Back to Journals » Infection and Drug Resistance » Volume 16
Preparing for the Next Influenza Season: Monitoring the Emergence and Spread of Antiviral Resistance
Authors Oh DY, Milde J, Ham Y, Ramos Calderón JP, Wedde M, Dürrwald R , Duwe SC
Received 8 September 2022
Accepted for publication 16 January 2023
Published 15 February 2023 Volume 2023:16 Pages 949—959
DOI https://doi.org/10.2147/IDR.S389263
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Djin-Ye Oh, Jeanette Milde, Youngsun Ham, Julia Patricia Ramos Calderón, Marianne Wedde, Ralf Dürrwald, Susanne C Duwe
Robert Koch Institute, Department 1: Infectious Diseases, Unit 17: Influenza and Other Respiratory Viruses, National Influenza Center, Berlin, Germany
Correspondence: Susanne C Duwe, Robert Koch Institute, Department 1: Infectious Diseases, Unit 17: Influenza Viruses and Other Respiratory Viruses | National Influenza Center, Seestr. 10, Berlin, 13353, Germany, Tel +49 30 18754 2283, Fax +49 30 18754 2699, Email [email protected]
Purpose: The relaxation of pandemic restrictions in 2022 has led to a reemergence of respiratory virus circulation worldwide and anticipation of substantial influenza waves for the 2022/2023 Northern Hemisphere winter. Therefore, the antiviral susceptibility profiles of human influenza viruses circulating in Germany were characterized.
Methods: Between October 2019 (week 40/2019) and March 2022 (week 12/2022), nasal swabs from untreated patients with acute respiratory symptoms were collected in the national German influenza surveillance system. A total of 598 influenza viruses were isolated and analyzed for susceptibility to oseltamivir, zanamivir and peramivir, using a neuraminidase (NA) inhibition assay. In addition, next-generation sequencing was applied to assess molecular markers of resistance to NA, cap-dependent endonuclease (PA) and M2 ion channel inhibitors (NAI, PAI, M2I) in 367 primary clinical samples. Furthermore, a genotyping assay based on RT-PCR and pyrosequencing to rapidly assess the molecular resistance marker PA-I38X in PA genes was designed and established.
Results: While NAI resistance in the strict sense, defined by a ≥ 10-fold (influenza A) or ≥ 5-fold (influenza B) increase of NAI IC50, was not detected, a subtype A(H1N1)pdm09 isolate displayed 2.3- to 7.5-fold IC50 increase for all three NAI. This isolate carried the NA-S247N substitution, which is known to enhance NAI resistance induced by NA-H275Y. All sequenced influenza A viruses carried the M2-S31N substitution, which confers resistance to M2I. Of note, one A(H3N2) virus displayed the PA-I38M substitution, which is associated with reduced susceptibility to the PAI baloxavir marboxil. Pyrosequencing analysis confirmed these findings in the original clinical specimen and in cultured virus isolate, suggesting sufficient replicative fitness of this virus mutant.
Conclusion: Over the last three influenza seasons, the vast majority of influenza viruses in this national-level sentinel were susceptible to NAIs and PAIs. These findings support the use of antivirals in the upcoming influenza season.
Keywords: influenza viruses, antiviral resistance, phenotypic assay, genotypic assay, surveillance, neuraminidase, cap-dependent endonuclease, baloxavir marboxil, molecular resistance marker
Introduction
Influenza remains one of the most important infectious diseases in the world, causing seasonal epidemics that result in estimated annual 3–5 million cases of severe illness and 300,000–500,000 deaths on a global level.1,2 In Germany, influenza type A and B viruses usually attack 5–10% of adults and 20–30% of children, thereby causing millions of acute respiratory infections.3
Three classes of antiviral agents have been approved for treatment and prevention of influenza infections in Germany and many other countries: M2 ion channel inhibitors (M2I), neuraminidase inhibitors (NAI) and the cap-dependent endonuclease inhibitor (PAI) baloxavir marboxil. Use of M2Is, or adamantanes, is currently not recommended due to their lack of activity against influenza B viruses, and because of the rapid emergence and transmission of drug-resistant influenza A viruses. NAIs, active against both influenza type A and type B viruses by preventing release and spread of progeny viruses, are the first-line agents recommended for influenza treatment.3 They include oseltamivir, zanamivir and peramivir, which are administered orally, by inhalation and intravenously, respectively. Peramivir marketing authorization, granted by the European Medical Agency (EMA) in 2018, was withdrawn at the request of the license holder in December, 2020. PAIs impede the cap-dependent endonuclease activity of the influenza polymerase acidic (PA) protein. The first PAI, baloxavir marboxil, approved as an oral agent for early treatment of uncomplicated influenza in adults, received its marketing authorization in the United States and Japan in 2018 and in the EU/EEA in 2021.3–7
The emergence and spread of viruses harboring reduced susceptibility to these antivirals may pose major challenges to the clinical management of influenza. Thus, the antiviral susceptibility assessment of currently circulating influenza viruses represents an essential, WHO-required component of influenza virologic surveillance at all National Influenza Centers (NICs).8 While NAI susceptibility is routinely assessed phenotypically, using a neuraminidase inhibition assay on selected samples, sequence analysis of the PA, NA and M2 genes is applied to identify known molecular resistance markers for all three classes of antivirals.3,9,10
During the COVID-19 pandemic, nonpharmaceutical interventions (NPIs), applied internationally in order to curb the spread of SARS-CoV-2, led to a substantial decrease of global influenza activity throughout the 2020/21 and 2021/22 seasons.11 In 2022, many if not all NPIs have been lifted in most parts of the world; accordingly, a substantial resurgence of influenza activity is anticipated for the 2022/23 influenza season. Indeed, Australian influenza surveillance in 2022, which is considered predictive of Northern hemisphere influenza activity, has revealed lab-confirmed influenza cases well above the historical average.12–14 Moreover, cocirculation of influenza viruses with SARS-CoV-2, RSV and other respiratory viruses in the upcoming winter season is to be expected; infections with these viruses, potentially complicated by secondary illnesses such as pneumonia, may lead to a significant strain of the health-care system. It can be assumed that this may also result in an increased use of available antivirals, which in turn could cause the emergence and spread of drug-resistant viruses.
Thus, preparation for a significant winter influenza season is prudent; this requires a sound understanding of the antiviral susceptibility profiles of the human influenza viruses that are currently in circulation.12
The aim of the study was to determine the antiviral susceptibility profiles of human influenza viruses in preparation for the next influenza seasons and before a new class of antiviral drugs is launched on the German market. Therefore, influenza viruses circulating in Germany in 2019/20 and 2021/22 were analyzed for molecular resistance markers of neuraminidase, cap-dependent endonuclease and M2 ion channel inhibitors, as well as in vitro activity of NAI and PAI.
Materials and Methods
Clinical Specimens and Influenza Virus Typing and Subtyping
Clinical specimens originated from ambulatory, untreated patients presenting with acute respiratory or influenza-like illness to clinics participating in Germany’s national sentinel system for monitoring acute respiratory infections (ARI).11 Nasal, throat or pharyngeal swabs, collected by sentinel physicians between October 2019 and March 2022, were delivered in 1 mL viral transport media to the German National Influenza Center (NIC) at Robert Koch-Institute. Swabs were washed in 3.0 mL cell culture medium (MEM/HEPES, Minimum Essential Media with Hepes and 1% penicillin/streptomycin) and RNA was extracted using the MagNAPure 96 DNA and Viral NA Small Volume or the MagNA Pure 24 Total NA Isolation Kits (Roche, Mannheim, Germany) eluting in 50 µL buffer. After synthesis of complementary DNA by random reverse transcription (Invitrogen, Carlsbad, California), primers and probes targeting the M, HA and NA genes were used for in-house multiplex influenza typing and subtyping as previously described.11,15,16
Ethics Statement
Written approval for the German national surveillance of influenza and other respiratory viruses was obtained from the Charité-Universitätsmedizin Berlin Ethical Board (reference EA2/126/11) and sentinel surveillance is covered by German legislation (§13, §14, Protection against Infection Act). All analyses were based on pseudonymized data. Written and informed consent was obtained from all sentinel patients.
Antiviral Drugs
Oseltamivir carboxylate was kindly provided by Hoffmann-La Roche Ltd. (Basel, Switzerland), zanamivir was kindly supplied by GSK plc. (London, United Kingdom) free of charge, and peramivir was provided by Hölzel Diagnostika Handels GmbH (Köln, Germany). All NAIs were resuspended and diluted in sterile ultra-pure bi-distilled water to generate 100 µM (oseltamivir carboxylate, zanamivir) and 10 µM (peramivir) stock solutions, which were stored at −20°C. For susceptibility assays, stock solutions were diluted in MES buffer [32.5 mM morpholineethanesulfonic acid (Merck KGaA/Sigma-Aldrich, Darmstadt, Germany), pH 6.5, and 4 mM CaCl2].
Baloxavir marboxil, provided by Hölzel Diagnostika Handels GmbH (Köln, Germany), was resolved in DMSO to generate 100 µM stock solutions which were stored at −80°C until use.
Genotypic Analysis of Influenza Genes
Next Generation Sequencing
Viral RNA was extracted with the ReliaPrep™ Cell Mini Kit (Promega, Walldorf, Germany), using a protocol adapted for extraction of RNA from seasonal influenza viruses. First, 200 µL diluted specimen, 50 µL water and 250 µL freshly prepared buffer (BL+TG lysis buffer) were mixed by vortexing. Next, 85 µL of isopropanol (100%, Carl Roth, Karlsruhe, Germany) were added and mixed by vortexing. All subsequent steps (including DNase digestion) were performed according to manufacturer’s instructions. Then, multisegment reverse transcription-PCR was carried out for influenza A and influenza B viruses as described elsewhere.17,18 NGS was performed using 1 ng of purified One-Step RT-PCR product, Nextera XT DNA Library Preparation Kit and subsequently the ISeq platform (Illumina, San Diego, USA). Trimming, reference mapping and generation of consensus sequences were done with Geneious software (11.1.5) and genome sequences (minority variants ≥10%) were deposited in GISAID (www.GISAID.org). The GISAID accession numbers of sequences analyzed and reference sequences used are listed in Supplementary Table 1, which is part of the supplementary data provided with this manuscript.
NGS data were analyzed for molecular resistance markers in NA, M2 and PA by FluSurver enabled by data from GISAID (https://flusurver.bii.a-star.edu.sg/).
Pyrosequencing (PSQ)
Cap Dependent Endonuclease PA of Influenza a Viruses
In order to perform rapid genotyping for the substitution I38X of the influenza virus cap dependent endonuclease (PA), which is associated with reduced susceptibility to baloxavir marboxil, a pyrosequencing method was designed and established, which is described in detail in the online protocol Pyrosequencing analysis for molecular marker I38X for reduced susceptibility of influenza A viruses to baloxavir marboxil [DOI: dx.doi.org/10.17504/protocols.io.n92ldzkpov5b/v1].
Primers were designed using PyroMark Assay Design version 2.0.2.5 (Qiagen, Germany) with A/Kansas/14/2017 (GISAID Acc.No EPI_ISL_292575) as reference; the reverse primer was biotinylated. PCR was validated using A(H1N1)pdm09 and A(H3N2) influenza A virus cell-cultured isolates. The 100 bp amplicons were analyzed on 1.5% agarose gels. Pyrosequencing was performed with up to 96 samples in parallel at 28°C with the PyroMark ID Instrument using PyroMark Q96 ID (Qiagen, Germany) enzyme and substrate mixture using SQA mode with 10fold CTGA and SNP analysis as described elsewhere.19
Phenotypic Analysis of Influenza Viruses
Virus Isolation
Influenza viruses were isolated by inoculating MDCK-SIAT 1 cell monolayers with 200 µL sterile filtered swab suspension in cell culture media (MEM/HEPES, containing EAA, L-Glutamine, Gentamycin, Geneticin, and 2 µg/mL TPCK-Trypsin).20 Cultures were incubated at 33°C and underwent daily microscopic examination for cytopathology, whereby culture media was changed twice a week. Once cytopathology of 75–100% was reached, the supernatant was harvested, the viral load was checked by hemagglutination titer (HA titer), and the supernatant stored at −80°C until further examination. If the hemagglutination titer (HA titer) was very low, a second passage was created and observed daily. After observing a cytopathic effect (CPE), successful virus cultivation was confirmed by rapid test (Quick_FLU A-B, Quidel, San Diego, USA) and the cultivation process was terminated. If the second passage of an influenza PCR-positive patient sample in the virus culture did not show a CPE, the rapid test (Quick_FLU A-B, Quidel, San Diego, USA) was used after 14 days of culturing to finally confirm the negative result.
NA Inhibition Test
Susceptibility of influenza viruses to neuraminidase inhibitors was measured in a fluorometric neuraminidase inhibition assay with 2’-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (Munana; Biosynth AG, Staad SG, Switzerland) used as substrate as described previously.19,21
Briefly, pre-titrated cell-cultured influenza viruses were adjusted to equivalent neuraminidase contents and preincubated with various concentrations (0 nM to 4000 nM) in MES buffer (32.5 mM morpholineethanesulfonic acid, pH 6.5) of oseltamivir carboxylate, zanamivir and peramivir (0 nM to 400 nM in MES buffer) for 1h at 37°C.
Additional incubation of 85 µM Munana in MES buffer for 2 h at 37°C was followed by adding stop solution (0.1 M glycine, 25% ethanol (99.7% stock), pH 10.7). Emitted fluorescence values of the released 4-methylumbelliferone were measured at wavelengths of 460 nm after excitation at wavelengths of 355 nm with a spectrofluorometer (Tecan AG, Männedorf, Switzerland). The 50% inhibitory concentration (IC50) for enzymatic activity of neuraminidase was determined from the dose–response curve, by using MS Excel software (MS Office 2010).19
The calculated 50% inhibition concentration values were means of 50% inhibitory concentration ± standard deviation (IC50 ± SD) of two- to fourfold examinations compared to reference IC50-values. According to WHO recommendations, reduced and highly reduced susceptibility to NAIs are defined by a ≥ 10 to 100-fold and >100-fold (influenza A) or ≥5 to 50-fold and >50-fold (influenza B) increase in the NAI IC50, compared to the NAI IC50 of the sensitive control (a wild-type virus of the same type or subtype).22
PA Inhibition Test
Cells and Virus
MDCK-SIAT1 cells (ECACC, Cat No. 05071502) were used for this assay, but not beyond passage 60. The MDCK-SIAT1 cells were grown in EMEM medium with 10% fetal bovine serum (FBS), 2mM L-Glutamine, 50µg/mL Gentamycin, 1% nonessential amino acids (NEAA) and 1mg/mL G418. Two different influenza A viruses were used for this study, A(H3N2) A/Hong Kong/1/1968 (HK/68) strain as a reference, and PA-I38M A(H3N2) to investigate baloxavir marboxil susceptibility. They were obtained by culturing in MDCK SIAT-1 cells in MEM/HEPES medium with the same supplements as mentioned above and stored at −80°C until use.
Virus Titration
MDCK-SIAT1 cells were seeded at the concentration of 3×105 cells/mL (100µL/well) in 96-well plates and incubated for 24 hours (5% CO2, 37°C). When cells were grown to 100% confluency and supernatants were removed, cells were washed gently twice with Trypsin EMEM (2 µg/mL Trypsin, 2mM L-Glutamine, 50µg/mL Gentamycin, 1% NEAA) to neutralize the culture media. Then, cells were inoculated in the plates with serial dilutions of virus and incubated for 24 or 48 hours in a 37°C incubator with 5% CO2 until at least 50% CPE (cytopathic effect) was observed by a light microscopy. A mixture of crystal violet (0.03%) and formaldehyde (3%) was used in a one-step procedure to stain cells. After supernatant was removed, cells were washed three times with Ca2+/Mg2+-free phosphate-buffered saline. Then, 50µL solution was added to fix and stain cells for 15min. After staining, cells were washed gently to remove the remaining solution. To elute crystal violet from cells, they were treated with 100µL lysis buffer (0.8979g of sodium citrate, 1.25mL of 1N HCl in 98.05mL 47.5% ethanol) for 20min. The optical densities (OD) were measured at 540/630nm using a Tecan Infinite 200 Pro (Tecan AG, Männedorf, Switzerland) photometer.23
PA Susceptibility Test
MDCK-SIAT1 cells were plated (3x104 cells/well) and incubated for 24 hours (37°C, 5% CO2). Virus dilutions were prepared, based on virus titration (HK/68:10−2, A(H3N2) PA-I38M substituted: 0.5). After washing twice with Trypsin EMEM, virus was inoculated to the MDCK-SIAT1 cells for 90 min at 37°C in 5% CO2 to absorb virus. Next, the plates were washed with PBS, and treated with baloxavir marboxil (25nM to 0.2nM, 2-fold dilution). The cells were incubated at 37°C in 5% CO2. The incubation time was different for each virus, according to the result from the virus titration (HK/68: 24 hours, PA-I38M: 24 to 48 hours), until a CPE was detectable in virus control. Cell staining and quantifying optical density (OD) procedures were done as outlined above. To calculate antiviral activity, the following equation was used:24
Results
Genotypic and Phenotypic Analyses of the Susceptibility of Influenza Viruses to Antiviral Compounds
Between week 40/2019 and week 39/2020, a total 1006 influenza viruses were detected in 5076 specimens analyzed at the German NIC. Subtyping of 847 influenza A viruses revealed co-circulation of influenza subtypes A(H1N1)pdm09 and A(H3N2) in roughly equal parts. Of the 134 type B viruses identified, 133 were B-Victoria-like (B-vic) and only one was a B-Yamagata-like virus (B-yam) (Table 1). Dual A(H3N2) / A(H1N1)pdm09 infections were detected in ten specimens, while A(H1N1)pdm09 / B-vic and A(H3N2) / B-vic dual infections were each detected in three specimens; no virus could be isolated from any specimen with dual infection. During the 2020/21 season, influenza circulation dropped to extraordinarily low levels and only three viruses (2 A(H3N2), 1 B-vic) were detected in a total 7190 specimens examined; cell-culture isolation and therefore further investigation failed.
 |
Table 1 Characterization of Influenza Viruses Circulating in Germany Between October 2019 and March 2022 |
During the 2021/22 influenza season, influenza viruses were detected at low levels, after NPIs had been eased. Between week 40/2021 and week 12/2022, a total 229 influenza viruses were detected in 4732 specimens; among these, 207 were classified as A(H3N2) and eleven as A(H1N1)pdm09; 40% of the detected influenza viruses were isolated by cell culture and further characterized (Table 1).
Susceptibility of Influenza Viruses to Neuraminidase Inhibitors
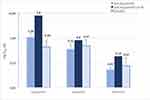
A total of 525 cell-cultured influenza viruses collected and isolated in 2019/20 were analyzed for susceptibility to oseltamivir, zanamivir and peramivir, using a neuraminidase inhibition assay. In addition, 88 viruses (85 A(H3N2, 2 A(H1N1)pdm09 and 1 B-vic) isolated in 2021/22 were analyzed for susceptibility to oseltamivir and zanamivir; peramivir susceptibility was not assessed because the marketing authorization for this agent had been revoked, leading to discontinuation of routine peramivir susceptibility screening. All NAIs were active against all types and subtypes of influenza tested, with peramivir being the most potent inhibitor (Figure 1). Resistance to NAI, which is defined by a ≥10-fold (influenza A) IC50 increase over the sensitive wild-type virus was not detected in any of the virus samples investigated. However, an A(H1N1)pdm09 isolate (A/NRW/142/2019), collected in December 2019 from an untreated, unvaccinated and otherwise healthy six-year old displayed an up to 7-fold IC50 increase for all three NAIs, and consequently oseltamivir, zanamivir and peramivir IC50s were classified as outliers (Figure 1).
To assess for the presence of molecular NAI resistance markers, NGS of neuraminidase genes was performed on 304 influenza viruses collected in 2019/20 and on 62 viruses collected in 2021/22, including the A(H1N1)pdm09 isolate A/NRW/142/2019 displaying reduced NAI susceptibility in vitro mentioned above. This virus was found to carry the NA-S247N substitution, which is known to slightly reduce NAI susceptibility and enhance NAI resistance induced by NA-H275Y (Figure 2). Neither the NA-H275Y substitution nor any other molecular markers associated with reduced NAI susceptibility or any molecular signatures were detected in the analyzed virus panel.
 |
Figure 2 Neuraminidase amino acid sequence alignment of A(H1N1)pdm09 isolate (A/NRW/142/2019) carrying the NA-S247N substitution and of vaccine strain A/Brisbane/02/2018 as wild-type reference. |
Susceptibility of Influenza Viruses to M2 Ion Channel Inhibitors (M2I)
All sequenced influenza A viruses of subtypes A(H3N2) and A(H1N1)pdm09 collected in 2019/20 (n = 325) and 2021/22 (n = 74), as well as all reference strains carried the molecular resistance marker M2-S31N, which is known to confer highly reduced susceptibility to M2I (Figure 3). Additionally, two A(H3N2) viruses (A/Berlin/9/2020, A/Saxony/5/2020), both collected in January 2020, carried the M2 substitution L27A, which is also associated with adamantane resistance.
Susceptibility of Influenza Viruses to Cap-Dependent Endonuclease Inhibitors (PAI)
Surveillance for molecular PAI resistance markers in 304 viruses collected in 2019/20 and 63 viruses collected in 2021/22 was based on NGS of the PA gene. It revealed presence of the PA-I38M substitution in an A(H3N2) virus (A/Berlin/9/2020) collected in January 2020 from a 66-year old, unvaccinated, untreated, and otherwise healthy female (Figure 4). This PA-I38M substitution is associated with reduced susceptibility to the PAI baloxavir marboxil and is known to lead to mild attenuation of the virus.25 To enable rapid PA-I38X genotyping, a pyrosequencing method was established and validated, using PCR amplification and sequence primers that were designed based on published and in-house NGS data. Next, we wished to assess whether the PA-I38M substitution remains stable during cell culture propagation even in the absence of drug selective pressure. Therefore, pyrosequencing analyses were performed, comparing c-DNA from primary material and from cell-culture propagated virus side-by-side. Both, the primary clinical sample as well as the cell cultured virus isolate, displayed the PA-I38M substitution (Figure 5).
Additionally, a cell-based inhibition assay for analyzing the susceptibility against baloxavir marboxil of the A(H3N2) PAI-I38M virus was established and validated, using the PAI-susceptible A/Hong Kong/1/1968 (HK/68) strain as reference wildtype virus.
Compared to the HK/68 virus, the PA-I38M mutant grew more slowly and took up to 24 hours longer to form a satisfactory CPE. Inhibition tests with serial dilutions of baloxavir marboxil showed an up to 5-fold reduction of antiviral activity of baloxavir marboxil in the PA-I38M isolate (A/Berlin/9/2020) compared to the reference virus (data not shown).
Discussion
Here we report both the phenotypic and genotypic antiviral susceptibility profiles of influenza viruses, monitored at the German national level over the last three years. Our data reveal that viruses displaying reduced antiviral in vitro susceptibility, or presence of molecular resistance markers are low in frequency. Antiviral agents against influenza are prescribed less frequently in Germany than in other countries; thus, it can be assumed that the selection pressure leading to the emergence of antiviral-resistant influenza viruses is considerably lower than, for example, in Japan, where use of these agents is widespread. However, our data provide real-life evidence that influenza antiviral resistance can arise in the absence of such selection pressure, occurring spontaneously even in untreated patients. Circulation and wider spread of such viruses carrying minor resistant variants within their quasispecies could lead to failure of an antiviral drug or even an entire drug class.10 This was observed in 2004 with the occurrence and spread of adamantane resistant influenza A(H3N2) viruses due to the M2-S31N substitution, resulting in the abandonment of adamantane use and loss of this entire drug class for influenza therapy.26 Similarly, the spread of oseltamivir resistant A(H1N1) viruses in the 2007/08 winter resulted in failure of one of the two NAIs licensed at the time; the later-approved peramivir displayed reduced efficacy due to cross-resistance.27,28 These viruses remained sensitive to zanamivir, at that time the only effective anti-influenza drug with certain limitations, including its application by inhalation rather than orally. Ever since the pandemic A(H1N1)pdm09 influenza virus has replaced seasonal A(H1N1) viruses in 2009, all circulating influenza A viruses have displayed NAI sensitivity and adamantane resistance.9,29,30 With the development of baloxavir marboxil (BLX), a novel drug class with a distinct mode of action has recently been approved for treatment of uncomplicated influenza.6,31,32 Recent clinical studies indicated that PA substitutions associated with BLX resistance, leading to an increase of TCID50 in phenotypic assays may arise rapidly.33–35 These substituted influenza viruses have been observed even in untreated influenza patients and seem to be stable during virus growth in cell culture.36–38 We detected the PA-I38M substitution in an A(H3N2) German primary specimen as well as the corresponding virus isolate. This substitution is known to confer a mild reduction of baloxavir marboxil susceptibility in vitro . During cell culture propagation, the proportion of PA-I38M viruses decreased, suggesting a detrimental effect of this substitution on virus growth. This observation confirms the findings of Chesnokov et al, who described a mild attenuation of PA-I38M viruses.25 On the other hand, selection of antiviral-resistant minor variants present within the quasispecies will likely occur during therapy. Almost three years since the beginning of the COVID-19 pandemic with very low concurrent circulation of influenza viruses, the coming influenza seasons will affect populations who have had little or no recent antigen contact for a relatively long time. Accordingly, higher levels of infections and a correspondingly high burden of disease are to be expected. The European I-MOVE network estimated preliminary influenza vaccine effectiveness against influenza A to be 36% (95% CI: 13–53) for all ages the 2020–2021 influenza season, based on seven study sites.39,40 For the 2019–2020 influenza season, the vaccine effectiveness point estimates for all ages were 29% to 61% against any influenza in the primary care setting.41 The clinical efficacy of vaccines depends not only on the circulating viruses, but is also influenced by e.g. the vaccination regimen, the adjuvant used, the duration of immunity induced by the particular vaccine virus, and the immune status of the vaccinee, which is determined by age, previous antigenic contacts with influenza viruses, immunological reactivity, and the timing of vaccination. With low vaccination prevalence and also low vaccine effectiveness, antiviral therapeutics will play a crucial role in the mitigation of upcoming influenza seasons. In order to preserve their efficiency, the risk of antiviral resistance emergence must be minimized. This provides the rationale not only for diligent antiviral resistance surveillance, but also for annual immunization campaigns, which help to decrease the use of antivirals. Finally, with only two classes of antiviral drugs available, of which one might be prone to induce antiviral resistance, there is an urgent need to advance the development of new antiviral compounds.
Conclusion
While the current frequency of influenza viruses demonstrating reduced antiviral susceptibility in Germany is low (<1%), antiviral resistance does occur spontaneously and even in the absence of treatment selection pressure. Therefore, the evolution of influenza viruses, their in vitro susceptibility to antivirals and the occurrence of molecular resistance markers need to be continuously monitored.
Acknowledgments
We are indebted to the patients, their families and the sentinel clinicians who have made these studies possible. The authors are most grateful to the laboratory team at the National Influenza Centre for excellent technical assistance; Ute Preuß, Anabel Hales, Louisa Schmidt and Mariella Szafraniec for outstanding support in recruiting sentinel physicians and coordinating the liaison with them; and Bernd Reinhardt for providing invaluable data management support. We would like to thank Andrea Thürmer and Aleksandar Radonic for the next-generation sequencing of the influenza genomes and Katja Winter and Sandra Kaiser for the bioinformatic analysis of the NGS data. We gratefully acknowledge the authors, originating and submitting laboratories of the sequences from GISAID’s EpiFlu™ Database on which this research is based.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Iuliano AD, Roguski KM, Chang HH, et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet. 2018;391(10127):1285–1300. doi:10.1016/s0140-6736(17)33293-2
2. Krammer F, Smith GJD, Fouchier RAM, et al. Influenza. Nat Rev Dis Primers. 2018;4(1):3. doi:10.1038/s41572-018-0002-y
3. Duwe SC, Schmidt B, Gärtner BC, et al. Prophylaxis and treatment of influenza: options, antiviral susceptibility, and existing recommendations. GMS Infect Dis. 2021;9:Doc02. doi:10.3205/id000071
4. Hayden FG, Sugaya N, Hirotsu N, et al. Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med. 2018;379(10):913–923. doi:10.1056/NEJMoa1716197
5. Ikematsu H, Hayden FG, Kawaguchi K, et al. Baloxavir marboxil for prophylaxis against influenza in household contacts. N Engl J Med. 2020;383(4):309–320. doi:10.1056/NEJMoa1915341
6. Baker J, Block SL, Matharu B, et al. Baloxavir marboxil single-dose treatment in influenza-infected children: a randomized, double-blind, active controlled Phase 3 safety and efficacy trial (miniSTONE-2). Pediatr Infect Dis J. 2020;39(8):700–705. doi:10.1097/inf.0000000000002747
7. Ison MG, Portsmouth S, Yoshida Y, et al. Early treatment with baloxavir marboxil in high-risk adolescent and adult outpatients with uncomplicated influenza (CAPSTONE-2): a randomised, placebo-controlled, phase 3 trial. Lancet Infect Dis. 2020;20(10):1204–1214. doi:10.1016/s1473-3099(20)30004-9
8. Govorkova EA, Takashita E, Daniels RS, et al. Global update on the susceptibilities of human influenza viruses to neuraminidase inhibitors and the cap-dependent endonuclease inhibitor baloxavir, 2018–2020. Antiviral Res. 2022;200:105281. doi:10.1016/j.antiviral.2022.105281
9. Lackenby A, Besselaar TG, Daniels RS, et al. Global update on the susceptibility of human influenza viruses to neuraminidase inhibitors and status of novel antivirals, 2016–2017. Antiviral Res. 2018;157:38–46. doi:10.1016/j.antiviral.2018.07.001
10. Hussain M, Galvin HD, Haw TY, Nutsford AN, Husain M. Drug resistance in influenza A virus: the epidemiology and management. Infect Drug Resist. 2017;10:121–134. doi:10.2147/idr.s105473
11. Oh DY, Buda S, Biere B, et al. Trends in respiratory virus circulation following COVID-19-targeted nonpharmaceutical interventions in Germany, January - September 2020: analysis of national surveillance data. Lancet Reg Health Europe. 2021;6:100112. doi:10.1016/j.lanepe.2021.100112
12. Zhang Y, Yakob L, Bonsall MB, Hu W. Predicting seasonal influenza epidemics using cross-hemisphere influenza surveillance data and local internet query data. Sci Rep. 2019;9(1):3262. doi:10.1038/s41598-019-39871-2
13. Australian Government, Department of Health and Age Care. Australian Influenza Surveillance Reports (AISR); 2022. Available from: https://www.health.gov.au/sites/default/files/documents/2022/10/aisr-fortnightly-report-no-14-26-september-to-9-october-2022.pdf.
14. World Health Organization. Bi-weekly influenza situation update; Western Pacific Region. World Health Organization; 2022. Available from: https://www.who.int/docs/default-source/wpro---documents/emergency/surveillance/seasonal-influenza/influenza-20220727.pdf?sfvrsn=39dcc97a_103.
15. Schulze M, Nitsche A, Schweiger B, Biere B, Liu DX. Diagnostic approach for the differentiation of the pandemic influenza A(H1N1)v virus from recent human influenza viruses by real-time PCR. PLoS One. 2010;5(4):e9966. doi:10.1371/journal.pone.0009966
16. Rath B, Chen X, Spies V, et al. Prospective surveillance of antiviral resistance in hospitalized infants less than 12 months of age with A(H3N2) influenza infection and treated with oseltamivir. Antivir Ther. 2017;22(6):515–522. doi:10.3851/imp3141
17. Zhou B, Donnelly ME, Scholes DT, et al. Single-reaction genomic amplification accelerates sequencing and vaccine production for classical and Swine origin human influenza a viruses. J Virol. 2009;83(19):10309–10313. doi:10.1128/jvi.01109-09
18. Zhou B, Lin X, Wang W, et al. Universal influenza B virus genomic amplification facilitates sequencing, diagnostics, and reverse genetics. J Clin Microbiol. 2014;52(5):1330–1337. doi:10.1128/jcm.03265-13
19. Duwe S, Schweiger B. A new and rapid genotypic assay for the detection of neuraminidase inhibitor resistant influenza A viruses of subtype H1N1, H3N2, and H5N1. J Virol Methods. 2008;153(2):134–141. doi:10.1016/j.jviromet.2008.07.017
20. Matrosovich M, Matrosovich T, Carr J, Roberts NA, Klenk HD. Overexpression of the −2,6-Sialyltransferase in MDCK Cells Increases Influenza Virus Sensitivity to Neuraminidase Inhibitors. J Virol. 2003;77(15):8418–8425. doi:10.1128/jvi.77.15.8418-8425.2003
21. Rath BC, Spies X, Muehlhans V, et al. Prospective surveillance of antiviral resistance in hospitalized infants less than 12 months of age with A(H3N2) influenza infection and treated with oseltamivir. Antivir Ther. 2016;22(6):515–522.
22. World Health Organization. Meetings of the WHO working group on surveillance of influenza antiviral susceptibility- Geneva, November 2011 and June 2012. Available from: https://apps.who.int/iris/bitstream/handle/10665/241965/WER8739_369-374.PDF?sequence=1&isAllowed=y.
23. Schmidtke M, Schnittler U, Jahn B, Dahse H, Stelzner A. A rapid assay for evaluation of antiviral activity against coxsackie virus B3, influenza virus A, and herpes simplex virus type 1. J Virol Methods. 2001;95(1–2):133–143. doi:10.1016/s0166-0934(01)00305-6
24. Pauwels R, Balzarini J, Baba M, et al. Rapid and automated tetrazolium-based colorimetric assay for the detection of anti-HIV compounds. J Virol Methods. 1988;20(4):309–321. doi:10.1016/0166-0934(88)90134-6
25. Chesnokov A, Patel MC, Mishin VP, et al. Replicative fitness of seasonal influenza a viruses with decreased susceptibility to baloxavir. J Infect Dis. 2020;221(3):367–371. doi:10.1093/infdis/jiz472
26. Bright RA, Medina MJ, Xu X, et al. Incidence of adamantane resistance among influenza A (H3N2) viruses isolated worldwide from 1994 to 2005: a cause for concern. Lancet. 2005;366(9492):1175–1181. doi:10.1016/S0140-6736(05)67338-2
27. Sheu TG, Deyde VM, Okomo-Adhiambo M, et al. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob Agents Chemother. 2008;52(9):3284–3292. doi:10.1128/AAC.00555-08
28. Ciancio BC, Meerhoff TJ, Kramarz P, et al. Oseltamivir-resistant influenza A(H1N1) viruses detected in Europe during season 2007–8 had epidemiologic and clinical characteristics similar to co-circulating susceptible A(H1N1) viruses. Euro Surveill. 2009;14(46). doi:10.2807/ese.14.46.19412-en
29. Takashita E, Meijer A, Lackenby A, et al. Global update on the susceptibility of human influenza viruses to neuraminidase inhibitors, 2013–2014. Antiviral Res. 2015;117:27–38. doi:10.1016/j.antiviral.2015.02.003
30. Hurt AC, Besselaar TG, Daniels RS, et al. Global update on the susceptibility of human influenza viruses to neuraminidase inhibitors, 2014–2015. Antiviral Res. 2016;132:178–185. doi:10.1016/j.antiviral.2016.06.001
31. Taieb V, Ikeoka H, Ma FF, et al. A network meta-analysis of the efficacy and safety of baloxavir marboxil versus neuraminidase inhibitors for the treatment of influenza in otherwise healthy patients. Curr Med Res Opin. 2019:1–10. doi:10.1080/03007995.2019.1584505
32. Vasiliy PM, Mira CP, Anton C, et al. Susceptibility of influenza A, B, C, and D viruses to baloxavir. Emerg Infect Dis J. 2019;25(10). doi:10.3201/eid2510.190607
33. Abed Y, Fage C, Checkmahomed L, Venable MC, Boivin G. Characterization of contemporary influenza B recombinant viruses harboring mutations of reduced susceptibility to baloxavir marboxil, in vitro and in mice. Antivir Res. 2020;179:104807. doi:10.1016/j.antiviral.2020.104807
34. Imai M, Yamashita M, Sakai-Tagawa Y, et al. Influenza A variants with reduced susceptibility to baloxavir isolated from Japanese patients are fit and transmit through respiratory droplets. Nature Microbiol. 2020;5(1):27–33. doi:10.1038/s41564-019-0609-0
35. Sato M, Takashita E, Katayose M, et al. Detection of variants with reduced baloxavir marboxil susceptibility after treatment of children with influenza A during the 2018–2019 influenza season. J Infect Dis. 2020;222(1):121–125. doi:10.1093/infdis/jiaa061
36. Omoto S, Speranzini V, Hashimoto T, et al. Characterization of influenza virus variants induced by treatment with the endonuclease inhibitor baloxavir marboxil. Sci Rep. 2018;8(1):9633. doi:10.1038/s41598-018-27890-4
37. Takashita E, Ichikawa M, Morita H, et al. Human-to-Human Transmission of Influenza A(H3N2) virus with reduced susceptibility to baloxavir, Japan, February 2019. Emerg Infect Dis. 2019;25(11):2108–2111. doi:10.3201/eid2511.190757
38. Takashita E, Kawakami C, Ogawa R, et al. Influenza A(H3N2) virus exhibiting reduced susceptibility to baloxavir due to a polymerase acidic subunit I38T substitution detected from a hospitalised child without prior baloxavir treatment, Japan, January 2019. Euro Surveill. 2019;24(12). doi:10.2807/1560-7917.es.2019.24.12.1900170
39. Valenciano M, Ciancio BC; on behalf of the I-MOVE study team C. I-MOVE: a European network to measure the effectiveness of influenza vaccines. Eurosurveillance. 2012;17(39):20281. doi:10.2807/ese.17.39.20281-en
40. Imoveflu. Preliminary influenza vaccine effectiveness estimates for 2021–22. I-Move 2020; 2022. Available from: https://www.imoveflu.org/news/.
41. Rose A, Kissling E, Emborg H-D, et al. Interim 2019/20 influenza vaccine effectiveness: six European studies, September 2019 to January 2020. Eurosurveillance. 2020;25(10):2000153. doi:10.2807/1560-7917.ES.2020.25.10.2000153
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.