Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 9
Presurgical cleft lip and palate orthopedics: an overview
Authors Alzain I, Batwa W, Cash A, Murshid ZA
Received 6 December 2016
Accepted for publication 15 March 2017
Published 31 May 2017 Volume 2017:9 Pages 53—59
DOI https://doi.org/10.2147/CCIDE.S129598
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Christopher E. Okunseri

Ibtesam Alzain,1 Waeil Batwa,2 Alex Cash,3 Zuhair A Murshid2
1Pediatric Dentistry, 2Orthodontic Department, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia; 3Cleft Lip and Palate Orthodontics, Queen Victoria NHS Foundation Trust, South Thames Cleft Service, London, UK
Abstract: Patients with cleft lip and/or palate go through a lifelong journey of multidisciplinary care, starting from before birth and extending until adulthood. Presurgical orthopedic (PSO) treatment is one of the earliest stages of this care plan. In this paper we provide a review of the PSO treatment. This review should help general and specialist dentists to better understand the cleft patient care path and to be able to answer patient queries more efficiently. The objectives of this paper were to review the basic principles of PSO treatment, the various types of techniques used in this therapy, and the protocol followed, and to critically evaluate the advantages and disadvantages of some of these techniques. In conclusion, we believe that PSO treatment, specifically nasoalveolar molding, does help to approximate the segments of the cleft maxilla and does reduce the intersegment space in readiness for the surgical closure of cleft sites. However, what we remain unable to prove equivocally at this point is whether the reduction in the dimensions of the cleft presurgically and the manipulation of the nasal complex benefit our patients in the long term.
Keywords: presurgical orthopedic, nasoalveolar molding, cleft lip and palate
Introduction
Providing a high-quality care to cleft patients can be as challenging as the myriad of clinical presentations of orofacial clefting that occur. The child born with an orofacial cleft will usually require multidisciplinary, advanced and lifelong treatments. This complex clinical care challenges those who provide that care, and even pioneering countries such as the UK are faced with such challenges. Nearly 15 years ago, the investigation by the Clinical Standard Advisory Group (CSAG)1 highlighted the paucity of clinical excellence in Britain and recommended a more centralized service with better training facilities for specialists in order to improve clinical outcomes for patients. The importance of understanding the cleft lip and/or palate (CLP) patient care pathway is of paramount importance in order to be able to support the patients throughout their treatment.
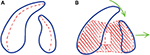
Infant patients who present with a complete bony cleft (Figure 1) may benefit from treatment in advance of the primary surgical repair of their lip and palate. Teams may offer initial treatment of their cleft to try to reduce the dimensions of the cleft with a process of treatments known as presurgical orthopedics (PSOs). CLP PSO treatment is usually provided by a cleft team clinician, commonly the orthodontist. Table 1 shows the different team members.
  | Figure 1 Complete unilateral cleft lip and palate patient. |
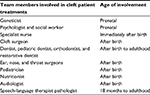  | Table 1 Different members of cleft team with suggested age of involvement |
The goals of repair of CLP are:2
- help patients to develop normal speech;
- restore dentition and oral functions;
- improve hearing;
- minimize facial difference;
- attain social acceptability of cleft individuals; and
- increase assimilation into society (psychological support)
- restore/reconstruct facial and oral anatomy.
In this review, we discuss the indications for PSOs and explore the literature and protocols that exist in this early infant treatment.
What are PSO treatments?
Molding the perioral structures of the infant with a CLP has been a clinical technique in use since before the 1950s. Attempts are made to reposition the nasolabial and maxillary segments closer to each other. It has been mainly used in the first few weeks after birth and in the months prior to palate repair. PSO treatment involves primarily the active movement of the maxillary fragments with passive or active alveolar plates prior to the surgical repair; this is often referred to as alveolar molding. Whenever a nasal stent is added to the alveolar plate, it is considered as nasoalveolar molding (NAM). Approximately half of surveyed centers in Europe used PSO techniques with mostly passive plates, whereas some teams also used a plate to assist with feeding (Figure 2).3
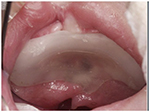  | Figure 2 Passive plate acts as a feeding plate. |
Objectives of PSOs
The main objectives of this presurgical step of treatment have been cited as:
- facilitating intra-oral feeding;
- improving maxillary growth;
- improving the projection of the nasal tip;
- reducing nasal deformity;
- facilitating primary lip, nasal, and alveolar surgeries; and
- retracting and repositioning the premaxilla more posteriorly in patients with bilateral cleft.
Controversies around PSOs
The use of orthopedic appliances has been always controversial, and there is much debate on this topic in the literature. It has been shown that it is possible to manipulate the infant’s oronasal complex, to narrow cleft width, to correct the anatomical position of the maxillary segment, and to improve the angulation of the palatal shelves to more horizontal position (Table 2).4 Some researchers question whether these short-term outcomes will have any beneficial long-term effects on the overall treatment outcome (Table 3).
  | Table 2 Suggested advantages of presurgical orthopedic treatment |
  | Table 3 Views of the opponent to presurgical orthopedic treatment Abbreviations: PSOs, presurgical orthopedics; NAM, nasoalveolar molding. |
Techniques of PSOs
Different approaches or techniques are suggested to achieve an orthopedic effect; they include alveolar molding, lip strap, NAM, and lip adhesion. The approach selection is usually determined by the operator preference and the type of cleft to be treated (Table 4).
  | Table 4 Presurgical orthopedic technique |
Alveolar molding
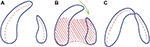
The maxillary segments of the child with a bony cleft are amenable to a degree of molding and repositioning if suitable appliances are used in the neonatal period. The ultimate goal is to attain an end-to-end position of the alveolar processes before lip operation. Appliances used to attain these positions of the alveolar processes are described as active (Figure 3) or passive appliances (Figure 4).
  | Figure 3 (A and B) Different shapes and designs for active appliances. |
  | Figure 4 Passive appliance. |
Active appliances mold the separate alveolar processes into position by applying active forces on them or, in other words, by directing them to grow or to be moved into a preplanned position. The construction of these appliances starts by creating an intraoral impression of the cleft infant and then pouring this impression into the plaster. Either the model is then sectioned and the acrylic mouth plate made on the adjusted plaster cast or a spring may be added to the plate to direct the alveolar processes to adapt a position where more normal maxillary arch form would be achieved (Figure 5).
Passive appliances are slightly different from active appliances. They are constructed on the poured study model and fit directly onto the alveolar processes. The clinician at the chairside may add flowable acrylic or remove acrylic in a process called negative sculpting. This alteration in the shape of the fit surface of the appliance will allow the alveolar processes to grow passively as planned by the clinician (Figure 6).
Lip strap/lip taping
A combination of intra-oral appliances and/or extra-oral orthopedic strapping (Figure 7) can be used in preparation for primary lip and plate surgery. In combination with the intraoral mouth plates, external tapes and elastics may be strapped to the cheeks to provide some external forces in the alveolar molding process. Elastic forces will exert a retracting, backward pressure against the protruding premaxilla, and careful use of forces on the cleft segments will improve their positions and allow definitive lip skin and muscle repair. In asymmetric cases, a lip bumper or pillow can be added to the tape to help to steer the segments to the desired position.
  | Figure 7 Lip strapping of the infant upper lip. |
If PSO correction is not able to be definitively completed, then the improved relations of the cleft segments may facilitate a temporary skin repair of the lip in a surgical operation known as a lip adhesion.
NAM
PSO has evolved, and NAM is a technique that has been adopted by several teams across the world. In this approach, a nasal stent is attached to the intra-oral mouth plate and is designed to improve nasolabial anatomy. It is reported that columella lengthening, reduction in alar asymmetry, and recovery of nasal tip projection can be achieved (Figure 8). The use of nasal stents in bilateral CLP in combination with lip tapes and elastics can lengthen the deficient columella.5 It has been proven that NAM improved surgical outcome for cleft patient, as it is effective in reducing hard and soft tissue deformity.6 Table 5 summarizes some of the findings of recent comparative studies.
  | Figure 8 Naso alveolar molding appliance. |
  | Table 5 Summary of findings from recent nasoalveolar molding studies |
PSOs between orthodontics and pediatric dentistry
In the literature, the role of the pediatric dentists and orthodontists may vary within different multidisciplinary teams, where the pediatric dentists’ role is mainly focused on oral anticipatory guidance to pregnant mothers and giving preventive advice and care as soon as the first primary tooth erupt in the CLP patient as well as restorative care as needed.7 However, it is not uncommon in some care centers to find that the role of the pediatric dentists starts much earlier than that, within the first few days after birth in constructing the PSO appliance.8,9 More commonly, the orthodontist is the responsible specialist who is involved in the construction of the PSO device.7 Nonetheless, who carries out the early treatment of CLP patients mainly depends on the setting of the multidisciplinary team within a specific hospital. It is therefore more important that the specialist has training in handling and managing young infants and that the procedure of taking an impression takes place in a hospital where the emergency team is ready to intervene if necessary.
Lip adhesion surgery
Many teams adopt a presurgical protocol to dovetail with their surgical protocols. Where PSO is not used, the use of previously discussed lip adhesion technique may be offered as the first stage of a two-stage repair of the lip. For the more displaced clefts, often bilateral cases, an initial bilateral lip adhesion is used where repair of the muscles is usually completed at a second surgical stage, perhaps 6 months later.
Bilateral lip adhesion acts like PSOs and helps to control the protrusive premaxilla and may enable a later definitive repair. Although there is no evidence that it would improve the outcome, it is often technically very difficult to close wide clefts with one surgical procedure. In addition, the repair of unilateral cleft can be difficult if the premaxilla has rotated to the repaired side. The use of lip adhesion within the first 3 months followed by a definitive lip revision usually permits the surgeon to perform surgery in stages as the face changes. However, definitive lip surgery can be performed at an earlier age (3 months) if the lip is to be repaired using one-stage technique (Table 6).
  | Table 6 Timing of lip surgery |
Surgical timing varies significantly from team to team and country to country, where some lip repairs are completed neonatally, perhaps as early as 3 weeks in some centers; in others, it may be completed at ≥3–6 months. However, it is quite reasonable to wait until the patient can undergo general anesthetic safely (the rule of “over ten” is usually followed [10 weeks of age, 10 pounds, and 10 g/dL of hemoglobin]).
The main goals of cleft lip surgery treatment are to 1) restore lip and nasal form; 2) reconstruct oral competence and orofacial muscle dynamicity; 3) improve cosmetic appearance; and 4) minimize maxillary growth disturbance (American Society of Maxillofacial Surgeons, 1994).10 Many techniques are discussed in the literature.
Every surgeon also can incorporate some modifications and variations depending on the case. However, the best therapeutic techniques in CLP surgery are those that have minimal negative effects on maxillofacial growth, and so ultimately as few and as conservative surgical episodes as possible are best when a patient has further natural growth to come.
Negative effects on growth may not become evident until after the pubertal growth spurt; however, whenever they do occur, it is usually associated with maxillofacial problems in all three planes of space and these may be reflected in the dental occlusion with incisor and buccal segment cross bites and/or cleft-centered open bite. These problems may add to the complexity of the later treatments and increase the need for orthognathic surgery. Interestingly, when investigators looked at unrepaired clefts of the palate, they found no interference with facial growth.11,12
Conclusion
Despite the fact that PSO treatments were popularized >60 years ago, the evidence related to this topic is still weak and inconclusive, mainly due to difficulty of study design and data collection. In addition, each procedure a patient undergoes muddies the waters and reduces our ability to tease out the effects of an individual treatment. All of this happens in a growing patient over a 20-year period.
As a result, different treatment protocols for different cleft subtypes were developed, according to Mossey et al3 – “The absence of a sound evidence base for selection of treatment protocols was shown by a striking diversity of practices across Europe for surgical care of just one cleft subtype—unilateral complete cleft of lip, alveolus, and palate”. Surprisingly, of 201 teams doing primary surgical repair for this cleft type, 194 different protocols were being practiced.
We know that PSO and NAM do help to approximate the segments of the cleft maxilla and do reduce the intersegment space in readiness for the surgical closure of cleft sites. However, what we remain unable to prove equivocally at this point is whether the reduction in the dimensions of the cleft presurgically and the manipulation of the nasal complex benefit our patients in the long term.
Our surgical colleagues anecdotally reported that they found smaller cleft gaps more straightforward to close than larger ones, but, as yet, the evidence does not support that the repair of a smaller cleft gap will lead to a better outcome.
The parents of the children in the images have provided written informed consent for the images to be published in this review.
Disclosure
The authors report no conflicts of interest in this work.
References
Sandy J, Williams A, Mildinhall S, et al. The Clinical Standards Advisory Group (CSAG) Cleft Lip and Palate Study. Br J Orthod. 1998; 25(1):21–30. | ||
Mosahebi A, Kangesu L. Cleft lip and palate. Surgery (Oxford). 2006; 24(1):33–37. | ||
Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. Lancet. 2009;374(9703):1773–1785. | ||
Prahl C, Kuijpers-Jagtman AM, van’t Hof MA, Prahl-Andersen B. A randomised prospective clinical trial into the effect of infant orthopaedics on maxillary arch dimensions in unilateral cleft lip and palate (Dutchcleft). Eur J Oral Sci. 2001;109(5):297–305. | ||
Penfold C, Dominguez-Gonzalez S. Bilateral cleft lip and nose repair. Br J Oral Maxillofac Surg. 2011;49(3):165–171. | ||
Retnakumari N, Ajith P, Divya S, Meenakumari S. Nasoalveolar molding treatment in presurgical infant orthopedics in cleft lip and cleft palate patients. Arch Med Health Sci. 2014;2(1):36–47. | ||
Ahmed MM, Brecht LE, Cutting CB, Grayson BH. 2012 American Board of Pediatric Dentistry College of Diplomates annual meeting: the role of pediatric dentists in the presurgical treatment of infants with cleft lip/cleft palate utilizing nasoalveolar molding. Pediatr Dent. 2012;34(7):e209–e214. | ||
Rivkin CJ, Keith O, Crawford PJ, Hathorn IS. Dental care for the patient with a cleft lip and palate. Part 1: from birth to the mixed dentition stage. Br Dent J. 2000;188(2):78–83. | ||
Rivkin CJ, Keith O, Crawford PJ, Hathorn IS. Dental care for the patient with a cleft lip and palate. Part 2: the mixed dentition stage through to adolescence and young adulthood. Br Dent J. 2000;188(3):131–134. | ||
Mitchell JC, Wood RJ. Management of cleft lip and palate in primary care. J Pediatr Health Care. 2000;14(1):13–19. | ||
Mars M, Houston WJ. A preliminary study of facial growth and morphology in unoperated male unilateral cleft lip and palate subjects over 13 years of age. Cleft Palate J. 1990;27(1):7–10. | ||
Mars M, James DR, Lamabadusuriya SP. The Sri Lankan Cleft Lip and Palate Project: the unoperated cleft lip and palate. Cleft Palate J. 1990; 27(1):3–6. | ||
Konst EM, Rietveld T, Peters HF, Kuijpers-Jagtman AM. Language skills of young children with unilateral cleft lip and palate following infant orthopedics: a randomized clinical trial. Cleft Palate Craniofac J. 2003;40(4):356–362. | ||
Abbott MM, Meara JG. Nasoalveolar molding in cleft care: is it efficacious? Plast Reconstr Surg. 2012;130(3):659–666. | ||
Garfinkle JS, King TW, Grayson BH, Brecht LE, Cutting CB. A 12-year anthropometric evaluation of the nose in bilateral cleft lip-cleft palate patients following nasoalveolar molding and cutting bilateral cleft lip and nose reconstruction. Plast Reconstr Surg. 2011;127(4):1659–1667. | ||
Spengler AL, Chavarria C, Teichgraeber JF, Gateno J, Xia JJ. Presurgical nasoalveolar molding therapy for the treatment of bilateral cleft lip and palate: a preliminary study. Cleft Palate Craniofac J. 2006;43(3):321–328. | ||
Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Cleft Palate J. 1987;24(1):5–77. | ||
Masarei AG, Wade A, Mars M, Sommerlad BC, Sell D. A randomized control trial investigating the effect of presurgical orthopedics on feeding in infants with cleft lip and/or palate. Cleft Palate Craniofac J. 2007;44(2):182–193. | ||
Knosel M, Fendel C, Jung K, Sandoval P, Engelke WG. Presurgical orthopedics by drink plates does not significantly normalize deglutition in infants with cleft lip and palate. Angle Orthod. 2016;86(2):315–323. | ||
Chang CS, Wallace CG, Pai BC, et al. Comparison of two nasoalveolar molding techniques in unilateral complete cleft lip patients: a randomized, prospective, single-blind trial to compare nasal outcomes. Plast Reconstr Surg. 2014;134(2):275–282. | ||
Liao YF, Wang YC, Chen IJ, Pai CJ, Ko WC, Wang YC. Comparative outcomes of two nasoalveolar molding techniques for bilateral cleft nose deformity. Plast Reconstr Surg. 2014;133(1):103–110. | ||
Clark SL, Teichgraeber JF, Fleshman RG, et al. Long-term treatment outcome of presurgical nasoalveolar molding in patients with unilateral cleft lip and palate. J Craniofac Surg. 2011;22(1):333–336. | ||
Shetty V, Vyas HJ, Sharma SM, Sailer HF. A comparison of results using nasoalveolar moulding in cleft infants treated within 1 month of life versus those treated after this period: development of a new protocol. Int J Oral Maxillofac Surg. 2012;41(1):28–36. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.