Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
Presence of Hepatocellular Carcinoma Does Not Affect Course and Response to Anticoagulation of Bland Portal Vein Thrombosis in Cirrhotic Patients
Authors Benevento F, Pecorelli A, Stefanescu H, Sparchez Z, Vukotic R, Pettinari I, Grigoras CA, Tovoli F, Ravaioli F , Stefanini B , Andreone P , Piscaglia F
Received 27 October 2022
Accepted for publication 15 March 2023
Published 27 March 2023 Volume 2023:10 Pages 473—482
DOI https://doi.org/10.2147/JHC.S390777
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Jörg Trojan
Francesca Benevento,1 Anna Pecorelli,2 Horia Stefanescu,3 Zeno Sparchez,3 Ranka Vukotic,1,4 Irene Pettinari,2 Crina-Anca Grigoras,3 Francesco Tovoli,1,5 Federico Ravaioli,1 Bernardo Stefanini,1 Pietro Andreone,6 Fabio Piscaglia1,5
1Department of Medicine and Surgical Sciences (DIMEC), University of Bologna, Bologna, Italy; 2Department of Radiology, IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy; 3Gastroenterology Department, Liver Unit & Ultrasound Laboratory, Regional Institute of Gastroenterology and Hepatology, Cluj-Napoca, Romania; 4Medicina Interna 4, Azienda Ospedaliero-Universitaria Pisana, Pisa, Italy; 5Division of Internal Medicine, Hepatobiliary and Immunoallergic Diseases, IRCCS Azienda Ospedaliero-Universitaria di Bologna, Bologna, Italy; 6Divisione di Medicina Interna a Indirizzo Metabolico-Nutrizionale, Azienda Ospedaliero-Universitaria di Modena, Modena, Italy
Correspondence: Fabio Piscaglia, Email [email protected]
Background: Malignancies are generally considered a risk factor for deep vein thrombosis and may hamper the recanalisation of thrombosed veins.
Aim: We investigate whether the natural course and response to anticoagulant treatment of bland portal vein thrombosis (PVT) in patients with cirrhosis complicated by hepatocellular carcinoma (HCC) differ from those without HCC.
Methods: Retrospective study in two hepatology referral centres, in Italy and Romania where patients with a diagnosis of PVT on cirrhosis and follow-up of at least 3 months with repeated imaging were included.
Results: A total of 162 patients with PVT and matching inclusion and exclusion criteria were identified: 30 with HCC were compared to 132 without HCC. Etiologies, Child-Pugh Score (7 vs 7) and MELD scores (11 vs 12, p=0.3679) did not differ. Anticoagulation was administered to 43% HCC vs 42% nonHCC. The extension of PVT in the main portal trunk was similar: partial/total involvement was 73.3/6.7% in HCC vs 67.4/6.1% in nonHCC, p=0.760. The remainder had intrahepatic PVT. The recanalization rate was 61.5% and 60.7% in HCC/nonHCC in anticoagulated patients (p=1). Overall PVT recanalisation, including treated and untreated patients, was observed in 30% of HCC vs 37.9% of nonHCC, p=0.530. Major bleeding incidence was almost identical (3.3% vs 3.8%, p=1). Progression of PVT after stopping anticoagulation did not differ (10% vs 15.9%, respectively, HCC/nHCC, p=0.109).
Conclusion: The course of bland non-malignant PVT in cirrhosis is not affected by the presence of active HCC. Treatment with anticoagulation in patients with active HCC is safe and as effective as in nonHCC patients, this can potentially allow us to use otherwise contraindicated therapies (ie TACE) if a complete recanalization is achieved with anticoagulation.
Keywords: LC, liver cirrhosis, HCC, hepatocellular carcinoma, PVT, portal vein thrombosis
Introduction
Portal vein thrombosis (PVT) consists of the presence of a venous thrombus located within the meso-splenic-portal system. It is a rare event in the general population but occurs more frequently in patients with liver cirrhosis due to various disease-related abnormalities,1 and its incidence increases with the severity of the liver disease. The prevalence of PVT ranges between 0.6% and 26% in cirrhotic patients.2,3 As PVT may cause short-term as well as long-term complications, adopting adequate diagnostic and therapeutic measures could be of paramount importance.4
The presence of active cancer is a known, very relevant factor favouring the occurrence of deep vein thrombosis and pulmonary embolism, and the cellular type may influence the clinical course of such complications.5 Moreover, it also increases the risk of recurrences of pulmonary thromboembolism and the occurrence of bleeding episodes in cases of anticoagulation compared to non-cancer conditions or even with only a history of cancer.6
Patients with hepatocellular carcinoma (HCC) may not only suffer portal vein tumour infiltration but are also often affected by bland non-neoplastic PVT, which is possibly favoured by malignancy and by the presence of underlying liver cirrhosis.7,8 The presence of bland PVT does not change the tumour stage but alters hepatic perfusion and impacts portal hypertension, affecting the possibility of delivering effective HCC treatment, which would be foreseen for that specific tumour stage. For instance, portal vein occlusion may contraindicate endovascular tumour treatment with chemoembolisation. The contraindication derives from the risk of inducing hepatic infarctions caused by the complete (arterial and portal) blood inflow blockade with consequent liver function deterioration. Moreover, an extensive PVT may hamper the technical possibility of liver transplantation, for which HCC has recently become a common indication. Finally, PVT occurrence induces portal hypertension, potentially contraindicating surgical resections of HCC. Therefore, resolving the presence of bland PVT in HCC patients could certainly be beneficial.
Whether the presence of HCC impacts the capacity of anticoagulant treatment to restore venous patency or increases the risk of bleeding under anticoagulation, as it happens in other cancers,6 has very scarcely been investigated so far, thus the decision to start an anticoagulant treatment in this group of patients is usually controversial.
Therefore, to elucidate this issue, we took advantage of a large retrospectively collected case series of patients with PVT,8 these patients were either treated with anticoagulants or did not receive any kind of treatment for PVT according to the physician choice since no clear recommendation was available at that time.
Patients and Methods
Patients
Patients for the present study were obtained from a previously published retrospective study investigating the safety and effectiveness of anticoagulants in cirrhosis.9 For general inclusion and exclusion criteria, see Pettinari et al.9
Briefly, a total of 182 patients with PVT were retrospectively identified in two hepatology referral centres in Italy and Romania. Inclusion criteria were as follows: diagnosis of bland non-neoplastic PVT on cirrhosis between January 2008 and March 2016 based on strict imaging criteria and biopsy when needed,10 at least 3 months of follow-up with repeated imaging after diagnosis.
The main exclusion criterion was the presence of active non-hepatocellular malignancy. For this study, a history of previously treated HCC with no recurrent active tumour was considered as an additional exclusion criterion since these patients could not have been attributed to either one or the other study group.
Recanalization of the PVT was defined as complete clearance of the main portal vein trunk (if involved) or reduction by 50% in thrombus size (thickness or longitudinal extension).
Statistical Analysis
Descriptive analyses of categorical variables were performed using absolute numbers and percentages and continuous variables using the mean and standard deviation or median and quartiles after assessing variable distribution using the Kolmogorov–Smirnov test. Categorical variables were compared with Fisher exact test and continuous variables with Student-t. Survival was calculated from the first PVT diagnosis to death/liver transplantation or the last follow-up visit and expressed as median and 95% confidence interval (95% CI). Survival curves were generated using the Kaplan–Meier method and compared with the Log rank test. A two-tailed p < 0.05 was considered statistically significant. All statistical analyses were performed using the ®SPSS 21.0 statistical package (SPSS Inc., Chicago, Illinois, USA).
Ethics
The study was conducted in compliance with the Declaration of Helsinki and was approved by the Ethics Committees of the General and University Hospital Sant’Orsola-Malpighi, Bologna, Italy, and of the University of Medicine and Pharmacy “Iuliu Hatieganu”, Cluj-Napoca, Romania (111/2015/O/OssN). Written informed consent was obtained from each patient.
Results
Patient’s Baseline Characteristics at the Time of PVT Diagnosis
After excluding 20 patients from the previous series due to a history of previously treated HCC with no recurrent active tumour, a final study population of 162 patients was obtained, of whom 30 with active untreated HCC and 132 without active HCC.
The mean age of patients was 57.6±11.4 years; most were male (n=111, 68.5%). Liver cirrhosis was mainly caused by alcohol abuse (n=51, 28.0%), followed by HCV infection (n=49, 26.8%). Splitting patients according to the presence or absence of active HCC, no differences were found between the two groups regarding age, sex and etiology of liver cirrhosis. BCLC stage in HCC patients was as follows: “Very early = BCLC-0” (n=2, 6.6%), “Early = BCLC-A” (n=22, 73.3%), “Intermediate = BCLC-B” (n=3, 10%) and “advanced = BCLC-C” (n=3, 10%). Also, liver function, expressed as either Child-Pugh score (7 [5–12] and 7 [5–13]; p=0.864) or MELD score (11 [8–22] and 12 [7–29]; p=0.367) did not differ between the two groups. Nonetheless, patients with HCC had slightly lower values of bilirubin and INR in comparison to patients without HCC (2.0 ± 1.3 and 2.5 ± 2.4 mg/dl; p=0.010; 1.2 ± 0.4 and 1.4 ± 0.5; p=0.010 respectively). Other demographic and clinical characteristics of the study population are summarised in Table 1.
 |
Table 1 Demographic and Clinical Characteristics of Patients with and without HCC at the Time of PVT Diagnosis |
Portal Vein Thrombosis Features at Diagnosis
Both in HCC and non-HCC groups, PVT was mostly diagnosed with US examinations, even though the diagnosis was made with CT scan in a higher proportion of patients with than without liver cancer (n=13, 43.3% vs n=27, 20.4% p=0.017), due to the more extensive imaging assessment in patients with an active malignancy. The majority of subjects showed thrombotic involvement of the main portal vein trunk (all patients: n=121, 74.7%; HCC patients: n=24, 80% and nonHCC patients: n=97, 73.5%; p=0.642). Approximately half of the patients showed involvement of the intrahepatic vein branches, either isolated or associated with portal trunk PVT, without a difference between the two groups (all patients: n=82, 50.6%; HCC patients: n=13, 43.3% and non-HCC patients: n=69, 52.3%; p=0.422). Table 2 shows that more patients with active HCC presented extension of PVT to the superior mesenteric vein at the time of diagnosis (n=11, 36.7% vs n=25, 15.9%; p=0.050), but fewer showed extension to the splenic vein (n=1, 3.3%/0 vs n=18, 13.6%/ n=3, 2.3%; p=0.184) than cirrhotics without HCC.
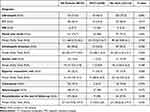 |
Table 2 Portal Vein Thrombosis and Imaging Characteristics of Patients with PVT |
Anticoagulant Treatment and Course of Portal Vein Thrombosis
Considering the whole study population, 69 (42.6%) patients were treated with anticoagulant therapy, with similar rates in the two study groups (HCC group: n=13, 43.3% and non-HCC group: n=56, 42.4%; p=1) (Table 3). Anticoagulation was promptly started after PVT diagnosis in most cases, as expected (Table 4). The mean treatment duration was 13.7 ±14.5 months but shorter in patients with liver cancer (6.5 ± 4.6 vs 15.5 ± 15.6 months; p=0.004). A total of 50 patients (30.9%) received low molecular weight heparin (LMWH), 10 (6.2%) oral anticoagulants (vitamin K antagonists VKAs) and 9 (5.5%) fondaparinux, without difference between patients with and without HCC. No differences were found in the administered dose (Table 4).
 |
Table 3 Baseline Characteristics of Patients Who Received Anticoagulation (n=69) |
 |
Table 4 Treatment Characteristics in Patients with and without HCC at the Time of PVT Diagnosis |
Portal Vein Recanalization
A total of 59 (36.4%) patients showed portal vein recanalization, which was partial in 27 (16.7%) and complete in 32 (19.7%), mean time to recanalization was 4.5 ± 3.6 months. No differences were found both in recanalization rates and in mean time to recanalization between HCC and non-HCC groups (n=9, 30% vs n=50, 37.9%; p=0.530 and 3.6 ± 3.6 vs 4.8 ± 3.6 months; p=0.469, respectively). Considering only patients treated with anticoagulant therapy, 35 experienced portal vein recanalisation at the end of follow-up, with no differences between HCC and non-HCC groups (n=6, 46.1%, n=29, 51.9%, p=0.631). Thirty-one non-HCC patients developed PVT progression, of whom 10 (7.5%) during and 21 (15.9%) after stopping anticoagulation, in comparison to 3 (10.0%) patients with active HCC who showed PVT progression, all of them after the stop of treatment. Bleeding complications led to premature discontinuation of anticoagulant therapy in 1 (3.3%) patient with HCC and 5 (3.8%) patients without HCC (p=1). At the end of follow-up (mean time 23.6 ± 18.6 months), 25 (83.3%) HCC patients and 108 (81.8%) non-HCC patients were alive. The median overall survival of patients with HCC was 50.0 months (95% CI: 35.3–64.8) versus 66.0 months (95% CI: 56.5–75.5) of patients without active HCC (p=0.739). The survival did not differ between the two groups, also considering only the anticoagulated patients (HCC group: 52.6 months (95% CI: 31.8–73.4); non-HCC group: 68.9 months (95% CI: 60.0–77.9); p=0.535).
Discussion
The present data show that the presence of early stage HCC does not negatively affect the course of bland PVT and the response to anticoagulation.
Malignancies are generally considered a risk factor for deep vein thrombosis and may hamper the recanalisation of thrombosed veins.11 HCC often occurs in cirrhosis, a condition suffering an incidence of up to 20%/year of bland non-neoplastic PVT, depending on the severity of liver dysfunction.7,8 PVT is a frequent complication in liver cirrhosis,2,7,8 but its natural history and therapeutic management have been partially and only recently explored by scientific research and international guidelines, but the specific field of patients with primary liver cancer with PVT and cirrhosis lack similar information and have been hardly objected of dedicated research. Liver cirrhosis has historically been considered a condition prone to coagulopathy-related bleeding risk due to the low platelet count and prolonged INR, however this paradigm has been recently challenged because spontaneous bleeding was not found to occur with increased frequency in cirrhosis (excluding that from the upper gastrointestinal system, which is specifically induced by portal hypertension), as demonstrated by a low rate of intracranial haemorrhage events compared with a control population.12
Due to these safety concerns and borderline clinical benefits13–15 anticoagulation treatment in cirrhotic patients with PVT has been largely underutilized, only recently consensus of expert shifted toward a more decise recommendation to treat with anticoagulation patients with bland PVT.16,17 However, given the relatively weak strength of evidence supporting this recommendation, the individual choice regarding anticoagulation is still often debated and physicians usually take in consideration also personal attitudes such as fear of bleeding or patient conditions, awaiting stronger scientific evidence.
While solid data from well-designed randomized trial are lacking, published evidence tends to suggest that anticoagulation in cirrhosis is at least safe,9,18 provided that patients are adequately managed (prophylaxis of esophageal bleeding and type and dosage of anticoagulation accurately tailored).8,9,17
In connection with the issue of any possible survival benefit from anticoagulation rather than harm, the published findings are far from conclusive.9,13,14,19,20 Unfortunately, only a few retrospective studies are available, which implies significant risks of bias when drawing conclusions about survival. In fact, factors such as the severity of liver dysfunction could have influenced both survival and the decision to start anticoagulation. In conclusion, data cannot lead to any message about generalised treatment with anticoagulation in all cirrhotic patients with PVT, but at the same time, point out the idea that this option should not be discarded “a priori” because held as hazardous.
Our current findings confirm that the option of anticoagulation should also be considered in patients with HCC, as these patients are not less responsive than cirrhotic patients without cancer because of the presence of cancer and are not at higher risk of complications. It is worth remarking that our data mainly apply to patients in the early tumour stage, as these made up the largest part of our population. This is consistent with the fact that many patients with HCC at an advanced stage frequently suffer from tumour portal vein invasion rather than bland thrombosis.2
Our results are apparently slightly different from a previous very small study,21 which showed no increase in recanalisation rates under coagulation. However, they only included 12 patients with PVT collected over a very long interval (2001–2015). In addition to this, authors did not clarify whether the presence of concomitant tumour portal vein infiltration, rather than only bland portal thrombosis, had been definitively ruled out. This limitation is particularly significant because patients who received anticoagulation were classified to be in the advanced tumour stage where neoplastic portal vein thrombosis is frequent. Additionally, also whether patients still had active HCC or not at the time of anticoagulation (most of the patients were treated) was not specified.
The limitations of our present study are mainly related to its retrospective nature. The first one is the lack of a standardised anticoagulation protocol, which makes it impossible to state a clear-cut recommendation regarding anticoagulation drug choice and doses. Moreover, the assessment of PVT extension and evaluation of the degree of response were provided using different imaging techniques. Ultrasound (US) is accurate in investigating the presence and extension of intrahepatic thrombosis; however, it is not as accurate as CT and MRI in the case of extrahepatic involvement. CT and MRI are expensive and require the injection of potentially harmful contrast agents, while the US is less costly and easily complemented by colour/duplex Doppler and by safe contrast agents. Computed tomography also implies exposure to radiation. Therefore, CT and MRI are much less feasible for the short-/mid-term follow-up of PVT to monitor progression or regression, especially in non-oncologic patients. For this reason, the US was the technique adopted in most patients in the present study. In the authors’ view, the different imaging techniques have complementary rather than competing roles in this setting.
Another point to highlight is that it is often impossible to date the thrombus correctly. In the present study, all patients were consecutively enrolled at the time of the first observation of PVT, regardless of the presence or absence of PVT-related symptoms. PVT is commonly asymptomatic; symptoms may develop only later when partial PVT progresses to complete PVT. Finally, only the detection of a cavernomatous transformation of the portal veins definitely excludes acute PVT. Hence, the presence/absence of symptoms is not a reliable index for dating the first occurrence of PVT when imaging cannot provide this information. Another limitation related to the variable imaging follow-up, either after anticoagulants or not, is that we cannot provide information about the speed of recanalization under anticoagulants, whether it occurs rapidly (eg <2 weeks) or slowly (e.g. >3 months). This information would be particularly relevant in the setting of HCC as it could influence the possibility to adopt or not some antitumoural treatments (surgical or endovascular), for which the patient cannot wait long.
In conclusion, the present study showed that active HCC does not negatively impact the course of bland non-malignant PVT and the effectiveness of anticoagulants to treat it.
Furthermore, the presence of HCC does not cause any additional concern in terms of safety compared to non-HCC cirrhosis and non-anticoagulated patients. Thus, early stages of HCC complicated by bland non-malignant PVT can be safely treated with anticoagulation, potentially enabling otherwise contraindicated therapies (ie TACE) if a complete recanalization of portal flow is to be obtained.
Data Sharing Statement
Individual data of patients included may be shared upon request to the corresponding author.
Acknowledgments
The co-investigators of the BOlogna LIVEr vascular Studies (BO-LIVES) study group are as follows: Morelli C, Serra C, Verucchi G, Badia L, Golfieri R, Mosconi C, Cucchetti A, Cescon M, Granito A, Mulazzani L, Colecchia A, Festi D.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
No grants or other financial support.
Disclosure
Dr Francesco Tovoli reports personal fees from Roche, Eisai, and Ipsen, outside the submitted work. Prof. Dr. Fabio Piscaglia reports personal fees from Bracco, Bayer, EISAI, ESAOTE, IPSEN, MSD, Roche, Samsung, Tiziana Life Sciences, Exact Science, and AstraZeneca during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Andriulli A, Tripodi A, Angeli P.; Under the Auspices of the Italian Association for the Study of Liver Diseases (AISF) and the Italian Society of Internal Medicine (SIMI). Hemostatic balance in patients with liver cirrhosis: report of a consensus conference. Dig Liver Dis. 2016;48(5):455–467. doi:10.1016/j.dld.2016.02.008
2. Tsochatzis EA, Senzolo M, Germani G, et al. Systematic review: portal vein thrombosis in cirrhosis. Aliment Pharmacol Ther. 2010;31(3):366–374. doi:10.1111/j.1365-2036.2009.04182.x
3. Violi F, Corazza RG, Caldwell SH, et al. Portalvein thrombosis relevance on liver cirrhosis: Italian Venous Thrombotic Events Registry. Intern Emerg Med. 2016;11:1059–1066. doi:10.1007/s11739-016-1416-8
4. von Kockritz L, De Gottardi A, Trebicka J, Praktiknjo M. Portal vein thrombosis in patients with cirrhosis. Gastroenterol Rep. 2017;5(2):148–156. doi:10.1093/gastro/gox014
5. Mahé I, Chidiac J, Bertoletti L, et al.; RIETE investigators. The clinical course of venousthromboembolism may differ to cancer site. Am J Med. 2017;130(3):337–347. doi:10.1016/j.amjmed.2016.10.017
6. Prins MH, Lensing AWA, Brighton TA, et al. Oral rivaroxaban versus enoxaparin with vitamin Kantagonist for the treatment of symptomatic venousthromboembolism in patients with cancer (EINSTEIN-DVTand EINSTEIN-PE): a pooled subgroup analysis of two randomised controlled trials. Lancet Haematol. 2014;1(1):e37–e46. doi:10.1016/S2352-3026(14)70018-3
7. Nery F, Chevret S, Condat B, et al. Causes and consequences of portal vein thrombosis in 1243 patients with cirrhosis: results of a longitudinal study. Hepatology. 2015;61:660–667. doi:10.1002/hep.27546
8. Villa E, Cammà C, Marietta M, et al. Enoxaparin prevents portal vein thrombosis and liver decompensation in patients with advanced cirrhosis. Gastroenterology. 2012;143:1253–1260. doi:10.1053/j.gastro.2012.07.018
9. Pettinari I, Vukotic R, Stefanescu H, et al.; BO-LIVES (Bologna LIVErvascular Studies). Clinical impact and safety of anticoagulants for portal vein thrombosis in chirrhosis. Am J Gastroenterol. 2019;114(2):258–266. doi:10.1038/s41395-018-0421-0
10. Piscaglia F, Gianstefani A, Ravaioli M, et al. Criteria for diagnosing benign portal vein thrombosis in the assessment of patients with cirrhosis and hepatocellular carcinoma for liver transplantation. Liver Transpl. 2010;16:658–667. doi:10.1002/lt.22044
11. Lip GY, Chin BS, Blann AD. Cancer and the prothrombotic state. Lancet Oncol. 2002;3(1):27–34. PMID: 11908507. doi:10.1016/s1470-2045(01)00619-2
12. Lai CH, Cheng PY, Chen YY. Liver cirrhosis and risk ofintracerebral haemorrhage: a 9-year follow-up study. Stroke. 2011;42:2615–2617. doi:10.1161/STROKEAHA.111.617076
13. Mancuso A, Politi F, Maringhini A. Portal vein thromboses in cirrhosis: to treat or not to treat? Gastroenterology. 2018;154:758. doi:10.1053/j.gastro.2017.07.053
14. Piscaglia F, Sansone V. Reply to anticoagulation for portal vein thrombosis in cirrhosis. Am J Gastroenterol. 2019;114(6):1001–1002. doi:10.14309/ajg.0000000000000274
15. Chak EW. Anticoagulation of portal vein thrombosis in cirrhosis: first, do no harm. Am J Gastroenterol. 2019. doi:10.14309/ajg.0000000000000351
16. European Association for the Study of the Liver. EASL Clinical Practice Guidelines on prevention and management of bleeding and thrombosis in patients with cirrhosis. J Hepatol. 2022;76(5):1151–1184. PMID: 35300861. doi:10.1016/j.jhep.2021.09.003
17. Hanafy AS, Abd-Elsalam S, Dawoud MM. Randomized controlled trial of rivaroxaban versus warfarin in the management of acute non-neoplastic portal vein thrombosis. Vascul Pharmacol. 2019;113:86–91. PMID: 29886103. doi:10.1016/j.vph.2018.05.002
18. Loffredo L, Pastori D, Farcomeni A, Violi F. Effects of anticoagulants in patients with cirrhosis and portal vein thrombosis: a systematic review and meta-analysis. Gastroenterology. 2017;153:480–487. doi:10.1053/j.gastro.2017.04.042
19. Turon F, Hernández-Gea V, García-Pagán JC. Portal vein thrombosis: yes or no on anticoagulation therapy. Curr Opin Organ Transplant. 2018;23:250–256. doi:10.1097/MOT.0000000000000506
20. Piscaglia F, Benevento F, Pecorell A, Forgione A, Stefanescu H. Anticoagulation in cirrhotic portal vein thrombosis: no harm, but survival benefit still unclear. Am J Gastroenterol. 2020;115(1):145–146. PMID: 31809302. doi:10.14309/ajg.0000000000000483
21. Mahmoudi TM, Marquez V, Kayal A, Carvalho R, Weiss AA HCC complicated by PVT: outcome and the role of anticoagulation therapy. Can Liver J 2019;27:121–126. doi:10.3138/canlivj.2018-0026
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
