Back to Journals » Nature and Science of Sleep » Volume 13
Prevalence and Characteristics of Posttraumatic Nightmares in War- and Conflict-Affected Students
Authors Schultz JH, Forsberg JT, Harb G, Alisic E
Received 21 September 2020
Accepted for publication 3 February 2021
Published 19 March 2021 Volume 2021:13 Pages 423—433
DOI https://doi.org/10.2147/NSS.S282967
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Jon-Håkon Schultz,1 June Thorvaldsen Forsberg,1 Gerlinde Harb,1,2 Eva Alisic3
1Department of Education, UiT, The Arctic University of Norway, Tromsø, Norway; 2Philadelphia VA Medical Center, Philadelphia, PA, USA; 3University of Melbourne, Melbourne, Australia
Correspondence: Jon-Håkon Schultz
Department of Education, UiT, The Arctic University of Norway, PO Box 6050 Langnes, Tromsø, 9037, Norway
Email [email protected]
Introduction: Recurrent nightmares, frequently associated with traumatic experiences, may impair quality of life and daily functioning. However, there have been few studies of posttraumatic nightmares occurring among children and youth, in particular for trauma-exposed populations in conflict zones.
Methods: Using two quantitative data sets, this study investigates the prevalence and characteristics of recurrent nightmares among conflict-exposed young people in the Gaza Strip (N = 300) and examines the characteristics of posttraumatic nightmares and their association with academic functioning among treatment-seeking students in Gaza (N = 1093).
Results: Among 300 students (10– 12 years old) who lived in the ongoing conflict area in Gaza, nightmares were often mentioned, with 56% reporting recurrent nightmares with an average weekly frequency of 4.20 nights in the past week (SD = 1.94) and a mean duration of 2.48 years (SD = 2.01). Similarly, the large sample of 1093 students (6– 17 years of age) who sought help for nightmares and sleep disturbance reported recurrent traumatic nightmares on average 4.57 nights per week, with an average duration of 2.82 years. Their self-reported academic functioning was negatively affected by whether they experienced nightmares but was not associated with nightmare frequency or intensity.
Discussion: Given the high prevalence of nightmares and the relation between nightmares and academic functioning, students in conflict-affected areas appear to be a particularly vulnerable group. This study proposes screening and treating conflict-affected students for recurrent posttraumatic nightmares.
Keywords: stress, trauma, PTSD, posttraumatic nightmares, nightmares, sleep, academic functioning
Introduction
The International Classification of Sleep Disorders (ICSD-3),1 defines nightmares as “repeated occurrences of extended, extremely dysphoric, and well-remembered dreams that usually involve threats to survival, security, or physical integrity”.1 Recurrent nightmares are experienced as emotionally distressing upon waking; further, they significantly impair sleep quality and daytime functioning, cause sleep avoidance, daytime sleepiness and fatigue, and affect comorbid psychiatric symptoms.2 Nightmares can be classified as either idiopathic (unaccompanied by clinical signs of psychopathology) or associated with mental health problems such as posttraumatic stress (including PTSD), substance abuse, stress and anxiety or other psychiatric illnesses such as schizophrenia-spectrum disorders.2
While prevalence estimates tend to vary in the research literature due to differing measures and definitions of nightmares,3 about 4% of the general adult population are affected by (idiopathic) nightmare disorders.1 Nightmares are experienced more commonly among young children,4 increasing in frequency up to the age of six and decreasing after the age of 10. During the peak period, 55% of children experience nightmares or night terrors, with 6% once a week or more frequently.5,6 While fluctuation in the prevalence and frequency of childhood nightmares is thought to reflect natural development, research also notes stress as a moderator of nightmares.7 Nightmares are classified as one of the recurring symptoms of Posttraumatic Stress Disorder (PTSD);8 approximately 80% of adults with PTSD report nightmares.9 A high prevalence of nightmares have been found among military personnel with sleep disturbances,10 and people with war experience report more nightmares than the general population.11 Posttraumatic nightmares have shown to be persistent and long-lasting. In a non-conflict population, manifestations of sleep disturbances were documented 16 years post-trauma among children who experienced avalanches12 and lasting for more than 40 years for war veterans.13
Recurrent posttraumatic nightmares among children and adolescents have received less research attention, but an increased incidence of sleep dysfunction and nightmare disturbance has also been found in children and adolescents.7 However, there is considerable variation in these studies, with the prevalence of children’s nightmares following exposure to traumatic events ranging from 20% to 81%. Recent smaller studies of dreams in Palestinian youths have demonstrated signs of nightmare disturbance: adolescents reported five nightmares per week that had lasted for an average of three years;14 75% had dreams with an unpleasant atmosphere, 66.8% unhappy endings, with fear the most common emotion;15 and 38.1% of students (primary school), 28.8% (preparatory), 25.6% (secondary) and 13.6% (university level) reported “bad dreams” most nights.16
Young people in the Gaza Strip have experienced dramatically high exposure to potentially traumatic events and stressful conditions that could trigger sleep disturbance and nightmares. A study conducted in June 2006 documented that children and adolescents (N=197: 9–18 years) living in the border areas had been exposed to a mean number of eight traumatic events during the previous six months.17 In the last 12 years, the people of Gaza were exposed to three major wars: in 2008–2009, 2012, and 2014. In addition, between the end of the military operation in January 2009 and November 2012, the United Nations Office for the Coordination of Humanitarian Affairs18 recorded an average of ten limited armed escalations per year in the Gaza Strip, each lasting on average 2.5 days. A study of the 2014 war showed that 99.1% of the students studied (N=572: 12–18 years of age) had experienced at least one war-related traumatic event.19 Examples of exposure included witnessing or hearing shelling by tanks, artillery, or military planes (89.3%); witnessing neighbors’ houses being destroyed (69.2%); and witnessing injury or killing (66.4%). One month after the war, 57.5% of these students met the PTSD criteria. Further, students reported moderate to severe: somatic symptoms (45.8%), cognitive symptoms (75.5%), emotional symptoms (72.1%) and academic dysfunction (52%).
Given the high level of potential traumatic exposure, it is not surprising that studies have indicated that about two-thirds (64–67%) of children in Gaza exhibit clinical levels of post-traumatic stress symptoms.20,21 A systematic review of research in Palestine22 found that the prevalence of PTSD in children and adolescents varied between 23% and 70%; further, the prevalence of conflict-related traumatic experiences correlated positively with the prevalence of mental, behavioral, and emotional problems. In addition to considerable psychosocial distress, students’ ability to learn has been found to be heavily affected, involving nervousness, sadness, and fear of another attack.16
Previous studies have documented how youth in general and specifically in Gaza are affected by trauma exposure. However, there is a gap in the literature focusing on traumatic nightmares of students in conflict-affected populations and how sleep disturbance may affect their academic functioning, and more broadly their school functioning. The description of the phenomenology of post-trauma symptomatology is seen as the initial step in designing and informing effective interventions.
The current project aimed to estimate the general prevalence of posttraumatic nightmares (the Prevalence sample), as well as to document the characteristics of posttraumatic nightmares among a large sample of students in Gaza who sought help for nightmares and sleep disturbance (the Posttraumatic Nightmare sample). Over a five-year period, we collected pre-treatment data for students screened for participation in the Better Learning Program (BLP), an intervention for students with persistent posttraumatic nightmares.23 In this article, we discuss the characteristics of nightmares (frequency, intensity, duration) as well as the relationship between nightmare symptoms and academic functioning. Our research questions were formulated as follows:
For the Prevalence sample:
- What is the prevalence and characteristics of nightmares among students in Gaza aged 10–12?
- Is there a difference in self-reported academic functioning among students who experience nightmares and those who do not?
For the Treatment-seeking sample:
- Is there a difference in posttraumatic nightmare frequency, intensity, and duration according to the demographic variables of gender and age?
- Is there a difference in self-reported academic functioning among students related to the frequency, intensity, or duration of posttraumatic nightmares?
Method
Participants
Two samples of children and young adolescents in Gaza were recruited for the study reported here and made up the Prevalence sample and the Posttraumatic Nightmare sample. In 2018, 300 children in Gaza (161 girls, 139 boys, ages 10–14) were included in the nightmare prevalence study (Prevalence sample). They were recruited from three schools chosen as a purposive sample of schools in different geographical areas of the Gaza Strip; these schools were all on the waiting list for implementation of the BLP nightmare intervention. The original Prevalence sample consisted of 300 students between the ages of 10 and 14. However, as there were only five students over the age of 12, we decided to exclude them from the analysis, to achieve a more homogeneous sample; thus, we focused on the nightmare prevalence of 10–12-year-olds. The final sample consisted of 134 boys and 161 girls, with a mean age of 11.46 years.
Children seeking help for nightmares and sleep disturbance in Gazan schools constituted the second (Posttraumatic Nightmare) sample. A total of 1093 children and teenagers (594 girls and 504 boys; age range 6–17: 179 between 6 and 9, 673 between 10 and 12, and 241 between 13 and 17 years old; mean age 11.07) participated in five different cohort studies of the BLP between 2012 and 2016 and were included in the analyses of nightmare characteristics and academic functioning. During this period, all students found eligible for the intervention were included in these studies (see inclusion criteria below). Participants were recruited from more than 100 schools geographically spread across the entire area of the Gaza Strip.
Procedure
Prevalence Sample
In the prevalence study, all students who were present at school on the day of the study were invited to fill out a self-administered 13-item questionnaire. Nightmares were explained as follows: “A nightmare is a scary dream that you wake up from during the night – and when you wake up you feel very scared.” It was not specified or required that there be a linkage between nightmare and trauma exposure. Group-based assistance for completing the questionnaire was given by teachers and research staff.
Treatment-Seeking Sample
Starting in 2011 in Gaza, the Norwegian Refugee Council (NRC) together with the United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA) started implementing the Better Learning Program,23,24 a trauma-focused and school-based intervention for students with persistent posttraumatic nightmares. Inclusion criteria for the BLP program were as follows: a) having nightmares related to a traumatic event, the average frequency of two or more nights per week, b) the nightmares had persisted for three months or more, and c) they impaired school or daily functioning. The bachelor-level school counselors at each school led the screening interview after extensive training in the recruitment and screening procedures. These counselors gave classroom presentations, explaining what constitutes nightmares and normalizing post-trauma nightmare experiences, and invited students with persistent trauma-related nightmares to sign up for the intervention to reduce their nightmares.
Posttraumatic nightmares were defined and explained the same way as for the prevalence sample, with an additional emphasis on conflict-related trauma exposure. The Arabic word for nightmare, kaboos, is a well-defined concept, both semantically and culturally. In previous studies in Arabic populations, the concept of “nightmare” has been readily understood by children and youth.25 The counselors in our study reported that respondents of all ages had a clear concept of a nightmare. However, there was a need for occasional further explanations to the youngest children. Participants were interviewed by the counselor either individually or in small groups, using a structured interview to assess the frequency, intensity, duration, and content of nightmares, as well as school functioning and general well-being. For example, students were helped to establish a time reference for estimating nightmare duration while completing the questionnaire. To ensure a homogeneous sample for the study of conflict-related nightmares, respondents who mentioned domestic violence or sexual abuse as the sole source of their nightmares were excluded from this study and given alternative treatment.
Participation in research for both samples was voluntary. Enrollment in the intervention required parental written consent given after individual parent meetings with teachers and school counselors explaining the intervention. Whereas participation in the prevalence sample required passive agreement from parents after being informed in writing. Students in both samples gave their informed consent after receiving a detailed explanation of the aims of the study, anonymization and the possibility of withdrawing at any time. The Department of Education and UNRWA reviewed and approved the ethics and procedures of our study protocol. This study was conducted in accordance with the Declaration of Helsinki.
Academic achievement or performance was defined as level of achievement of students’ educational goals, whereas academic functioning usually refers more to the cognitive process of learning. School functioning describes the overall situation including wellbeing, academic functioning and achievement.
Measurement
Prevalence Sample
The presence of nightmares and their frequency was measured with two items: “I have nightmares” (Yes/No); and “In the last week, how many nights with nightmares did you have in total?” Nightmare duration was assessed on a 7-point scale: “How long have you experienced nightmares?” (0 = less than a year, 1=1 year ... to 6= more than 5 years). Nightmare intensity was measured with the 3-item Nightmare Intensity Scale developed for assessing the intensity of imagery, sensory details, and emotional experience in nightmares rated on a 6-point scale (0 = not at all, to 5 = very strong). The questionnaire measured current nightmares as opposed to the lifetime prevalence of “ever having had a nightmare”.
Further, respondents were asked to rate the adequacy of their academic functioning on an 11-point scale (0= not at all to 10= all the time): two items covered their self-assessed ability to concentrate in school and to perform to the best of their abilities.
Treatment-Seeking Sample
Posttraumatic nightmare frequency and the duration of the nightmare disturbance were measured as in the Prevalence sample. The intensity was measured with two items: “Do you see images from the nightmare during the daytime?” and “Can you usually get back to sleep after a nightmare?” Students were also asked whether their nightmares were linked to their worst experience, whether the nightmares reflected actual events that had happened to them, and whether the same nightmare recurred again and again. Self-rated academic functioning was assessed only in cohorts 3–5, with two items on an 11-point scale, as in the Prevalence sample. Trauma exposure was not formally assessed in the questionnaire, only during the screening interview. All questionnaires were translated from English to Arabic and then back-translated by certified translators.
Statistical Analysis
The statistical analyses were performed with SPSS 25.0 (IBM, SPSS, Chicago, IL). Prevalence was assessed by descriptive statistics. Differences in self-reported academic functioning and life satisfaction with and without nightmares were examined through a multivariate analysis of variance (MANOVA). Both theoretically important and significant effects were further investigated with contrast analysis; the least significant difference (LSD) adjustment was chosen for the multiple comparisons. A significant p-value of 0.05 indicated statistical significance.
Results
Prevalence Sample: Nightmare Prevalence
Over half of the students (56%, n=168) reported experiencing nightmares. There was no main effect of gender (F = 2.12, p = 0.15) or age (F = 1.22, p = 0.30) in whether or not students reported nightmares. Average nightmare frequency of those who reported nightmares was 4.2 nights in the past week (SD = 1.940). As shown in Figure 1, of the 56% (n=168) respondents who reported nightmares, 20.4% (n=34) reported low nightmare frequency (1–2 nights), 38.9% (n=65) reported medium frequency (3–4 nights), and 40.7% (n=68) reported high frequency (5–7 nights). There was no main effect of gender (F = 1.423, p = 0.24) or age (F = 0.49, p = 0.74) on nightmare frequency.
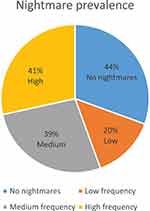 |
Figure 1 Nightmare prevalence. Notes: Low nightmare frequency = one or two nights; medium frequency = 3–4 nights; high frequency = 5–7 nights of nightmares pr. week. |
Mean duration of the occurrence of nightmares was approximately 2.48 years (SD = 2.01), with 39.2% reporting short (one year or less), 48.5% medium (2–4 years) and 20.4% long duration (5 years or more). There was no main effect of gender (F = 0.09, p = 0.76) or age (F = 1.07, p = 0.38) on nightmare duration. Further, there was no main effect of gender (F = 0.033, p = 0.86) or age (F = 1.93, p = 0.11) in nightmare intensity.
Prevalence Sample: Academic Functioning
There was a main effect of nightmares on academic functioning (F = 7.19, p = 0.01). Students who had experienced nightmares in the past week reported significantly lower academic functioning (mean = 7.74, SD = 0.16) than those who had not experienced nightmares (mean = 8.364, SD = 0.175 (t = 3.09, p = 0.002)). Gender (F = 32.01, p < 0.001) and age group (F = 4.23, p < 0.001) were significant covariates. Figure 2 shows academic functioning for those with and without nightmares.
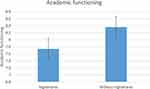 |
Figure 2 Academic functioning with and without nightmares. |
In contrast to the effect of the presence of nightmares, there was no main effect of nightmare frequency, duration, or intensity on academic functioning (F = 0.56, p = 0.58; F = 0.56, p = 0.57, and F= 1.35, p = 0.13, respectively).
Treatment-Seeking Sample: Nightmare Characteristics
Cohorts 1–5 assessed nightmare characteristics such as frequency, duration, and intensity. Table 1 presents the descriptive nightmare characteristics of the 1093 participants who reported experiencing recurrent posttraumatic nightmares.
 |
Table 1 Descriptive Statistics, All Participants in Cohorts 1–5 |
Students reported a mean frequency of 4.86 nights with nightmares per week (SD = 1.69). There was a main effect of age on nightmare frequency (F = 4.98, p = 0.007); the group of 6–9-year-olds reported higher frequency compared to the 13–17-year-olds (p = 0.005). There was no main effect of gender on nightmare frequency (F = 0.65, p = 0.42). Nightmare frequencies are shown in Figure 3.
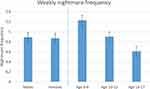 |
Figure 3 Nights with nightmares per week for males, females and the different age groups. |
The mean nightmare duration was 2.87 years (SD = 1.74). There was a main effect of gender on nightmare duration (F = 6.22, P = 0.013), with females reporting longer duration than males (p = 0.013). There was also a main effect of age on nightmare duration (F = 5.22, p = 0.006). The 10–12-year-olds reported a longer duration compared to the younger age group (p = 0.006). There were no other differences between the age groups (see Figure 4).
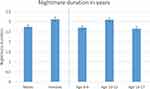 |
Figure 4 Nightmare duration in years for males, females and the different age groups. |
There was no main effect of gender on nightmare intensity (F = 0.78, p = 0.38) or age group (F = 0.40, p = 0.67).
Further, 60.6% of the total sample had nightmares about an actual event they had experienced; 63.7% reported that the content reflected their “worst experience.” More than half (54.2%) had mostly the same traumatic nightmare, and 64.9% had problems going back to sleep after nightmares. As many as 56.4% reported seeing “pictures of the nightmare” during the day—indicating intrusive re-experiencing of the traumatic nightmare content. In these characteristics, there were no significant gender differences (F = 0.099, p = 0.75) or age differences (F = 1.98, p = 0.04).
Treatment-Seeking Sample: Academic Functioning
Cohorts 3 to 5 (860 students: 412 males, 447 females; mean age of 11.26; SD = 1.78) assessed self-reported academic functioning.
There was a main effect of nightmare frequency on academic functioning (F = 5.15, p = 0.00), suggesting that when students experience nightmares, they also have reduced academic functioning. In this subsample, the average nightmare frequency was 4.88 (SD = 1.62), with no students reporting low frequency (1–2 nights with nightmares per week). Three or four nights with nightmares per week (medium frequency) were reported by 43.9% of students, and 56.1% reported five, six, or seven nights with nightmares per week (high frequency). All students that experienced nightmares had reduced academic functioning, but those who experienced high nightmare frequency reported significantly more reduced academic functioning (mean = 5.91, SD = 2.48) compared to those who reported medium frequency (mean = 6.55, SD = 2.30, F = 14.37, p = < 0.001). Academic functioning is illustrated in Figure 5.
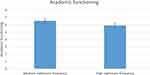 |
Figure 5 Academic functioning in the medium and high nightmare frequency group. |
There was no main effect of nightmare intensity on academic functioning (F = 1.61, p = 0.19). However, there was an interaction effect of nightmare intensity*frequency on academic functioning (F = 2.00, p = 0.015). This indicates that students reporting high frequency and high nightmare intensity experience further reduced academic functioning.
As to nightmare duration, 24.9% reported having experienced nightmares for one year or less (low duration); 57.0% reported two to four years (medium duration); and 18.1% reported having had nightmares for five years or more (long duration). However, there was no main effect of nightmare duration on academic functioning (F = 0.07, p = 0.93).
Discussion
Nightmare Characteristics and Academic Functioning
In the general population of students in Gaza aged 10–12 years, those who experienced recurrent nightmares reported significantly lower academic functioning than those without nightmares. On the whole, there was a recurrent nightmare prevalence of 56%, with an average weekly frequency of 4.2 nights with nightmares (SD = 1.94) with an average duration of 2.48 years (SD = 2.00). These findings are in line with earlier studies in Gaza indicating nightmare prevalence of approximately 55% (6–11 years), 52% (9–15 years), and one study reporting the prevalence of distressing dreams at 81% (12–16 years).17,26,27 The nightmare prevalence reported here is considerably higher than that among a non-conflict population of children and adolescents: it is estimated that nightmares occur in 10–20% of the general youth population,7 and recurrent weekly nightmares among only 6%.5,6
We found similarities in nightmare frequency and duration between the two samples of young people studied in this investigation—a general sample of students in Gaza, and a sample of treatment-seeking students. Treatment-seeking students reported an average weekly posttraumatic nightmare frequency of 4.86 nights (SD = 1.69) with an average duration of 2.87 years (SD = 1.74). It should be noted that only students with medium or high nightmare frequency were selected for the treatment-seeking sample; of those, 46% reported three or four nights and 43.9% reported six or seven nights with posttraumatic nightmares. The highest frequency was found in those aged 6–9 years, the longest duration among those 10–12 years of age, but the intensity of nightmares did not differ among the age groups. However, we found significant differences in nightmare characteristics as regards gender and age: younger boys had a higher frequency of nightmares, whereas older girls reported lower frequency but higher intensity. Females in the treatment-seeking sample reported longer nightmare duration than males, but there was no gender difference in nightmare frequency or intensity in either of the samples. This is somewhat in contrast to a large general population nightmare prevalence study11 where women reported significantly more frequent nightmares than men. Higher frequency in the younger age groups is consistent with the literature and the developmental theory of nightmares being linked to the development and consolidation of rapid eye movement (REM) sleep, particularly up to 10 years of age. REM sleep time increases until adolescence and then decreases with aging (see e.g.7,28). In this age group, the general frequency of nightmares is higher, so nightmares are expected; this probably affected our findings on nightmare prevalence.
Significantly, in both samples in our study, there was a main effect of nightmares on academic functioning. In the prevalence sample, those who had experienced nightmares in the past week reported significantly lower academic functioning than those who had not experienced nightmares. However, in this sample, there was no main effect of nightmare frequency, duration, or intensity on academic functioning. Thus, it appears that the presence, or occurrence, of nightmares impairs self-reported academic functioning rather than how frequent or distressing they are. This suggests that the presence of recurrent nightmares may be an indicator of posttraumatic difficulties in children similar to what has been suggested in adult survivors of trauma, where sleep disturbance is seen as a hallmark of post-trauma symptoms.29,30
In the sample of treatment-seeking students, all students reported nightmares and reduced academic functioning. In addition, there was an interaction effect of intensity and frequency on academic functioning. These findings indicate that students who report high nightmare frequency and high nightmare intensity are experiencing a further reduction in academic functioning—that is, among those students who are willing to disclose nightmares and to seek treatment. However, this unclear pattern between the two samples regarding the effect of frequency and intensity on academic functioning might be a result of the limited range in nightmare frequency and intensity in the prevalence sample (N=300), and/or the slight difference in measurement procedures.
Multiple Traumas and Ongoing Stress
Our investigation of the duration of nightmares in various cohorts starting from 2012 to 2016 shows that posttraumatic nightmares seem to be evenly distributed throughout this time period, indicating that nightmares are not necessarily caused solely by the wars immediately preceding our cohort assessments. The three wars experienced by the majority of our study participants involved extreme traumatic exposure. However, in the ongoing conflict there appear to be additional traumatic events that may cause nightmares in-between the actual wars, as is likely during the military occupation and ongoing military incursions.
Experience of multiple traumas is frequent in war and ongoing conflict, resulting in severe challenges for the development, mental health and academic functioning of young people. Chronic exposure to stress hormones has an impact on brain structures involved in cognition and mental health31 and influences health and well-being throughout the lifespan.32 A systematic review of 83 studies found that students with cumulative or severe exposure to traumatic events were at significant risk for impairments in cognitive functioning, academic difficulties, and social/emotional/behavioral problems.33
The relationship of sleep to learning and memory has long been recognized showing sleep to be an important component of memory reprocessing and how memories are formed and shaped.34,35 Studies examining sleep deprivation show a clear impact on cognition. Sleep deprivation during a week of sleep restricted to 4–5 hours per night increased fatigue, confusion, tension-anxiety, mood disturbance and decreased vigor.36 In one study,37 early adolescents (ages 10–13) appraised their main worry as significantly more threatening when sleep deprived, compared to when rested. Sleep-deprived adolescents show reduced positive affect such as being less interested, excited, happy, strong, energetic, cheerful, active, proud and delighted.37 There is growing evidence that sleep disturbance may be a marker for vulnerability to poor psychiatric outcomes in general, thus increasing the importance of identification of sleep difficulties and their treatment.38
While there is strong evidence in adults that sleep disturbances play a fundamental and complex role in PTSD (e.g.,)30, within pediatric PTSD, research on sleep disturbances has been more limited. However, the available literature suggests significantly more sleep problems and nightmares among children and adolescents exposed to trauma than in non-trauma-exposed samples.7 A recent study14 of 58 treatment-seeking students (12–16 years old) in Gaza found evidence of disturbed sleep as indicated by approximately five weekly posttraumatic nightmares for an average of 3.1 years, an average 50 minutes of nightly sleep latency, waking after sleep onset (several times a week to almost every night), and only once per week feeling rested in the morning. This suggests that recurrent posttraumatic nightmares are likely associated with reduced daily functioning which can lead to impaired academic development. As in adults, it appears that sleep disturbances may serve as a critical marker not only for current difficulties but also as an important signal for the development of pediatric PTSD, and may provide key therapeutic targets.7 Given that poor sleep quality is associated with increased stress and anxiety1,8 normalizing sleep patterns can most likely alleviate symptoms of PTSD and improve resilience to new stressors, in turn reducing stress and anxiety.7 All this speaks for better screening and treatment of recurrent posttraumatic nightmares for children living in conflict-affected and high-risk areas.
Strengths and Limitations of This Study
We have offered an estimate of nightmare prevalence among youth living in a situation of ongoing armed conflict. Further, the study design provides unique data on nightmare characteristics among 1093 treatment-seeking students in Gaza and how their self-reported academic functioning is affected. The large sample offers a broad picture that highlights prominent tendencies and patterns evident across age and gender and among cohorts over a five-year period. However, we acknowledge some limitations of this study. First, in the prevalence sample, we were not able to distinguish between trauma-related nightmares and other nightmares, which complicated interpretation, especially concerning age differences. Second, reliance on self-reporting may have inflated the relationships between measures of nightmare disturbance and functioning. In addition, in the treatment-seeking sample, nightmares were discussed individually when filling out the questionnaire; however, establishing nightmare duration is particularly challenging when nightmare experiences persist over several years. The measure of nightmare duration should therefore be used with caution. Third, the classroom-based self-reporting did not allow us to engage in individual explanations to distinguish between nightmares, anxiety dreams, and night terrors in cases when students might be in doubt. Fourth, students’ PTSD symptoms were not formally assessed, beyond identifying exposure to traumatic events and identifying a recurrent trauma-related nightmare and daily functioning was assessed only partly, by focusing on self-reported academic functioning. No standardized sleep measures were used, therefore it was not possible to determine how much of the decrements in academic functioning was caused by reductions in sleep quality/quantity versus the experience of recurrent nightmares alone. Finally, we used purposive sampling: this causes the risk of participants not being a representative sample for all the Gaza Strip.
Conclusions
This study documented the overrepresentation of nightmare experiences among 300 students aged 10 to 12 years in the ongoing conflict zone in Gaza, as evidenced by reports of recurrent nightmares by 56% of the study participants, with 4.2 nights with recurrent nightmares in the last week and a mean duration of approximately 2.5 years. Further, a large sample of 1093 treatment-seeking students aged 6 to17 showed recurrent traumatic nightmares with a weekly frequency of 4.57 nights with nightmares and an average duration of 2.82 years. Nightmares were significantly associated with reduced self-reported academic functioning: students reporting high nightmare duration and intensity experienced a more severe reduction in their academic functioning. Due to their long duration, the nightmare disturbances create substantial challenges for these students, in the learning process and their chances for successfully completing their education. School students experiencing ongoing conflict emerge as particularly vulnerable to recurrent posttraumatic nightmares due to the combination of traumatic stress and sleep deprivation affecting their academic functioning.
In addition, and in line with earlier research in the field of sleep disturbances and PTSD, the high incidence of recurrent posttraumatic nightmares documented in this study poses severe potential threats for the mental health, development and daily functioning of these young people. In view of this, we highlight the need for screening and treatment of students in conflict-affected areas for posttraumatic nightmares. Seeing recurrent posttraumatic nightmares as a key therapeutic marker for reduced mental health and reduced academic functioning, we would also recommend a precautionary measure: treating recurrent posttraumatic nightmares in students who have not yet reported reduced academic or daily functioning. Finally, screening and treatment should also include posttraumatic nightmares caused by other reasons than conflict and war, ie, domestic violence, assault and motor vehicle accidents.
Further Research
The findings in this study help to fill gaps in the research literature on the prevalence and characteristics of posttraumatic nightmares in trauma-affected populations of children and young people. Since the experience of recurrent nightmares affects sleep quality (e.g.,39) and PTSD can independently affect sleep continuity and quality (e.g.,40), future research should address in more detail whether reduced school performance is affected by general sleep disturbance independently of nightmares in addition to the effects of nightmare frequency. In view of the high numbers of students affected by posttraumatic nightmares in conflict areas, more research is needed on how to adapt available treatments from individual to group-based treatments made available through school to make these interventions more accessible to young populations. Further, more research is needed on how best to scale up treatment in the wake of war, crisis and in situations of protracted crisis.
Acknowledgments
Close collaboration with the UNRWA in Gaza was instrumental for reaching informants. This study was a collaborative venture between the UiT/Arctic University of Norway and the Norwegian Refugee Council (NRC).
Disclosure
The authors declare no conflicts of interest for this work.
References
1. American Academy of Sleep Medicine (AASM). International Classification of Sleep Disorders.
2. Aurora RN, Zak RS, Auerbach SH, et al. Best practice guide for the treatment of nightmare disorder in adults. J Clin Sleep Med. 2010;6(4):389–401. doi:10.5664/jcsm.27883
3. Zadra A, Donderi DC. Nightmares and bad dreams: their prevalence and relationship to well-being. J Abnorm Psychol. 2000;109(2):273–281. doi:10.1037//0021-843X.109.2.273
4. Mindell JA, Barrett KM. Nightmares and anxiety in elementary-aged children: is there a relationship? Child Care Health Dev. 2002;28:317–322. doi:10.1046/j.1365-2214.2002.00274.x
5. Fisher BE, Wilson AE. Selected sleep disturbances in school children reported by parents: prevalence, interrelationships, behavioral correlates and parental attributions. Percept Mot Skills. 1987;64(3, suppl.):1147–1157. doi:10.2466/pms.1987.64.3c.1147
6. Floress MT, Kuhn BR, Bernas RS, Dandurand M. Nightmare prevalence, distress, and anxiety among young children. Dreaming. 2016;26(4):280–292. doi:10.1037/drm0000034
7. Kovachy B, O’Hara R, Hawkins N, et al. Sleep disturbance in pediatric PTSD: current findings and future directions. J Clin Sleep Med. 2013;9:501–510. doi:10.5664/jcsm.2678
8. American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington, DC; 2013.
9. Kilpatrick D, Resnick H, Freedy J, et al. Posttraumatic stress disorder field trial: evaluation of PTSD construct criteria A through E. In: Widiger T, Frances A, Pincus H, et al., editors. DSM-IV Sourcebook. Vol. 4. Washington, D.C.: American Psychiatric Press; 1994.
10. Creamer JL, Brock MS, Matsangas P, Motamedi V, Mysliwiec V. Nightmares in United States military personnel with sleep disturbances. J Clin Sleep Med. 2018;14(3):419–426. doi:10.5664/jcsm.6990
11. Sandman N, Valli K, Kronholm E, et al. Nightmares: prevalence among the Finnish general adult population and war veterans during 1972–2007. Sleep. 2013;36(7):1041–1050. doi:10.5665/sleep.2806
12. Thordardottir EB, Hansdottir I, Valdimarsdottir UA, Shipherd JC, Resnick H, Gudmundsdottir B. The manifestations of sleep disturbances 16 years post-trauma. Sleep. 2016;39(8):1551–1554. doi:10.5665/sleep.6018
13. Schreuder BJN, Kleijn WC, Rooijmans HGM. Nocturnal re-experiencing more than forty years after war trauma. J Trauma Stress. 2000;13:453–463. doi:10.1023/A:1007733324351
14. Harb GC, Schultz J-H. Posttraumatic nightmares and school functioning in war-affected youth. PLoS One. 2020;15(11):e0242414. doi:10.1371/journal.pone.0242414
15. Qouta SR, Peltonen K, Diab SY, Anttila S, Palosaari E, Punamäki R-L. Psychosocial intervention and dreaming among war-affected Palestinian children. Dreaming. 2016;26(2):95–118. doi:10.1037/drm0000025
16. Kostelny K, Wessells M. Psychosocial assessment of education in Gaza and recommendations for response. United Nations Educational Scientific and Cultural Organization (UN-UNESCO); 2010.
17. Thabet AA, Abu Tawahina A, El Sarraj E, Vostanis P. Exposure to war trauma and PTSD among parents and children in the Gaza Strip. Eur Child Adolesc Psychiatry. 2008;17(4):191–199. doi:10.1007/s00787-007-0653-9
18. UN-OCHA. Fragmented lives: humanitarian overview. Jerusalem: United Nations Office for the Coordination of Humanitarian Affairs (UN-OCHA); 2013. Available from: https://www.ochaopt.org/sites/default/files/ocha_opt_fragmented_lives_annual_report_2013_english_web.pdf.
19. El-Khodary B, Samara M. Effectiveness of a school-based intervention on the students’ mental health after exposure to war-related trauma. Front Psychiatry. 2020;1031(10):1–10. doi:10.3389/fpsyt.2019.01031
20. Qouta SR, Palosaari E, Diab M, Punamäki R-L. Intervention effectiveness among war-affected children: a cluster randomized controlled trial on improving mental health. J Trauma Stress. 2012;25(3):288–298. doi:10.1002/jts.21707
21. Thabet AA, Abu Tawahina A, El Sarraj E, Vostanis P. Death anxiety, PTSD, trauma, grief, and mental health of Palestinian victims of war on Gaza. Health Care Current Rev. 2013;1:112–2016. doi:10.4172/hccr.1000112
22. Dimitry L. A systematic review on the mental health of children and adolescents in areas of armed conflict in the Middle East. Child Care Health Dev. 2011;38(2):153–161. doi:10.1111/j.1365-2214.2011.01246.x
23. Schultz JH, Raundalen M, Dalset M, Norheim HS, Støen JA. Fighting Nightmares and Sleeping Problems. Better Learning Program. Norway: University of Tromsø; 2013.
24. Schultz JH, Marshall L, Norheim H, Al-Shanti K. School-based intervention in ongoing crisis: lessons from a psychosocial and trauma-focused approach in Gaza schools. J Educ Emergencies. 2016;2(1):142–156. ISSN 2518-6833.
25. Abdel-Khalek AM. Reported nightmares and trait anxiety among Arab children, adolescents and adults. J Sleep Disord Ther. 2016;5:4. doi:10.4172/2167-0277.1000248
26. Thabet AA, Vostanis P. Post-traumatic stress disorder reactions in children of war: a longitudinal study. Child Abuse Negl. 2000;24:291–298. doi:10.1016/S0145-2134(99)00127-1
27. Thabet AA, Abed Y, Vostanis P, et al. Comorbidity of PTSD and depression among refugee children during war conflict. J Child Psychol Psychiatry. 2004;45(3):533–542. doi:10.1111/j.1469-7610.2004.00243.x
28. Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–1273. doi:10.1093/sleep/27.7.1255
29. Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. 1989;146(6):697–707. doi:10.1176/ajp.146.6.697
30. Germain A. Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry. 2013;170(4):372–382. doi:10.1176/appi.ajp.2012.12040432
31. Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10:434–445. doi:10.1038/nrn2639
32. Felitti JV, Anda FR, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi:10.1016/S0749-3797(98)00017-8
33. Perfect MM, Turley MR, Carlson JS, Yohanna J, Saint Gilles MP. School-related outcomes of traumatic event exposure and traumatic stress symptoms in students: a systematic review of research from 1990 to 2015. School Ment Health. 2016;8(1):7–43. doi:10.1007/s12310-016-9175-2
34. Stickgold R, Hobson JA, Fosse R, Fosse M. Sleep, learning, and dreams: off-line memory reprocessing. Science. 2001;294:1052–1057. doi:10.1126/science.1063530
35. Stickgold R. Sleep-dependent memory consolidation. Nature. 2005;437:1272–1278. doi:10.1038/nature04286
36. Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep. 1997;20:267.
37. Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010;10(6):831–841. doi:10.1037/a0020138
38. Pigeon WR, Bishop TM, Krueger KM. Insomnia as a precipitating factor in new onset mental illness: a systematic review of recent findings. Curr Psychiatry Rep. 2017;19–44. doi:10.1007/s11920-017-0802-x
39. Simor P, Horváth K, Gombos F, Takács KP, Bódizs R. Disturbed dreaming and sleep quality: altered sleep architecture in subjects with frequent nightmares. Eur Arch Psychiatry Clin Neurosci. 2012;262:687–696. doi:10.1007/s00406-012-0318-7
40. Harvey AG, Jones C, Schmidt DA. Sleep and posttraumatic stress disorder: a review. Clin Psychol Rev. 2003;23(3):377–407. doi:10.1016/S0272-7358(03)00032-1
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
