma
Middle Eastern cultures value family honor and the concealing of emotions. These values contribute greatly to stigma regarding mental health services, as those who seek such services could be viewed as weak and thus bring shame to their families.42 Mental health stigma leads to delays in seeking help, suboptimal treatment, and poor outcomes.43 Hence, preventive programs in medical schools should be seen as an essential component of the curriculum.
In a systematic review of studies addressing MHS in the general population in Qatar, Zolezzi et al concluded that “most people have poor mental health literacy, insufficient information about the causes and symptoms of mental illness, and stigmatized perceptions toward people with mental illness” [p1324]47 Zolezzi et al also found a wide range of stigmatizing beliefs, actions, and attitudes regarding the treatment of mental illness.48 This explains our finding that students in Qatar are likely to have stigmatized views of mental health problems, influenced by several sociodemographic factors such as parents’ education, year of studies, and repetition of an academic year.
Past studies have shown that students who have repeated a year of their studies develop low self-esteem and perceive the cause of repeating the year as personal inability to perform, which leads to higher risks of mental health problems and stronger MHS.45,46
We also found a correlation between living with family and higher mental health stigma. Living with family can affect a person with mental illness either positively or negatively depending on whether or not their family responds supportively to the difficulties they face. Families’ attitudes in general often reflect the social stigma toward mental illness. Past studies have indicated that family members of persons with mental illness often express stigma in relation to their relatives’ illnesses.47 This stigma is transferred to the people experiencing mental illness—in this case the medical students—who feel increasingly stigmatized and avoid seeking help.
Implications for Practice
The results of this study demonstrate the need for more effective and numerous awareness campaigns, workshops, and lectures designed to break the stigma surrounding mental illness in the general population and among medical students in particular in Qatar. This will increase the chance that students will seek help in earlier stages of their illnesses and alleviate academic, social, and other complications. We believe that incorporating wellbeing programs in medical schools curricula, tailored to the sociocultural context and the needs of students, can be a preventive action that will encourage students to seek help when they need it. Such programs can help students in manage their time, stress, and energy in a way that helps them find time to care for themselves and boosts their mental health. We also recommend that medical educators act as role models to their students and discuss these issues openly, sharing their personal stories of mental illness and how they sought help and recovered. We recommend including activities like empowerment and life skills workshops within the curriculum, which can indirectly help to prevent and treat mental illness among students.
Conclusion and Limitations
Based on the data we collected in this study, we conclude that the medical curriculum is not the sole cause of mental health problems among medical students; rather, a combination of several factors and structures is responsible. The heavy academic demands on students interact with sociodemographic factors and with social attitudes and stigma towards mental illness. Such stigma prevents them from seeking help and leads to a deterioration that could be prevented with earlier intervention. Although this study provides evidence for the association of several factors with stigma, it is important to consider further factors that could contribute to students’ hesitancy to seek help. Among these factors are level of religiosity, self-esteem, family support, and reasons for choosing to pursue medicine. This study invites deeper analysis and further qualitative investigation to better explain its findings. In addition, it should be noted that the COVID-19 pandemic, which began a few months after our survey was conducted, has caused significant impact on medical students’ mental health. It is important to examine this impact, and any decrease in MHS and subsequent changes in students’ help-seeking behaviors which may have resulted from the widespread mental health crisis which accompanied the pandemic.
The main limitation of this study was its inability to include medical students from the other college of medicine in Qatar due to bureaucratic obstacles. Of the two colleges of medicine in Qatar, the one in which this study was conducted is larger and more diverse. However, future studies that include both medical schools in Qatar may be able to determine whether the type of curriculum influences students’ mental health in the same context.
Acknowledgments
The authors would like to thank Dr. Tawanda Chivese, College of Medicine, Qatar University, for his support and consultation on the data analysis. The authors would like also to thank the College of Medicine, Qatar University, for funding part of the publication fees of this study.
Disclosure
The authors declare no conflicts of interest in relation to this work.
References
1. Schwenk TL, Davis L, Wimsatt LA. Depression, stigma, and suicidal ideation in medical students. J Am Med Assoc. 2010;304(11):1181–1190. doi:10.1001/jama.2010.1300
2. Onyishi M, Talukdar D, Sanchez R. Prevalence of clinical depression among medical students and medical professionals: a systematic review study. Arch Med. 2016;8:6. doi:10.21767/1989-5216.1000178
3. Quek TTC, Tam WWS, Tran BX, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. 2019;16(15):2735–2752. doi:10.3390/ijerph16152735
4. Maser B, Danilewitz M, Guérin E, Findlay L, Frank E. Medical student psychological distress and mental illness relative to the general population: a Canadian cross-sectional survey. Acad Med. 2019;94(11):1781–1791. doi:10.1097/ACM.0000000000002958
5. Gaspersz R, Frings-Dresen MH, Sluiter JK. Prevalence of common mental disorders among Dutch medical students and related use and need of mental health care: a cross-sectional study. Int J Adolesc Med Health. 2012;24(2):169–172. doi:10.1515/ijamh.2012.025
6. Pacheco JP, Giacomin HT, Tam WW, et al. Mental health problems among medical students in Brazil: a systematic review and meta-analysis. Braz J Psychiatry. 2017;39(4):369–378. doi:10.1590/1516-4446-2017-2223
7. Kumar M, Sharma S, Gupta S, Vaish S, Misra R. Medical education effect of stress on academic performance in medical students—a cross sectional study. Indian J Physiol Pharmacol. 2014;58(1):81–86.
8. Meeks LM, Murray JF. Mental health and medical education. In: Zappetti D, Avery JD, editors. Medical Student Well-Being: An Essential Guide. Cham, Switzerland: Springer; 2019:17–58. doi:10.1007/978-3-030-16558-1
9. Abdulghani HM, AlKanhal AA, Mahmoud ES, Ponnamperuma GG, Alfaris EA. Stress and its effects on medical students: a cross-sectional study at a college of medicine in Saudi Arabia. J Health Popul Nutr. 2011;29(5):516–522. doi:10.3329/jhpn.v29i5.8906
10. Elzubeir MA, Elzubeir KE, Magzoub ME. Stress and coping strategies among Arab medical students: towards a research agenda. Educ Health. 2010;23(1):355–370.
11. Masri R, Kadhum M, Farrell SM, Khamees AA, Al-Taiar H, Molodynski A. Wellbeing and mental health amongst medical students in Jordan: a descriptive study. Int Rev Psychiatry. 2019;31(7–8):619–625. doi:10.1080/09540261.2019.1670402
12. Al-Alawi M, Al-Sinawi H, Al-Qubtan A, et al. Prevalence and determinants of burnout syndrome and depression among medical students at Sultan Qaboos University: a cross-sectional analytical study from Oman. Arch Environ Occup Health. 2019;74(3):130–139. doi:10.1515/IJAMH.2012.025
13. Hankir AK, Northall A, Zaman R. Stigma and mental health challenges in medical students. BMJ Case Rep. 2014;2014:bcr2014205226–bcr2014205226. doi:10.1136/bcr-2014-205226
14. Goffman E. Stigma. London: Penguin Books; 1963.
15. Stigma and Discrimination. Geneva: World Health Organization; 2014. Available from: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/mental-health/priority-areas/stigma-and-discrimination.
16. Sayers J. The world health report 2001 — mental health: new understanding, new hope. Bull World Health Organ. 2001;79(11):1085.
17. Schomerus G, Matschinger H, Angermeyer MC. The stigma of psychiatric treatment and help-seeking intentions for depression. Eur Arch Psychiatry Clin Neurosci. 2009;259(5):298–306. doi:10.1007/s00406-009-0870-y
18. Kopera M, Suszek H, Bonar E, et al. Evaluating explicit and implicit stigma of mental illness in mental health professionals and medical students. Community Ment Health J. 2015;51(5):628–634. doi:10.1007/s10597-014-9796-6
19. Maalouf FT, Alamiri B, Atweh S, et al. Mental health research in the Arab region: challenges and call for action. Lancet Psychiatry. 2019;6(11):961–966. doi:10.1016/S2215-0366(19
20. Dardas LA, Simmons LA. The stigma of mental illness in Arab families: a concept analysis. J Psychiatr Ment Health Nurs. 2015;22(9):668–679. doi:10.1111/jpm.12237
21. Ghuloum S, Bener A, Abou-Saleh MT. Prevalence of mental disorders in adult population attending primary health care setting in Qatari population. J Pak Med Assoc. 2011;61(3):216–221. doi:10.1016/j.jomh.2010.09.044
22. Kowal P, Chatterji S, Naidoo N, et al. Data resource profile: the World Health Organization Study on global AGEing and adult health (SAGE). Int J Epidemiol. 2012;41(6):1639–1649. doi:10.1093/ije/dys210
23. Shehata WM, Abdeldaim DE. Stigma towards mental illness among Tanta university students, Egypt. Commun Ment Health J. 2020;56(3):464–470. doi:10.1007/s10597-019-00502-9
24. Khaled SM, Amro I, Bader L, et al. Factors associated with depression and anxiety in the adult population of Qatar after the first COVID-19 wave: a cross-sectional study. Discov Psychol. 2021;1. doi:10.21203/rs.3.rs-729213/v2
25. Kronfol Z, Khalifa B, Khoury B, et al. Selected psychiatric problems among college students in two Arab countries: comparison with the USA. BMC Psychiatry. 2018;18(1):1–9. doi:10.1186/s12888-018-1718-7
26. Patient Health Questionnaire (PHQ-9 & PHQ-2)—construct: depressive symptoms. Washington, DC: American Psychological Association; 2020. Available from: https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/patient-health.
27. Sun Y, Fu Z, Bo Q, Mao Z, Ma X, Wang C. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry. 2020;20(1):474. doi:10.1186/s12888-020-02885-6
28. Dhira TA, Rahman MA, Sarker AR, Mehareen J. Validity and reliability of the Generalized Anxiety Disorder-7 (GAD-7) among university students of Bangladesh. PLoS One. 2021;16(12). doi:10.1371/journal.pone.0261590
29. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
30. Khaled SM. Prevalence and potential determinants of subthreshold and major depression in the general population of Qatar. J Affect Disord. 2019;252:382–393. doi:10.1016/j.jad.2019.04.056
31. Saller FV, Khaled SM. Potential psychosocial influences on gender differences in physical activity among Qatari adolescents: a first insight through descriptive observation. Int J Adolesc Youth. 2019;24(2):234–251. doi:10.1080/02673843.2018.1515087
32. Khaled SM, Wilkins SS, Woodruff P. Lifetime prevalence and potential determinants of psychotic experiences in the general population of Qatar. Psychol Med. 2020;50(7):1110–1120. doi:10.1017/S0033291719000977
33. Ghuloum S, Bener A, Dafeeah EE, Al-Yazidi T, Mustapha A, Zakareia A. Lifetime prevalence of common mental disorders in Qatar using WHO composite international diagnostic interview (WHO-CIDI). Int J Clin Psychiatry Ment Health. 2014;2(1):38–46. doi:10.5339/qfarc.2014.HBOP0878
34. Your mind matters: a resource to support good mental health and wellbeing for the people of Qatar. Doha: Ministry of Public Health; 2018. Available from: https://sehanafsia.moph.gov.qa/English/Pages/default.aspx.
35. Sharkey T. Mental health strategy and impact evaluation in Qatar. BJPsych Int. 2017;14(1):18–21. doi:10.1192/s2056474000001628
36. Puthran R, Zhang MWB, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50(4):456–468. doi:10.1111/medu.12962
37. Moir F, Yielder J, Sanson J, Chen Y. Depression in medical students: current insights. Adv Med Educ Pract. 2016;9:323–333. doi:10.2147/AMEP.S137384
38. Iqbal S, Gupta S, Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J Med Res. 2015;141(3):354–357. doi:10.4103/0971-5916.156571
39. Park AL, Fuhrer R, Quesnel-Vallée A. Parents’ education and the risk of major depression in early adulthood. Soc Psychiatry Psychiatr Epidemiol. 2013;48(11):1829–1839. doi:10.1007/s00127-013-0697-8
40. Ibrahim N, Dania AK, Lamis EK, Ahd AH, Asali D. Prevalence and predictors of anxiety and depression among female medical students in King Abdulaziz University, Jeddah, Saudi Arabia. Iran J Public Health. 2013;42(7):726.
41. Overton SL, Medina SL. The stigma of mental illness. J Couns Dev. 2008;86(2):143–151. doi:10.1002/j.1556-6678.2008.tb00491.x
42. Marwood MR, Hearn JH. Evaluating mental health literacy in medical students in the United Kingdom. J Ment Health Train Educ Pract. 2019;14(5):339–347. doi:10.1108/JMHTEP-01-2019-0001
43. Cuttilan AN, Sayampanathan AA, Ho RCM, Gotti V. Mental health issues amongst medical students in Asia: a systematic review [2000–2015]. Ann Transl Med. 2016;4:4. doi:10.3978/j.issn.2305-5839.2016.02.07
44. Zolezzi M, Elshami S, Obaidi W. An exploratory analysis of the portrayal of mental illness in Qatar’s newspapers. Psychol Res Behav Manag. 2020;13:1323–1332. doi:10.2147/PRBM.S280360
45. Zolezzi M, Alamri M, Shaar S, Rainkie D. Stigma associated with mental illness and its treatment in the Arab culture: a systematic review. Int J Soc Psychiatry. 2018;64(6):597–609. doi:10.1177/0020764018789200
46. Schulte-Körne G. Mental health problems in a school setting in children and adolescents. Deutsches Ärzteblatt Int. 2016;113(11):183–190. doi:10.3238/arztebl.2016.0183
47. Vankar JR, Prabhakaran A, Sharma H. Depression and stigma in medical students at a private medical college. Indian J Psychol Med. 2014;36(3):246–254. doi:10.4103/0253-7176.135372
48. Karnieli-Miller O, Perlick DA, Nelson A, Mattias K, Corrigan P, Roe D. Family members of persons living with a serious mental illness: experiences and efforts to cope with stigma. J Ment Health. 2013;22(3):254–262. doi:10.3109/09638237.2013.779368
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
