Back to Journals » Clinical Epidemiology » Volume 11
Pretreatment Hemoglobin Adds Prognostic Information To The NCCN-IPI In Patients With Diffuse Large B-Cell Lymphoma Treated With Anthracycline-Containing Chemotherapy
Authors Clausen MR , Maurer MJ , Ulrichsen SP , Larsen TS, Himmelstrup B , Rønnov-Jessen D, Link BK, Feldman AL , Slager SL, Nowakowski GS, Thompson CA, Pedersen PT, Madsen J, Pedersen RS, Gørløv JS, Cerhan JR , Nørgaard M , D'Amore F
Received 15 June 2019
Accepted for publication 25 September 2019
Published 14 November 2019 Volume 2019:11 Pages 987—996
DOI https://doi.org/10.2147/CLEP.S219595
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eyal Cohen
Michael R Clausen,1 Matthew J Maurer,2 Sinna Pilgaard Ulrichsen,3 Thomas S Larsen,4 Bodil Himmelstrup,5 Dorthe Rønnov-Jessen,6 Brian K Link,7 Andrew L Feldman,8 Susan L Slager,2 Grzegorz S Nowakowski,9 Carrie A Thompson,9 Per Trøllund Pedersen,10 Jakob Madsen,11 Robert S Pedersen,12 Jette Sønderskov Gørløv,13 James R Cerhan,2 Mette Nørgaard,1 Francesco D’Amore1
1Department of Hematology, Aarhus University Hospital, Aarhus, Denmark; 2Department of Health Sciences Research, Mayo Clinic, Rochester, MN, USA; 3Department of Clinical Epidemiology, Aarhus University Hospital, Aarhus, Denmark; 4Department of Hematology, Odense University Hospital, Odense, Denmark; 5Department of Hematology, Zealand University Hospital, Roskilde, Denmark; 6Department of Hematology, Sygehus Lillebaelt, Vejle, Denmark; 7Department of Internal Medicine, University of Iowa, Iowa City, IA, USA; 8Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN, USA; 9Department of Medicine, Mayo Clinic, Rochester, MN, USA; 10Department of Hematology, Sydvestjysk Sygehus, Esbjerg, Denmark; 11Department of Hematology, Aalborg University Hospital, Aalborg, Denmark; 12Department of Hematology, Hospitalsenheden Vest, Holstebro, Denmark; 13Department of Hematology, Rigshospitalet, Copenhagen, Denmark
Correspondence: Michael R Clausen
Department of Hematology, Aarhus University Hospital, Palle Juul-Jensens Blvd 35, Aarhus, Denmark
Email [email protected]
Background: Hemoglobin (Hgb) concentration at diagnosis is associated with outcome in cancer. In a recently reported simplified 3-factor prognostic score in Hodgkin lymphoma, Hgb, along with age and clinical stage, outperformed the classical International Prognostic Score with seven parameters.
Methods: In the present study, we investigated if pretherapeutic Hgb concentration added prognostic information to the NCCN-IPI in diffuse large B-cell lymphoma. We included patients from the Danish Lymphoma Registry (LYFO; N = 3499) and from the Molecular Epidemiology Resource (MER; N = 1225), Mayo Clinic and University of Iowa. Four sex-specific Hgb groups were defined: below transfusion threshold, from transfusion threshold to below lower limit of normal, from lower limit of normal to the population mean, and above the mean. We used multivariable Cox regression to estimate the hazard rate ratios (HR) and 95% CIs for overall survival (OS) and event-free survival (EFS), adjusting for sex, NCCN-IPI, comorbidity, and rituximab treatment.
Results: Approximately half of the patients had Hgb levels below the lower limit of normal. Compared to patients with Hgb levels above the mean, an inferior OS was directly correlated with lower pretreatment Hgb within the predefined groups (HR=1.23, HR=1.51, and HR=2.05, respectively). These findings were validated in the MER.
Conclusion: Based on multivariable analysis, lower pretreatment Hgb, even within the normal range but below the mean, added prognostic information to established indices such as the NCCN-IPI and the Charlson comorbidity index.
Keywords: diffuse large B-cell lymphoma, hemoglobin, prognosis, NCCN-IPI
Introduction
Diffuse large B-cell lymphoma (DLBCL) is the most frequent lymphoid malignancy among adults.1 It is primarily a disease of the elderly but it occurs in all age groups and extranodal involvement is present in up to a third of the cases.1,2 At the time of diagnosis, almost half of patients with DLBCL have a hemoglobin (Hgb) concentration fulfilling the definition of anemia.3–7 Anemia is associated with decreased life expectancy in many cancers.8 Pretreatment anemia is included as an adverse factor in prognostic indices for lymphoid malignancies other than DLBCL, e.g., the International Prognostic Score for advanced Hodgkin lymphoma (IPS) and the Follicular Lymphoma International Prognostic Index (FLIPI).9,10 Notably, the prognostic importance of anemia was not examined in the large international patient cohorts used to establish the International Prognostic Index (IPI) or the subsequent National Comprehensive Cancer Network International Prognostic Index (NCCN-IPI) developed to reflect the introduction of rituximab in the first-line treatment of DLBCL.11,12 Anemia has previously been associated with features of high-risk disease in DLBCL such as bone marrow infiltration and elevated lactate dehydrogenase (LDH).3,4 A possible prognostic relevance of Hgb levels in newly diagnosed patients with DLBCL may be clinically useful in order to improve risk-adapted management strategies. Therefore, we investigated the impact of pretreatment Hgb levels on the prognosis of newly diagnosed DLBCL patients treated with anthracycline-containing regimens and validated our findings in an independent cohort from the USA.
Methods
Data from two registries with prospective inclusion of DLBCL patients were used for this study. For discovery, we used the Danish Lymphoma Registry (LYFO).
Discovery Cohort - LYFO
This study was approved by the Danish Data Protection Agency (1-16-02-562-13) and the Danish Health and Medicines Authority (3-3013-1079/1/).
Patients registered in the LYFO with DLBCL between January 1, 2000, and December 31, 2012, were included if they were registered with a diagnosis of de novo DLBCL (patients had neither a past diagnosis of indolent lymphoma or composite/discordant lymphoma), did not have primary CNS-lymphoma, and had received anthracycline-containing chemotherapy with or without the addition of rituximab. The International Classification of Disease for Oncology, third edition histology codes (ICD-O-3) for DLBCL (9680), was used to identify all patients with DLBCL. The LYFO registry prospectively includes all patients with lymphoid malignancies referred to hematology departments in Denmark and has had nationwide coverage since 2000.13 Recently, LYFO was described to include 98% of all lymphomas in Denmark with a completeness of registered variables of 99% and positive predictive values for variables ranging from 88% to 99%.14 Treatment data are registered according to the type of chemo- and immunotherapy, date of start and end of treatment, and the number of treatment courses administered.14 In the present study, chemotherapy regimens included were: CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone), CHOEP (cyclophosphamide, doxorubicin, etoposide, vincristine, prednisone), and more intensive anthracycline-containing regimens. In order to maximize the completeness of treatment data, we combined the information contained in the LYFO registry with treatment information from the Danish National Patient Registry (DNPR). The DNPR is an administrative register that contains individual data on diagnoses, treatments, and time periods for each contact with the public health care system.15 Pathology reports of the primary as well as the relapse biopsies were retrieved from the Danish National Pathology Registry, which contains detailed descriptions of all pathology specimens analyzed in Denmark since 1997.16
Exposures
Values of pretreatment Hgb and LDH were collected from regional laboratory systems of the five administrative health regions of Denmark.17 For two regions, all laboratory measurements were retrieved from a common clinical laboratory information database. For the remaining three regions, laboratory data were obtained directly from the departments of clinical biochemistry of the treating centers. We categorized Hgb levels according to four sex-specific Hgb groups (in g/L for males, females) as below the transfusion threshold (<98, <98), from transfusion threshold to below lower limit of normal (98–133, 98–117), from lower limit of normal to the population mean (134–149, 118–134), and above the mean (>149, >134).18,19 If more than one value of Hgb was registered in the time frame between 14 days prior to the diagnostic biopsy and the date of treatment start, we used the lowest of these values. This was done in order to minimize the risk of misclassifying patients to a higher pretreatment Hgb subgroup due to blood transfusion.
Covariates
The NCCN-IPI categories were calculated as described in the original publication with a score of 0–1 for low, 2–3 low-intermediate, 4–5 high-intermediate, and ≥6 for high risk.12 A Charlson comorbidity index (CCI) was computed based on diagnoses recorded for the individual patient in the DNPR up to 10 years prior to the date of DLBCL diagnosis.20,21 We used the same 19 diagnoses as in the original CCI publication and defined three levels of comorbidity: CCI score 0 (no comorbidity), 1–2 (moderate), or >2 (severe).20 The use of DNPR data to estimate comorbidity has previously been validated for the time period covering this study.22
Data on vital status (dead/alive) were obtained by linking the LYFO registry to The Danish Civil Registration System, which contains daily updated vital status on all Danish citizens. This register operates through a unique 10-digit personal identification number and contains several demographic parameters thoroughly described in a previous report.23
Validation Cohort – MER
From the Molecular Epidemiology Resource (MER), we obtained data on DLBCL patients to validate our findings. This study was reviewed and approved by the human subject’s institutional review boards at the Mayo Clinic and the University of Iowa. Written informed consent was obtained from all participants. Briefly, consecutive patients with newly diagnosed lymphoma were prospectively enrolled from 2002 to 2015; for this analysis, we included DLBCL patients enrolled through 2013 who were treated with an anthracycline-based immunochemotherapy regimen.24,25 Patients with primary CNS lymphoma, posttransplant lymphoproliferative disorders, and primary mediastinal B-cell lymphoma were excluded. Baseline clinical, laboratory, and treatment data were abstracted from medical records by using a standard protocol. Disease progression/relapse, retreatment, and death were prospectively collected and validated by medical record review. Event-free survival (EFS) was defined as the time from the date of diagnosis (date from the first biopsy specimen containing lymphoma) to disease progression, retreatment, or death due to any cause. Cell of origin (COO) was determined from clinical results based on the Hans algorithm.26
Statistics
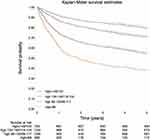
Patient baseline characteristics were presented as proportions for categorical variables and as a range with median and interquartile range (IQR) for continuous variables. Overall survival (OS) was calculated from the date of primary biopsy to the date of death or end of follow-up (February 18, 2016) and EFS was calculated from primary biopsy to the date of progression, death or last follow-up. We used Kaplan–Meier curves and Cox proportional hazard regression to assess the association of Hgb levels with OS and EFS.27,28 Cox models were adjusted for NCCN-IPI, rituximab treatment (LYFO only), sex, and level of comorbidity. We also conducted analyses stratified by sex, age, treatment, and NCCN-IPI (grouped as low and low-intermediate risk vs high-intermediate and high risk). The proportional hazard assumption was evaluated graphically with log minus log plots and was accepted. To evaluate for nonlinear associations of Hgb levels with OS, we used a restricted cubic spline with knots at the Hgb percentiles 5, 17.5, 50, 67.5, and 95 and stratified by sex.29 As a reference, we used the mean Hgb value for the Scandinavian background population reported by three previous studies.18,19,30 Only patients with available Hgb values were included in the discovery analysis. In a separate analysis, we used multiple imputation to account for missing values for Hgb or NCCN-IPI parameters. This was performed using chained equations under the assumption that data were missing at random.31
For validation in the MER, we used MER-specific Hgb cut-points and presented KM curves and Cox models, both unadjusted and adjusted for sex, NCCN-IPI and comorbidity (none vs any). All estimates were presented with 95% CI.
Statistical analyses were done using Stata14 (Stata Statistical Software: Release 14.2 College Station, TX: StataCorp LP). We used the STROBE and RECORD statements to guide our report of the study.32,33
Results
Discovery
Through the LYFO registry, we identified 4765 patients with DLBCL and 3499 fulfilled the inclusion criteria for the analysis. Figure S1 shows the algorithm leading to the study cohort. Baseline demographic characteristics are summarized in Table 1. The median age at diagnosis was 65 years (range 15–95; IQR 56–73) and the majority of the patients were men (56%). Regarding the NCCN-IPI, 424 patients (12.1%) had a low, 1382 (39.5%) a low-intermediate, 1216 (34.8%) a high-intermediate, and 422 (12.1%) a high-risk NCCN-IPI profile. The majority of patients received a combination of rituximab and CHOP/CHOP-like chemotherapy 2615 (75%).
 |
Table 1 Clinical Features And Treatment Background According To Pretreatment Hgb Subgroups (Discovery Cohort) |
At diagnosis, anemia was present in 1612 (46%) patients, with 1246 (36%) in the range from the transfusion threshold to the lower limit of normal and 366 (11%) below the transfusion threshold. Lower pretreatment Hgb levels were associated with older age, male sex, advanced clinical stage, extranodal disease, bone marrow infiltration, high LDH, PS ≥2, higher NCCN-IPI score, and higher CCI. Anemia was more frequent in men (Table 1, Figure S2A and B); although there was no difference in the frequency of bone marrow infiltration among sexes, neither overall (15% men vs 14% women) nor within the two anemia subsets, i.e., “below transfusion threshold” (31% men vs 28% women) and “between transfusion threshold and lower limit of normal” (19% men vs 20% women).
At a median follow-up time of 7.9 years (IQR 5.3 −10.8), 1820 events had occurred. Five-year OS was 79% (95% CI 76–82) for patients with Hgb above the mean, 71% (95% CI 68–73) for those with Hgb in the normal range but at or below the mean, 54% (95% CI 51–57) for patients with Hgb below the normal range to or at the transfusion threshold, and 37% (95% CI 32–42) for patients with Hgb below the transfusion threshold (Figure 1).
The calculated crude and adjusted hazard ratios (HR) are summarized in Table 2. Compared to patients with Hgb above the mean, the other three groups in decreasing order of Hgb levels had inferior OS (HR=1.23, 95% CI 1.01–1.49; HR=1.51, 95% CI 1.25–1.83; and HR=2.05 95% CI 1.65–2.56, respectively) after adjustment for sex, NCCN-IPI, rituximab treatment, and comorbidity. Similar results were observed for EFS (Table 2). In the model with imputed values, accounting for missing information for both exposure (n=32) and covariates (n=91), results compared well to the results obtained without imputation in both the crude and adjusted analysis (Table S1).
 |
Table 2 Crude And Adjusted HRs For OS According To Hgb For Both LYFO And MER |
To estimate the Hgb association for selected subgroups, we conducted analyses stratified on age, sex, and rituximab treatment (Table 3). Regarding age strata (≤60 vs >60 years), an association of lower Hgb concentrations with inferior OS was observed in both strata but was more prominent in patients above 60 years. Similarly, the association of lower Hgb levels and poorer OS was also observed when stratifying for sex. Interestingly, this association was stronger in men (Table 3). To analyze the influence on mortality of Hgb concentrations, considered as a continuous variable, we used cubic splines with knots at Hgb percentiles 5, 17.5, 50, 67.5, and 95 (Figure 2).
 |
Table 3 Five-Year OS And Adjusted HRs Stratified On Selected Factors In The Discovery Cohort |
This showed that there was an almost linear association of Hgb level and mortality below the 50th Hgb percentile for both men and women. Notably, the cubic spline analysis demonstrated that also a Hgb concentration in the lower end of the normal range was associated with increased mortality. In a further analysis, we stratified patients according to whether they received rituximab in their primary treatment. The association between Hgb levels and OS was present in both treatment groups but was stronger for rituximab-treated patients. This observation finally, when stratifying NCCN-IPI risk groups, the association of OS with Hgb level was evident for both strata (low/low-intermediate vs high-intermediate/high risk) (Figure 3).
To illustrate the ability of Hgb levels to add prognostic information to an established index such as the NCCN-IPI, a comparison can be drawn to the NCCN-IPI low-intermediate risk group. The 5-year OS reported for this group in the original NCCN-IPI publication was 82%. In our cohort, the corresponding value for the same risk group according to the four Hgb subsets (in decreasing order of Hgb concentration) was 83% (95 CI% 78–87), 79% (95 CI% 74–82), 68% (95 CI% 63–73), and 49% (95 CI% 34–62), respectively.
Patient Characteristics In The Validation Dataset
Patients in the validation cohort had a median age of 63 years (range 18–93 years: IQR 54–72), slightly younger than the LYFO. In the MER, men were also more likely to have lower Hgb at diagnosis and were otherwise comparable regarding comorbidity, NCCN-IPI, and other clinical baseline characteristics (Table S2). The NCCN-IPI risk group distribution was: 10.6% low, 39.3% low-intermediate, 40.8% intermediate-high, and 9.2% high. All patients in the validation cohort received immunochemotherapy with rituximab in combination with a CHOP/CHOP-like regimen. The same sex-related differences in anemia occurrence were also found in the validation cohort (Figure S3A and B). Similar findings for OS were obtained from the analysis of the validation cohort (Table 2), both overall (Figure S4) and stratified by NCCN-IPI (Figure S5), although the outcome of the lowest Hgb group was better than in the LYFO. Compared to patients with Hgb above the mean, the next two groups in decreasing order of Hgb levels had inferior OS (HR=1.43, 95% CI 1.03–1.97 and HR=1.53, 95% CI 1.14–2.05, respectively) after adjustment for sex, NCCN-IP,I and any comorbidities, while the risk estimate for the lowest Hgb levels was attenuated and not statistically significant (HR=1.27, 95% CI 0.86–1.86).
In the MER cohort, 70% of the cases had COO data available (Table S3). Patients with lower Hgb were more likely to have a non-GCB signature (50%), while the opposite was observed for patients with Hgb above mean (25%). Overall, 35% of the patients were classified as non-GCB.
Discussion
In this study of prospectively collected data, we found that lower Hgb concentration was associated with increased mortality both in the discovery cohort from LYFO and in the validation cohort from the US. Most provocatively, patients with Hgb below the mean but still within the normal range also had inferior OS compared to the reference group (normal values at or above the mean).
Strengths of this study include the population-based design through linkage of high-quality data from both regional and national registries, homogeneous treatments based on national recommendations, and a near-complete follow-up. Moreover, we were able to validate our findings in an independent cohort of community-based participants. As in all observational studies, some limitations have to be considered. We identified the patients using the LYFO register which captures virtually every patient diagnosed with lymphoma in Denmark. A validation analysis of this registry showed that the number of patients who escaped registration was very low (1.6%) and primarily consisted of low-grade lymphomas.14 With regard to the information on follow-up time and vital status, accuracy was secured on the basis of the daily updates performed by the Danish Civil Registration System.23 Thus, selection bias in our discovery study cohort is likely to be minor. In terms of potential misclassification of Hgb values, a Scandinavian quality control study on Hgb measurements from different Scandinavian laboratories, including those relevant to the present study, found that all values were within ±2% of the mean for all measurements.19 Regarding Hgb measurements in the MER, they were performed as part of routine evaluation of a new lymphoma. Furthermore, we were able to adjust for known prognostic factors included in well-established international prognostic indices and, in addition to LYFO, we also had access to data allowing us to adjust for comorbidity. A parameter, which could not be elucidated reliably in the LYFO, was the COO. In the MER, the Hans classifier was used to determine COO, and non-GCB patients overall had lower Hgb than those with GCB phenotype. Two studies have not found an association between Hgb and COO, which might be explained by lack of power to detect a difference.
In previous reports, anemia was found at variable frequencies (34%–77%) among patients with DLBCL.4–7,34 In contrast to these studies, where Hgb concentrations were dichotomized (anemic vs nonanemic), we examined Hgb concentrations across the range of values both within the normal range and at two levels of anemia (i.e., at or above and below transfusion threshold). Through this approach, we demonstrated a pattern of association between decreasing pretreatment Hgb concentrations and increased mortality in the study population. The underlying explanation for this association is not clear. The same applies to the observed sex-related differences, where anemia seemed to have a stronger adverse impact on men. The latter cannot be explained as being related to comorbidity since the prevalence of mild and severe comorbidity was similar for men and women. Other factors such as body mass index and menopausal status may play a role in this context. Age imbalances cannot explain this either, since men had a lower median age (64 vs 66 years). A higher impact of treatment-related toxicity and a possible hypoxia-induced lower treatment sensitivity, for example in cases with bulky disease, may also be considered as possible contributing factors. Although not previously described in lymphoma, the latter consideration is well recognized in solid tumors such as head-and-neck cancer.35 Furthermore, the additional prognostic information of hemoglobin concentration found in the present study may suggest the existence of a specific biology behind the not otherwise specified DLBCL-associated pretreatment anemia. For instance, extranodal disease was present in 17% vs 59% of patients in the highest vs lowest Hgb group, an observation not explained by bone marrow infiltration alone (6% vs 29%). The causality of this observation cannot be determined within the present study, but could for example be either: 1) extranodal lymphoma leads to anemia via inflammation or 2) the biology of a specific subgroup of DLBCL increases the likelihood of dissemination to extra-nodal sites and anemia merely represents an epiphenomenon, both manifestations could also be mediated by inflammation.36
In the light of an increasing number of experimental treatment options in both fit and frail DLBCL patients, the allocation to risk-adapted treatment strategies is necessary and it may be improved by the addition of an easily accessible and broadly available parameter such as Hgb.
Acknowledgements
The authors gratefully acknowledge help from the departments of clinical biochemistry at the University Hospitals of Aalborg, Odense, Copenhagen-Herlev, Copenhagen-Rigshospitalet, Vejle Hospital, and West Zealand Hospital. The authors also wish to thank the funders of this study: Karen Elise Jensen Foundation, the Program for Clinical Research Infrastructure in Denmark, the Aase & Ejnar Danielsen Foundation, the Eva and Henry Frænkel Memorial Foundation, the Danish Cancer Research Foundation, the Dagmar Marshall Foundation, and Takeda Denmark. The study was also supported by the MER: P50CA97274 grant from National Cancer Institute (NCI), USA, and grant U01CA195568 for The Lymphoma Epidemiology of Outcomes (LEO) Cohort Study. An abstract of this paper was presented at the 15th International Conference on Malignant Lymphoma 18–22 June 2019 as publication only. The abstract was published in Hematological Oncology 2019 vol: 37 pp: 418-420: https://onlinelibrary.wiley.com/doi/10.1002/hon.88_2631.
Author Contributions
All authors contributed toward data analysis, drafting and revising the paper, gave final approved version to be published and agree to be accountable for all aspects of the work.
Disclosure
MRC reports grants from Takeda Denmark, grants from Karen Elise Jensen Foundation, non-financial support from Program for Clinical Research Infrastructure in Denmark, grants from Aase & Ejnar Danielsen Foundation, grants from Eva and Henry Frænkel Memorial Foundation, grants from Danish Cancer Research Foundation, grants from Dagmar Marshall Foundation, during the conduct of the study and non-financial support from Roche, non-financial support from Gilead, outside the submitted work. MM reports being on the advisory board and a consultant of Morphosys, grants from Celgene and grants from Nanostring outside the submitted work. GSN reports grants and personal fees from Celgene, grants and personal fees from Morphosys, personal fees from Selvita, grants from Roche and grants from Nanostring during the conduct of the study. JRC reports grants from NIH during the conduct of the study, grants from NanoString and grants from Celgene outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Smith A, Crouch S, Lax S, et al. Lymphoma incidence, survival and prevalence 2004–2014: sub-type analyses from the UK’s Haematological Malignancy Research Network. Br J Cancer. 2015;112:1575–1584. doi:10.1038/bjc.2015.94
2. Engholm G, Ferlay J, Christensen N, et al. NORDCAN: cancer incidence, mortality, prevalence and survival in the nordic countries, Version 5.3. April 25, 2013. Available from: http://www.ancr.nu.
3. Moullet I, Salles G, Ketterer N, et al. Frequency and significance of anemia in non-Hodgkin’s lymphoma patients. Ann Oncol. 1998;9:1109–1115. doi:10.1023/a:1008498705032
4. Troppan KT, Melchardt T, Deutsch A, et al. The significance of pretreatment anemia in the era of R-IPI and NCCN-IPI prognostic risk assessment tools: a dual-center study in diffuse large B-cell lymphoma patients. Eur J Haematol. 2015;95:538–544. doi:10.3109/10428194.2013.802314
5. Adams HJA, de Klerk JMH, Fijnheer R, et al. Prognostic value of anemia and c-reactive protein levels in diffuse large B-cell lymphoma. Clin Lymphoma Myeloma Leuk. 2015;15:671–679. doi:10.1016/j.clml.2015.07.639
6. Tisi MC, Bozzoli V, Giachelia M, et al. Anemia in diffuse large B-cell non-Hodgkin lymphoma: the role of interleukin-6, hepcidin and erythropoietin. Leuk Lymphoma. 2014;55:270–275. doi:10.3109/10428194.2013.802314
7. Zinzani PL, Tani M, Alinari L, et al. Role of anemia in survival of patients with elderly aggressive non-Hodgkin’s lymphoma after chemotherapy. Leuk Lymphoma. 2005;46:1449–1454. doi:10.1080/10428190500178688
8. Caro JJ, Salas M, Ward A, Goss G. Anemia as an independent prognostic factor for survival in patients with cancer: a systemic, quantitative review. Cancer. 2001;91:2214–2221.
9. Ziepert M, Hasenclever D, Kuhnt E, et al. Standard international prognostic index remains a valid predictor of outcome for patients with aggressive CD20+ B-cell lymphoma in the rituximab era. J Clin Oncol. 2010;28:2373–2380. doi:10.1200/JCO.2009.26.2493
10. Solal-Céligny P, Roy P, Colombat P, et al. Follicular lymphoma international prognostic index. Blood. 2004;104:1258–1265. doi:10.1182/blood-2003-12-4434
11. Shipp MA. A predictive model for aggressive non-Hodgkin’s lymphoma. The International Non-Hodgkin’s lymphoma prognostic factors project. N Engl J Med. 1993;329:987–994. doi:10.1056/NEJM199309303291402
12. Zhou Z, Sehn LH, Rademaker AW, et al. An enhanced International Prognostic Index (NCCN-IPI) for patients with diffuse large B-cell lymphoma treated in the rituximab era. Blood. 2014;123:837–842. doi:10.1182/blood-2013-09-524108
13. Arboe B, Josefsson P, Jørgensen J, et al. Danish National Lymphoma Registry. Clin Epidemiol. 2016;8:577–581. doi:10.2147/CLEP.S99470
14. Arboe B, El-Galaly TC, Clausen MR, et al. The Danish national lymphoma registry: coverage and data quality. PLoS One. 2016;11:e0157999. doi:10.1371/journal.pone.0157999
15. Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449. doi:10.2147/CLEP
16. Bjerregaard B, Larsen OB. The Danish Pathology Register. Scand J Public Health. 2011;39:72–74. doi:10.1177/1403494810393563
17. Grann AF, Erichsen R, Nielsen AG, Frøslev T, Thomsen R. Existing data sources for clinical epidemiology: the clinical laboratory information system (LABKA) research database at Aarhus University, Denmark. Clin Epidemiol. 2011;3:133. doi:10.2147/CLEP.S17901
18. Kotze SR, Pedersen OB, Petersen MS, et al. Predictors of hemoglobin in Danish blood donors: results from the Danish Blood Donor Study. Transfusion. 2015;55:1303–1311. doi:10.1111/trf.13011
19. Nordin G, Mårtensson A, Swolin B, et al. A multicentre study of reference intervals for haemoglobin, basic blood cell counts and erythrocyte indices in the adult population of the Nordic countries. Scand J Clin Lab Invest. 2004;64:385–398. doi:10.1080/00365510410002797
20. Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. doi:10.1016/0021-9681(87)90171-8
21. Nørgaard M, Larsson H, Pedersen G, Schønheyder HC, Sørensen HT. Haematological malignancies - a predictor of a poor outcome in patients with bacteraemia. J Infect. 2006;53:190–198. doi:10.1016/j.jinf.2005.10.024
22. Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sørensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83. doi:10.1186/1471-2288-11-83
23. Pedersen CB. The Danish civil registration system. Scand J Public Health. 2011;39:22–25. doi:10.1177/1403494810387965
24. Maurer MJ, Ghesquières H, Jais J-P, et al. Event-free survival at 24 months is a robust end point for disease-related outcome in diffuse large B-cell lymphoma treated with immunochemotherapy. J Clin Oncol. 2014;32:1066–1073. doi:10.1200/JCO.2013.51.5866
25. Cerhan JR, Link BK, Habermann TM, et al. Cohort profile: the lymphoma specialized program of research excellence (SPORE) molecular epidemiology resource (MER) cohort study. Int J Epidemiol. 2017;46:1753–1754i. doi:10.1093/ije/dyx119
26. Hans CP, Weisenburger DD, Greiner TC, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275–282. doi:10.1182/blood-2003-05-1545
27. Cox D. Regression models and life tables. J R Stat Soc Ser B. 1972;34:187–220.
28. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi:10.1080/01621459.1958.10501452
29. Royston P, Altman DG, Sauerbrei W. Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med. 2006;25:127–141. doi:10.1002/sim.2331
30. Martinsson A, Andersson C, Andell P, Koul S, Engström G, Smith JG. Anemia in the general population: prevalence, clinical correlates and prognostic impact. Eur J Epidemiol. 2014;29:489–498. doi:10.1007/s10654-014-9929-9
31. Beesley LJ, Bartlett JW, Wolf GT, Taylor JMG. Multiple imputation of missing covariates for the Cox proportional hazards cure model. Stat Med. 2016;35:4701–4717. doi:10.1002/sim.7048
32. Benchimol EI, Smeeth L, Guttmann A, et al. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12:e1001885. doi:10.1371/journal.pmed.1001885
33. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi:10.7326/0003-4819-147-8-200710160-00010
34. Truong PT, Parhar T, Hart J, Alexander C, Wai ES. Population-based analysis of the frequency of anemia and its management before and during chemotherapy in patients with malignant lymphoma. Am J Clin Oncol. 2010;33:465–468. doi:10.1097/COC.0b013e3181b4b147
35. Prosnitz RG, Yao B, Farrell CL, Clough R, Brizel DM. Pretreatment anemia is correlated with the reduced effectiveness of radiation and concurrent chemotherapy in advanced head and neck cancer. Int J Radiat Oncol Biol Phys. 2005;61:1087–1095. doi:10.1016/j.ijrobp.2004.07.710
36. Gupta M, Han JJ, Stenson M, et al. Elevated serum IL-10 levels in diffuse large B-cell lymphoma: a mechanism of aberrant JAK2 activation. Blood. 2012;119:2844–2853. doi:10.1182/blood-2011-10-388538
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.